Abstract
Background
We compared serum vitamin C (VIC) status of the adult (≥20 years) US population in the National Health and Nutrition Examination Survey (NHANES) 2017–2018 with combined data from 2003–2004 and 2005–2006.
Methods
VIC was measured using high performance liquid chromatography (HPLC) with electrochemical detection. Mean data were stratified by age, sex, race/Hispanic origin, income, body mass index, dietary intake, supplement use, and smoking status. Prevalence of VIC deficiency (<11.4 μmol/L) was calculated.
Results
In NHANES 2017–2018, the mean VIC was 8 μmol/L higher in people ≥60 y compared with those 20–59 y old, 10 μmol/L lower in men vs women, 8 μmol/L lower in low vs high income, 11 μmol/L lower in obese vs healthy weight, and 15 μmol/L lower in smokers vs non-smokers. Differences in mean VIC across race/Hispanic origin groups ranged from 2–7 μmol/L. Mean VIC was 27 μmol/L higher with vitamin C-containing supplement use and positively associated (Spearman ρ=0.33; p<0.0001) with increasing dietary intake. The associations between mean VIC and the investigated covariates were generally consistent between the survey periods. The prevalence of deficiency was not significantly different between survey periods (6.8% vs 7.0%; p=0.83). However, a few subgroups, such as those with low dietary intake and smokers, had double the risk. We found no significant survey differences in mean VIC (51.2 vs 54.0 μmol/L; p=0.09).
Conclusions
Overall VIC status of the US adult population has remained stable since last assessed in the NHANES 2005–2006 survey. Vitamin C deficiency remained high for those with low dietary intake and who smoke.
Keywords: NHANES, ascorbic acid, survey, HPLC, scurvy
Introduction
Vitamin C is an essential nutrient that comes from fruits, vegetables, fortified foods and supplements. The main sources of vitamin C in the US diet are citrus, tomato products and potatoes (1). Consuming only five varied servings of fruits and vegetables a day can provide more than 200 mg of vitamin C (2), a level more than twice the current 90 mg Daily Value (3). As an indicator of serum vitamin C (VIC) status, stabilized serum or plasma concentrations are measured. VIC concentrations <11.4 μmol/L define prevalence of VIC deficiency. Within 1 month of little to no vitamin C intake, signs and symptoms of vitamin C deficiency can occur (2). These may include fatigue, loss of appetite, easy bruising, dry skin and bleeding gums. Ascorbic acid (10 mg/day) will cure or prevent scurvy, the severest form of vitamin C deficiency (4).
There is only one US population survey that uses biological specimens to study the health and nutritional status of the noninstitutionalized civilian population. The National Health and Nutrition Examination Survey (NHANES) is a two-year nationally representative study using questionnaires combined with physical examinations and biochemical measurements. The CDC lab measures VIC for NHANES. Additional NHANES data include demographic factors such as age, sex, and race/Hispanic origin and lifestyle factors such as dietary intake and supplement use. Based on NHANES data, vitamin C dietary intake in US adults decreased by ~13% from 2003 to 2018 (5). From the literature, overall dietary supplement use increased by ~4% from 2007–2008 to 2017–2018 (6). As has been shown previously, smoking and obesity were associated with lower mean VIC and increased deficiency (7). The percentage of adults who smoked declined by ~10% from 2003–2006 to 2017–2018 (unpublished observations). However, the prevalence of obesity among adults increased by ~9% from 2003–2006 to 2017–2018 (8).
Although VIC is the preferred vitamin C status indicator, 24-hr dietary recall is more commonly used such as in the 2013 Philippine National Nutrition Survey and 2008–2012 Korean NHANES (9, 10). Among the few recent surveys that measured serum or plasma vitamin C are the UK National Diet Survey (2008–2010) and the Canadian Health Measures Survey (2012–2013) (11, 12). VIC was last measured in the US population during the 2005–2006 NHANES. Because not all nutritional biomarkers can be monitored continuously throughout NHANES, it is important to periodically assess and document whether changes in the US population occurred over time. The aim of this study was to update the information on the VIC status in the US population.
Methods
Study Design and Participants
Since 1999, NHANES has been a continuous survey with public use data released in 2-y survey periods. The two-year weights released as part of the public-use data provide nationally representative estimates for the US civilian noninstitutionalized population. Through 2006 the NHANES sampling domains included oversampling of Mexican-American people, adolescents aged 12–19 y, older people aged ≥60 y, and a supplemental sample of pregnant women. Starting in 2007, NHANES no longer oversampled adolescents and pregnant women, oversampled the entire Hispanic population (compared to only the Mexican-American population), non-Hispanic Black people, low-income non-Hispanic White people and other people, and non-Hispanic White people and other people aged ≥80 y. In 2011, NHANES began also oversampling Asian-American people. More details on the NHANES sampling designs can be found elsewhere (13–15). Overall response rates for the examined sample in 2003–2004, 2005–2006 and 2017–2018 were 76%, 77% and 49%. Complete interview and examination response rates for each survey period are publicly available on the NHANES website (16). The current study compared NHANES 2017–2018 with the combined data from NHANES 2003–2004 and 2005–2006. There was no evidence of a statistically significant difference of average serum vitamin C levels between NHANES 2003–2004 and 2005–2006, 53.9 μmol/L [95% CI (51.2, 56.6)] compared to 54.0 μmol/L [95% CI (52.6, 55.1)], respectively (p=0.92). Therefore, the cycles were combined to increase sample size and improve statistical precision. (17). Of the 14,780 persons 20 years and older who were interviewed and examined, 13,824 (93%) had serum vitamin C measurements. Participants were categorized by age (overall ≥20 y, 20–39 y, 40–59 y, or ≥60 y), sex (men or women), race/Hispanic origin (Mexican American, non-Hispanic Asian, non-Hispanic Black, or non-Hispanic White). Participants self-reported race and Hispanic origin. Although non-Hispanic Asian people have been oversampled since NHANES 2011–2012, NHANES 2017–2018 was the first-time representative data for non-Hispanic Asian people were available for VIC. Individuals whose race/Hispanic origin was recorded as “other Hispanic” or “other race”, including people who report multiple races, were too small to reliably report separately but included in the overall and all other demographic and lifestyle categories. Poverty income ratio (PIR), which is the ratio of family income to poverty guidelines specific to family size. PIR was defined as low (0–1.85), middle (1.86–3.5), or high (>3.5). Body mass index (BMI) was defined as healthy weight (18.5–24.99 kg/m2), overweight (25–29.99 kg/m2), or obesity (≥30 kg/m2). Self-reported 24-hour total dietary vitamin C intake on questionnaire recorded at the mobile examination center (MEC) as reliable was stratified in quartiles as: 0–<20, 20–<50, 50–<110, and ≥110 mg/day. Any vitamin C-containing supplement use in the previous thirty days was assessed. Serum cotinine concentrations were used to determine smoking status: non-smokers (≤10 ng/mL) and smokers (>10 ng/mL).
For all surveys, serum was obtained within 30 minutes of blood clotting. One part serum was mixed with four parts 6% metaphosphoric acid to stabilize ascorbic acid. The metaphosphoric acid-stabilized sera were shipped frozen. In our laboratory, samples were stored at −70°C until analysis.
Laboratory Method
A sensitive chromatographic method with electrochemical detection was used for quantitating VIC in NHANES 2003–2004, 2005–2006 and 2017–2018 (7, 18). For NHANES 2003–2006 VIC (oxidized and reduced) was measured as described by McCoy et al. with the following equipment and/or setting changes for NHANES 2017–2018 (19). A 4-μL injection was separated using a Waters Acquity UPLC HSS T3 column (1.8 μm particle size (100Å); 150 mm × 2.1 mm (inner diameter)) at a flow rate of 0.4 mL/min. All chromatographic peaks eluted within 8 min and VIC was detected on a Waters 2465 electrochemical detector set at +450mV with a 2 mm glassy carbon working electrode and in situ Ag/AgCl (ISAAC) reference electrode. For NHANES 2017–2018, the analytical measurement range was 7.3 – 146 μmol/L. Limit of detection was 1.7 μmol/L. Bench QC pool means (3 pools measured in each analytical run in duplicate) ranged from 15.8–118 μmol/L with an overall CV of 4%. Blind QC pool means (6 different pools with 1 pool per 20 samples) ranged from 11.2–98.6 μmol/L with an overall CV of 6%. See Supplemental Table 1 for QC pool statistic details. Bench QC were evaluated using a SAS Institute Incorporated (Cary, NC) QC program (20). Blind QC results were evaluated against 3SD of the characterization means (20 runs per pool). Two levels of National Institute of Standards and Technology (Gaithersburg, MD) NIST standard reference material (SRM) 970 were obtained for NHANES surveys. They were used during NHANES 2003–2006 (~18 runs) and in 2017–2018 (~22 runs) average differences from targets ranged from −0.3% to 0.4%. The laboratory methods for measuring VIC are thoroughly documented on the National Center for Health Statistics (NCHS) website (21–23).
Statistical Analysis
We performed statistical analyses using SAS (version 9.4) and SAS-callable SUDAAN (version 11.0.3, RTI, Research Triangle Park, NC), to account for the complex sample design. Variance estimation was based on Taylor Series Linearization and the MEC weights were used to account for unequal probabilities of selection, nonresponse and noncoverage. Degrees of freedom (df) were calculated based on the total number of primary sampling units minus the number of strata defined by the survey design. Weighted arithmetic means for VIC concentrations and weighted prevalences of VIC deficiency are shown for selected variables, for NHANES 2017–2018. Prevalence estimates were suppressed if they did not meet the statistical reliability criteria (24). Spearman correlation was used to assess the association between VIC and selected variables (25). Further, bivariate associations for each nutritional biomarker and categorical variables were based on geometric means (or arithmetic means where appropriate) and 95% confidence intervals across the categories. For the historical comparisons, weighted arithmetic means are computed from combined NHANES 2003–2004 and 2005–2006 cycles to provide estimates with greater statistical precision. Four-year weights for 2003–2006 were calculated using the original two-year MEC weights (original weight/2). P-values to compare either the weighted means or weighted prevalences across multiple categories were based on an overall Wald F-test. If the null hypothesis of equality among the means or prevalences across the categories was rejected at 0.05 significance level, pairwise tests were performed applying the Bonferroni method to control for multiple comparisons using a t-statistic with 15 df. Estimated mean differences between 2017–2018 and 2003–2006 along with 95% confidence intervals are presented to assess whether there have been any changes. P-values for the pairwise differences between the two survey periods for each category were assessed using a t-statistic with 45 df. Multiple linear regression modeling was used to explore correlates of VIC concentrations. The a priori modeling plan was to enter all pre-selected variables into a regression model (25). The pre-selected variables were: age, sex, race/Hispanic origin, PIR, BMI, dietary vitamin C intake, vitamin C-supplement use, and smoking status. A 0.05 significance level to stay was evaluated against Satterthwaite adjusted F p-values in combination with whether the covariable was a potential confounder regardless of statistical significance. The final step was to investigate all pairwise interactions between variables in the model. In the interest of parsimony, the beta coefficients for significant interactions were not presented in the final regression model. However, to demonstrate that these interactions did not appreciably change the pattern of the associations between the variables and VIC, the conditional marginal means from the final model with the interactions included are presented for the statistically significant pairwise interactions.
Results
Prevalence in NHANES 2017–2018
The prevalence of VIC deficiency in 2017–2018 is shown in Table 1. We assessed absolute differences between categories. There were no significant differences in prevalence of VIC deficiency among age subgroups or sex. Among race/Hispanic origin groups the only significant difference in prevalence was between non-Hispanic White people and non-Hispanic Asian people with non-Hispanic Asian people having lower prevalence by 4.7% [95% CI (2.0%, 7.4%)]. High income was associated with significantly lower prevalence of VIC deficiency compared to low income, a difference of 5.2% [95% CI (2.7%, 7.8%)]. Although the healthy weight and obesity VIC deficiency prevalences are similar (~0.1% different), the only significant difference in BMI categories was between those with obesity compared to overweight adults, a difference of 3.2% [95% CI (1.2%, 5.3%)]. Low (<20 mg/day) vitamin C dietary intake was associated with the highest risk of VIC deficiency whereas high (≥110 mg/day) intake was associated with the lowest risk, a difference of 11.8% [95% CI (8.4%, 15.2%)]. Likewise, those whose intake was between 50–110 mg/day had a difference of 11.0% [95% CI (7.3%, 14.7%)] compared to those with the lowest intake (<20 mg/day). Prevalence of VIC deficiency was significantly lower in vitamin C-containing supplement users compared to non-users, a difference of 9.0% [95% CI (6.0%, 11.9%)]. Non-smokers had significantly lower prevalence of VIC deficiency compared to smokers, a difference of 10.2% [95% CI (6.2%, 14.3%)].
Table 1.
For the US population 20 years and older, weighted prevalence (in percent) of vitamin C deficiency (serum vitamin C <11.4 μmol/L) and weighted mean serum vitamin C concentrations, National Health and Nutrition Examination Survey, 2017–2018
| Variables | Variable Categories | n | Prevalence (95% CI)1 | Wald F | Mean (95% CI)1 | Wald F |
|---|---|---|---|---|---|---|
| (%) | p-value2 | (μmol/L) | p-value2 | |||
| Age (years) | Overall ≥20 | 4,932 | 6.8 (5.0, 9.0) | 0.69 | 51.2 (48.3, 54.1) | 0.0005 |
| 20–39 | 1,463 | 6.2 (4.1, 9.3) | 48.4 (45.3, 51.6)a | |||
| 40–59 | 1,563 | 7.0 (5.1, 9.5) | 49.4 (46.3, 52.5)a | |||
| ≥60 | 1,906 | 7.2 (5.1, 9.9) | 56.8 (53.0, 60.6)b | |||
| Sex | Men | 2,377 | 7.7 (5.5, 10.6) | 0.10 | 46.1 (43.2, 48.9)a | <0.0001 |
| Women | 2,555 | 5.9 (4.3, 8.1) | 56.0 (52.8, 59.3)b | |||
| Race/Hispanic Origin | Mexican American | 675 | 4.5 (2.6, 7.7)a,b | 0.0313 | 49.7 (45.0, 54.4)a,b | 0.0085 |
| Non-Hispanic Asian | 693 | 3.0 (2.2, 4.1)b | 54.6 (51.6, 57.6)b | |||
| Non-Hispanic Black | 1,117 | 6.0 (3.5, 10.0)a,b | 47.4 (44.0, 50.8)a | |||
| Non-Hispanic White | 1,728 | 7.7 (5.5, 10.6)a | 52.2 (48.8, 55.6)a,b | |||
| Poverty Income Ratio | Low (0 – 1.85) | 1,893 | 9.8 (6.9, 13.6)a | 0.002 | 46.3 (42.5, 50.1)a | 0.0004 |
| Middle (1.86 – 3.5) | 1,095 | 6.7 (4.5, 10.0)a,b | 52.1 (47.9, 56.4)b | |||
| High (>3.5) | 1,304 | 4.6 (3.0, 6.8)b | 54.2 (50.6, 57.8)b | |||
| Body Mass Index3 (kg/m2) | Healthy (18.5 – 24.99) | 1,173 | 7.6 (5.2, 11.1)a,b | 0.0154 | 56.1 (51.7, 60.5)a | <0.0001 |
| Overweight (25 – 29.99) | 1,563 | 4.4 (3.0, 6.4)a | 55.9 (53.4, 58.3)a | |||
| Obesity (≥30) | 2,049 | 7.7 (5.5, 10.5)b | 45.4 (42.3, 48.5)b | |||
| Dietary Intake Quartiles (mg/day) | (0 – <20) | 1,163 | 13.9 (10.5, 18.3)a | <0.0001 | 41.2 (37.3, 45.0)a | <0.0001 |
| (20 – <50) | 1,139 | 7.4 (5.2, 10.4)b | 45.5 (41.9, 49.2)b | |||
| (50 – <110) | 1,095 | 2.9 (1.9, 4.6)c | 56.2 (53.4, 59.0)c | |||
| ≥110 | 1,085 | 2.2 (1.1, 4.2)c | 63.3 (59.8, 66.7)d | |||
| Vitamin C-containing Supplement Use | Yes | 1,133 | 0.5 (0.2, 1.5)a | <0.0001 | 70.6 (67.5, 73.7)a | <0.0001 |
| No | 3,336 | 9.2 (6.9, 12.1)b | 43.5 (40.9, 46.2)b | |||
| Smoking Status | Non-smokers | 3,751 | 4.4 (3.2, 5.9)a | 0.0002 | 54.7 (51.6, 57.7)a | <0.0001 |
| Smokers | 1,162 | 14.6 (10.6, 19.8)b | 39.9 (36.8, 43.1)b |
Compact letter display is used to show statistically significant differences between pairwise comparisons after Bonferroni adjustment. Categories sharing one or more letters were not significantly different. Pairwise comparisons were only assessed if the null hypothesis of equality among the prevalences across the categories was rejected at 0.05 significance level.
P-value based on Wald F test, which tests whether at least one of the prevalences or means across the categories were significantly different
Relative CI width for underweight was greater than 130%. Estimate was suppressed (23).
Mean concentrations in NHANES 2017–2018
Mean VIC concentrations stratified by demographic or lifestyle factors for NHANES 2017–2018 are shown in Table 1. Based on age, 60+y adults had significantly higher mean VIC than other age groups ranging 7.4 – 8.4 μmol/L. Women had significantly higher VIC than men by 10.0 μmol/L [95% CI (7.7, 12.3)]. Among race/Hispanic origin groups, the only significant difference was between non-Hispanic Black people and non-Hispanic Asian people with non-Hispanic Asian people higher by 7.2 μmol/L [95% CI (3.4, 11.0)]. Mean VIC was 5.9–7.9 μmol/L higher in the middle and high PIR groups compared to low PIR. Adults with healthy weight or overweight had 10.5–10.7 μmol/L significantly higher vitamin C than adults with obesity. VIC concentrations were significantly higher in each ascending dietary intake quartile ranging 4.3 – 22.1 μmol/L compared to the lowest (<20 mg/day). Mean VIC concentrations were significantly higher by 22.3 μmol/L [95% CI (19.5, 25.1)] in those taking vitamin C-containing supplements. Non-smokers had significantly higher mean VIC than smokers by 14.8 μmol/L [95% CI (11.7, 17.8)].
Regression Model
After adjusting for all covariates, there were no longer any significant differences among race/Hispanic origin groups or PIR seen in 2017–2018 (Table 2). But differences in mean VIC concentrations by age, sex, BMI, dietary vitamin C intake, vitamin C-containing supplement use, and smoking status continued to be statistically significant. Namely, adults 40–59 y had 5.3 μmol/L [95% CI (2.3, 8.3)] lower VIC concentrations than those ≥60 y. VIC concentrations in women were higher than men by 5.7 μmol/L [95% CI (2.5, 8.9)]. Adults with healthy weight or overweight had 8.3–9.3 μmol/L higher VIC concentrations. Those in the highest quartile of dietary intake had 17.5 μmol/L [95% CI (13.9, 21.2)] higher VIC than those in the lowest quartile while those who consumed vitamin C-containing supplements had 19.2 μmol/L [95% CI (16.7, 21.6)] higher VIC concentrations than those who did not. Non-smokers had 8.6 μmol/L [95% CI (5.9, 11.3)] higher VIC concentrations than smokers. After examining all the pairwise interactions from the model, there were three statistically significant interactions: age and sex (p=0.0243), age and vitamin C-containing supplement use (p=0.0001), and sex and smoking status (p=0.0247). Selected estimated conditional marginal means from the model presented in Table 2 plus the three significant interactions are shown in Figure 1 to demonstrate the interpretation of the significant interactions. Figure 1a demonstrates a larger significant difference in VIC between men and women aged ≥60 y (12.2 μmol/L; p<0.0001) compared to those 20–39 y (7.4 μmol/L; p=0.0005). Figure 1b demonstrates that differences in VIC among supplement users compared to non-users were larger among those ≥60 y (28.5 μmol/L; p<0.0001) than for people 20–39 y (11.7 μmol/L; p<0.0001). Figure 1c demonstrates a significant difference in VIC between non-smoking women and non-smoking men (9.62 μmol/L; p<0.0001) but not between smoking women and smoking men (3.4 μmol/L; p=0.20).
Table 2.
Multiple linear regression results1 for serum vitamin C concentrations in the US population 20 years and older, National Health and Nutrition Examination Survey, 2017–2018
| Variables2 | Variable Categories | Reference Category | Beta coefficient (95% CI) | p-value3 |
|---|---|---|---|---|
| Age (years) | Intercept4 | ≥60 | 50.4 (45.2, 55.7) | <0.0001 |
| 20–39 | −3.1 (−6.6, 0.4) | 0.07 | ||
| 40–59 | −5.3 (−8.3, −2.3) | 0.0019 | ||
| Sex | Men | Women | −5.7 (−8.9, −2.5) | 0.0017 |
| Race/Hispanic Origin | Mexican American | Non-Hispanic White | −0.8 (−3.3, 1.8) | 0.52 |
| Non-Hispanic Asian | −1.6 (−4.6, 1.4) | 0.28 | ||
| Non-Hispanic Black | −0.4 (−4.1, 3.3) | 0.82 | ||
| Poverty Income Ratio | Low (0 – 1.85) | High (>3.5) | −1.4 (−4.2, 1.4) | 0.30 |
| Middle (1.86 – 3.5) | 0.2 (−4.0, 4.4) | 0.91 | ||
| Body Mass Index (kg/m2) | Healthy (18.5 – 24.99) | Obesity (≥30) | 8.3 (4.6, 12.0) | 0.0002 |
| Overweight (25 – 29.99) | 9.3 (6.6, 12.0) | <0.0001 | ||
| Dietary Intake Quartiles (mg/day) | (0 – <20) | ≥110 | −17.5 (−21.2, −13.9) | <0.0001 |
| (20 – <50) | −14.7 (−18.4, −11.0) | <0.0001 | ||
| (50 – <110) | −7.5 (−10.5, −4.5) | 0.0001 | ||
| Vitamin C-containing Supplement Use | Yes | No | 19.2 (16.7, 21.6) | <0.0001 |
| Smoking Status | Non-smokers | Smokers | 8.6 (5.9, 11.3) | <0.0001 |
R2 = 29.4%
Data were adjusted for the following variables: age, sex, race/Hispanic origin, poverty income ratio, body mass index, dietary intake quartiles, vitamin C-containing supplement use, and smoking status.
Student’s t-statistic with 15 degrees of freedom
The regression intercept is the average vitamin C level when all model covariates are set to the reference level.
Figure 1:
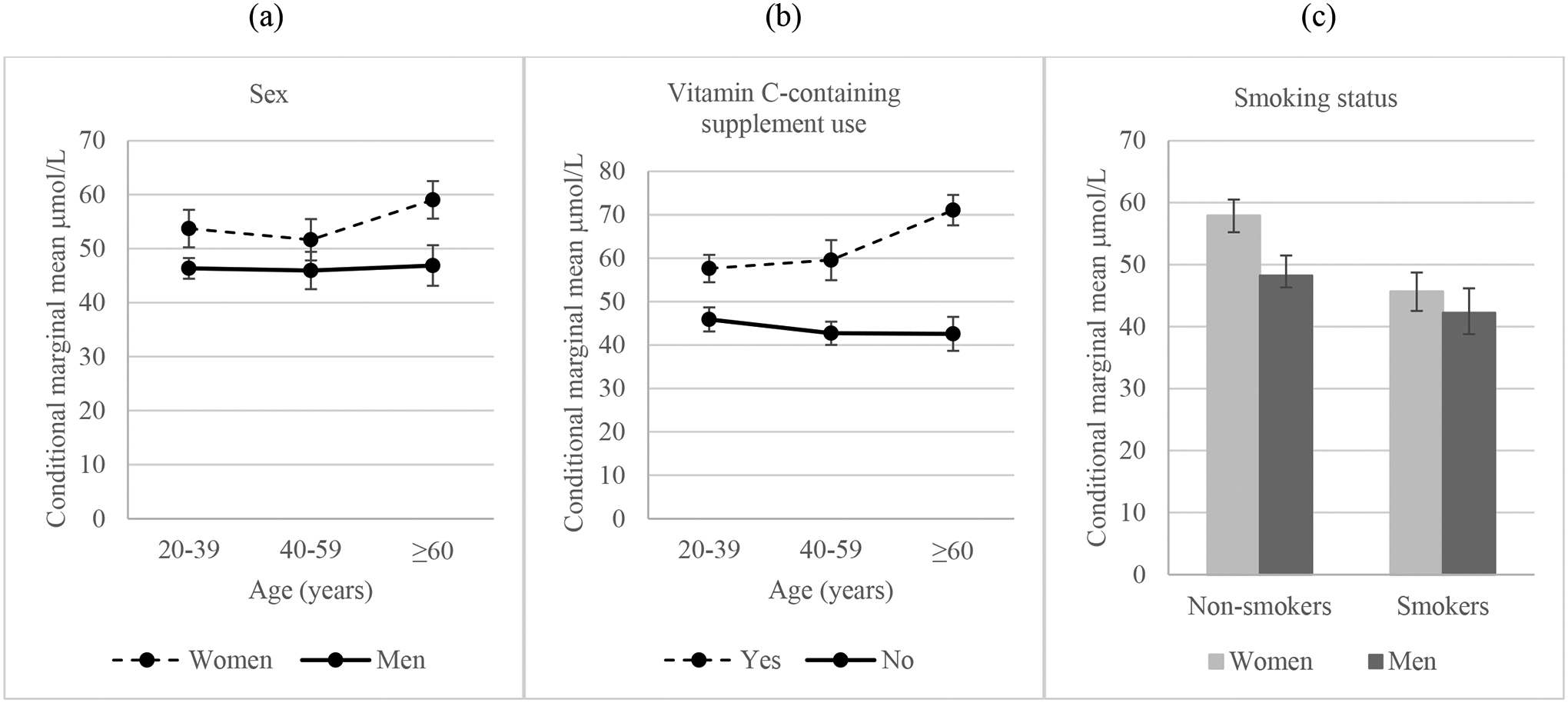
NHANES 2017–2018 conditional marginal means and 95% confidence intervals derived from a multiple linear regression with interactions for age and sex, age and vitamin C-containing supplement use, and smoking status and sex.
Survey Period Comparisons
Comparing both survey periods, the overall prevalence of VIC deficiency was similar in 2017–2018 (Table 1) vs 2003–2006 (Table 3) with a difference of 0.2% [95% CI (-2.0%, 2.5%), p=0.83]. Additionally, after adjusting for all covariates the difference remained not significant (p=0.65) (unpublished observations).
Table 3.
For the US population 20 years and older, weighted prevalence (in percent) of vitamin C deficiency (serum vitamin C <11.4 μmol/L) and weighted mean serum vitamin C concentrations, National Health and Nutrition Examination Survey, 2003–2006. And estimated mean difference between National Health and Nutrition Examination Survey 2017–2018 and 2003–2006.
| Variables | Variable Categories | n1 | 2003–06 Prevalence (95% CI) | 2003–06 Mean (95% CI) | Mean Difference 2017–18 minus 2003–06 (95% CI) | p-value of Mean Differences2 |
|---|---|---|---|---|---|---|
| (%) | (μmol/L) | (μmol/L) | ||||
| Age (years) | Overall ≥20 | 8,892 | 7.0 (5.7, 8.5) | 54.0 (52.4, 55.5) | −2.74 (−5.89, 0.41) | 0.09 |
| 20–39 | 3,233 | 6.9 (5.4, 8.9) | 51.0 (48.8, 53.2) | −2.55 (−6.24, 1.14) | 0.17 | |
| 40–59 | 2,635 | 8.1 (6.3, 10.5) | 51.6 (49.7, 53.4) | −2.19 (−5.66, 1.28) | 0.21 | |
| ≥60 | 3,024 | 5.1 (3.8, 6.8) | 63.0 (61.5, 64.6) | −6.23 (−10.1, −2.35) | 0.0023 | |
| Sex | Men | 4,296 | 8.7 (7.0, 10.7) | 49.4 (47.7, 51.0) | −3.31 (−6.48, −0.13) | 0.0415 |
| Women | 4,596 | 5.4 (4.3, 6.8) | 58.3 (56.5, 60.0) | −2.23 (−5.77, 1.30) | 0.21 | |
| Race/Hispanic Origin | Mexican American | 1,799 | 3.9 (2.6, 5.8) | 51.3 (48.9, 53.8) | −1.61 (−6.53, 3.32) | 0.51 |
| Non-Hispanic Black | 1,840 | 5.7 (4.3, 7.6) | 50.3 (48.3, 52.2) | −2.87 (−6.59, 0.86) | 0.13 | |
| Non-Hispanic White | 4,616 | 8.0 (6.5, 9.8) | 54.9 (52.9, 56.9) | −2.15 (−6.64, 2.34) | 0.15 | |
| Poverty Income Ratio | Low (0 – 1.85) | 3,455 | 9.7 (8.0, 11.6) | 49.2 (47.4, 51.1) | −2.94 (−6.99, 1.11) | 0.15 |
| Middle (1.86 – 3.5) | 2,246 | 7.6 (5.9, 9.8) | 53.6 (51.6, 55.6) | −1.46 (−5.91, 2.99) | 0.51 | |
| High (>3.5) | 2,749 | 4.7 (3.6, 6.1) | 57.6 (55.9, 59.3) | −3.41 (−7.21, 0.39) | 0.08 | |
| Body Mass Index3 (kg/m2) | Healthy (18.5 – 24.99) | 2,552 | 6.2 (4.9, 7.9) | 59.6 (57.6, 61.7) | −3.50 (−8.12, 1.12) | 0.13 |
| Overweight (25 – 29.99) | 3,053 | 5.8 (4.7, 7.3) | 55.4 (53.7, 57.2) | 0.43 (−2.45, 3.32) | 0.76 | |
| Obesity (≥30) | 2,996 | 8.5 (6.6, 10.8) | 47.4 (45.7, 49) | −1.97 (−5.32, 1.39) | 0.24 | |
| Dietary Intake Quartiles (mg/day) | (0 – <20) | 1,775 | 14.2 (11.6, 17.2) | 43.2 (40.7, 45.7) | −2.01 (−6.43, 2.42) | 0.37 |
| (20 – <50) | 2,068 | 9.0 (7.2, 11.1) | 48.2 (46.1, 50.2) | −2.63 (−6.62, 1.35) | 0.19 | |
| (50 – <110) | 2,084 | 4.2 (3.0, 5.8) | 57.2 (55.7, 58.7) | −1.03 (−4.06, 2.00) | 0.50 | |
| ≥110 | 2,551 | 1.7 (1.1, 2.6) | 65.8 (64.1, 67.5) | −2.54 (−6.22, 1.13) | 0.17 | |
| Vitamin C-containing Supplement Use | Yes | 3,603 | 1.7 (1.3, 2.3) | 66.7 (65.4, 68.1) | −0.39 (−3.29, 2.51) | 0.79 |
| No | 5,176 | 11.2 (9.2, 13.6) | 43.8 (41.9, 45.8) | −1.32 (−4.52, 1.88) | 0.41 | |
| Smoking Status | Non-smokers | 6,562 | 3.6 (2.8, 4.6) | 58.8 (57.5, 60.0) | −4.07 (−7.21, −0.93) | 0.0122 |
| Smokers | 2,324 | 15.4 (13.1, 18.0) | 42.1 (40.2, 44.1) | −2.19 (−5.72, 1.34) | 0.22 |
n refers to sample size in NHANES 2003–2006
Student’s t statistic with 45 degrees of freedom
Relative CI width for underweight was greater than 130%. Estimate was suppressed (23).
The overall mean VIC concentrations were not significantly different between the two survey periods (unadjusted difference 2003–2006 minus 2017–2018 was 2.74 μmol/L [95% CI (-0.41, 5.89), p=0.09)] as shown in Table 3. After adjusting for all covariates this difference remained non-significant (p=0.52) (unpublished observations). Nevertheless, there were a few significantly lower VIC concentrations in 2017–2018 compared with 2003–2006, namely 60+y, men, and non-smokers.
Discussion
Overall population prevalence for VIC deficiency has remained unchanged (~7%) from 2003–2006 to 2017–2018, however, some covariates were associated with higher prevalence of deficiency. For instance, low dietary intake was associated with double the prevalence of deficiency compared to the overall population (Table 1). We divided 24-hour dietary intake into quartiles with the lowest quartile between 0 to 20 mg/day. It is known that signs of vitamin C deficiency can appear within 1 month of little or no vitamin C intake (below 10 mg/day). In NHANES 2017–2018, 14% of adults were consuming <10 mg/day (unpublished observations). Smoking, the other lifestyle factor associated with increased risk of low VIC, had 3 times the prevalence of VIC deficiency compared to not smoking.
Mean VIC was essentially unchanged in US adults since last assessed in a nationally representative survey (51.2 vs 54.0 μmol/L; p=0.09). These data are similar to UK National Diet Survey (2008–2012) and the Canadian Health Measures Survey (2012–2013) that produced means of 51.3 and 53 μmol/L, respectively (11, 12). Although the VIC concentration data were similar to the US, the prevalence of deficiencies was lower; US 7%, Canadian 3%, and UK 2%. In both NHANES survey periods, vitamin C-containing supplement users had mean VIC concentrations 30% higher than non-users. In NHANES 2017–2018, multi-vitamins were the most commonly used dietary supplements (6). Multi-vitamins typically contain vitamin C (26) with the most popular vitamin C doses ranging from 60–180 mg. Thirty-seven percent [95% CI (34.3, 40.3)] of adults were taking vitamin C-containing supplements and among them only 0.5% were deficient compared with 9% of those not taking vitamin C-containing supplements, demonstrating risk reduction with supplement intake (Table 1). Serum or plasma vitamin C <5 μmol/L is a concentration consistent with signs and symptoms of scurvy (27–30). There are relatively few scurvy cases in the literature but in NHANES 2017–2018, about 1% of US adults had VIC <5 μmol/L. Consuming five varied servings of fruits and vegetables a day can provide more than 200 mg of vitamin C (2); 8% of adults fell into this intake category with mean VIC of 65.6 μmol/L [95% CI (61.9, 69.3)] which is 28% higher than the overall mean. As noted in some other surveys but not all, low socioeconomic status and high BMI were also associated with lower VIC (7, 11, 31, 32). Carr, et al., showed body weight dependency between daily vitamin C intake and steady state plasma vitamin C. They found that those with higher body weight require additional intake of vitamin C to increase their VIC. This important observation will require confirmation.
The pairwise interactions deepen our understanding about the impact of multiple variables on mean VIC (Figure 1 panels a-c). The interactions between age and sex and age and supplement use were primarily among those ≥60 y. These differences in VIC (men vs women and supplement users vs non-users) were approximately twice the size of the other age groups. Regarding smoking, the mean VIC difference between men and women is only significant in non-smokers.
A major strength of this study is that essentially the same analytical method has been used to compare data over two time periods more than a decade apart. The precision of the laboratory method was excellent with bench QC CVs ranging from 1.7–7.6% (2003–2004), 3.7–5.7% (2005–2006), and 3.6–4.1% (2017–2018). Although we did not participate in external quality assurance programs such as INSTAND (Düsseldorf, Germany) and The Royal College of Pathologists of Australasia (New South Wales, Australia), and a direct method comparison between the old and new method could not be done because the old instrument was no longer available, nevertheless we used two NIST standard reference materials, which showed minimal bias (<1%) in both survey periods. The sample size for the VIC measurements was close to 5000 participants per survey period providing a large sample to assess nationally representative VIC status data. Smoking was assessed using a state-of-the-art tandem mass spectrometry method to measure the biomarker cotinine. A limitation of the survey was that only 44 women scored positive on the pregnancy test during 2017–2018 and therefore were not included in our assessment; thus, our findings do not extend to pregnant women.
Conclusion
VIC status of the US adult population was essentially the same in 2017–2018 since last assessed in 2003–2006. Prevalence of vitamin C deficiency remained high for smokers or those with low vitamin C intake.
Supplementary Material
Impact Statement.
The VIC status of the US adult population was reassessed using NHANES 2017–2018 data. The overall mean and prevalence of deficiency were essentially unchanged compared with NHANES 2003–2006. Smoking status, obesity, low socioeconomic status, low dietary intake, or not using supplements were confirmed to still be associated with low VIC. Additionally, younger people, non-Hispanic Black people and men had low VIC compared to their counterparts.
Abbreviations:
- VIC
serum vitamin C
- NHANES
National Health and Nutrition Examination Survey
- BMI
body mass index
- PIR
poverty income ratio
- MEC
mobile examination center
- df
degrees of freedom
- NCHS
National Center for Health Statistics
Footnotes
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of [the Centers for Disease Control and Prevention/the Agency for Toxic Substances and Disease Registry].
References
- 1.Institute of Medicine. Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. Washington, DC: The National Academies Press; 2000. p. 154. [PubMed] [Google Scholar]
- 2.Levine M, Rumsey SC, Daruwala R, Park JB, Wang Y. Criteria and recommendations for vitamin C intake. J Am Med Assoc 1999;281:1415–23. [DOI] [PubMed] [Google Scholar]
- 3.FDA Daily Value on the New Nutrition and Supplement Facts Labels. https://www.fda.gov/food/new-nutrition-facts-label/daily-value-new-nutrition-and-supplement-facts-labels#:~:text=Daily%20Value%20Increases%20%20%20%20Nutrient%20,%20%20120mcg%20%206%20more%20rows%20 (Accessed April 2022).
- 4.Levine M. New concepts in the biology and biochemistry of ascorbic acid. N Engl J Med 1986;314:892–902. [DOI] [PubMed] [Google Scholar]
- 5.What we eat in America nutrient intake data tables 2003–2004 and 2017–2018. https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/wweia-data-tables/ (Accessed April 2022).
- 6.Mishra S, Stierman B, Gahche JJ, Potischman N. Dietary supplement use among adults: United States, 2017–2018. NCHS data brief, no 399. Hyattsville, MD: National Center for Health Statistics. 2021. [PubMed] [Google Scholar]
- 7.Schleicher RL, Carroll MD, Ford ES, Lacher DA. Serum vitamin C and the prevalence of vitamin C deficiency in the United States: 2003–2004 National Health and Nutrition Examination Survey (NHANES). Am J Clin Nutr 2009;90:1252–63. [DOI] [PubMed] [Google Scholar]
- 8.Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017–2018. NCHS data brief, no 360. Hyattsville, MD: National Center for Health Statistics. 2020. [PubMed] [Google Scholar]
- 9.Angeles-Agdeppa I, Sun Y, Denney L, Tanda KV, Octavio RD, Carriquiry A, Capanzana MV. Food sources, energy and nutrient intakes of adults: 2013 Philippines National Nutrition Survey. Nutr J 2019;18:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim J, Choi Y-H. Physical activity, dietary vitamin C, and metabolic syndrome in the Korean adults: the Korea National Health and Nutrition Examination Survey 2008 to 2012. Public Health. 2016;135:30–7. [DOI] [PubMed] [Google Scholar]
- 11.National diet and nutrition survey Results from years 1, 2, 3, and 4 (combined) of the rolling programme (2008/2009 – 2011–2012). https://www.gov.uk/government/statistics/national-diet-and-nutrition-survey-results-from-years-1-to-4-combined-of-the-rolling-programme-for-2008-and-2009-to-2011-and-2012 (Accessed April 2022).
- 12.Langlois K, Cooper M, Colapinto CK. Vitamin C status of Canadian adults: Findings from the 2012/2013 Canadian Health Measures Survey. Statistics Canada Health Reports 2016; 27:3–10. [PubMed] [Google Scholar]
- 13.Curtin LR, Mohadjer LK, Dohrmann SM, Montaquila JM, Kruszon-Moran D, Mirel LB, et al. The National Health and Nutrition Examination Survey: Sample Design, 1999–2006. Vital Health Stat 2. 2012;155:1–39. [PubMed] [Google Scholar]
- 14.Curtin LR, Mohadjer LK, Dohrmann SM, Kruszon-Moran D, Mirel LB, Carroll MD, et al. National Health and Nutrition Examination Survey: Sample Design, 2007–2010. Vital Health Stat 2. 2013;160:1–23. [PubMed] [Google Scholar]
- 15.Johnson CL, Dohrmann SM, Burt VL, Mohadjer LK. National Health and Nutrition Examination Survey: Sample Design, 2011–2014. Vital Health Stat 2. 2014;162:1–33. [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention, National Center for Health Statistics. Response rates & CPS population totals, National Health and Nutrition Examination Survey. https://wwwn.cdc.gov/nchs/nhanes/ResponseRates.aspx (Accessed April 2022).
- 17.Centers for Disease Control and Prevention, National Center for Health Statistics. National health and nutrition examination survey: analytic guidelines, 2011–2014 and 2015–2016. https://wwwn.cdc.gov/nchs/data/nhanes/analyticguidelines/11-16-analytic-guidelines.pdf (Accessed June 2022)
- 18.US Centers for Disease Control and Prevention. Second National Report on Biochemical Indicators of Diet and Nutrition in the US Population 2012. Atlanta (GA): National Center for Environmental Health; 2012. p.72–84. [Google Scholar]
- 19.McCoy LF, Bowen MB, Xu M, Chen H, Schleicher RL. Improved HPLC assay for measuring serum vitamin C with 1-methyluric acid used as an electrochemically active internal standard. Clin Chem 2005;51:1062–4. [DOI] [PubMed] [Google Scholar]
- 20.Caudill SP, Schleicher RL, Pirkle JL. Multi-rule quality control for the age-related eye disease study. Stat Med 2008;27:4094–106. [DOI] [PubMed] [Google Scholar]
- 21.National Health and Nutrition Examination Survey 2003–2004 Vitamin C. https://wwwn.cdc.gov/nchs/data/nhanes/2003-2004/labmethods/l06_c_met_vitamin-c.pdf (Accessed July 2022)
- 22.National Health and Nutrition Examination Survey 2005–2006 Vitamin C. https://wwwn.cdc.gov/nchs/data/nhanes/2005-2006/labmethods/vic_d_met.pdf (Accessed July 2022)
- 23.National Health and Nutrition Examination Survey 2017–2018 Vitamin C: https://wwwn.cdc.gov/nchs/data/nhanes/2017-2018/labmethods/VIC-J-MET-508.pdf (Accessed July 2022)
- 24.Parker JD, Talih M, Malec DJ, Beresovsky V, Carroll M, Gonzalez JF, Hamilton BE, et al. National Center for Health Statistics data presentation standards for proportions. National Center for Health Statistics. Vital Health Stat 2017;2:175. [PubMed] [Google Scholar]
- 25.Sternberg MR, Schleicher RL, Pfeiffer CM. Regression modeling plan for 29 biochemical indicators of diet and nutrition measured in NHANES 2003–2006. J Nutr 2013;143(6):948S–56S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vitamin C fact sheet for health professionals. https://ods.od.nih.gov/factsheets/VitaminC-HealthProfessional/ (Accessed April 2022)
- 27.Angeli AM, Megna B, Mazepa M, Ivy ZK, Sultan S, Sloan JA. Transfusion-dependent anemia secondary to vitamin C deficiency. Am J Hematol 2022;97:E166–E188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berry CT, Berry KG, Abbott J, Jiang AJ, Ronner L, Mollanazar NK, et al. Resolution of acquired palmoplantar keratoderma and scurvy after treatment of multivitamin deficiencies. JAAD Case Rep 2022;22:27–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nastro A, Rosenwasser N, Daniels SP, Magnani J, Endo Y, Hampton E, et al. Scurvy due to selective diet in a seemingly healthy 4-year-old boy. Pediatrics 2019;144:e20182824. [DOI] [PubMed] [Google Scholar]
- 30.Eissen F, Jacocks C, Matthew C. Sailing the ship of life: scurvy and autoimmunity. Ther Adv Chronic Dis 2022;13:1–3.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Crook J, Horgas A, Yoon S-J, Grundmann O, Johnson-Mallard V. Insufficient vitamin C levels among adults in the United States: Results from the NHANES surveys, 2003–2006. Nutrients 2021;13:3910–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carr AC, Block G, Lykkesfeldt J. Estimation of vitamin C intake requirements based on body weight: implications for obesity. Nutrients 2022;14:1460–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


