Abstract
Background
Up to 67% of adults experience shoulder pain in their lifetime. Numerous factors are related to the etiology of shoulder pain, one of which is thought to be scapular dyskinesis (SD). Given the prevalence of SD among the asymptomatic population a concern is that the condition is being medicalized (clinical findings suggested to require treatment but is ultimately a normal finding). Therefore, the purpose of this systematic review was to investigate the prevalence of SD among both symptomatic and asymptomatic populations.
Methods
A systematic review of the literature up to July of 2021. Relevant studies identified from PubMed, EMBASE, Cochrane and CINAHL were screened utilizing the following inclusion and exclusion criteria; inclusion: (a) individuals being assessed as having SD, including reliability and validity studies (b) subjects aged 18 or older; (c) sport and non-sport participants; (d) no date restriction; (e) symptomatic, asymptomatic, or both populations; (f) all study designs except case reports. Studies were excluded if: (a) they were not published in the English language; (b) they were a case report design; (c) the presence of SD was part of the studies inclusion criteria; (d) data were not present distinguishing the number of subjects with or without SD; (e) they did not define participants as having or not having SD. Methodological quality of the studies was assessed utilizing the Joanna Briggs Institute checklist.
Results
The search resulted in 11,619 after duplicates were removed with 34 studies ultimately retained for analysis after three were removed due to low quality. A total of 2,365 individuals were studied. Within the studies for the symptomatic athletic and general orthopedic population there were 81% and 57% individuals with SD, respectively, and a total of 60% among both symptomatic groups (sport and general orthopedic population). Within the studies for the asymptomatic athletic and general population there were 42% and 59% individuals with SD, respectively, and a total of 48% among both asymptomatic groups (sport and general orthopedic population).
Limitation
A strict inclusion and exclusion criteria was used to identify studies that provided the appropriate data for the purpose of this study. There was a lack of consistency for measuring SD across studies.
Conclusion
A considerable number of individuals with shoulder symptoms do not present with SD. More revealing is the number of asymptomatic individuals who do present with SD, suggesting that SD may be a normal finding among nearly half of the asymptomatic population.
Level of Evidence
2a
Keywords: shoulder pain, scapular dyskinesis, overhead sports, scapular translation, symptomatic, asymptomatic
INTRODUCTION
Within the adult population, 67% of individuals will experience shoulder pain at some point throughout their lifetime.1 There are numerous factors related to the etiology of shoulder pain and it has been hypothesized that the presence of scapular dyskinesis (SD) is a contributing factor to shoulder pathology.2,3 Scapular dyskinesis has been defined as alterations in scapular positioning at rest as well as during dynamic movement. Common variations in scapular movement4,5 include increased scapular superior translation along with reduced scapular posterior tilt, upward rotation, and internal rotation.6 Give the theorized relationship between SD and certain shoulder pathologies there have been several methods proposed to evaluate these alterations in scapular positions and movements.
McClure et al.7 developed a commonly used method of identifying SD, the scapular dyskinesis test (SDT), to identify the presence of SD and classify individuals into three levels: normal motion, subtle dyskinesis, and obvious dyskinesis. This is one of several methods commonly used during an evaluation related to shoulder pathology presented in Supplement A Though the SDT has been proven to be a reliable and valid method of identifying SD6,7 not all clinicians are trained to use this tool and current literature describes a wide variation of assessment methodology.6 Along with this lack of homogeneity in assessment of SD, there is a lack of evidence to support the idea that identification and correction of SD may help to prevent or treat shoulder pathology. Even with this lack of evidence, identifying SD is a common screening tool for both symptomatic and asymptomatic individuals. The evaluation is especially common in predicting or preventing injury in overhead athletes, however there is conflicting evidence regarding the link between SD and injury in this population exists.8,9 Clinicians often direct their treatment toward correcting the SD which could be normal movement variability.10,11
Because the identification of SD is a common part of a patient evaluation, it is often used to guide clinical decision making; however, there is considerable debate around linking the presence of SD to certain shoulder pathologies. Some studies have shown no difference in the prevalence of SD between symptomatic and asymptomatic populations.12 This raises the question of utility when screening for SD in patients seeking treatment for shoulder pain as well as for the asymptomatic population.
The purpose of this systematic review of the current literature to investigate the prevalence of SD among both symptomatic and asymptomatic populations. Understanding the relationship between SD and the presence or absence of symptoms may help to direct conversations regarding the clinical utility of SD. The authors hypothesized that SD is a common finding that has been medicalized (clinical findings suggested to require treatment but is ultimately a normal finding).
MATERIALS AND METHODS
Guidelines
This systematic review utilized the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines during the search and reporting phase of the research process. The PRISMA statement includes a 27-item checklist designed to improve reporting of systematic reviews and meta-analyses.13
Literature search
An online literature search was conducted utilizing PubMed, EMBASE, Cochrane and CINAHL from the dates of their origin until July 2021. The search strategy was created and performed by a biomedical librarian. An example of the search strategy used for the PubMed database is provided (Supplement B) and similar strategies were utilized for the remaining databases. The study was registered using the International Prospective Register of Systematic Reviews (PROSPERO) in May of 2020 with a corresponding reference number: CDR42020187045.
Study selection
All titles were independently appraised by two authors (TB) and (AW) after the initial online literature search for studies to be retained. The abstracts of these titles were read to determine if the studies met the inclusion criteria. Studies with abstracts that met the inclusion criteria were accessed in their full-text format and then read to determine their eligibility for the review. The same two authors performed the study selection process for this review with a third author (PS) available to handle disagreements. The inclusion criteria for studies to be retained in the present review consisted of: (a) individuals being assessed as having SD, including reliability and validity studies (b) subjects aged 18 or older; (c) sport and non-sport participants; (d) no date restriction; I symptomatic, asymptomatic, or both populations; (f) all study designs except case reports. Studies were excluded if: (a) they were not published in the English language; (b) they were a case report design; (c) the presence of SD was part of the studies inclusion criteria; (d) data were not present distinguishing the number of subjects with or without SD; I they did not define participants as having or not having SD.
Data extraction
The data and results from the studies that were retained as part of the review were extracted using a format to identify study type, population, methods for evaluating SD, and the prevalence of SD. Data were extracted, reviewed, and analyzed by the primary author (PS) and verified by a research assistant (ZS). Discrepancies in data collection were resolved through discussion.
Methodological Quality Assessment Tool
The Joanna Briggs Institute (JBI) checklist for prevalence studies was used to evaluate methodological quality within the individual studies.14 There are nine items related to methodological quality included in the checklist which can be answered as yes, no, unclear, or not applicable. Following the scoring of each item, those individuals scoring the study are asked to provide an overall appraisal to include, exclude, or seek further information regarding if the article should be retained. The decision to include or exclude each article is then made by the reviewer(s) based on the completed checklist and consensus. Two authors, (DH) and (AM), performed the methodological quality assessment independently with discrepancies handled by the primary author if necessary. Prior to methodological quality assessment those involved in worked through scoring several unrelated prevalence studies in order to align definitions and interpretations of the various elements present in the JBI tool.
Data Synthesis and Analysis
Data were extracted and pooled to include the incidence of scapular dyskinesis, as defined by the authors, among those individuals that were symptomatic and those that were asymptomatic. The results were reported on percentage of incidence differentiating between classification of individuals with SD and shoulders with SD among each identified population. Data on relevant subcategories were identified and individually accounted for with separate analyses. Data from the identified studies did not allow for a quantitative analysis given the heterogeneity of several variables.
RESULTS
Search Results
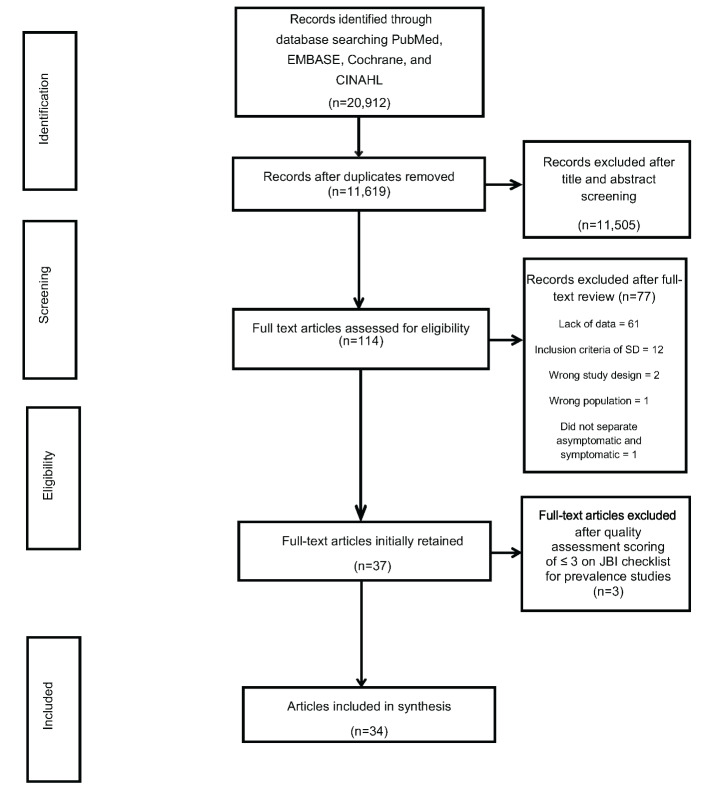
The initial search resulted in 11,619 after duplicates were removed. Following title and abstract screening 11,505 were removed. Full text articles were retrieved for the remaining 114 studies of which 77 were removed due to not meeting the inclusion criteria. The remaining 37 studies were retained for quality assessment Figure 1.
Figure 1. PRISMA flow diagram outlining study selection process.
Following quality assessment 34 articles were ultimately retained for analysis. Study characteristics for each of the 34 studies consisting that examined 2,365 individuals can be seen in Table 1. Retained studies were categorized into either symptomatic or asymptomatic within either an athletic population or a general orthopedic population.
Table 1. Characteristics for each of the retained studies.
| Authors | Setting Type | Population Type | Total Population/Shoulders (n/n) | With Scapular Dyskinesis (n) | Symptomatic (Y or N) | Methods |
| Akodu et al 2018 | General population (from Department of Physiotherapy, U of Lagos) | 77 undergraduates without history of shoulder or neck pathology | 77/77 (reported as individuals with SD) | 54 (a 1.5 cm asymmetry between R/L scapulae was considered the threshold for SD) | No | SICK scapula, Static Measurements 0 to 20 Point Rating Scale |
| Alves de Oliveira et al 2013 | Amateur Athletes | 30M amateur athletes (15 with SIS and 15 without); SIS mean age 22; control mean age 20.27 | 30/30 (dominant shoulders only) | SIS (14 (93.3%) present, 1 (6.7%) absent) Control (6 (40%) present, 9 (60%) absent) |
15 symptomatic 15 asymptomatic |
LSST |
| Balci et al 2016 | Outpatient clinic at a university | 53 subjects (40F/13M); diagnosed as unilateral AC (stage II) and SPN for at least 3 months | 53/53 (shoulder in pain) | 22 | Yes | LSST |
| Bullock et al 2021 | Wake Forest pitching lab | 33 asymptomatic M high school baseball pitchers; mean age 16.3 | 33/33 | 15 | No | McClure method (5 reps, etc.) |
| Camci et al 2013 | General population | 64 asymptomatic individuals | 64/64 (reported as individuals with SD) | 40 yes (24 no) | No | Yes/no method |
| Castelein et al 2016 | General F population | 19F with idiopathic neck pain; mean age 28.3 19F without (serving as control); mean age 29.3 |
38/38 (dominant shoulders only) | Neck pain group (9 yes, 10 no) Control group (8 yes, 11 no) |
19 symptomatic 19 asymptomatic |
Yes/no method described by Uhl et al. (visual observation) |
| Chen et al 2018 | General orthopedic with SPN | 186 (115F and 71M) individuals with shoulder conditions; mean age 45.74 SIS: 59, partial cuff tear: 6, FS: 23, bicep tendonitis: 15, GH OA: 13, cuff tendonitis: 10, SLAP tear: 10 |
186/186 (reported as individual, not shoulder) | Yes: 140 (type I, II, III) No: 46 (type IV) |
Yes (all) | Kibler method |
| Christiansen et al 2017 | Rehabilitation units, physical therapy clinics, and hospital setting | 40 patients (27M and 13F) with SIS | 40/40 (reported as individual with SD) | 18 | Yes (SIS) | McClure method (5 reps, etc.) |
| Da Silva et al 2008 | Elite tennis players and controls (compare SD and subacromial space in tennis players) | 73 individuals (53 elite tennis players (31M and 22F) and 20 controls (9M and 11F)); tennis players mean age 14.8; control mean age 14.6 | 73/73 (reported individuals but then also broke it down into bilateral and dominant %) | Tennis: 23/53 had SD (19 bilateral, 3 dominant, and 1 non dominant) Control: 4/20 had SD (2 dominant and 2 non dominant) |
No | Kibler method (static, dynamic and ascending, descending) |
| Deng et al, 2017 | Rehabilitation outpatient departments | 102 patients (49M and 53F) with shoulder conditions (SIS: 28, cuff tear: 27, SLAP: 16, OA:15, FS: 8, bicipital tendonitis: 8) | 102/102 (reported as individuals with SD) | Rest (type I-III): 83 Anterflexion (type I-III): 37 Scaption (type I-III): 39 Abduction (type I-III): 36 |
Yes | Kibler method |
| Frizziero et al 2018 | Bowed string instrument students at conservatory | 32 individuals (27F and 5M) | 32/32 (reported as individuals with SD) | 15 | No | Flexion and abduction with 1 or 2 kg weight and videotaped. Scapular movement was classified as: normal (both tests were evaluated as normal, or one movement is evaluated as normal and the other as slightly abnormal); slightly abnormal (both movements are evaluated as slight or uncertain abnormality); abnormal (one of the two movements is evaluated as severe abnormality) |
| Hannah et al 2017 | Strength profiles in healthy individuals with and without SD | 40 healthy college aged participants (12M and 28F) *initial before age matched brought in to even SD numbers; mean age 22.2 | 40/40 (individuals with SD) | 27 of 40 | No | Yes/no method |
| Huang et al 2015 | Outpatient clinic at a university hospital | 60 patients (4 M and 15F) with unilateral shoulder condition | 50/60 for raising phase 41/60 for lower phase (reported as individuals with SD and agreement levels) |
Raising phase 6 of 50 had SD Lowering phase 29 of 41 had SD |
Yes | Kibler and McClure combined method |
| Johansson et al 2016 | Pain in flatwater kayakers and relationship to ROM and SD | 31 kayakers (20M and 11F) (17 with SPN and 14 without SPN); F mean age 16.6; M mean age 18.2 | 31/31 (reported as individuals with SD) | Pain: 15/17 had SD No Pain: 4/14 had SD Total: 19/31 had SD |
Yes and No | Kibler and Sciasca method |
| Kawasaki et al 2012 | Does SD effect Rugby players during a season | 103M rugby players; mean age 24.6 | 103/103 used for primary analysis | Type I: 6 Type II: 4 Type III: 23 Total Yes: 33 Type IV (No): 70 |
No | Kibler method Type I-IV |
| Lee et al 2017 | Findings in asymptomatic elite volleyball players | 26 elite indoor volleyball players | 26/26 (dominant asymptomatic shoulders utilized) | 7 | No | Visual examination |
| Madsen et al 2011 | Training and SD in competitive swimmers | 78 competitive swimmers (44F and 34M); mean age 17 | 78/78 (athletes with SD) | After first time trial: 29 After half of training session: 53 Last three quarters of the training session: 57 Last quarter of the training session: 64 |
No | Yes/No system by McClure |
| Maor et al 2017 | SD among competitive swimmers | 20 competitive swimmers (6F and 14M); mean age 15.35 | 20/20 (athletes with SD) | Baseline: 6 1 hour of practice: 14 1.5 hours of practice: 17 |
No | Yes/No system by McClure |
| Moghadam et al 2018 | General orthopedic | 100F (47 hypermobile and 53 non-hypermobile) | 100/200 | Total (shoulders) Dominant Flexion: 60 Scaption: 62 Abduction: 61 Nondominant Flexion: 68 Scaption: 71 Abduction: 65 |
No (47 with GHJ generalized joint hypermobility but no symptoms) | Visual SD test |
| Nodehi et al 2020 | Acromiohumeral distance and SD comparison | 44F (21 with RSP and 23 controls); mean age of control 22.43; mean age of RSP 22.95 | 44/88 (looked at dominant vs non-dominant) | Total (shoulders) Flexion: 17 Abduction: 29 RSP: (flexion dominant: 4, non-dominant: 5; abduction dominant: 22, non-dominant: 4) Control: (flexion dominant: 3, non-dominant: 5; abduction dominant: 1, non-dominant: 2) |
No | Uhl yes/no method |
| Park et al, 2013 | Athletic population assessment of SD | 89 athletes (178 shoulders) (75 baseball players, 7 other overhead sports, 2 golf, and 5 occasional sport) SLAP: 15, SIS:12, SLAP + SIS: 6, MCL: 22, SLAP + MCL: 2, VEO: 9, cuff tear: 5, glenoid OCD: 4, capitellum OCD: 4, multidirectional instability: 5, posterior labral tear: 5 |
89/178 | Type I: 73 Type II: 39 Type III: 10 122: Total shoulders with SD out of 178 shoulders |
Yes | Type I-IV via visual observation |
| Park et al, 2014 | Athletic population evaluation of SD | 165 patients, 127 were baseball players, 5 were athletes of other over- head sports, 5 played golf, 2 played table tennis, 1 was a diver, 1 participated in bowling, 1 was an archer, and 26 enjoyed occasional sports activities. Elbow: MCL tear: 54, VEO: 40, OCD: 3, medial epicondylitis: 2, common flexor muscle strain: 3 Shoulder: SLAP: 49, multidirectional instability: 6, SLAP: 31, Bennett lesion: 3, internal impingement: 8, long head of biceps tendon tendonitis: 20, cuff tear: 3, impingement: 44, functional impingement: 8, sub coracoid impingement: 8, GIRD: 53, subscapularis tear: 1 |
165/330 | Type I: 130 Type II: 98 Type III: 52 280: Total shoulders with SD out of 330 |
Yes | Kibler’s 4 type method |
| Plummer et al 2017 | Observational SD | 135 individuals (67 with shoulder pain (33 F and 34 M) and 68 healthy controls (41 F and 27 M); pain mean age 32.5; control mean age 27.4 | 135/135 (individuals with SD) | Flexion (87/135) Symptomatic:45 Asymptomatic:42 Abduction (81/135) Symptomatic: 45 Asymptomatic:36 |
67 symptomatic 68 asymptomatic |
McClure Method |
| Rabin et al 2018 | Shoulder outpatient clinic | 74 consecutive patients referred to an outpatient shoulder surgery unit (6F/68M) | 74/74 (reported as individual) | 33 | Yes | Visual observation, Kibler method |
| Sahinoglu et al 2020 | Posterior shoulder tightness on SD | 121 college aged M (non-overhead athletes); mean age 21 | 121/242 (dominant and non-dominant shoulder) | Total-115 (dominant-56) (non-dominant-59) |
No | McClure yes/no method |
| Sant et al 2018 | SD in asymptomatic water polo players | 25M semi-professional water polo players; study group mean age 23.3; control mean age 23.1 | 25/25 (individuals with SD) | 23 | No | Kibler method Type I-IV |
| Seitz et al 2015 | Overhead athletes, comparing change in scapular kinematics between unweighted & maximal weighted contractions | 25 asymptomatic overhead athletes (swimming-5, volleyball-15, water polo-5); SD mean age 20.3; w/o SD mean age 20.5 | 25/25, dominant shoulder | 14 | No | SD test, visual observation |
| Shah et al 2016 | Musicians (guitar): presence of SD | 40 participants (20 guitar professional guitar players and 20 age matched non guitar players) |
40/40 (dominant shoulders only) | Asymmetrical (5 guitar players) (0 non guitar players) Dyskinetic (4 guitar players) (0 non guitar players) |
No | LSST at 0, 45, and 90 with and without weights |
| Silva et al 2018 | Musicians: presence of SD | 72 musicians (24M & 48F). Selected 36 symptomatic (cervical, shoulder or upper extremity pain in the last year with constant symptoms lasting more than 1 week) & 36 control; symptomatic mean age 23.28; control mean age 25.03 | 72/72 | Total - 35 (26 from symptomatic group, 9 from control group) |
36 | McClure and Tate method (Visually assessed participants by having them do five repetitions of bilateral, active, weighted shoulder flexion in the sagittal plane and bilateral, active, weighted shoulder abduction in the frontal plane) |
| Struyf et al 2014 | Amateur sports, evaluating risk factors for developing SPN | 113 recreational overhead athletes (59F & 54M), all aged>18 (tennis: 26, volleyball: 27, baseball: 5, badminton: 35, handball: 10); pain mean age 36.6; pain free mean age 33.2 | 113/113 | 62/113 demonstrated SD in dominant shoulder (33 winging & 29 forward tilting) | Baseline no pain 25/113 developed pain within 2 years |
Diagnosed by visual observation in 3 positions: static with both arms relaxed (thumbs facing forward), hands placed on ipsilateral hips (thumbs facing backward) and arms in 90° of humeral abduction in the frontal plane (thumbs facing up) |
| Tsuruike et al 2018 | Sport study (collegiate baseball) | 30M collegiate baseball players (13 pitchers) | 30/30 | 14 (Mild SD in 7 pitchers + 7 position players) | No | Kibler method |
| Welbeck et al 2019 | Link between thoracic rotation, SD, and pain among swimmers | 34 division I swimmers (13M and 21F); mean age 19.6; | 34/34 (as individuals, not shoulders) | Total: 15 (6 male and 9 female) | No | McClure yes/no method |
| Yesilyaprak et al | University research laboratory | 148 participants (58F/90M); no sporting activity or work with overhead movements | 148/296 | 87 (reported as individual shoulder: 87/296) | No | SDT |
| Yüksel et al 2014 | Reliability of SDT & LSST | 83 healthy participants (32F & 51M), mean age 21.74, have active full shoulder motion | 83/83 | SDT detected 44 (53%), LSST detected 30 (36%). Both detected 20 (24%) | No | SDT & LSST |
Abbreviations: AC; acromioclavicular, FS; frozen shoulder, GHJ; glenohumeral joint, GH OA; glenohumeral joint osteoarthritis, GIRD; glenohumeral internal rotation deficit, LSST; lateral scapular slide test, MCL; medial collateral ligament, OCD; osteochondritis dissecans, ROM; range of motion, ROTC; reserve officer training corps, RSP; rounded shoulder posture, SD; scapular dyskinesis, SDT; scapular dyskinesis test, SICK scapula; scapular malposition + inferior medial border prominence + coracoid pain and malposition + dyskinesis of scapular movement, SIS; shoulder impingement syndrome, SLAP; superior labrum anterior to posterior, VEO; valgus extension overload, M; Male, F; female, SPN; shoulder pain.
The general orthopedic population among the retained studies included study participants where the upper extremity was of interest, primarily the shoulder. However, there were a small number of individuals that had neck pain where SD was also evaluated, which is more clearly identified in the results section.
Methodological Quality
Of the 37 articles assessed three15–17 were excluded and 3412,18–50 were included for synthesis (Table 2).
Table 2. Joanna Briggs Institute critical appraisal checklist for studies reporting prevalence data.
| Authors | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Overall |
|---|---|---|---|---|---|---|---|---|---|---|
| Akodu et al 2018 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | I |
| Alibazi et al 2017 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | E |
| Alves de Oliveira et al 2013 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | I |
| Camci et al 2013 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | I |
| Castelein et al 2016 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | I |
| Chen et al 2015 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | E |
| Chen et al 2018 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | I |
| Christiansen et al 2017 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | I |
| Balci et al 2016 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | I |
| Bullock et al 2021 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | I |
| Da Silva et al 2008 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | I |
| Deng et al 2017 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | I |
| Frizziero et al 2018 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | I |
| Hannah et al 2017 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | I |
| Huang et al 2015 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | I |
| Johansson et al 2016 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | I |
| Kawasaki et al 2012 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | I |
| Lee et al 2017 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | I |
| Madsen et al 2011 | 1 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | I |
| Maor et al 2017 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | I |
| Moghadam et al 2018 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | I |
| Murty et al 2015 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | E |
| Nodehi Moghadam et al 2019 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | I |
| Park et al 2013 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | I |
| Park et al 2014 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | I |
| Plummer et al 2017 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | I |
| Rabin et al 2018 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | I |
| Sahinoglu et al 2020 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | I |
| Sant et al 2018 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | I |
| Seitz et al 2015 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | I |
| Shah et al 2016 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | I |
| Silva et al 2018 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | I |
| Struyf et al 2014 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | I |
| Tsuruike et al 2018 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | I |
| Welbeck et al 2019 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | I |
| Yesilyaprak et al 2016 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | I |
| Yüksel et al 2014 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | I |
1=Yes, 0=No, Unclear, or Not Applicable, I=Included, E=Excluded; 1. Was the sample frame appropriate to address the target population?; 2. Were study participants sampled in an appropriate way?; 3. Was the sample size adequate?; 4. Were the study subjects and the setting described in detail?; 5. Was the data analysis conducted with sufficient coverage of the identified sample?; 6. Were valid methods used for the identification of the condition?; 7. Was the condition measured in a standard, reliable way for all participants?; 8. Was there appropriate statistical analysis?; 9. Was the response rate adequate, and if not, was the low response rate managed appropriately?
The excluded articles all had a score ≤ 3 on the JBI tool. The reasoning for exclusion of articles was to remove poor quality studies due to low quality or high risk of bias. Otherwise, there would be little value in scoring quality if high- and low-quality studies are all given the same “voice”. Additionally, the JBI tool is specifically designed to give the raters the choice of including or excluding the scored study based on their interpretation of the scoring. Of the included studies, 1812,21–27,32,37–41,44,45,49,50 addressed the target population appropriately with the sample frame and had adequate sample sizes. However, only 13 studies12,19,23,24,26,28,31,32,41,42,47,49,50 reported both the study subjects and setting in detail. Additionally, 11 studies19,20,22–24,26,27,38,45,47,50 measured the condition in a standard reliable way, 15 studies12,19,22,23,26,30,32,34–36,40–42,48,50 used valid methods to identify the condition, and 8 studies21,22,32,37,39,41,48,50 included information on response rate as most studies were one-time measures. The JBI tool, like other quality and risk of bias assessment tools, does not advocate for a summative score as the constructs being scored are not similar. Therefore, in order to be as transparent as possible, we listed each item in the table along with their score, as well as provided a summary of those studies and which were the most common items not reported as you mention above.
Prevalence Results
The number of studies with available data for the asymptomatic and symptomatic populations and relevant subgroups are reported. Table 3 reflects studies with available subgroup data for asymptomatic and symptomatic populations. Data for asymptomatic individuals are reported in Table 4. Finally, symptomatic athletic population results are reported in Table 5 while the asymptomatic general population results ae reported in Table 6.
Table 3. Studies with available subgroup data for both asymptomatic and symptomatic populations.
| SYMPTOMATIC - Individuals (counted SD for an individual) | ||||||
|---|---|---|---|---|---|---|
| Athletic/Musicians | Study | Individuals (n) | With Scapular Dyskinesis (n) | Percentage | Without Scapular Dyskinesis (n) | Percentage |
| Alves de Oliveira et al 2013 | 15 | 14 | 93% | 1 | 7% | |
| Johansson et al 2016 | 17 | 15 | 88% | 2 | 12% | |
| Sliva et al 2018 | 36 | 26 | 72% | 10 | 28% | |
| Total | 68 | 55 | 81% | 13 | 19% | |
| General Orthopedic Population | Study | Individuals (n) | With Scapular Dyskinesis (n) | Percentage | Without Scapular Dyskinesis (n) | Percentage |
| Balci et al 2016 | 53 | 22 | 42% | 31 | 58% | |
| Castelein et al 2016 | 19 | 9 | 47% | 10 | 53% | |
| Chen et al 2018 | 186 | 140 | 75% | 46 | 25% | |
| Christiansen et al 2017 | 40 | 18 | 45% | 22 | 55% | |
| Deng et al 2017 | 102 | 37 | 36% | 65 | 64% | |
| Huang et al 2015 | 41 | 29 | 71% | 12 | 29% | |
| Plummer et al 2017 | 67 | 45 | 67% | 22 | 33% | |
| Rabin et al 2018 | 74 | 33 | 45% | 41 | 55% | |
| Total | 582 | 333 | 57% | 249 | 43% | |
| Symptomatic Total | Individuals (n) | With Scapular Dyskinesis (n) | Percentage | Without Scapular Dyskinesis (n) | Percentage | |
| 650 | 388 | 60% | 262 | 40% | ||
Table 4. Asymptomatic Individuals (counted SD for an individual).
| ASYMPTOMATIC - Individuals (counted SD for an individual) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Athletic / Musicians | Study | Individuals (n) | With Scapular Dyskinesis (n) | Percentage | Without Scapular Dyskinesis (n) | Percentage | |||
| Alves de Oliveira et al 2013 | 15 | 6 | 40% | 9 | 60% | ||||
| Bullock et al 2021 | 33 | 15 | 45% | 18 | 55% | ||||
| Da Silva et al 2008 | 53 | 23 | 43% | 30 | 57% | ||||
| Frizziero et al 2018 | 32 | 15 | 47% | 17 | 53% | ||||
| Johansson et al 2016 | 14 | 4 | 29% | 10 | 71% | ||||
| Kawasaki et al 2012 | 103 | 33 | 32% | 70 | 68% | ||||
| Lee et al 2017 | 26 | 7 | 27% | 19 | 73% | ||||
| Madsen et al 2011 | 78 | 29 | 37% | 49 | 63% | ||||
| Maor et al 2017 | 20 | 6 | 30% | 14 | 70% | ||||
| Sant et al 2018 | 25 | 23 | 92% | 2 | 8% | ||||
| Seitz et al 2015 | 25 | 14 | 56% | 11 | 44% | ||||
| Shah et al 2016 | 20 | 4 | 20% | 16 | 80% | ||||
| Silva et al 2018 | 36 | 9 | 25% | 27 | 75% | ||||
| Struyf et al 2014 | 113 | 62 | 55% | 51 | 45% | ||||
| Tsuruike et al 2018 | 30 | 14 | 47% | 16 | 53% | ||||
| Wellbeck et al 2019 | 34 | 15 | 44% | 19 | 56% | ||||
| Total | 657 | 279 | 42% | 378 | 58% | ||||
| General Population | Study | Individuals (n) | With Scapular Dyskinesis (n) | Percentage | Without Scapular Dyskinesis (n) | Percentage | |||
| Akodu et al 2018 | 77 | 54 | 70% | 23 | 30% | ||||
| Camci et al 2013 | 64 | 40 | 63% | 24 | 37% | ||||
| Castelein et al 2016 | 19 | 8 | 42% | 11 | 58% | ||||
| Da Silva et al 2008 | 20 | 4 | 20% | 16 | 80% | ||||
| Hannah et al 2017 | 40 | 27 | 68% | 13 | 32% | ||||
| Plummer et al 2017 | 68 | 42 | 62% | 26 | 38% | ||||
| Shah et al 2016 | 20 | 0 | 0% | 20 | 100% | ||||
| Yüksel et al 2014 | 83 | 54 | 65% | 29 | 35% | ||||
| Total | 391 | 229 | 59% | 162 | 41% | ||||
| Asymptomatic Total | Individuals (n) | With Scapular Dyskinesis (n) | Percentage | Without Scapular Dyskinesis (n) | Percentage | ||||
| 1048 | 508 | 48% | 540 | 52% | |||||
Table 5. Athletic Population - Symptomatic.
| Study | Shoulders (n) | With Scapular Dyskinesis (n) | Percentage | Without Scapular Dyskinesis (n) | Percentage | Shoulders (n) |
|---|---|---|---|---|---|---|
| Park et al 2013 | 178 | 122 | 69% | 56 | 31% | 178 |
| Park et al 2014 | 330 | 280 | 85% | 50 | 15% | 330 |
| Total | 508 | 402 | 79% | 106 | 21% | 508 |
*Shoulders (counted SD for each shoulder)
Table 6. General Population – Asymptomatic.
| Study | Shoulders (n) | With Scapular Dyskinesis (n) | Percentage | Without Scapular Dyskinesis (n) | Percentage |
|---|---|---|---|---|---|
| Moghadam et al 2018 | 200 | 128 | 64% | 72 | 36% |
| Nodehi et al 2020 | 88 | 17 | 19% | 71 | 81% |
| Sahinoglu et al 2020 | 242 | 115 | 48% | 127 | 52% |
| Yesilyaprak et al | 296 | 87 | 29% | 209 | 71% |
| Total | 826 | 347 | 42% | 479 | 58% |
*Shoulders (counted SD for each shoulder)
Although the inclusion criteria were intentionally broad in respect to diagnoses for the symptomatic population, all but three studies20,35,40 consisted of individuals with some form of shoulder pain including diagnoses such impingement, instability, rotator cuff tear, labral tear, and upper extremity pain, all of which are listed in Table 1. Two of the three studies35,40 consisted of mixed upper extremity diagnoses but the SD data was not parsed out by diagnosis. The authors were able to examine them based on the inclusion criteria. This was an attempt to be transparent in instances were other diagnosis outside of shoulder conditions may have been considered as we were examining those studies that identify SD but could have been in a population of individuals with cervical or upper extremity conditions. The remaining study20 included individuals with neck pain only with a total number of 19 subjects. Within the studies for the symptomatic athletic and general orthopedic population there were 81% and 57% individuals with SD, respectively, and a total of 60% among both groups. The two studies within symptomatic athletic population that looked at both shoulders individually demonstrated a total of 79% of individuals with SD considering at least one shoulder. Within the studies for the asymptomatic athletic and general population there were 42% and 59% individuals with SD, respectively, and a total of 48% among both. The four studies within asymptomatic general population that looked at both shoulders individually there was a total of 42% of individuals with SD.
DISCUSSION
The purpose of this systematic review was to examine the available literature in order to report the prevalence of SD among both the symptomatic and asymptomatic population. The results of this systematic review indicate that there is an overall presence of SD of 60% among symptomatic individuals. Among the asymptomatic population there is an overall presence of SD of 48% among those studies that identify individuals with SD. The low number of studies that identified individuals with SD per shoulder makes it difficult to determine true differences between those with and without symptoms. Despite the overall prevalence of SD being higher among those with symptoms compared to those without, there is still a considerable number of those that present with SD (nearly half of those studied) that are asymptomatic which questions the relevance of this finding. Furthermore, the total number of symptomatic individuals, 650, within studies investigating SD was just over half the number of those studies investigating SD among asymptomatic individuals, 1,048. This was reported for transparency in how the data were presented.
When considering the population of those with general shoulder pain there were a total of 582 individuals within the studies examined in this review. Among this population there was a higher percentage of individuals with SD (57%) compared to those without (43%). However, whether SD is contributing to the symptoms experienced by this populations remains unclear. If SD is a contributing factor to the symptoms among the general orthopedic population with shoulder pain, then how is the high prevalence (57%) of SD among the general population studied without symptoms explained?
There is considerable discussion in the literature regarding the presence of SD among overhead athletes with or without symptoms, as well as the presence of SD being a potential risk factor for sustaining injury in the future.8,9,31,32,37 The current findings from the current study support the high incidence of SD among athletes with shoulder symptoms. However, it is important to note that only three studies with a total of 68 individuals investigated the presence of SD within the symptomatic athlete population while 16 studies with a total of 657 individuals investigating the presence of SD in the asymptomatic athletic population were included. Given the larger number of asymptomatic athletes who were described as having SD (from 20%-92%) it is clear that a large number of athletes present with SD and have no symptoms. This may indicate that it is a possibility that SD may be a normal adaptation for those participating in overhead sports.
Additionally, the timing of measuring SD is not consistently reported among the studies that contain overhead athletes and may add further evidence that SD is a normal adaptation within this population. Two studies31,32 measured SD of asymptomatic competitive swimmers at various points of an individual training session. Both studies found that as training progressed, the number of individuals presenting with SD increased with a large number of participants presenting with SD at the end of the training session (82%31 and 85%32). At first glance the initial perception may be that these results are suggestive of weakness or some compensatory mechanism that requires attention, however, it is possible that there is a normal adaptation related to the overall shoulder complex that causes this change to occur, particularly since these athletes were all competing at a high level without symptoms. This would not be unlike what is known regarding the increase in external rotation range of motion at the glenohumeral joint within a single game and over the course of the season in a baseball pitcher.51 Within baseball pitchers this adaptation is not only normal, but necessary to perform at a high level.
Limitations
There are several limitations to this systematic review. The first limitation is that only included studies published in the English language were included which may have excluded published studies on this topic. Additionally, a very strict inclusion and exclusion criteria was applied in order to identify those studies that would provide the appropriate data for the purpose of this study. Lastly, there is a lack of consistency among how SD is measured across studies as well as populations, so it was not possible to perform a meta-analysis.
CONCLUSION
Within the symptomatic population, athletes have a higher percentage SD than the general orthopedic population. However, there are a considerable number of individuals with symptoms that do not present with SD. Perhaps more revealing is the number of asymptomatic individuals that present with SD, suggesting that SD may be a relatively normal finding among nearly half of the asymptomatic population studied within the literature. Until longitudinal studies are completed that monitor the predictive value of SD over time amongst asymptomatic populations, the relevance of this finding will remain uncertain.
Conflict of interest declaration
The authors declare no conflict of interest.
Supplemental File B.
Supplemental File A.
Acknowledgments
Acknowledgements
Melinda Johnson, Reference/Academic Support Services Librarian, Nova Southeastern University and Zachary Smith
References
- Luime JJ, Koes BW, Hendriksen IJM, et al. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol. 2004;33(2):73-81. doi:10.1080/03009740310004667 [DOI] [PubMed]
- Kibler WB, Ludewig PM, McClure PW, Michener LA, Bak K, Sciascia AD. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘scapular summit.’ Br J Sports Med. 2013;47(14):877-885. doi:10.1136/bjsports-2013-092425 [DOI] [PubMed]
- Kibler WB, Sciascia A. Current concepts: scapular dyskinesis. Br J Sports Med. 2010;44(5):300-305. doi:10.1136/bjsm.2009.058834 [DOI] [PubMed]
- Ratcliffe E, Pickering S, McLean S, Lewis J. Is there a relationship between subacromial impingement syndrome and scapular orientation? A systematic review. Br J Sports Med. 2014;48(16):1251-1256. [DOI] [PubMed]
- Timmons MK, Thigpen CA, Seitz AL, Karduna AR, Arnold BL, Michener LA. Scapular kinematics and subacromial-impingement syndrome: a meta-analysis. J Sport Rehabil. 2012;21(4):354-370. doi:10.1123/jsr.21.4.354 [DOI] [PubMed]
- Tate AR, McClure P, Kareha S, Irwin D, Barbe MF. A clinical method for identifying scapular dyskinesis, part 2: validity. J Athl Train. 2009;44(2):165-173. doi:10.4085/1062-6050-44.2.165 [DOI] [PMC free article] [PubMed]
- McClure P, Tate AR, Kareha S, Irwin D, Zlupko E. A clinical method for identifying scapular dyskinesis, part 1: reliability. J Athl Train. 2009;44(2):160-164. doi:10.4085/1062-6050-44.2.160 [DOI] [PMC free article] [PubMed]
- Hickey D, Solvig V, Cavalheri V, Harrold M, McKenna L. Scapular dyskinesis increases the risk of future shoulder pain by 43% in asymptomatic athletes: a systematic review and meta-analysis. Br J Sports Med. 2018;52(2):102-110. doi:10.1136/bjsports-2017-097559 [DOI] [PubMed]
- Hogan C, Corbett JA, Ashton S, Perraton L, Frame R, Dakic J. Scapular dyskinesis Is not an isolated risk factor for shoulder injury in athletes: A systematic review and meta-analysis. Am J Sports Med. 2020;49(10):2843-2853. doi:10.1177/0363546520968508 [DOI] [PubMed]
- McQuade KJ, Borstad J, de Oliveira AS. Critical and Theoretical Perspective on Scapular Stabilization: What Does It Really Mean, and Are We on the Right Track? Phys Ther. 2016;96(8):1162-1169. doi:10.2522/ptj.20140230 [DOI] [PubMed]
- Willmore EG, Smith MJ. Scapular dyskinesia: evolution towards a systems-based approach. Shoulder Elbow. 2016;8(1):61-70. doi:10.1177/1758573215618857 [DOI] [PMC free article] [PubMed]
- Plummer HA, Sum JC, Pozzi F, Varghese R, Michener LA. Observational Scapular Dyskinesis: Known-Groups Validity in Patients With and Without Shoulder Pain. J Orthop Sports Phys Ther. 2017;47(8):530-537. doi:10.2519/jospt.2017.7268 [DOI] [PubMed]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264-269, w64. doi:10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed]
- Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J EvidBased Healthc. 2015;13(3):147-153. doi:10.1097/xeb.0000000000000054 [DOI] [PubMed]
- Alibazi RJ, Moghadam AN, Cools AM, Bakhshi E, Ahari AA. The effect of shoulder muscle fatigue on acromiohumeral distance and scapular dyskinesis in women with generalized joint hypermobility. J Appl Biomech. 2017;33(6):424-430. doi:10.1123/jab.2016-0056 [DOI] [PubMed]
- Murty S. Do stingers affect scapular kinematics in rugby players? New Zealand J Physiother. 2015;43(3):113-113.
- Chen BJ, Chen WY. Scapular motion and muscle activation in patients with subacromial impingement syndrome and scapular dyskinesis. Physiotherapy. 2015;101:e220-e221. doi:10.1016/j.physio.2015.03.390
- Alves de Oliveira VM, da Silva Paixão Batista L, Torres Pirauá AL, Rodarti Pitangui AC, Cappato de Araújo R. Electromyographic activity and scapular dyskenesia in athletes with and without shoulder impingement syndrome. Br J Kineanthropy Human Perf. 2013;15(2):193-203.
- Camci E, Duzgun I, Hayran M, Baltaci G, Karaduman A. The effect of muscular strength on scapular kinematics in asymptomatic shoulders with or without scapular dyskinesis. Ann Rheum Dis. 2013;72.
- Castelein B, Cools A, Parlevliet T, Cagnie B. Are chronic neck pain, scapular dyskinesis and altered scapulothoracic muscle activity interrelated?: A case-control study with surface and fine-wire EMG. J Electromyog Kinesiol. 2016;31:136-143. doi:10.1016/j.jelekin.2016.10.008 [DOI] [PubMed]
- Chen K, Deng S, Ma Y, Yao Y, Chen J, Zhang Y. A preliminary exploration of plain-film radiography in scapular dyskinesis evaluation. J Shoulder Elbow Surg. 2018;27(7):e210-e218. doi:10.1016/j.jse.2017.12.032 [DOI] [PubMed]
- Christiansen DH, Møller AD, Vestergaard JM, Mose S, Maribo T. The scapular dyskinesis test: Reliability, agreement, and predictive value in patients with subacromial impingement syndrome. J Hand Ther. 2017;30(2):208-213. doi:10.1016/j.jht.2017.04.002 [DOI] [PubMed]
- Da Silva RT, Hartmann LG, De Souza Laurino CF, Bilo JPR. Clinical and ultrasonographic correlation between scapular dyskinesia and subacromial space measurement among junior elite tennis players. J Arthroc Rel Surg. 2011;27(10):e113. [DOI] [PubMed]
- Deng S, Chen K, Ma Y, Chen J, Huang M. The Influence of Test Positions on Clinical Assessment for Scapular Dyskinesis. PM R. 2017;9(8):761-766. doi:10.1016/j.pmrj.2016.11.011 [DOI] [PubMed]
- Frizziero A, Gasparre G, Corvo S, et al. Posture and scapular dyskinesis in young bowed string instrumental musicians. Muscle Ligaments Tendons J. 2018;8(4):507-512. doi:10.32098/mltj.04.2018.08
- Hannah DC, Scibek JS, Carcia CR. Strength Profiles in Healthy Individuals with and without Scapular Dyskinesis. Int J Sports Phys Ther. 12(3):305-313. [PMC free article] [PubMed]
- Huang TS, Huang HY, Wang TG, Tsai YS, Lin JJ. Comprehensive classification test of scapular dyskinesis: A reliability study. Man Ther. 2015;20(3):427-432. doi:10.1016/j.math.2014.10.017 [DOI] [PubMed]
- Johansson A, Svantesson U, Tannerstedt J, Alricsson M. Prevalence of shoulder pain in Swedish flatwater kayakers and its relation to range of motion and scapula stability of the shoulder joint. J Sports Sci. 2016;34(10):951-958. doi:10.1080/02640414.2015.1080852 [DOI] [PubMed]
- Kawasaki T, Yamakawa J, Kaketa T, Kobayashi H, Kaneko K. Does scapular dyskinesis affect top rugby players during a game season? J Shoulder Elbow Surg. 2012;21(6):709-714. doi:10.1016/j.jse.2011.11.032 [DOI] [PubMed]
- Lee CS, Stetson WB, Goldhaber NH, Davis SM, Brock A, Wosmek J. Magnetic resonance imaging findings in asymptomatic elite volleyball players. J Arthro Relat Surg. 2017;33(10):e58-e59. doi:10.1016/j.arthro.2017.08.036
- Madsen PH, Bak K, Jensen S, Welter U. Training induces scapular dyskinesis in pain-free competitive swimmers: A reliability and observational study. Clin J Sports Med. 2011;21(2):109-113. doi:10.1097/jsm.0b013e3182041de0 [DOI] [PubMed]
- Maor MB, Ronin T, Kalichman L. Scapular dyskinesis among competitive swimmers. J Bodywk Movem Ther. 2017;21(3):633-636. doi:10.1016/j.jbmt.2016.11.011 [DOI] [PubMed]
- Nodehi Moghadam A, Sarabadani Tafreshi E, Abdollahi S, Bakhshi E. The comparison of acromiohumeral distance and scapular dyskinesis prevalence in females with and without rounded shoulder posture. Med J Islam Reb. 2020;34(19). doi:10.47176/mjiri.34.19 [DOI] [PMC free article] [PubMed]
- Park JY, Hwang JT, Kim KM, Makkar D, Moon SG, Han KJ. How to assess scapular dyskinesis precisely: 3-dimensional wing computer tomography-a new diagnostic modality. J Should Elbow Surg. 2013;22(8):1084-1091. doi:10.1016/j.jse.2012.10.046 [DOI] [PubMed]
- Park JY, Hwang JT, Oh KS, Kim SJ, Kim NR, Cha MJ. Revisit to scapular dyskinesis: Three-dimensional wing computed tomography in prone position. J Shoulder Elbow Surg. 2014;23(6):821-828. doi:10.1016/j.jse.2013.08.016 [DOI] [PubMed]
- Sahinoglu E, Karadibak D. Investigation of Posterior Shoulder Tightness on Scapular Dyskinesis. J Basic Clin Health Sci. 2020;4(3):237-242.
- Sant KN, Busuttil L, Salo A. Scapular dyskinesis in asymptomatic water polo players: does prehabilitation prevent negative outcomes? Int J Physiother. 2018;5(4):132-140. doi:10.15621/ijphy/2018/v5i4/175694
- Seitz AL, McClelland RI, Jones WJ, Jean RA, Kardouni JR. A comparison of change in 3d scapular kinematics with maximal contractions and force production with scapular muscle tests between asymptomatic overhead athletes with and without scapular dyskinesis. Int J Sports Phys Ther. 10(3):309-318. [PMC free article] [PubMed]
- Shah NA, Shimpi AP, Rairikar SA, Ashok S, Sancheti PK. Presence of scapular dysfunction in dominant shoulder of professional guitar players. Int J Occup Safety. 2016;22(3):422-425. doi:10.1080/10803548.2016.1154720 [DOI] [PubMed]
- Silva FM, Brismée JM, Sizer PS, Hooper TL, Robinson GE, Diamond AB. Musicians injuries: upper quarter motor control deficits in musicians with prolonged symptoms - a case-control study. Musculoskel Sci Pract. 2018;36:54-60. doi:10.1016/j.msksp.2018.04.006 [DOI] [PMC free article] [PubMed]
- Struyf F, Nijs J, Meeus M, et al. Does scapular positioning predict shoulder pain in recreational overhead athletes? Int J Sports Med. 2014;35(1):75-82. [DOI] [PubMed]
- Welbeck AN, Amilo NR, Le DT, et al. Examining the link between thoracic rotation and scapular dyskinesis and shoulder pain amongst college swimmers. Phys Ther Sport. 2019;40:78-84. doi:10.1016/j.ptsp.2019.08.013 [DOI] [PubMed]
- Yüksel E, Yeşilyaprak SS. Correlation between scapular Dyskinesis test and lateral scapular slide test in scapular assessment. Orthop J Sports Med. 2014;2(11):2325967114S0027. doi:10.1177/2325967114s00279
- Akodu AK, Akinbo SR, Young QO. Correlation among smartphone addiction, craniovertebral angle, scapular dyskinesis, and selected anthropometric variables in physiotherapy undergraduates. J Taibah Uni Med Sci. 2018;13(6):528-534. doi:10.1016/j.jtumed.2018.09.001 [DOI] [PMC free article] [PubMed]
- Balci NC, Yuruk ZO, Zeybek A, Gulsen M, Tekindal MA. Acute effect of scapular proprioceptive neuromuscular facilitation (PNF) techniques and classic exercises in adhesive capsulitis: a randomized controlled trial. J Phys Ther Sci. 2016;28(4):1219-1227. doi:10.1589/jpts.28.1219 [DOI] [PMC free article] [PubMed]
- Moghadam AN, Salimi MM, Bakhshi E. The relationship between scapular dyskinesis and generalized joint hypermobility in young women. Cres J Med Bio Sci. 2018;5(3):189-193.
- Rabin A, Chechik O, Dolkart O, Goldstein Y, Maman E. A positive scapular assistance test is equally present in various shoulder disorders but more commonly found among patients with scapular dyskinesis. Phys Ther Sport. 2018;34:129-135. doi:10.1016/j.ptsp.2018.09.008 [DOI] [PubMed]
- Tsuruike M, Ellenbecker TS, Hirose N. Kerlan-Jobe Orthopaedic Clinic (KJOC) score and scapular dyskinesis test in collegiate baseball players. J Shoulder Elbow Surg. 2018;27(10):1830-1836. doi:10.1016/j.jse.2018.06.033 [DOI] [PubMed]
- Yeşilyaprak SS, Yüksel E, Kalkan S. Influence of pectoralis minor and upper trapezius lengths on observable scapular dyskinesis. Phys Ther Sport. 2016;19:7-13. doi:10.1016/j.ptsp.2015.08.002 [DOI] [PubMed]
- Bullock GS, Strahm J, Hulburt TC, Beck EC, Waterman BR, Nicholson KF. Relationship between clinical scapular assessment and scapula resting position, shoulder strength, and baseball pitching kinematics and kinetics. Orthop J Sports Med. 2021;9(3):2325967121991146. [DOI] [PMC free article] [PubMed]
- Freehill MT, Archer KR, Diffenderfer BW, Ebel BG, Cosgarea AJ, McFarland EG. Changes in collegiate starting pitchers’ range of motion after single game and season. Phys Sportsmed. 2014;42(1):69-74. doi:10.3810/psm.2014.02.2049 [DOI] [PubMed]