1. Case
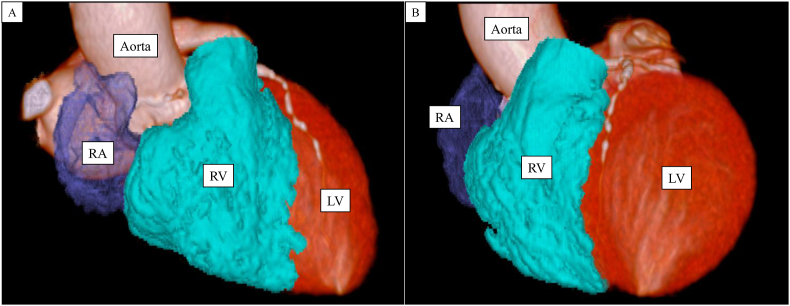
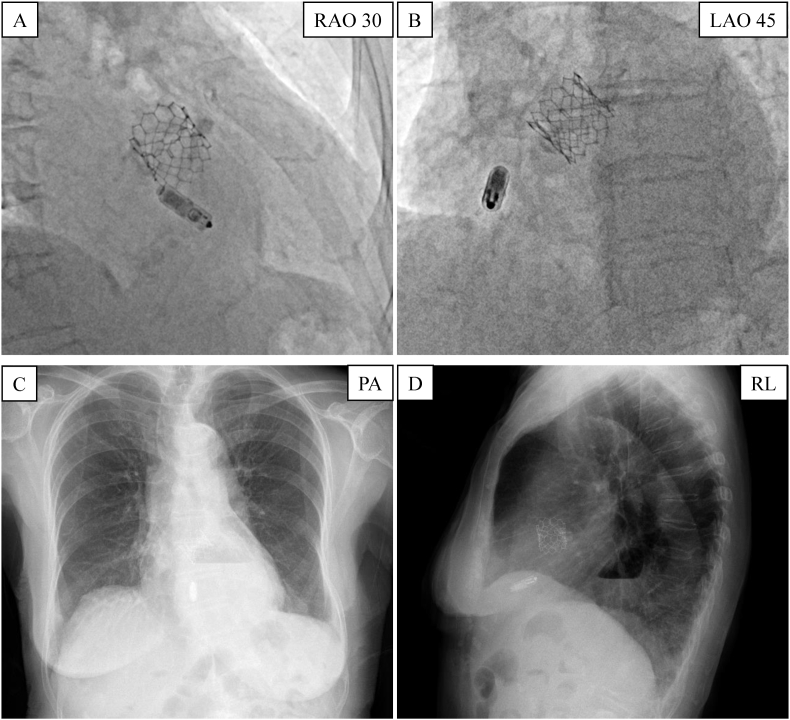
An 89-year-old woman underwent a leadless pacemaker (Micra TPS, Medtronic Inc, Minneapolis, MN) implantation because of iatrogenic transient atrioventricular block after a percutaneous transcatheter aortic valve replacement. According to the computed tomography analysis, no obstructed veins or venous anomalies were found. This patient had a relatively small right heart, with a right atrium (RA) of 30 ml and right ventricle (RV) of 78 ml. Moreover, this patient's heart was rotated in the counterclockwise direction, and we could not see the heart's apex tangentially without a shallow left-anterior-oblique view (left-anterior-oblique 20°) (Fig. 1A and B). However, the first deployment allowed the Micra TPS to be implanted on the RV mid-septum. The electrical parameters were also stable after the tug test: the pacing threshold was 0.25 V at 0.24 ms, RV sensing 5.2 mV, and impedance 490 Ω. Those measurements were comparable to those obtained before the tug test. During the fluoroscopy examination, two out of four tines seemed to be engaged in the RV. Although the pacing impedance was relatively low, the pacing threshold was stable and no migration of the Micra TPS was observed on the fluoroscopy images. Thus, it was decided to consider the release was good. After pulling the tether very gently, no changes in the electrical parameters or device position were observed and we concluded the operation (Fig. 2A and B).
Fig. 1.
Three-D cardiac CT reconstruction images of the right heart in the right anterior oblique 40° (A) and left anterior oblique 20° (B) views.
CT = computed tomography; LV = left ventricle. RA = right atrium; RV = right ventricle.
Fig. 2.
Fluoroscopic images in the RAO (A) and LAO (B) views during the Micra TPS implantation. The chest radiograph in the PA (C) and RL (D) views shows the migration of the Micra TPS.
LAO = left anterior oblique; PA = posterior-anterior; RAO = right anterior oblique; RL = right-left.
The day after the Micra TPS implantation, an electrocardiogram showed non-captured pacing impulses and the Micra TPS electrical evaluation revealed no capture regardless of the output voltage. A chest radiograph demonstrated the migration of the Micra TPS (Fig. 2C and D). No pericardial effusion was observed on the echocardiography. Fortunately, the patient was asymptomatic thanks to her escape beats.
An attempt at the device retrieval was performed 3 days after the index implant. The Micra TPS interrogation just before the procedure indicated that the RV sensing was 4.6 mV and that the pacing impedance had dropped to 360 Ω.
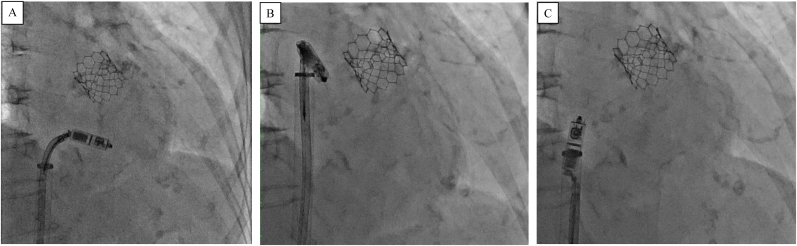
An Atrieve snare (Argon Medical, Frisco, Texas, USA) was used to capture the proximal end of the Micra TPS and engage it (Fig. 3A). Despite constant traction, the Micra TPS failed to pull out from the myocardium. Conversely, by applying a pushing force, the Micra TPS was successfully extracted, and the entire system was pulled out in one piece (Fig. 3B and C). During the same procedure, a new transvenous dual-chamber pacemaker was successfully implanted.
Fig. 3.
A: A single loop retrieval snare entrapped the retrieval feature at the proximal end of the Micra TPS.
B: The Micra TPS was successfully extracted by applying a pushing force.
C: The captured device was subsequently withdrawn via the Micra TPS introducer sheath.
Even in retrospect, we believe it would have been difficult to have anticipated such a device migration because of the quite good pacing threshold during the implantation.
2. Discussion
An insufficient tine insertion into the trabecular tissue of the RV may be the cause of a sudden rise in the pacing threshold and device migration [1], nevertheless, the electrical measurements at the time of the implantation and visualization of the tine migration with heartbeats may not allow for a diagnosis. In this case, fluoroscopic checks and an evaluation of the electrical parameters were performed before and after the removal of the delivery catheter and 23 French sheath at the time of the implantation of the Micra TPS. In particular, the pacing threshold was consistently 0.25 V/0.24 ms. However, the electrical parameters and radiographs showed that the Micra TPS was not sufficiently fixed to the trabeculated tissue only on the day after the implantation.
A previous study demonstrated that optimal pacing thresholds of ≦ 1 V during the Micra TPS operation likely do not require repositioning.
However, the pacing impedance after the fixation has been reported to predict an increased pacing threshold during the follow-up period.
Kiani et al. showed that a pacing impedance of <800 Ω at the time of the implantation was associated with an increased capture threshold at 12 months [2]. Other reports have indicated that a pacing impedance at the time of the implantation of >600 Ω or 660 Ω is a predictor of an acceptable threshold [3,4]. In this case, the low impedance (490 Ω at the time of the implantation) may have indicated poor contact of the Micra TPS with the myocardium. Furthermore, this patient had a counterclockwise rotation of the heart. That may have led to difficulty in placing the Micra TPS perpendicular to the RV myocardium. In this case, right ventriculography was not performed. Recently, the technique of right ventriculography via a contrast injection under fluoroscopy has been used to place the pacing lead tip in the RV septum. That may help us to place the Micra TPS on the RV septum [5]. Furthermore, a previous study showed that a mid-septal implantation of the Micra TPS has advantages in terms of the surgical safety and a narrower paced QRS duration than an implantation in the RV apex [6]. Therefore, during the Micra TPS operation, paying attention to not only the pacing threshold but also the pacing impedance and right ventriculography to guide the Micra TPS implantation may be a useful method, especially for patients with specific cardiac anatomical variations such as a counterclockwise rotation observed in routine clinical practice. On the other hand, multiple deployments have a potential risk of causing devastating complications [7]. Implanters should decide on the treatment strategy by balancing the potential for the device to become dislodged again with the risk of cardiac complications.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: The Section of Arrhythmia is supported by an endowment from Abbott JAPAN, Medtronic JAPAN, and Boston Scientific JAPAN. Ken-ichi Hirata chairs the Section, and Koji Fukuzawa and Mitsuru Takami belong to the Section. However, all authors report no conflict of interest for this manuscript's content.
Acknowledgment
We would like to thank Mr. John Martin for his linguistic assistance.
Footnotes
Peer review under responsibility of Indian Heart Rhythm Society.
References
- 1.Eggen M.D., Grubac V., Bonner M.D. Design and evaluation of a novel fixation mechanism for a transcatheter pacemaker. IEEE Trans Biomed Eng. 2015;62:2316–2323. doi: 10.1109/TBME.2015.2449320. [DOI] [PubMed] [Google Scholar]
- 2.Kiani S., Wallace K., Stromberg K., Piccini J.P., Roberts P.R., El-Chami M.F., Soejima K., Garweg C., Fagan D.H., Lloyd M.S. A predictive model for the long-term electrical performance of a leadless transcatheter pacemaker. JACC Clin Electrophysiol. 2021;7:502–512. doi: 10.1016/j.jacep.2020.09.010. [DOI] [PubMed] [Google Scholar]
- 3.Tolosana J.M., Guasch E., San Antonio R., Apolo J., Pujol-Lopez M., Chipa-Ccasani F., Trucco E., Roca-Luque I., Brugada J., Mont L. Very high pacing thresholds during long-term follow-up predicted by a combination of implant pacing threshold and impedance in leadless transcatheter pacemakers. J Cardiovasc Electrophysiol. 2020;31:868–874. doi: 10.1111/jce.14360. [DOI] [PubMed] [Google Scholar]
- 4.Higuchi M., Shinoda Y., Hasegawa T., Ishibashi M., Yamada N., Chiba Y., Ohira K., Murata M., Aonuma K. Predictors of increase in pacing threshold after transcatheter pacing system implantation due to micro-dislodgement. Pacing Clin Electrophysiol. 2020;43:1351–1357. doi: 10.1111/pace.14080. [DOI] [PubMed] [Google Scholar]
- 5.Shimeno K., Yoshiyama T., Abe Y., Akamatsu K., Kagawa S., Matsushita T., Matsuo M., Matsumura Y., Matsumoto R., Kamimori K., Naruko T., Doi A., Takagi M., Yoshiyama M. The usefulness of right ventriculography to aid anchoring a pacing lead to the right ventricular septum. Europace. 2018;20:1154–1160. doi: 10.1093/europace/eux165. [DOI] [PubMed] [Google Scholar]
- 6.Sharma P., Singh Guleria V., Bharadwaj P., Datta R. Assessing safety of leadless pacemaker (MICRA) at various implantation sites and its impact on paced QRS in Indian population. Indian Heart J. 2020;72:376–382. doi: 10.1016/j.ihj.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Piccini J.P., Cunnane R., Steffel J., El-Chami M.F., Reynolds D., Roberts P.R., Soejima K., Steinwender C., Garweg C., Chinitz L., Ellis C.R., Stromberg K., Fagan D.H., Mont L. Development and validation of a risk score for predicting pericardial effusion in patients undergoing leadless pacemaker implantation: experience with the Micra transcatheter pacemaker. Europace. 2022;24:1119–1126. doi: 10.1093/europace/euab315. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.