Abstract
Understanding patient characteristics associated with scheduling and completing telehealth visits can identify potential biases or latent preferences related to telehealth usage. We describe patient characteristics associated with being scheduled for and completing audio and video visits. We used data from patients at 17 adult primary care departments in a large, urban public healthcare system from August 1, 2020 to July 31, 2021. We used hierarchical multivariable logistic regression to generate adjusted odds ratios (aOR) for patient characteristics associated with having been scheduled for and completed telehealth (vs in-person) visits and for video (vs audio) scheduling and completion during two time periods: a telehealth transition period (N = 190,949) and a telehealth elective period (N = 181,808). Patient characteristics were significantly associated with scheduling and completion of telehealth visits. Many associations were similar across time periods, but others changed over time. Patients who were older (≥ 65 years old vs 18–44 years old: aOR for scheduling 0.53/completion 0.48), Black (0.86/0.71), Hispanic (0.76/0.62), or had Medicaid (0.93/0.84) were among those less likely to be scheduled for or complete video (vs audio) visits. Patients with activated patient portals (1.97/3.34) or more visits (≥ 3 scheduled visits vs 1 visit: 2.40/1.52) were more likely to be scheduled for or complete video visits. Variation in scheduling/completion explained by patient characteristics was 7.2%/7.5%, clustering by provider 37.2%/34.9%, and clustering by facility 43.1%/37.4%. Stable and dynamic associations suggest persistent gaps in access and evolving preferences/biases. Variation explained by patient characteristics was relatively low compared with that explained by provider and facility clustering.
Keywords: Telemedicine, Health services accessibility, Healthcare disparities, COVID-19, Access to primary care, Primary health care
Introduction
During the coronavirus disease 2019 pandemic, many health systems began offering telehealth services in efforts to protect the health of patients and providers by promoting social distancing [1]. Telehealth services include synchronous telephonic (audio) and video (audio-visual) encounters whereby patients and clinicians can communicate with each other remotely. Even prior to this rapid implementation of telehealth, there were concerns about equitable access to telehealth services (the “digital divide”); for example, certain demographic groups may have differing access to, literacy with, or attitudes towards technology that would influence participation in telehealth [2-4]. Early studies during the pandemic demonstrated differences in telehealth usage based on patients’ identified sex, age, and language [5-10]. However, most studies were conducted in settings where a majority of patients were White and speak English as their preferred language [6-10]. Also, studies largely looked at completion of encounters rather than scheduling [5-10]. Appointment scheduling is an opportunity for patients to make their preference for appointment type known and may also be a point where bias can influence who receives telehealth appointments. Whether disparities exist in more diverse settings and in the scheduling process are less well-established.
We seek to describe the characteristics of patients who have been scheduled for or have utilized telehealth at a large, urban public healthcare system in New York City. Understanding the extent to which patient characteristics relate to telehealth scheduling and usage will inform policies and interventions around telehealth.
Methods
Data Source
In this observational study, we examine electronic health record (EHR) data from all patients with scheduled or completed encounters in 17 adult primary care departments at a large, multi-site, urban public healthcare system in New York City from August 1, 2020 to July 31, 2021. During this time, system-mandated restrictions on in-person visits imposed during the early pandemic were lifted. For each appointment, patients could elect to be scheduled for one of three different types of visits: in-person, audio, and video. Clinicians and patients could decide upon scheduling which visit type would be appropriate or preferable for a given visit. No explicit inclusion or exclusion criteria were used at a system level for scheduling and usage of telehealth. Only visits scheduled for physicians, physician associates, nurse practitioners, and residents were included in analysis.
We further divided the data into two periods: (1) a telehealth transition period (August 1, 2020 to February 28, 2021) when patients just began having the option of elective telehealth usage, 40–50% of visits were being scheduled as telehealth, and video visit scheduling was < 5% and (2) a telehealth elective period (March 1, 2021 to July 31, 2021) when patients had already been able to schedule telehealth visits electively for six months, 20–40% of visits were being scheduled as telehealth, and video visit scheduling was > 5%.
This study was exempt from full review by the Biomedical Research Alliance of New York institutional review board.
Primary Outcomes
The primary outcomes are binary, patient-level classifications of being scheduled for telehealth visits and, separately, completion of telehealth visits. We classified patients as having been scheduled for or completed: only in-person visits (in-person only scheduled, in-person only user), at least one telehealth visit but by audio (audio telehealth scheduled, audio telehealth user), or at least one telehealth visit including at least one video visit (video telehealth scheduled, video telehealth user). For telehealth visit types (audio and video visits), a visit may be scheduled as one visit type but completed using another; for example, a patient may be scheduled for a video visit but complete an audio visit (or vice versa). Some patients may be scheduled for video visits (are video telehealth scheduled) but only complete audio visits (and thus are audio telehealth users).
We identified scheduled telehealth encounters based on a “visit type” field in the EHR and completed telehealth encounters based on procedure billing codes. Encounters with telephone evaluation and management codes (99441–99443) were classified as telephonic (audio) visits, and other encounters with GT or 95 modifiers were classified as video visits. Encounters that did not have telephonic codes or telehealth modifiers were classified as in-person visits.
Patient Characteristics
We collected patient characteristics that have previously been shown to be associated with telehealth usage including: age, sex, race/ethnicity, primary language, insurance, patient portal activation status, and number of scheduled appointments during the sample interval [5-11]. Additionally, we identified Elixhauser comorbidity flags based on EHR problem lists and encounter diagnoses during the study interval [12].
Statistical Analysis
We calculated the proportion of patients with our primary outcomes. We performed descriptive statistics for patient characteristics and bivariate analyses between patients who did and did not have scheduled or completed telehealth visits using chi-squared or t tests as appropriate.
We used hierarchal multiple logistic regression to test for associations between the primary outcomes and patient characteristics while accounting for variation at the level of clinicians and facilities using random effects. We include all patient characteristics as covariates in the model to account for each characteristic’s independent association with the outcomes.
For the telehealth transition period, because of the low proportion of video visits scheduled, we combine audio and video groups as “telehealth scheduled” and “telehealth user” groups for the regression model (with in-person only scheduled and in-person only user as the reference groups).
For the elective telehealth period, we use a similar grouping to compare patient characteristics for telehealth versus in-person only scheduled and user groups.
Then, among telehealth scheduled and telehealth user groups, we use hierarchal multiple logistic regression to identify patient characteristics’ associations with audio versus video scheduled and user groups. We also report the relative contribution (intraclass correlation) of patient characteristics, clustering by clinician, and clustering by facility in patients’ telehealth scheduling and usage patterns.
A threshold of p < 0.05 was used to determine statistical significance. All statistical analyses were done using Stata SE, Version 15.
Results
Sample Description
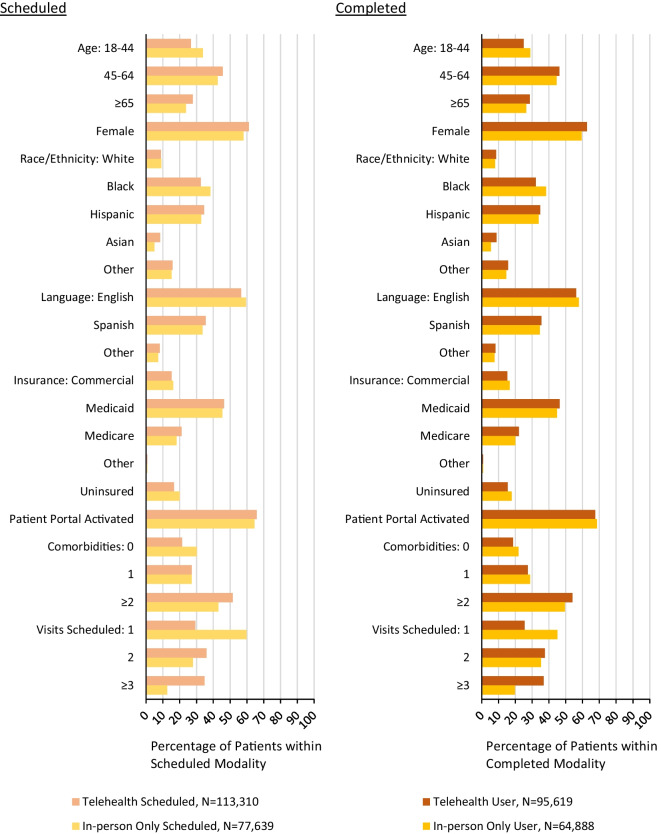
There were 190,949 patients with scheduled primary care appointments and 160,507 patients with completed primary care appointments in the telehealth transition period. Of patients with scheduled appointments, 113,310 (59.3%) were telehealth scheduled (Fig. 1). Of patients with completed appointments, 95,619 (59.6%) were telehealth users (Fig. 1). During this period, 94.9% of telehealth visits were scheduled as audio. Of patients that were scheduled for telehealth visits, 95,619 (84.4%) completed at least one telehealth visit.
Fig. 1.
Characteristics of patients with and without any scheduled and completed telehealth visits during the telehealth transition period. p < 0.001 for all comparisons between telehealth and in-person
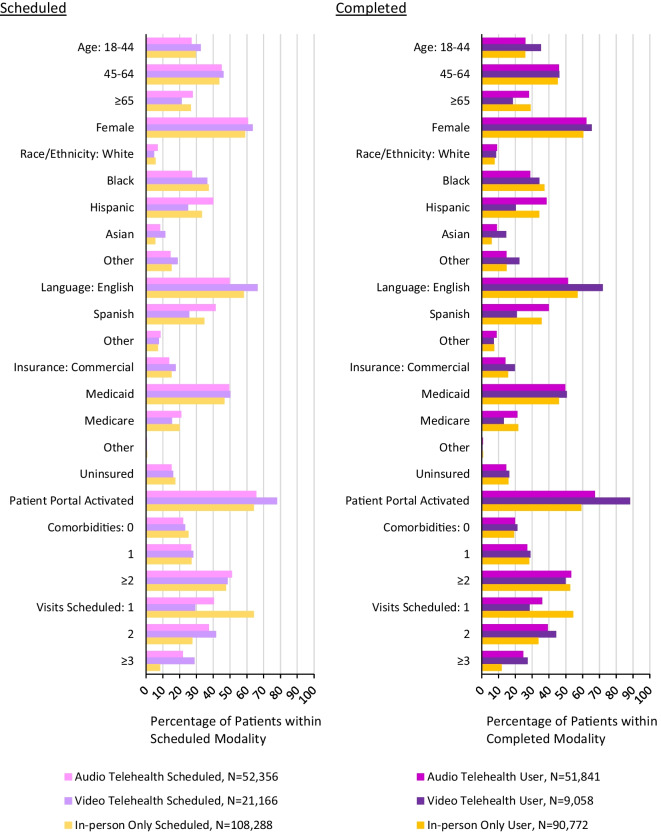
There were 181,808 patients with scheduled primary care appointments and 151,668 patients with completed primary care appointments in the telehealth elective period. Of patients with scheduled appointments, 52,356 (28.8%) were audio telehealth scheduled and 21,165 (11.6%) were video telehealth scheduled (Fig. 2); the remainder were in-person only scheduled. Of patients with completed appointments, 51,840 (34.2%) were audio telehealth users and 9,057 (6.0%) were video telehealth users (Fig. 2). During this period, 74.4% of telehealth visits were scheduled as audio and 25.6% were scheduled as video visits.
Fig. 2.
Characteristics of patients with in-person only, audio telehealth, and video telehealth scheduled and completed visits during the telehealth elective period. p < 0.001 for all comparisons between telehealth and in-person
Scheduling and Completion of Telehealth Visits Between Time Periods
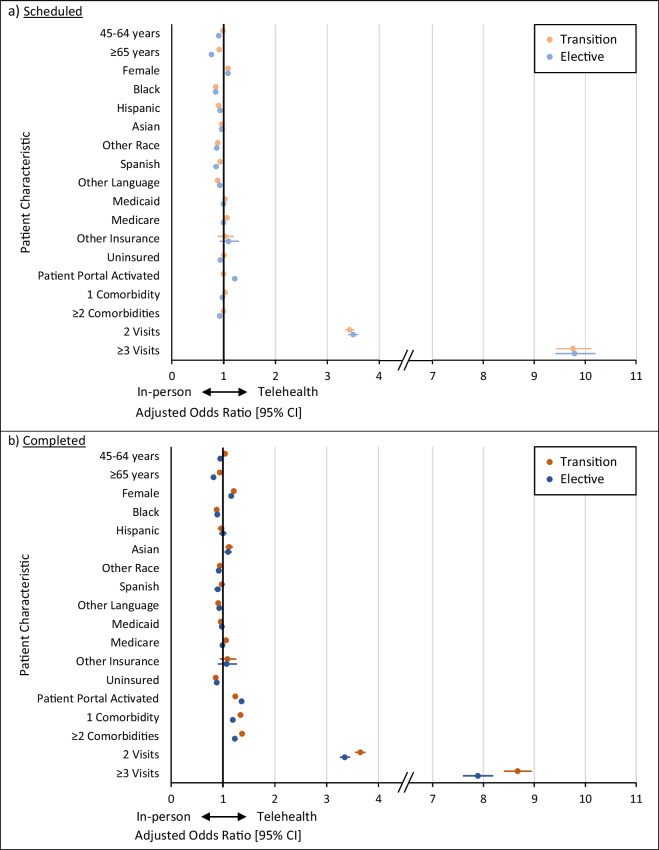
Patient characteristics associated with having telehealth visits scheduled were generally similar across both time periods (Fig. 3a). In both time periods, patients who were female (compared to male) or who had two or more scheduled visits (compared to one visit) during the time periods were more likely to have been scheduled for telehealth visits. In both time periods, patients who were 65 years old or older (compared with patients 18–44 years old), Black or other race (compared with White), or had a primary language other than English or Spanish (compared with English) were less likely to have been scheduled for telehealth visits. In the transition period only, patients who had Medicare (compared to commercial insurance) were more likely to have been scheduled for telehealth visits. In the transition period only, patients who were Hispanic (compared with White) were less likely to have been scheduled for telehealth visits. In the elective period only, patients who were 45–64 years old (compared with patients 18–44 years old), had a primary language of Spanish (compared with English), were uninsured (compared with having commercial insurance), or had two or more comorbidities (compared with no comorbidities) were less likely to have been scheduled for telehealth visits. In the elective period only, patients with an activated patient portal (compared with not having an activated patient portal) were more likely to have been scheduled for telehealth visits.
Fig. 3.
Patient characteristics in telehealth transition and elective periods associated with having telehealth visits scheduled and completed, organized by visit scheduled and completed statuses
Many patient characteristics associated with having completed telehealth visits were also generally similar across time periods (Fig. 3b). In both time periods, patients who were female, Asian, had an activated patient portal, had one or more comorbidities, and had two or more scheduled visits were more likely to have completed telehealth visits. In both time periods, patients who were 65 years old or older, Black or other race, had a primary language other than English or Spanish, or were uninsured were less likely to have completed telehealth visits. In the transition period only, patients aged 45–64 and patients who had Medicare were more likely to have completed telehealth visits. In the transition period only, patients who had Medicaid were less likely to have completed telehealth visits. In the elective period only, patients who were 45–64 years old and patients who had a primary language of Spanish were less likely to have completed telehealth visits.
Scheduling and Completion of Telehealth Visits Within Time Periods
When considering scheduling and completion of telehealth visits within the transition period (Fig. 4a), patients who were female, had Medicare, and had two or more visits scheduled were more likely to both be scheduled for and have completed telehealth visits than their comparators. While patients who were 45–64 years old, Asian, had an activated patient portal, and had one or more comorbidities were not more likely to be scheduled, they were more likely to have completed telehealth visits. Patients who were 65 years old or older, Black or other race, or had a primary language other than English or Spanish were less likely to be scheduled for or have completed telehealth visits. Patients who were Hispanic were less likely to be scheduled for, but not less likely to complete, telehealth visits. Patients who had Medicaid or were uninsured were not less likely to be scheduled for but were less likely to have completed telehealth visits.
Fig. 4.
Patient characteristics associated with having telehealth visits scheduled and completed, organized by time period (telehealth transition and elective periods)
When considering scheduling and completion of telehealth visits within the elective period (Fig. 4b), patients who were female, had an activated patient portal, or had two or more visits scheduled were more likely to be scheduled for and have completed telehealth visits than their comparators. While patients who were Asian or had one or more comorbidities were not more likely to be scheduled, they were more likely to have completed telehealth visits. Patients who were 45 years old or older, Black or other race, had a primary language of Spanish or other language, or were uninsured were less likely to be scheduled for or complete telehealth visits. Patients with two or more comorbidities were less likely to be scheduled for but not less likely to have completed telehealth visits.
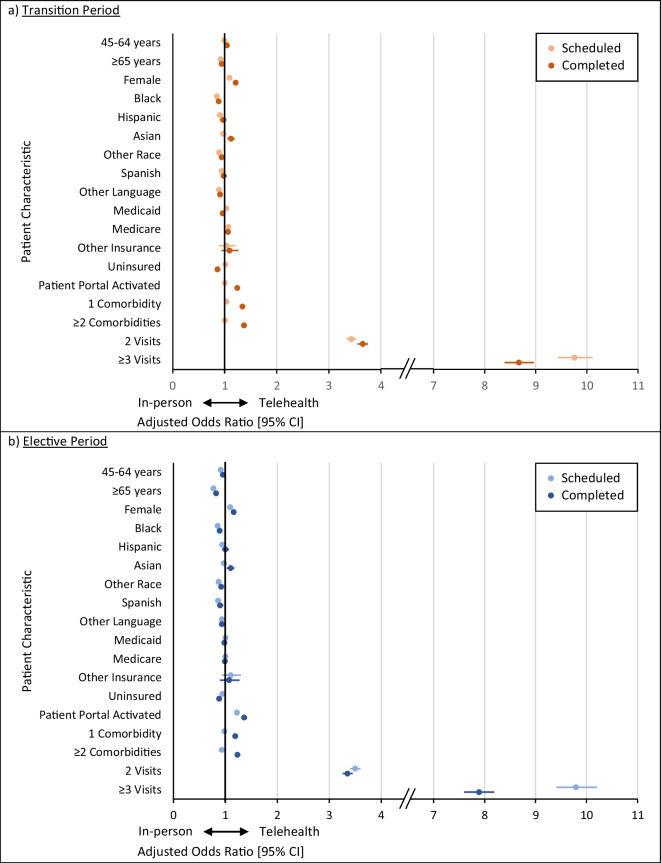
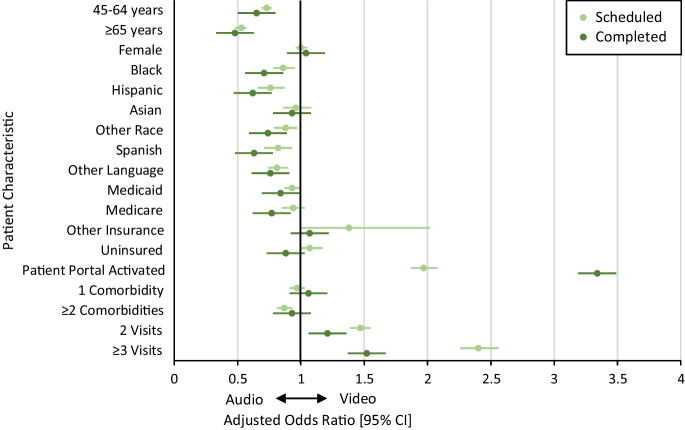
Patient Characteristics Associated with Audio vs Video Telehealth in the Elective Period
Patients who had an activated patient portal or who had two or more scheduled visits were more likely to be scheduled for and have completed video (versus audio) visits (Fig. 5). Patients who were 45 years old or older, Black, Hispanic, or another race (aside from Asian), or had Spanish or another non-English language as their primary language, or had Medicaid were less likely to be scheduled for and have completed video visits. Patients who have Medicare or who were uninsured were not less likely to be scheduled for but were less likely to have completed video visits.
Fig. 5.
Patient characteristics associated with having audio vs video telehealth visits scheduled and completed (among telehealth users) during the telehealth elective period
Contributions to Variation by Patient Characteristics vs Provider and Facility
The percentage of variation in having telehealth versus solely in-person visits scheduled explained by patient characteristics was 7.2%, clustering by provider 37.2%, and clustering by facility 43.1% (with the remaining variation unexplained by the model). The percentage of variation in having completed telehealth versus solely in-person visits explained by patient characteristics was 7.5%, clustering by provider 34.9%, and clustering by facility 37.4%.
Discussion
In this observational study of scheduled and completed primary care visits at a large, urban, public healthcare system, we found that there were modest differences between demographic groups in patterns of telehealth scheduling and completion and variation in these differences over time. However, while there were some differences in telehealth usage based on patient characteristics, far more variation could be explained by clustering at provider or facility levels, with patient-level variation contributing the least.
Demographic differences were present in scheduled visits, suggesting potential latent preferences by patients, clinicians, or facilities or biases in offering telehealth modalities. In the telehealth transition period, patients who were older than 65 years old, Black, Hispanic, or Other Race, or who preferred Other Languages were less likely to have telehealth visits scheduled relative to patients in their comparator groups. In the telehealth elective period (compared with the telehealth transition period), some differences became more pronounced; for example, patients older than 65 years old were even less likely relative to younger patients to scheduled telehealth visits. New differences also emerged; for example, during the telehealth transition period, patients at all levels of comorbidity had similar propensities to schedule telehealth visits, but in the elective telehealth period, patients with two or more comorbidities were less likely than those with no comorbidities to schedule telehealth visits. Overall, this suggests that there is selection happening at the time of scheduling that may influence demographic differences in telehealth utilization and that such selection may change over time.
Our findings show decreased propensity to complete telehealth visits and to participate in video telehealth for older, Black, Hispanic, other race, non-English speaking, and uninsured patients and higher propensity for patients who were female, Asian, had an activated patient portal, more comorbidities, and more scheduled visits. Prior literature on demographic factors associated with telehealth usage has generally been mixed, with some factors being positively associated in some studies but negatively associated in others [2-10]. While the relevant factors remain relatively constant, this variation hints that there may be contextual elements that may be more influential than demographic block identifiers.
In both time periods, the factor most positively associated with audio or video telehealth scheduling and completion was the number of scheduled visits during the period of study. To our knowledge, this study is among the first to report on this association [11]. This suggests that patients can, over time and with exposure, learn to become telehealth users (and video users) despite any differences related to demographic variation. Additionally, it suggests that for patients who have multiple visits over the course of a year, it may make sense for both the provider and patient for some of those visits to be done using telehealth.
Consistent with a study of a large, integrated health system that reported proportions of observed variation in telehealth completion explained by patient factors versus clinician- or facility-level clustering [3], we saw that a majority of observed variation is due to clinician and facility clustering. While much discussion has been centered around disparities or inequities in care delivery driven by patient demographic factors or proxies for digital access and literacy, additional focus is needed to examine and address gaps in clinician comfort with telehealth, workflows/practices, and potential biases therein. These issues may partly relate to design of telehealth platforms, and presence or absence of critical functions for diverse patient, clinician, and staff user populations such as interpreter services integration and a simple user experience. Beyond this, more clinician and staff training and usage of structured assessments for patients’ telehealth capabilities or preferences may help minimize variation in practice due to biases from within the health system.
Limitations
While we did observe differences in demographics for scheduled visits, we are unable to determine the root cause of these differences (i.e. implicit or explicit bias in offering of telehealth services to patients of certain demographic groups versus actual patient preferences or ability at the time). We did not control for factors such as geographic distance from the patient’s address to their primary care facility, patient income, education level, or broadband access. Our health system had a high utilization of audio telehealth visits, which may not be representative of other health systems’ experiences or service design choices.
Conclusions
There are differences in demographic profiles of patients who participate in audio telehealth, video telehealth, and in-person only services in primary care. Most of the variation observed may be due to variability at the level of clinicians and facilities rather than patient characteristics. Future studies should further refine phenotypic categorization of telehealth users and non-users and associated characteristics and examine potential interventions (including those focused on clinicians and facility staff) to ensure equitable participation in telehealth.
Acknowledgments
This work was supported in part by a grant (21–12977) from the New York Health Foundation (https://nyhealthfoundation.org/) for establishing a telehealth navigator program (KC, HJ). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Baum A, Kaboli PJ, Schwartz MD. Reduced In-Person and Increased Telehealth Outpatient Visits During the COVID-19 Pandemic. Ann Intern Med. 2021;174(1):129–131. doi: 10.7326/M20-3026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reed ME, Huang J, Graetz I, et al. Patient Characteristics Associated With Choosing a Telemedicine Visit vs Office Visit With the Same Primary Care Clinicians. JAMA Netw Open. 2020;3(6):e205873. doi: 10.1001/jamanetworkopen.2020.5873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rodriguez JA, Saadi A, Schwamm LH, Bates DW, Samal L. Disparities In Telehealth Use Among California Patients With Limited English Proficiency. Health Aff (Millwood) 2021;40(3):487–495. doi: 10.1377/hlthaff.2020.00823. [DOI] [PubMed] [Google Scholar]
- 4.Ramsetty A, Adams C. Impact of the digital divide in the age of COVID-19. J Am Med Inform Assoc. 2020;27(7):1147–1148. doi: 10.1093/jamia/ocaa078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodriguez JA, Betancourt JR, Sequist TD, Ganguli I. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care. 2021;27(1):21–26. doi: 10.37765/ajmc.2021.88573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yuan N, Pevnick JM, Botting PG, Elad Y, Miller SJ, Cheng S, Ebinger JE. Patient Use and Clinical Practice Patterns of Remote Cardiology Clinic Visits in the Era of COVID-19. JAMA Netw Open. 2021;4(4):e214157. doi: 10.1001/jamanetworkopen.2021.4157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Eberly LA, Kallan MJ, Julien HM, et al. Patient Characteristics Associated With Telemedicine Access for Primary and Specialty Ambulatory Care During the COVID-19 Pandemic. JAMA Netw Open. 2020;3(12):e2031640. doi: 10.1001/jamanetworkopen.2020.31640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Darrat I, Tam S, Boulis M, Williams AM. Socioeconomic Disparities in Patient Use of Telehealth During the Coronavirus Disease 2019 Surge. JAMA Otolaryngol Head Neck Surg. 2021;147(3):287–295. doi: 10.1001/jamaoto.2020.5161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eberly LA, Khatana SAM, Nathan AS, et al. Telemedicine Outpatient Cardiovascular Care During the COVID-19 Pandemic: bridging or Opening the Digital Divide? Circulation. 2020;142(5):510–512. doi: 10.1161/CIRCULATIONAHA.120.048185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pierce RP, Stevermer JJ. Disparities in use of telehealth at the onset of the COVID-19 public health emergency. J Telemed Telecare. 2020 1357633X20963893 [DOI] [PMC free article] [PubMed]
- 11.Chen K, Zhang C, Gurley A, Akkem S, Jackson H. Primary care utilization among telehealth users and non-users at a large urban public healthcare system. PLoS ONE. 2022;17(8):e0272605. doi: 10.1371/journal.pone.0272605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]