Abstract
Introduction
Red Ear Syndrome (RES) is a condition often considered to be a localized form of erythromelalgia. It can be related to structural cervical defects or idiopathic. RES is generally very difficult to treat.
Discussion
A 57-year-old male presented to the dermatology clinic complaining of a 4-month history of intermittent redness and severe burning of bilateral ears. On examination, the patient exhibited edematous erythema and tenderness to palpation affecting the right and left ear and right malar cheek. A skin biopsy revealed mild superficial perivascular lymphocytic infiltrate with hypertrophy of endothelial cells. The patient was found to have a normal lab work-up including complete blood count, metabolic panel, erythrocyte sedimentation rate, anti-nuclear antibody and type II collagen antibody. A diagnosis of Red Ear Syndrome was made. After failing multiple medications over several months, the patient was started on aspirin and paroxetine which was gradually titrated until he was completely asymptomatic. To date, there is only one other case presentation illustrating the effectiveness of this treatment regimen.
Conclusion
There are a limited number of cases describing idiopathic RES with inconsistent results in treatment. With a relatively small number of cases reported, further research is needed into the pathophysiology of RES along with the dual therapy of aspirin and paroxetine in patients that suffer from both primary and secondary RES.
Keywords: red ear syndrome, pain/diagnosis, syndrome, erythema/physiopathology, ear diseases, erythromelalgia, paroxetine, aspirin
Case Presentation
A 57-year-old male presented to the dermatology clinic with a 4-month history of intermittent, severe redness and burning that started on his right ear and progressed to his right cheek and left ear. The episodes would last several hours but, in some cases, persisted for days. The redness and pain worsened with sun exposure and overheating. Conversely, cool weather and cold compresses seemed to alleviate his symptoms temporarily. The patient had already been established with an otolaryngologist for this issue and had failed prior therapies including gabapentin, pregabalin, imipramine, carbamazepine, brimonidine, amitriptyline, propranolol, labetalol and verapamil. The patient was notably frustrated given the impact this had on his physical and mental health.
Physical examination revealed significant erythema, swelling and pain with palpation of the right and left external ear and partial right malar cheek. (Figure 1) Given the patient’s insecurities with the redness, he was wearing makeup daily to cover this. Both earlobes were notably involved. On subsequent visits, the redness and pain began affecting bilateral hands.
Figure 1.
Erythema and swelling of the right external ear and right malar cheek observed after wiping away makeup.
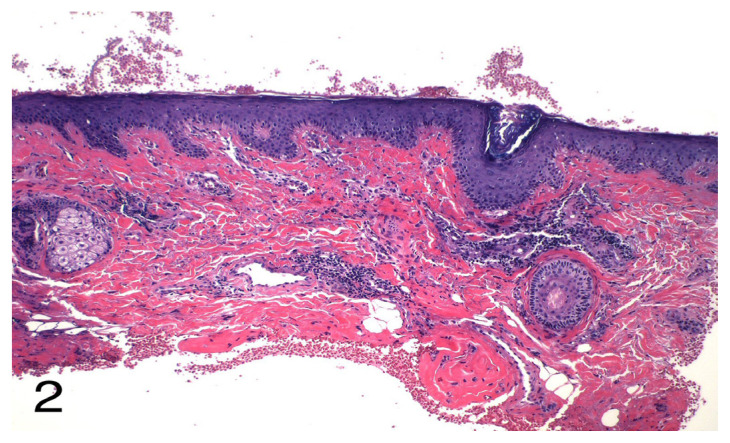
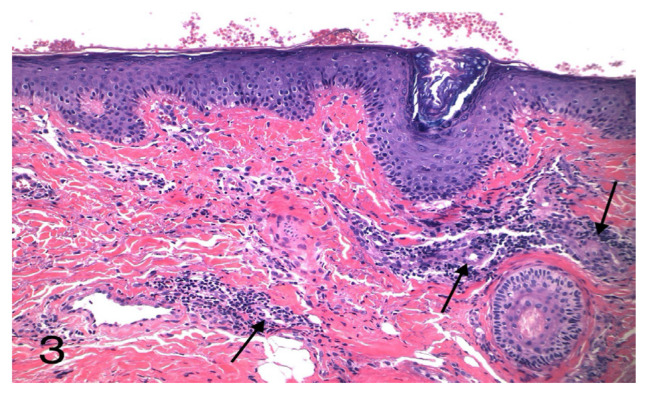
We first obtained punch biopsies from skin of the right posterior ear and right superior malar cheek, revealing mild superficial perivascular lymphocytic infiltrate with mild hypertrophy of endothelial cells. (Figures 2 and 3) The histology revealed no increase in mast cells. While the biopsy results were pending, a complete blood count, metabolic panel, erythrocyte sedimentation rate, anti-nuclear antibody and type II collagen antibody were obtained and found to be within normal limits. Based on the patient’s clinical, histologic and laboratory findings, a diagnosis of Red Ear Syndrome (RES) with erythromelalgia of the hands was made. Brain and cervical spine magnetic resonance imaging (MRI) were performed to look for structural neurologic defects, but only mild age-appropriate degenerative changes were observed at C4–5.
Figure 2.
Histopathology of Red Ear Syndrome. Punch biopsy revealed mild superficial perivascular lymphocytic infiltrate and hypertrophy of endothelial cells. (H&E, original magnification x10)
Figure 3.
Histopathology of Red Ear Syndrome. Punch biopsy revealed mild superficial perivascular lymphocytic infiltrate and hypertrophy of endothelial cells (Arrows). (H&E, original magnification x20)
Additional therapies based on prior case reports were attempted including topical anesthetics, aspirin, indomethacin, duloxetine, mexiletine and nerve blocks, which only provided minimal relief. After months of poor therapeutic response, the patient was referred to neurosurgery, but further medical treatment was recommended before any surgical intervention.
Almost one year after the patient first developed symptoms and multiple treatment regimens, he was started on paroxetine 10 mg, while continuing aspirin 325 mg twice daily. The dose of paroxetine was gradually increased up to 80 mg daily over the course of three months until the patient’s symptoms resolved.
Discussion
RES is a rare condition that is characterized by episodic erythema of the ear accompanied by a burning sensation or otalgia. Both ears, or more commonly one ear, may be affected, and the syndrome can extend to the face. Symptoms can be spontaneous or triggered by touch, exertion, heat or cold, stress and even dietary triggers.1, 2 RES has a predilection for females with a mean age of affliction of 40.2 years.3 Only 47 cases of men suffering from RES had been reported prior to a 2013 study.4
RES was first described by Lance in 1994 as a neurological syndrome presenting with flushing, tightness and pain in one ear lobe.5 He later distinguished between primary (either isolated or associated with headache attacks) and secondary cases.6 Primary RES is an idiopathic form that more commonly occurs in adolescents and is typically associated with headaches or migraines. This type is less likely to be triggered by stimulation.3 The secondary form more frequently affects adults and has been attributed to a wide range of illnesses including cervical spondylosis, traction injury of upper cervical roots, atypical glossopharyngeal/trigeminal neuralgias, TMJ dysfunction and thalamic syndrome.5, 7–10
Diagnostic criteria have been proposed for RES by Lambru.4 Criteria require at least 20 attacks of ear pain accompanied by redness lasting up to four hours. These attacks generally occur more than once daily and have at least two of the following characteristics: burning pain, unilateral, mild to moderate severity and triggering by cutaneous or thermal stimulation of the ear.4, 10 The pathophysiology of RES is unclear, but many theories have been postulated. In the case of secondary RES, irritation of the C3 nerve root has been suggested.5 This nerve innervates the skin of the ear causing a pain sensation through the release of vasodilating substances. A central mechanism has also been proposed, regarding the connection between the trigeminal nerve and facial parasympathetic outflow, especially for those patients that experience migraines.10, 11 Lastly, local damage to small nerve fibers and vessels as seen in erythromelalgia has been a possible explanation.8, 10 One of the most common conditions included in the differential of RES is erythromelalgia, which is a rare autosomal dominant neuropathy, characterized by a combination of recurrent burning pain, warmth and redness of the hands and feet. Pain and redness are usually bilateral. Patients have reported involvement of the face but there is controversy over the possibility that this denotes a unique pain syndrome rather than RES itself.12–14 RES is commonly considered an auricular version of erythromelalgia.15 Histology is similar between the two conditions with both showing perivascular lymphocytic inflammation, perivascular edema and arteriolar smooth muscle hyperplasia.13 RES can clinically be distinguished from its erythromelalgia counterpart by the classic presentation affecting solely the external ear.
Due to the association of secondary RES with upper cervical spine pathology, an MRI of the cervical spine should be carried out when RES is suspected. In addition, if TMJ dysfunction is a possibility, an orthodontic assessment is warranted. Lastly, an MRI scan of the brain should be included to rule out thalamic lesions.4 If skin involvement is more generalized, a complete blood count and thermograph should be completed to rule out other secondary causes.16 RES is generally considered refractory to treatment and most cases show multiple trials of medications with little to no relief. Medications that have been shown to be at least partially effective for primary RES include gabapentin, amitriptyline, paroxetine, indomethacin, ibuprofen, aspirin, flunarizine, nimodipine, pregabalin and a greater auricular nerve blockade.3, 4 Secondary RES has also been effectively treated with gabapentin, amitriptyline, imipramine, verapamil, propranolol and methysergide.4 In general, nonsteroidal anti-inflammatory drugs have been used first line due to the association with headaches and to exclude a nonsteroidal anti-inflammatory drug-sensitive headache disorder.17 Complementary and alternative treatments like acupuncture have also been utilized for refractory cases, however, there is a lack of evidence supporting its efficacy.4
Conclusion
In this report, we present a rare case of primary RES in a 57-year-old male and provide a discussion of its medical associations, along with a potential successful treatment option. No secondary causes were found on imaging or lab workup for our patient, making this a unique case to examine. There are a limited number of cases describing idiopathic RES with inconsistent results in treatment. After months of refractory therapy, our patient saw vast improvements after starting a regimen of aspirin and paroxetine and continues to be free of all symptoms 12 months later. With a relatively small number of cases reported, further research is needed into the pathophysiology of RES along with the dual therapy of aspirin and paroxetine in patients that suffer from both primary and secondary RES.
Acknowledgements
The patient has provided permission to publish these features of his case.
Funding Statement
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity.
Footnotes
Conflicts of Interest
The authors declare they have no conflicts of interest.
Drs. Brackenrich and Sternad are employees of LewisGale Hospital - Montgomery, a hospital affiliated with the journal’s publisher.
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
References
- 1. Chan CC, Ghosh S. Red ear syndrome precipitated by a dietary trigger: a case report. J Med Case Rep. 2014;8:338. doi: 10.1186/1752-1947-8-338. Published 2014 Oct 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Raieli V, Monastero R, Santangelo G, Eliseo GL, Eliseo M, Camarda R. Red ear syndrome and migraine: report of eight cases. Headache. 2002;42(2):147–151. doi: 10.1046/j.1526-4610.2002.02033.x. [DOI] [PubMed] [Google Scholar]
- 3. Chen MC, Xu QF, Luo DQ, Li X, He DY. Erythema associated with pain and warmth on face and ears: a variant of erythermalgia or red ear syndrome? J Headache Pain. 2014;15(1):18. doi: 10.1186/1129-2377-15-18. Published 2014 Mar 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lambru G, Miller S, Matharu MS. The red ear syndrome. J Headache Pain. 2013;14(1):83. doi: 10.1186/1129-2377-14-83. Published 2013 Oct 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lance JW. The mystery of one red ear. Clin Exp Neurol. 1994;31:13–18. [PubMed] [Google Scholar]
- 6. Lance JW. The red ear syndrome. Neurology. 1996;47(3):617–620. doi: 10.1212/WNL.47.3.617. [DOI] [PubMed] [Google Scholar]
- 7. Kalladka D, Paul M, Tyagi A. Teaching NeuroImages: Red ear syndrome. Neurology. 2016;86(16):e177–e178. doi: 10.1212/WNL.0000000000002588. [DOI] [PubMed] [Google Scholar]
- 8. Chan TLH, Becker WJ, Jog M. Indomethacin-Responsive Idiopathic Red Ear Syndrome: Case Report and Pathophysiology. Headache. 2018;58(2):306–308. doi: 10.1111/head.13237. [DOI] [PubMed] [Google Scholar]
- 9. Raieli V, Compagno A, D’Amelio M. Red Ear Syndrome. Curr Pain Headache Rep. 2016;20(3):19. doi: 10.1007/s11916-016-0547-y. [DOI] [PubMed] [Google Scholar]
- 10. Purdy RA, Dodick DW. Red ear syndrome. Curr Pain Headache Rep. 2007;11(4):313–316. doi: 10.1007/s11916-007-0210-8. [DOI] [PubMed] [Google Scholar]
- 11. Coleman J, Ream MA. A Boy With Red Ears. Semin Pediatr Neurol. 2018;26:92–93. doi: 10.1016/j.spen.2017.03.015. [DOI] [PubMed] [Google Scholar]
- 12. Davis MDP. Facial erythromelalgia? J Am Acad Dermatol. 2018;78(5):e127. doi: 10.1016/j.jaad.2017.10.056. [DOI] [PubMed] [Google Scholar]
- 13. Tang Z, Chen Z, Tang B, Jiang H. Primary erythromelalgia: a review. Orphanet J Rare Dis. 2015;10:127. doi: 10.1186/s13023-015-0347-1. Published 2015 Sep 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Grandy K, Corsten G, Hong P. Pediatric-isolated auricular erythromelalgia: a case report. Case Rep Pediatr. 2012;2012:854081. doi: 10.1155/2012/854081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Purdy RA. Red Ear Syndrome or Red Ear Symptom/Sign? Headache. 2018;58(6):792–794. doi: 10.1111/head.13335. [DOI] [PubMed] [Google Scholar]
- 16. Kang BC, Nam DJ, Ahn EK, Yoon DM, Cho JG. Secondary erythromelalgia - a case report. Korean J Pain. 2013;26(3):299–302. doi: 10.3344/kjp.2013.26.3.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. de Amorim IL, Kauppila LA, Martins IP. Red Ear: Syndrome or Symptom? Headache. 2018;58(6):885–891. doi: 10.1111/head.13333. [DOI] [PubMed] [Google Scholar]