Abstract
Objectives
Prayer is a devotional practice used across religious traditions to commune with the sacred and has been used as a coping strategy for pain. Previous research on prayer as a pain coping strategy has had mixed results, with prayer associated with both greater and lesser pain depending on prayer type. To date, there has been only 1 measure of pain-related prayer, the prayer subscale of the Coping Strategies Questionnaire–Revised, which measures solely passive prayer, neglecting other types of prayer (eg, active and neutral). To better understand the relationship between pain and prayer, a comprehensive measure of prayer for pain is needed. The aim of this study was to develop and validate the Pain-related PRAYER Scale (PPRAYERS), a questionnaire exploring active, passive, and neutral petitionary prayers to God or a higher power in response to pain.
Methods
Adults with chronic pain (n = 411) completed demographic, health, and pain-related questionnaires, including PPRAYERS.
Results
Results of an exploratory factor analysis yielded a 3-factor structure consistent with active, passive, and neutral subscales. A confirmatory factor analysis resulted in adequate fit after the removal of 5 items. PPRAYERS showed good internal consistency and convergent and discriminant validity.
Discussion
These results provide preliminary validation for PPRAYERS, a novel measure for pain-related prayer.
Keywords: pain, prayer, chronic pain, coping, religion
Introduction
Chronic pain, defined as pain that persists for longer than 3 months, affects between 11% and 40% of Americans and is associated with costs of $635 billion annually.1–3 Pain has been associated with widespread morbidity, increased depression, and poorer quality of life.3 Given the widespread nature of pain, there are considerable individual differences in the pain experience. Pain coping style has been shown to account for some of these differences.4–7
Prayer is an ancient practice to honor a higher power and seek benevolence toward the one doing the praying (eg, for health, harvest, longevity, prosperity, mercy). Prayer practices have been described in a variety of ways, with diverging terminology (eg, supplication, petitionary, intercessory, thanksgiving, contemplative, adoration, confession, etc.) used by both religious and nonreligious people.8 These can be practiced solo (ie, personal prayer) or in a group (ie, community based). For the purposes of the present study, prayer is defined as “an act of [personal] communication by humans with the sacred or holy—God, the gods, the transcendent realm, or supernatural powers.”9
Prayer has been proposed as a potentially useful adjunct therapy in the treatment of pain, yet the relationship between pain and personal prayer remains unclear.10 Although some studies indicate that prayer is associated with greater anxiety and depression, greater pain and disability, and poorer pain tolerance,11–14 others have found that prayer is associated with greater pain tolerance and less pain.7,15 Perhaps the substantive variability in the type, target, and content of the prayer, as well as the characteristics of the participants taking part in these studies, can account for the discrepant outcomes in these studies.10 Consistent with Ferreira-Valente’s taxonomy, prayer can be classified into private or communal (by number of devotees), active or passive (by content type), and participatory or distant intercessory praying.16 These characteristics are crucial in understanding the relationship between prayer and pain.10 For example, prayer to a religious entity or higher power (ie, “God”) is associated with lower pain intensity and unpleasantness than is secular prayer (ie, prayer directed not to a higher entity, but to an archetypal non-persona).11,17 Furthermore, a recent meta-analysis demonstrated that private prayer is associated with lower pain intensity and greater pain tolerance.18 Notably, distant intercessory prayer and group-based prayer studies have fallen into disfavor because of methodological challenges that undermine the ability to draw conclusions from the data.19
The content of petitionary prayer (ie, what the person in pain is requesting) can be categorized as active or passive prayer. This categorization is based on the broader differentiation between active and passive coping styles.20 Active coping refers to strategies to control pain or function, in spite of pain, whereas passive coping involves relinquishing control of pain to others.21 Active prayer involves petitioning God or a higher power to help the patient manage pain or function in spite of pain (eg, “God, help me endure the pain”) and is associated with greater pain tolerance than that associated with passive prayer, which involves petitioning God or a higher power to relieve the patient of pain (eg, “God, take the pain away”).22 In the latter context, the patient might display a distinct “self-motivating” outlook set apart from the more “deferring” attitude of passive prayer content.11
In addition to the active and passive prayer content, there are people whose notion of a higher power or a healing influence in the universe is nonreligious. The latter group might include meditators, agnostics, atheists, naturalists, and those who are spiritual but not religious. Hence, the “neutral” category in the present project reflects a generic “wish” that is not based on a given religious dogma or belief and that could be accessible or practiced outside religious circles. Neutral prayer, therefore, will not be specifically directed to a deity or supernatural being but rather to a more generic universal healing influence. The meaning of this healing influence will be particular to each person.
Currently, the Praying subscale of the Coping Strategies Questionnaire–Revised (CSQ-R23) is the only validated measure of prayer in response to pain, and it assesses only passive prayer. Because prayer in all its expressions can have a different, complex association with pain,10,18 it is necessary to develop a more comprehensive measure of prayer for pain to better understand the relationship between prayer and pain. Specifically, this measure should include an active style of prayer, as well as neutral prayer, which will capture those who might not pray to God, might be agnostic, or might meditate, using spiritual as opposed to religious prayer to cope with their pain.
In the present study, we developed and validated the Pain-related PRAYER Scale (PPRAYERS), a comprehensive measure of active, passive, and neutral prayer for coping with pain. This measure includes petitionary prayer wishful statements that are applicable to both religious and nonreligious patients.
Methods
Measure development
Two authors (S.M.M. and M.I.), one religious and one nonreligious, developed a comprehensive list of verbal, nonsectarian, nondenominational, active, passive, and neutral petitionary prayer statements to God or a higher power that individuals might use in response to pain. These items were based on available empirical data evaluating pain outcomes in randomized control studies,10,17,20,22 as well as on validated questionnaires that assess prayer and religiosity both within and outside the context of pain and pain coping.23,24,25 Using a nondenominational approach, we chose prayer petitions that could be applicable to people of all religions, faiths, and beliefs, including those who meditate, are agnostic, or pray using neutral prayer petitions to a higher power. We limited the number of items per proposed prayer category to 8 in order to minimize participant burden while maximizing content.
We then consulted a 7-member expert advisory panel with varied expertise, consisting of pain researchers, theology scholars, clinical psychologists, and measurement development experts, who individually provided qualitative reviews and commentary on the items. The reviews and commentary were then synthesized by the authors. At least one panel participant had a personal history of chronic pain. Panel members provided individual feedback and were blinded to other panel members’ feedback.
All active statements were developed de novo, except one that was incorporated from a published study (“God, help me endure the pain”).22 Passive statements included the 3 items from the CSQ-R praying subscale, 1 item from the Meints (2018) study (“God, take the pain away”), and 4 de novo items.22,26 There were 7 newly developed neutral statements in which the acting agency was neither God nor the self (eg, nature, the body, the universe). On the basis of feedback from the expert panel, 1 item was deleted, 2 items were added, and 12 items were reworded from the initial list.
The result of these efforts is the present measure, the Pain-related PRAYER Scale (PPRAYERS). It is a 22-item self-report questionnaire that asks participants to rate the frequency of their use of various prayer statements on a scale ranging from 0 (never) to 7 (always) (see Supplementary Material). The chosen latent variables were active, passive, and neutral prayer reflecting the petitionary content of personal prayers used by the patient “in situ” and were not intended for groups or distant intercessory styles.
Participants
Participants were eligible if they were English speakers, 18 years of age or older, reported chronic pain of at least 3 months’ duration with an average severity of 3 or greater on a 0- to 10-point numeric rating scale,27 and endorsed the use of prayer or meditation related to their pain. Participants were recruited through the use of a variety of strategies, including Web-based advertisements; unpaid social media advertisements (eg, Facebook, Twitter, Instagram); diocesan resources from the Episcopal Church of Delaware (eg, the Episcopal News Service, parish newsletters); community outreach to health care, interfaith, and chaplaincy groups across the United States; electronic medical record–based research databases at Brigham and Women’s Hospital; and Amazon’s Mechanical Turk.
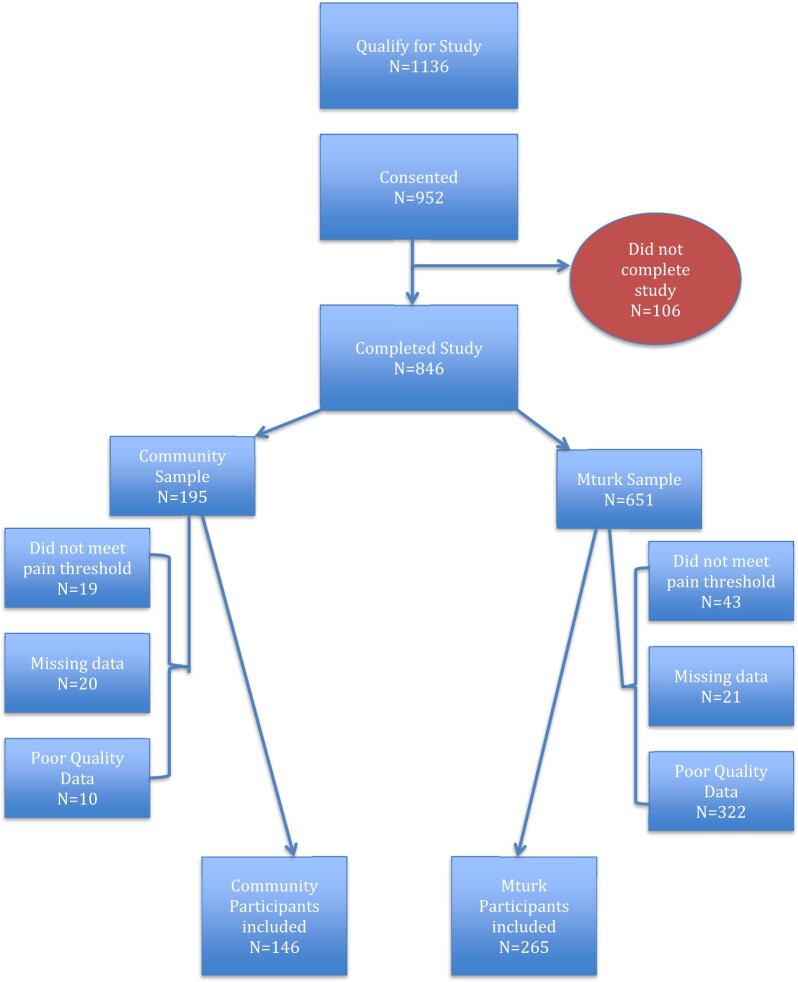
Participants who expressed interest in participating in the study were provided a link to an online screening questionnaire via the Research Electronic Data Capture (REDCap) data collection system.28 Those eligible were then redirected to an additional REDCap survey in which they were asked to review and provide informed consent before completion of the online questionnaires described in “Measures.” Participants who expressed a preference to complete the study on paper were screened via telephone before being sent a hard copy of the informed consent and questionnaire battery. They then returned these in a pre-stamped envelope without any other personally identifying information. All study procedures could be completed within 30 minutes. Of note, we included attention checks to detect inattentive respondents and improve data quality, which is especially important when data are collected with Mechanical Turk.29 All procedures were approved by the Brigham and Women’s Hospital Institutional Review Board (IRB# 2020P002278). Of the 1591 individuals who completed the eligibility screener, 1136 initially qualified to participate, 952 provided informed consent, and 846 completed the study (see Figure 1 for the participant flow chart). Of the 846 study completers, 62 did not meet the inclusion criteria for pain threshold (ie, pain ≥3 for ≥3 months), 41 had missing data on the PPRAYERS questionnaire, and 332 did not pass attention checks. After exclusion of those individuals, our final sample included 411 participants.
Figure 1.
Participant flow chart from screening through study completion.
Measures
Patient-Reported Outcomes Measurement Information System–29
The Patient-Reported Outcomes Measurement Information System–29 (PROMIS 29) is a 29-item self-report measure of health.30 The scale consists of 7 domains (ie, physical function, fatigue, pain interference, depressive symptoms, anxiety, ability to participate in social roles and activities, and sleep disturbance), each of which is assessed with 4 items on a Likert scale. A single item is also used to assess pain intensity, ranging from 0 to 10. In the present study, we used the pain interference, depression, anxiety, and pain intensity subscales. These subscales demonstrated good reliability in the present sample (pain interference: α = 0.86; depression: α = 0.90; anxiety: α = 0.86). The measure has good reliability and has been shown to be valid for use in populations with chronic pain.31–33
Pain Catastrophizing Scale
The Pain Catastrophizing Scale (PCS) is a 13-item self-report measure of pain catastrophizing, a set of cognitive and emotional responses to pain characterized by magnification, rumination, and helplessness.34 Participants were asked to reflect on their past pain experiences and rate the degree to which they experience specific thoughts and feelings on a scale from 0 (not at all) to 4 (all the time). Scores are summed and can range from 0 to 52, with higher scores indicative of greater catastrophizing. The measure demonstrated good reliability in the present sample (α = 0.93).
Duke University Religion Index
The Duke University Religion Index (DUREL) is a 5-item self-report measure of religiosity and religious involvement that has been used widely in health care research.24 The subscales of the DUREL include nonorganizational religious activity (NORA; ie, religious activities performed in private such as prayer), organizational religious activity (ORA; ie, attending religious services), and intrinsic religiosity (IR; ie, personal religious commitment or motivation). Participants rated the frequency of their involvement in religious activities from 1 (never) to 6 (more than once per week) and rated the accuracy of several religious statements from 1 (definitely not true) to 5 (definitely true of me). Total scores for this measure are summed and can range from 5 to 27, with higher scores indicative of greater religiosity and religious involvement.
Coping Strategies Questionnaire–Revised
The CSQ-R is a 27-item self-report questionnaire that examines the frequency with which individuals engage in pain-related coping strategies.23 Participants rate their use of each of 6 coping strategies (ie, catastrophizing, coping self-statements, ignoring sensations, reinterpreting pain sensations, diverting attention, and praying/hoping) on a 7-point Likert scale from 0 (never do that) to 6 (always do that). For the present study, we were particularly interested in the praying subscale, which includes items such as “I pray to God it won’t last long” and “I pray for the pain to stop.” This subscale has previously been shown to assess a passive style of prayer.35,36 The subscale demonstrated adequate reliability in the present sample (α = 0.68).
Data analysis
Assumptions of normality were assessed before the analyses were conducted. The total sample (n = 411) was split into 2 equal samples for the exploratory factor analysis (n = 205) and confirmatory factor analysis (n = 206).
Exploratory factor analysis
A maximum likelihood factor analysis with an oblimin rotation was used to examine the underlying structure of the PPRAYERS. Factors with eigenvalues greater than 1 were retained. Factor loadings and cross-loadings were used to evaluate individual items. Recommendations for factor loading thresholds vary in the literature, with loadings greater than 0.3 or 0.4 commonly accepted.37–39 We reported loadings greater than 0.3 for evaluation. Statistical results were reviewed by the study team for theoretical soundness. All statistical analyses for the exploratory factor analysis were conducted in IBM SPSS Statistics for Windows, Version 28.0 (IBM Corp., Armonk, NY, 2021).
Confirmatory factor analysis
In the second sample, the factor structure determined by the exploratory factor analysis was evaluated in a confirmatory factor analysis through the use of structural equation modeling. Goodness-of-fit indices used to evaluate model fit included the chi-squared test, chi-squared / degrees of freedom ratio, root mean squared error of approximation, Tucker Lewis index, comparative fit index, and standardized root mean square residual. Given that chi-squared is influenced by sample size, the chi-squared / degrees of freedom ratio was included to provide further assessment of fit. The chi-squared / degrees of freedom ratio assesses the minimum sample discrepancy divided by the degrees of freedom,40 with values less than 3 considered adequate and values less than 2 indicating excellent fit.41 After the initial model, suggested modification indices were reviewed for theoretical and statistical soundness. An adjusted model was run and compared with the original model with the chi-squared difference statistic.41 MPLUS (V6, Muthen & Muthen) was used for all structural equation modeling analyses.
Reliability and validity
Internal consistency of the final PPRAYERS subscales was evaluated with coefficient alpha.42 Convergent validity and discriminant validity were evaluated by examination of the cross-sectional associations between the PPRAYERS subscales (active, passive, and neutral) and existing relevant measures (DUREL and CSQ-R praying subscale).
Results
The overall sample had an average age of 43 years (SD = 15.88); was 50.1% female; and was predominantly non-Hispanic Caucasian (73.4%), married (65.0%), and of Christian faith (79.8%). Sample descriptives for the full sample and the divided samples are included in Table 1. On average, the sample reported a PROMIS-29 pain intensity rating of 6.24 (SD = 1.65) over the prior 7 days. According to recommended PROMIS 29 cut points,43 on average, the sample reported a moderate level of pain interference (mean = 62.84, SD = 5.34) and endorsed moderate levels of depression (mean = 57.94, SD = 8.99) and anxiety (mean = 61.22, SD = 8.19) symptoms.
Table 1.
Sample demographics.
| Full sample (n = 411) | Exploratory factor analysis (n = 205) | Confirmatory factor analysis (n = 206) | |
|---|---|---|---|
| Age, years, mean ± SD | 43.8 ± 25.9 | 43.7 ± 15.8 | 43.9 ± 16.0 |
| Sex, n (%) | |||
| Female | 206 (50.1) | 102 (49.8) | 104 (50.5) |
| Male | 204 (49.6) | 103 (50.2) | 101 (49.0) |
| Prefer not to answer / missing | 1 (0.2) | 0 (0.0) | 1 (0.5) |
| Gender, n (%) | |||
| Female | 202 (49.1) | 99 (48.3) | 103 (50.0) |
| Male | 205 (49.9) | 104 (50.7) | 101 (49.0) |
| Other | 1 (0.2) | 1 (0.5) | 0 (0.0) |
| Prefer not to answer / missing | 3 (0.7) | 1 (0.5) | 2 (1.0) |
| Race, n (%) | |||
| African American or Black | 35 (8.5) | 17 (8.3) | 18 (8.7) |
| Caucasian | 258 (62.8) | 133 (64.9) | 125 (60.7) |
| Asian | 80 (19.5) | 42 (20.5) | 38 (18.4) |
| American Indian / Alaskan Native | 15 (3.6) | 7 (3.4) | 8 (3.9) |
| Native Hawaiian or other Pacific Islander | 1 (0.2) | 0 (0.0) | 1 (0.5) |
| Other | 16 (3.9) | 5 (2.4) | 11 (5.3) |
| Prefer not to answer / missing | 6 (1.5) | 1 (0.5) | 5 (2.4) |
| Ethnicity, n (%) | |||
| Hispanic or Latino | 83 (20.2) | 42 (20.5) | 41 (19.9) |
| Not Hispanic or Latino | 303 (73.7) | 156 (76.1) | 147 (71.4) |
| Prefer not to answer / missing | 25 (6.1) | 7 (3.4) | 18 (8.8) |
| Marital status, n (%) | |||
| Never married | 74 (18.0) | 29 (14.1) | 45 (21.8) |
| Living with a partner | 19 (4.6) | 12 (5.9) | 7 (3.4) |
| Married | 267 (65.0) | 135 (65.9) | 132 (64.1) |
| Divorced/separated | 28 (6.8) | 21 (10.2) | 7 (3.4) |
| Widowed | 12 (2.9) | 6 (2.9) | 6 (2.9) |
| Prefer not to answer / missing | 11 (2.7) | 2 (1.0) | 9 (4.3) |
| Education, n (%) | |||
| Some high school | 1 (0.2) | 1 (0.5) | 0 (0.0) |
| High school graduate / GED | 21 (5.1) | 8 (3.9) | 13 (6.3) |
| Technical school gradudate | 8 (1.9) | 3 (1.5) | 5 (2.4) |
| Some college | 45 (10.9) | 27 (13.2) | 18 (8.7) |
| College graduate | 197 (47.9) | 97 (47.3) | 100 (48.5) |
| Graduate school graduate | 136 (33.1) | 68 (33.1) | 68 (33.0) |
| Prefer not to answer / missing | 3 (0.7) | 1 (0.5) | 2 (1.0) |
| Employment, n (%) | |||
| Yes | 300 (73.0) | 155 (75.6) | 145 (70.4) |
| No | 103 (25.1) | 50 (24.4) | 53 (25.7) |
| Prefer not to answer / missing | 8 (1.9) | 0 (0.0) | 8 (3.9) |
| Household income, n (%) | |||
| Less than $22 500 | 61 (14.8) | 26 (12.7) | 35 (17.0) |
| $22 501 to $45 000 | 120 (29.2) | 59 (28.8) | 61 (29.6) |
| $45 001 to $100 000 | 160 (38.9) | 89 (43.4) | 71 (34.5) |
| More than $100 000 | 52 (12.7) | 24 (11.7) | 28 (13.6) |
| Prefer not to answer / missing | 18 (4.4) | 7 (3.4) | 11 (5.4) |
| Religious affiliation, n (%) | |||
| Buddhist | 3 (0.7) | 0 (0.0) | 3 (1.5) |
| Christian | 328 (79,8) | 165 (80.5) | 163 (79.1) |
| Jewish | 4 (1.0) | 2 (1.0) | 2 (1.0) |
| Hindu | 44 (10.7) | 22 (10.7) | 22 (10.7) |
| Muslim | 11 (2.7) | 5 (2.4) | 6 (2.9) |
| Other faith religions | 12 (2.9) | 3 (1.5) | 9 (4.4) |
| Unaffiliated | 8 (1.9) | 7 (3.4) | 1 (0.5) |
| Prefer not to answer / missing | 1 (0.2) | 1 (0.5) | 0 (0.0) |
Exploratory factor analysis
A maximum likelihood factor analysis with oblimin rotation yielded 3 factors with eigenvalues greater than 1 that explained 63.66% of the total variance. Factor loadings from the pattern matrix are presented in Table 2. The first component, labeled neutral prayer, accounted for 40% of the total variance. The second component, labeled passive prayer, accounted for 13% of the total variance. The third component, labeled active prayer, accounted for 10% of the total variance. The 3 components were significantly correlated (r for all= 0.30 to 0.40). With the exception of items 1, 5, 16, and 17, all items demonstrated a primary loading on 1 factor (primary loading >0.50; difference between primary and secondary loadings >0.20). Item 16 was excluded because its primary loading did not reach the 0.50 cutoff. Items 1 and 5 were excluded because they had primary loadings on 2 factors. Although item 17 also had primary loadings on 2 factors, this item was retained for confirmatory factor analysis because of its theoretical association with other neutral prayer items.
Table 2.
PPRAYERS rotated factor loadings (pattern matrix).
| Item Number | Item | Neutral | Passive | Active |
|---|---|---|---|---|
| 2 | Help me so that I can endure this pain. | 0.74 | ||
| 3 | Help me to manage this pain. | 0.71 | ||
| 4 | Help my body to deal with this pain. | 0.61 | ||
| 6 | Show me how to handle my pain. | 0.74 | ||
| 7 | Help me to rise above this pain. | 0.53 | ||
| 8 | I pray for your support to help me function while in pain. | 0.79 | ||
| 16 | Take care of me. | 0.30 | 0.43 | |
| 1 | Help me so that I can overcome this pain. | 0.41 | 0.43 | |
| 9 | Take my pain away. | 0.84 | ||
| 10 | Cure my pain. | 0.92 | ||
| 11 | Dissolve this pain. | 0.58 | ||
| 13 | Lift up this painful condition from me. | 0.61 | ||
| 15 | I pray for God to make the pain stop. | 0.79 | ||
| 14 | I pray that God won’t make the pain last long. | 0.31 | 0.56 | |
| 12 | Help me understand why you sent me this pain. | 0.54 | ||
| 18 | I surrender my pain to the balancing influence of the universe. | 0.88 | ||
| 19 | May my body align with the universe’s healing power. | 0.86 | ||
| 20 | The greater whole will heal my pain. | 0.89 | ||
| 21 | Nature’s cycles will drive my pain away. | 0.91 | ||
| 22 | My body will be renewed. | 0.66 | ||
| 5 | Help me to direct my body to fight this pain. | 0.38 | 0.36 | |
| 17 | Pain is just a part of life. | 0.43 | 0.35 |
Note: Primary factor loadings shown in bold. Grayed-out items were eliminated at the exploratory factor analysis stage.
Confirmatory factor analysis
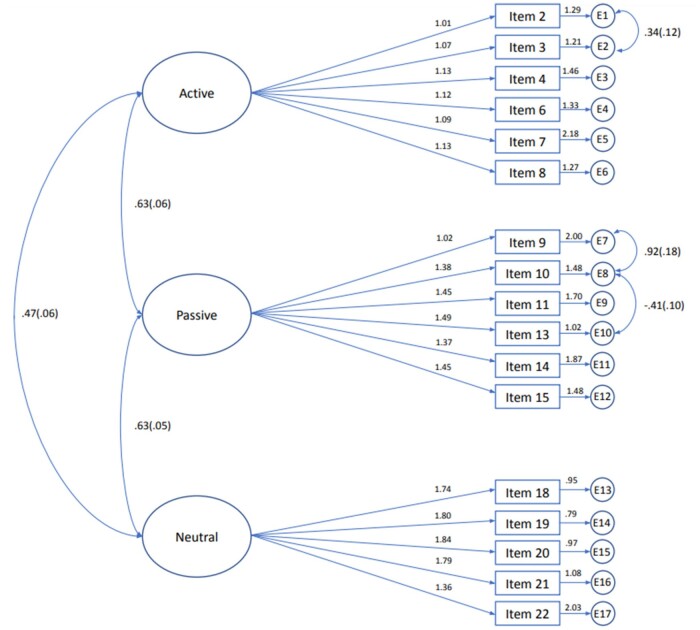
In the second sample, the 3-factor model demonstrated suboptimal fit based on model fit indices (Table 3). After review of the modification indices and further theoretical evaluation of the items, items 12 and 17 were removed from the model to improve model fit. Additionally, error variances between items within the same scale were allowed to correlate (item 2 with 3, 9 with 10, and 10 with 13). The revised model demonstrated better fit to the data (x2(36) = 189.62, P < .01) and improvement in several goodness-of-fit indices (chi-squared / degrees of freedom = 2.36, root mean squared error of approximation = 0.08, Tucker Lewis index = 0.91, and standardized root mean square residual = 0.06, Table 3, Figure 2). Comparative fit index remained at 0.92, just below the currently recommended threshold of 0.95.
Table 3.
Confirmatory factor analysis model fit indices.
| Ideal value | Model | Revised model | |
|---|---|---|---|
| Chi-squared | |||
| χ2 | Depends on n | 456.54 | 266.92 |
| P | >.05 | 0.00 | 0.00 |
| df | 149.00 | 113.00 | |
| Chi-squared / df ratio | ≤3 = good, <2 = superior | 3.06 | 2.36 |
| RMSEA | <0.05 = close fit, 0.05 to 0.08 = fair fit, >0.10 = poor fit | 0.10 | 0.08 |
| TLI | >0.90 | 0.84 | 0.91 |
| CFI | ≥0.95 | 0.86 | 0.92 |
| SRMR | ≤0.08 | 0.09 | 0.06 |
| Reliability | ≥0.90 | ||
| Active | 0.83 | 0.83 | |
| Passive | 0.88 | 0.92 | |
| Neutral | 0.92 | 0.93 |
Abbreviations: df= degrees of freedom; RMSEA= root mean squared error of approximation; TLI= Tucker Lewis index; CFI= comparative fit index; SRMR= standardized root mean square residual.
Figure 2.
Path diagram for the final PPRAYERS measure, including active, passive, and neutral prayer as latent variables, item loadings, and error variances.
Reliability and validity
All PPRAYERS subscales demonstrated good internal consistency (active, α = 0.83; passive, α = 0.92; neutral, α = 0.93). Bivariate correlations between the active, passive, and neutral prayer subscales and existing relevant measures of prayer and religiosity are detailed in Table 4.
Table 4.
Correlations between PPRAYERS scales, CSQ-R prayer subscale, and DUREL subscales.
| PPRAYERS |
|||
|---|---|---|---|
| Active scale | Passive scale | Neutral scale | |
| CSQ-R prayer subscale | 0.45** | 0.54** | 0.28** |
| DUREL ORA subscale | 0.21** | 0.02 | –0.06 |
| DUREL NORA subscale | 0.19** | –0.07 | –0.05 |
| DUREL IR subscale | 0.26** | 0.04 | 0.06 |
P < .01.
Abbreviations: CSQ-R= Coping Strategies Questionnaire–Revised; DUREL= Duke University Religion Index; IR= intrinsic religiosity; NORA= nonorganizational religious activities; ORA= organizational religious activities; PPRAYERS= Pain and Prayer Scale.
Active prayer demonstrated a positive relationship with the CSQ-R prayer subscale and with the subscales of the DUREL, including ORA, NORA, and IR. Passive prayer demonstrated a significant positive relationship with only the CSQ-R prayer subscale. Similar to passive prayer, neutral prayer demonstrated a significant positive relationship with only the CSQ-R prayer subscale. A Fisher r-to-z transformation was used to assess for significant differences in the correlations between PPRAYERS subscales and existing measures of prayer and religiosity. The passive prayer subscale had a significantly stronger relationship with the CSQ-R prayer subscale than did the neutral prayer subscale (z = 4.32, P < .001). The active prayer subscale also had a significantly stronger relationship with the CSQ-R prayer subscale than did the neutral prayer subscale (z = 2.63, P < .01). Additionally, the active prayer subscale had a significantly stronger relationship with the subscales of the DUREL than did either the passive prayer subscale (ORA: z = 2.82, P < .01; NORA: z = 3.85, P < .001; IR: z = 3.30, P < .001) or the neutral prayer subscale (ORA: z = 2.06, P < .05; NORA: z = 3.20, P < .001; IR: z = 2.71, P < .01) (Table 4).
Discussion
Findings from the present study provide evidence of validity for PPRAYERS, a self-report measure of petitionary prayer to cope with pain. Expanding on the work of the CSQ-R,23 which includes only passive prayer, our results indicate the fit of a 3-factor structure consisting of active, passive, and neutral prayer. PPRAYERS showed good internal consistency, and patterns of correlations with other measures indicate good convergent and divergent validity. Our exploratory factor analysis resulted in a 3-factor model, consistent with our theory, including 3 prayer subscales: active, passive, and neutral prayer. As a result of our analysis combined with theoretical rationale, 5 items were removed from the original 22 items, resulting in a 17-item scale. Results of our confirmatory factor analysis demonstrated adequate fit for this final scale consistent with the 3-factor model. Together, the heterogeneity of correlations between PPRAYERS and extant measures of religious coping suggests that PPRAYERS explores nuanced and novel aspects of prayer as it relates to the experience of pain and is not simply replicating measures already in existence.
Active prayer, which is praying for the means to endure or overcome pain, was associated with higher scores on the CSQ-R prayer subscale as well as on the ORA, NORA, and IR subscales of the DUREL. On the other hand, the passive and neutral prayer subscales correlated with only the CSQ-R prayer subscale. It is likely that the active prayer subscale is correlated with the DUREL subscales because the DUREL subscales assess participants’ engagement in religious activities, which are inherently active processes. Because the CSQ-R prayer subscale measures passive styles of prayer, we did not expect the PPRAYERS active prayer subscale to correlate with it. However, it is likely that those who pray use a variety of prayer types. Thus, participants who engage in active prayer can also engage in passive prayer. We did find, however, that the PPRAYERS passive prayer subscale showed a correlation with the CSQ-R prayer subscale that was significantly larger than the relationships between the active and neutral prayer subscales and the CSQ-R prayer subscale. This provides evidence that we are indeed measuring passive prayer with this PPRAYERS subscale, as the CSQ-R has been shown to measure only passive prayer.36
In addition to assessing active and passive prayer to God or a higher power, PPRAYERS assesses neutral prayer, which is not directed to a specific entity and can be nonreligious. Because religion and spirituality are increasingly being considered an important aspect of people’s overall wellness,44–47 it was important that we assess the prayer of individuals who might not pray to God (eg, agnostic, Buddhist, atheist, etc.) or who consider themselves “spiritual but not religious.” The latter point is important in the United States, given that there is a substantial proportion of religiously unaffiliated people who pray weekly.48 In assessing this type of prayer, the content of the PPRAYERS measure is more comprehensive and will apply to a larger and more diverse population of people with pain.
PPRAYERS has the potential for both research and clinical utility. This newly developed, brief, self-report measure will be a valuable tool in studying pain coping, as well as the relationship between religious and spiritual engagement and pain outcomes. However, we are hopeful that it could also provide clinical utility in both the health care and pastoral fields. Indeed, this measure could be used to help pastoral workers to assess the prayer of those who are experiencing physical pain. Should future research replicate findings suggesting that active prayer is associated with better pain outcomes than those experienced with passive prayer, PPRAYERS could be used by chaplains and pastors to help individuals with chronic pain expand their prayer practices, including the adoption of an active style of prayer as a way to cope with their pain.21,35 To facilitate this, 2 authors (S.M.M. and M.I.) are working to create a “bedside prayer tool” to be used by pastoral and health care providers to assist people in understanding their prayer style and how it relates to their pain experience. Future studies are needed to better understand the relationship between prayer type and pain outcomes, as well as to understand the potential utility of the bedside prayer tool. The latter, in turn, could help also to inform pastoral workers on the scientific advances that might open collaborative avenues to strengthen the emergent models of integrative and patient-centered health care models.
The results of the present study should be interpreted in the context of several limitations. First, the study participants were largely Caucasian (63%), Christian (80%), married (65%), and middle-aged (average age 43.8 years) and held a bachelor’s or master’s degree (81%), and thus the results might not generalize to a more diverse sample. Of note, participants self-reported chronic pain without specifying etiology, diagnosis, or specific duration. Because these factors could influence the use of prayer for pain, future studies should examine these variables. It is important to consider that 71% of individuals in the United States identify as Christian, and thus the religious background of our sample is relatively consistent with, or perhaps even more diverse than, that of the religious landscape of the United States as a whole.49 However, future studies should consider studying PPRAYERS in diverse religious and ethnic communities to strengthen the validation of this instrument and inform the use of prayer as a response to pain. This is particularly true for communities of Black, Indigenous, and People of Color (BIPOC) who have historically been either excluded from research or coerced into research participation and then treated unethically.50
It is also important to note that although we recruited participants who endorsed the use of prayer and/or meditation, there could be differences between individuals who primarily pray and those who primarily meditate. Future studies should examine whether this measure functions differently among these 2 potentially distinctly different groups. Second, we focused on only active, passive, and neutral verbal, petitionary prayer. It is possible that some elements of active, passive, or neutral prayer were overlooked. However, we conducted an exhaustive review of the literature and conducted extensive qualitative exploration among experts in both pain and prayer to arrive at our survey elements. Furthermore, although individuals might use other types of prayer (eg, unitive prayer, nonverbal prayer, contemplative prayer) not captured by this measure, verbal petitionary prayers have been central to the American prayer life historically and thus are important to assess.51–53 However, future studies could seek to use qualitative methodology to further assess additional types of prayer used by people with chronic pain, especially those who do not ascribe to an Abrahamic orientation.51,54 Third, although we used an expert advisory panel to develop the items in this measure, only one person with chronic pain was included in the panel. In the future, more patient stakeholders should be included at all levels of research, including the development of measures and studies. Lastly, because neutral prayer is a novel construct, there are no other measures available at this time to compare it with to provide evidence for discriminant validity. It is also possible that neutral prayer might not be a “style” of prayer or coping but instead might focus on the “object” of the prayer. Future qualitative research should further explore neutral prayer to understand how it fits into the conceptualization of prayer for pain.
PPRAYERS is a validated, helpful instrument with the potential for broad clinical and pastoral utility. At 17 items, it is ideal for research purposes to explore the coping mechanisms of people with chronic pain, as well as for clinicians and chaplains to assess prayer in clinical settings. Further strengthening PPRAYERS is its rigorous validation through structural equation modeling protocols in a diverse population, its comparison to extant spirituality and religiosity scales, and its focus on the experience of pain.
Supplementary Material
Acknowledgments
We thank all of our volunteers who helped with participant recruitment and data collection, including Barbara Bradley, Cindi Cozza, Christine Lockwood, Lyndie Mozzoni, Sr. Julian Wilson, Janice Meyer, and Paula Higgins. We also thank Drs. Robert Edwards, Adam Hirsh, Harold Koenig, and Ylisabyth Bradshaw, Daniel Carr, and the Rt. Rev. Dr. Ketlen Solak for providing their expert opinion in the development of this measure.
Contributor Information
Samantha M Meints, Department of Anesthesiology, Perioperative and Pain Medicine, Brigham and Women’s Hospital, Chestnut Hill, MA 02467, United States; Harvard Medical School, Boston, MA 02115, United States.
Marta Illueca, The Episcopal Church in Delaware, Wilmington, DE 19803, United States; Yale Program for Medicine, Spirituality and Religion, Yale School of Medicine, New Haven, CT 06510, United States.
Megan M Miller, Division of Behavioral Medicine & Clinical Psychology, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH 45229, United States; Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, OH 45229, United States.
Dikachi Osaji, Boston University School of Medicine, Boston, MA 02118, United States.
Benjamin Doolittle, Yale Program for Medicine, Spirituality and Religion, Yale School of Medicine, New Haven, CT 06510, United States.
Supplementary material
Supplementary material is available at Pain Medicine online.
Funding
This work was completed with financial support from the 2020 United Thank Offering Grant, a ministry throughout The Episcopal Church and Provinces of the Anglican Communion, provided to M.I. and financial support from the National Institutes of Health (NIH K23AR077088) provided to S.M.M.
Conflicts of interest: None declared.
References
- 1. Institute of Medicine. Relieving Pain in America. Washington, DC: National Academies Press; 2011. [Google Scholar]
- 2. Treede R-D, Rief W, Barke A, et al. Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain. 2019;160(1):19-27. [DOI] [PubMed] [Google Scholar]
- 3. Dahlhamer J, Lucas J, Zelaya C, et al. Prevalence of chronic pain and high-impact chronic pain among adults—United States, 2016. Mmwr Morb Mortal Wkly Rep. 2018;67(36):1001-1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. McCracken LM. “Attention” to pain in persons with chronic pain: a behavioral approach. Behav Ther. 1997;28(2):271-284. [Google Scholar]
- 5. Turner J, Jensen M, Romano J.. Do beliefs, coping, and catastrophizing independently predict functioning in patients with chronic pain? Pain. 2000;85(1):115-125. [DOI] [PubMed] [Google Scholar]
- 6. Turner JA, Ersek M, Kemp C.. Self-efficacy for managing pain is associated with disability, depression, and pain coping among retirement community residents with chronic pain. J Pain. 2005;6(7):471-479. [DOI] [PubMed] [Google Scholar]
- 7. Dezutter J, Wachholtz A, Corveleyn J.. Prayer and pain: the mediating role of positive re-appraisal. J Behav Med. 2011;34(6):542-549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Whittington BL, Scher SJ.. Prayer and subjective well-being: an examination of six different types of prayer. Int J Psychol Relig. 2010;20(1):59-68. [Google Scholar]
- 9. Hamman A. Prayer. Encyclopedia Britannica. July 26, 1999. https://www.britannica.com/topic/prayer. [Google Scholar]
- 10. Illueca M, Doolittle BR.. The use of prayer in the management of pain: a systematic review. J Relig Health. 2020;59(2):681-699. [DOI] [PubMed] [Google Scholar]
- 11. Andersson G. Chronic pain and praying to a higher power: useful or useless? J Relig Health. 2008;47(2):176-187. [DOI] [PubMed] [Google Scholar]
- 12. Koenig HG, George LK, Peterson BL.. Religiosity and remission of depression in medically ill older patients. Am J Psychiatry. 1998;155(4):536-542. [DOI] [PubMed] [Google Scholar]
- 13. Rippentrop AE, Altmaier EM, Chen JJ, Found EM, Keffala VJ.. The relationship between religion/spirituality and physical health, mental health, and pain in a chronic pain population. Pain. 2005;116(3):311-321. [DOI] [PubMed] [Google Scholar]
- 14. Meints SM, Hirsh AT.. In vivo praying and catastrophizing mediate the race differences in experimental pain sensitivity. J Pain. 2015;16(5):491-497. [DOI] [PubMed] [Google Scholar]
- 15. Lysne CJ, Wachholtz AB.. Pain, spirituality, and meaning making: what can we learn from the literature? Religions. 2010;2(1):1-16. [Google Scholar]
- 16. Ferreira-Valente A, Jarego M, Queiroz-Garcia I, et al. Prayer as a pain intervention: protocol of a systematic review of randomised controlled trials. BMJ Open. 2021;11(7):e047580- [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jegindø E-ME, Vase L, Skewes JC, et al. Expectations contribute to reduced pain levels during prayer in highly religious participants. J Behav Med. 2013;36(4):413-426. [DOI] [PubMed] [Google Scholar]
- 18. Jarego M, Ferreira-Valente A, Queiroz-Garcia I, et al. Are prayer-based interventions effective pain management options? A systematic review and meta-analysis of randomized controlled trials. J Relig Health. 2022;1-30. [DOI] [PubMed] [Google Scholar]
- 19. Masters KS, Spielmans GI.. Prayer and health: review, meta-analysis, and research agenda. J Behav Med. 2007;30(4):329-338. [DOI] [PubMed] [Google Scholar]
- 20. Elmholdt E-M, , SkewesJ, , Dietz M,. et al. Reduced pain sensation and reduced BOLD signal in parietofrontal networks during religious prayer. Front Hum Neurosci. 2017;11(1):337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brown GK, Nicassio PM.. Development of a questionnaire for the assessment of active and passive coping strategies in chronic pain patients. Pain. 1987;31(1):53-64. [DOI] [PubMed] [Google Scholar]
- 22. Meints SM, Mosher C, Rand KL, Ashburn-Nardo L, Hirsh AT.. An experimental investigation of the relationships among race, prayer, and pain. Scand J Pain. 2018;18(3):545-553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Riley J, Robinson ME.. CSQ: five factors or fiction? Clin J Pain. 1997;13(2):156-162. [DOI] [PubMed] [Google Scholar]
- 24. Koenig H, Büssing A.. The Duke University Religion Index (DUREL): a five-item measure for use in epidemiological studies. Religions. 2010;1(1):78-85. [Google Scholar]
- 25. Pargament K, Koenig HG, Perez LM.. The many methods of religious coping: development and initial validation of the RCOPE. J Clin Psychol. 2000;56(4):519-543. [DOI] [PubMed] [Google Scholar]
- 26. Rosenstiel AK, Keefe FJ.. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17(1):33-44. [DOI] [PubMed] [Google Scholar]
- 27. Treede R-D, Rief W, Barke A, et al. A classification of chronic pain for ICD-11. Pain. 2015;156(6):1003-1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG.. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Abbey JD, Meloy MG.. Attention by design: using attention checks to detect inattentive respondents and improve data quality. J Oper Manage. 2017;53(1):63-70. [Google Scholar]
- 30. Cella D, Riley W, Stone A, et al. ; PROMIS Cooperative Group. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63(11):1179-1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Katz P, Pedro S, Michaud K.. Performance of the Patient-Reported Outcomes Measurement Information System 29-item profile in rheumatoid arthritis, osteoarthritis, fibromyalgia, and systemic lupus erythematosus. Arthritis Care Res (Hoboken). 2017;69(9):1312-1321. [DOI] [PubMed] [Google Scholar]
- 32. Rose AJ, Bayliss E, Huang W, et al. Evaluating the PROMIS-29 v2. 0 for use among older adults with multiple chronic conditions. Qual Life Res. 2018;27(11):2935-2944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Khutok K, Janwantanakul P, Jensen MP, Kanlayanaphotporn R.. Responsiveness of the PROMIS-29 scales in individuals with chronic low back pain. Spine. 2021;46(2):107-113. [DOI] [PubMed] [Google Scholar]
- 34. Sullivan MJ, Bishop SR, Pivik J.. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7(4):524-532. [Google Scholar]
- 35. Snow-Turek AL, Norris MP, Tan G.. Active and passive coping strategies in chronic pain patients. Pain. 1996;64(3):455-462. [DOI] [PubMed] [Google Scholar]
- 36. Meints SM, Miller MM, Hirsh AT.. Differences in pain coping between Black and White Americans: a meta-analysis. J Pain. 2016;17(6):642-653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Comrey AL, Lee HB.. A First Course in Factor Analysis. New York, NY: Psychology Press; 2013. [Google Scholar]
- 38. Stevens JP. Applied Multivariate Statistics for the Social Sciences. New York, NY: Routledge; 2012. [Google Scholar]
- 39. Tabachnick BG, Fidell LS, Ullman JB.. Using Multivariate Statistics. Boston, MA: Pearson; 2007. [Google Scholar]
- 40. Wheaton B, Muthen B, Alwin DF, Summers GF.. Assessing reliability and stability in panel models. Sociol Methodol. 1977;8(1):84-136. [Google Scholar]
- 41. Hu L-t, Bentler PM.. Fit indices in covariance structure modeling: sensitivity to underparameterized model misspecification. Psychol Methods. 1998;3(4):424-453. [Google Scholar]
- 42. Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297-334. [Google Scholar]
- 43. Nagaraja V, Mara C, Khanna PP, et al. Establishing clinical severity for PROMIS® measures in adult patients with rheumatic diseases. Quality of Life Research. 2018;27(3):755-764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Koenig HG. Religion, spirituality, and health: the research and clinical implications. Int Scholar Res Not. 2012;2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Gonçalves JP, Lucchetti G, Menezes PR, Vallada H.. Religious and spiritual interventions in mental health care: a systematic review and meta-analysis of randomized controlled clinical trials. Psychol Med. 2015;45(14):2937-2949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. JPdB G, Lucchetti G, Menezes PR, Vallada H.. Complementary religious and spiritual interventions in physical health and quality of life: a systematic review of randomized controlled clinical trials. PLoS One. 2017;12(10):e0186539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Abu B, Nursalam N, Adriani M, Kusnanto K, Siti NQ, Ferry E.. The development of Islamic caring model to improve psycho-spiritual comfort of coronary disease patients. Indian J Public Health Res Dev. 2018;9(10):312317. [Google Scholar]
- 48. Pew Research Center. Religious Landscape Study. Washington, DC: Pew Research Center; 2014. [Google Scholar]
- 49. Pew Research Center. 2014 Religious Landscape Study. Washington, DC: Pew Research Center; 2014. [Google Scholar]
- 50. Janevic MR, Mathur VA, Booker SQ, et al. Making pain research more inclusive: why and how. J Pain. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wahbeh H, Sagher A, Back W, Pundhir P, Travis F.. A systematic review of transcendent states across meditation and contemplative traditions. Explore. 2018;14(1):19-35. [DOI] [PubMed] [Google Scholar]
- 52. Nuth J. Acatamiento: living in an attitude of affectionate awe—an Ignatian reflection on the unitive way. Spiritus. 2010;10(2):173-191. [Google Scholar]
- 53. Moore JP. Jr Prayer in America: A Spiritual History of Our Nation. New York, NY: Image; 2009. [Google Scholar]
- 54. Smith-Stoner M. How Buddhism influences pain control choices. Nursing2020. 2003;33(4):17. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.