Abstract
Description
Low back pain (LBP) is frequently encountered in outpatient clinics and affects individual patients and society in general with decreased physical function, quality of life, disability, and/or economic burden. Although most acute LBP resolves on its own, recurrent and chronic LBP is a common reason for outpatient clinic visits. This review explores pragmatic approaches to LBP in the clinical setting, focusing on recognizing prognostic factors, initial approaches to evaluation, including selective imaging, and conservative management including patient education, therapeutic exercises and bracing.
Keywords: low back pain, low back pain/therapy, conservative management, pragmatic approach, therapeutic exercise, therapeutics, exercise therapy, chronic pain, acute pain
Introduction
Low back pain (LBP) is very common, affecting up to 80% (14–85% depending on definition) of the population during their lifetime in the Western world.1 It remains one of the most common reasons for a physician visit in developed countries.2 In general, the peak incidence of LBP occurs in the third decade, and overall prevalence increases until 60–65 years of age, without specific gender preference.3 LBP also has substantial societal implications. It is the most common cause of work-related disability in those younger than 45 years of age and the economic burden of LBP in the United States ranges from 84.1 billion to 624.8 billion USD, with lost work productivity being the primary driver.4 In 2010, it was the second most common cause of adult disability after arthritis and rheumatism.5 Chronic low back pain (CLBP) affects quality of life adversely in physical function, sleep and psychological well-being including mood and self-perception.6
LBP management has been extensively studied considering the aforementioned impacts on the individual patient and the community. However, there is still a gap between this information and its applications in clinical practice, particularly in the area of detailing conservative (non-invasive) management. As surgeries and interventional therapies are not recommended in most patients with acute LBP and limited in their role in most CLBP, it is important for primary care physicians (PCPs) to know the details of non-invasive treatment.7 In this article, we will explore a pragmatic approach to both acute and chronic LBP management with a focus on non-invasive management from the perspective of a PCP.8
Initial Evaluation: History, Physical Examination, Assessment, Classification and Prognostic Indicators
The low back is typically defined as the area between the lower rib margins and the buttock creases, and LBP arises from a variety of heterogenous pathologies in this region. The location, quality/characteristics, intensity and duration of pain, preceding event or trauma, aggravating or relieving factors and associated symptoms, and medical/surgical histories should be obtained at the initial evaluation. Red flags, defined as clinical features believed to increase the risk of a serious disease, can be identified in either the history of present illness or in the past medical history.9 The list of symptoms to look for in the history is extensive, including significant trauma, pain increased or unrelieved by rest, pain that worsens at night, unexplained weight loss, fever, associated neurological deficits, bowel or bladder incontinence and/or urinary retention. Conditions associated with these red flags include cancer, immunosuppressive states (e.g., prolonged steroid use), intravenous drug use, recent urinary tract infection, inflammatory arthritis, osteoporosis and/or recent surgery.10
In addition to red flags, PCPs can evaluate yellow flags, defined as psychological factors and maladaptive pain coping behaviors, such as fear avoidance and catastrophizing (negative thoughts, statements about the future). Other yellow flags include low mood, job dissatisfaction and ongoing litigation.11 Knowledge of yellow flags during the evaluation can be important in the early engagement of psychological and behavioral interventions such as cognitive behavioral therapy (CBT) and mindfulness.12 Presence of yellow flags can be related to prolonged or delayed recovery. Conversely, low levels of fear avoidance and low baseline functional impairment are associated with favorable recovery.13
Pain intensity and accompanying pain in the leg or at multiple body sites were identified as predictors of disabling CLBP.9 In addition, pain intensity measured by a numeric rating scale from 0 to 10 or visual analogue scale on a 100 mm horizontal line can be useful for a baseline measure before any intervention. Reviewing functional level such as limitations in activities of daily living can be useful not only for prognostication, but also for follow up of the interval change. The Oswestry Disability Index and the Roland-Morris Disability Questionnaire are widely available tools to evaluate functional limitations systematically. The Defense and Veterans Pain Rating Scale is a quick tool utilizing a numeric rating scale combined with easy functional descriptors.14
Neurological and musculoskeletal examination including motor, sensory, deep tendon reflexes of lower extremities, straight leg raise test and other provocative tests for facet joint, sacroiliac joint and hip joint pathologies can be useful in addition to inspection (skin, bony deformity, muscle atrophy, asymmetry, leg length and posture), range of motion and palpation of bony and soft tissue structures in the region. Information systemically acquired by history and physical examination can be helpful for the classification of these heterogenous conditions.
During physical examination, PCPs can also look for Waddell’s nonorganic signs. These are a group of physical examination findings made up of five physical signs, including the presence of superficial or nonanatomic tenderness, pain on axial loading or simulated rotation, non-reproducibility of pain when distracted, regional weakness or sensory change and overreaction. The presence of Waddell’s nonorganic signs account for functional impairment, general health status and the presence of psychiatric comorbidities (depression, anxiety, stress).13 Waddell’s signs represent exaggerated emotional and psychological symptoms and somatic over-reporting; therefore, the evaluation can be helpful in a risk assessment of developing CLBP and somatic symptom amplification.15
There are many classification systems available to categorize subgroups of LBP in order to optimize management and better communicate among the medical community. These systems can be divided into diagnostic classifications, prognostic classifications and treatment-based classifications. For diagnostic classification, the International Statistical Classification of Diseases (ICD)-Clinical Modification (CM) codes are widely used in clinical practice for billing purposes, and these diagnostic codes are often shared between the health care providers. The Quebec Task Force Classification system, a widely used diagnostic classification system in clinical research,16 is based on the patient’s symptoms and can aid the clinician to plan further work-up and management. For example, if there is no leg pain, a straight leg raise test may not be helpful. Centralized (localized) LBP without leg pain or sensory/motor deficits is less likely to require a formal evaluation of radiculopathy with electromyography (EMG).17 Based on the duration of symptoms, LBP can be classified into acute LBP being defined as less than 4 weeks, subacute between 4 to 12 weeks, and CLBP as more than 12 weeks, which is an important prognostic factor.18 LBP can also be diagnostically classified based on the location of pathologies or underlying etiologies. Patho-anatomical diagnosis can be used to classify LBP by pathologies in intervertebral discs, sacroiliac joints, facet joints, bone, muscle, ligament, nerve roots, plexus and individual nerves.19
Classification based on the presence of psychosocial factors is an example of prognostic classification; the presence of high levels of maladaptive pain coping behaviors, high baseline functional impairment, psychiatric comorbidities, low general health status and/or nonorganic signs is predictive of worse outcomes at 1 year after initial LBP.13,20 Interpreting the outcome of CLBP can be challenging, as there are a large number of different outcome measures and instruments used across the studies without a standardized approach.21
In addition, the utility of universal application of red flag screening in predicting adverse outcomes or poor prognosis has been debated.22 Although red flags do not necessarily justify advanced imaging or other costly tests, they can aid the clinician in preparing for an atypical course of LBP and help guide the decision-making process.
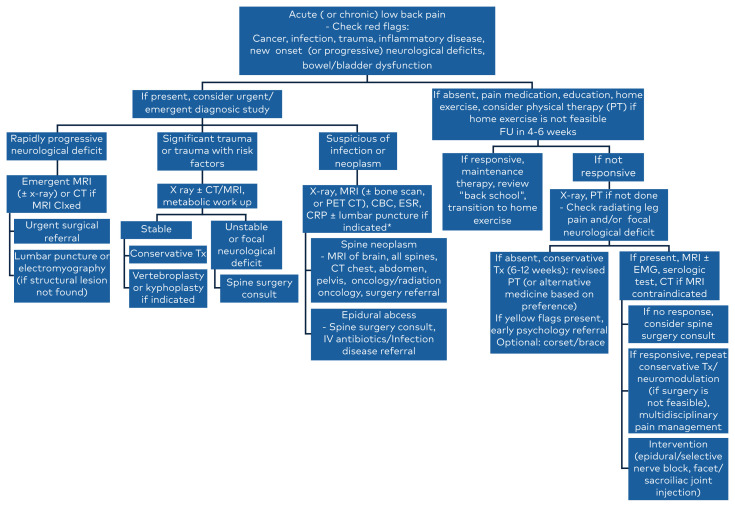
A working diagnosis based on history, physical examination and available objective data can help the clinician plan the best management and evaluate if the initial intervention would be effective on follow-up. If a serious pathology is suspected, early or immediate diagnostic imaging should be considered. (Figure 1) Imaging workup can include x-ray, computerized tomography (CT) scan and magnetic resonance imaging (MRI) depending on availability and structure of interest. For example, x-ray is useful for screening (flexion/extension view for dynamic instability), MRI for soft tissue pathologies including disc, nervous structures, intracortical bony pathologies and tissue changes, and lastly CT scan for bony details and subtle bony pathologies (or when MRI is not accessible).23 (Figure 1)
Figure 1.
Initial assessment and plan for low back pain based on symptoms and signs. Modified from Lee, S.W., Musculoskeletal Injuries and Conditions: Assessment and Management. 2017, NY, Demos Medical. *Lumbar puncture is contraindicated in suspected spinal epidural abscess, increased intracranial pressure and bleeding diathesis.
It is useful to be aware of proper imaging guidelines, for example, the Choosing Wisely® guidelines or American College of Radiology Appropriateness Criteria for low back pain.24 Early imaging without red flags or other risk factors for serious pathologies is discouraged because of higher frequency of incidental findings (e.g., disc degeneration in 37% to 96% of asymptomatic 20- to 80-year-old individuals), which may result in unnecessary interventions such as injections and surgeries.25
Management Based on Different Visits
This review approaches the management of LBP based on each visit to the physician and focuses on the frequently utilized nonoperative management by PCPs. We provide a practical and efficient approach for this common and costly problem.
Initial Visit
Management of Acute Low Back Pain Without Red Flags
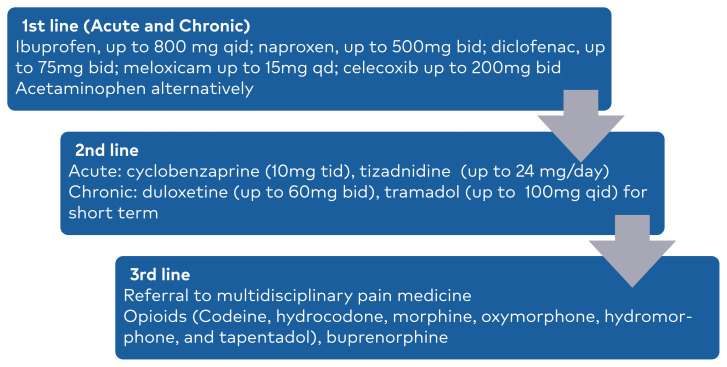
If a serious pathology is unlikely based on absence of red flags and clinical evaluation, education on the nature of pain, favorable course, self-management and continuing daily activities with minimal relative rest will be important for a favorable prognosis in patients with acute LBP, defined as less than 4 weeks of duration. Clinicians can focus on the symptomatic treatment of acute LBP and prevention of LBP recurrence. Superficial heating is a readily available modality and initially should be tried for 20 minutes twice daily with a hot pack or 8 hours per day with a heat wrap at home.18,26 A short course of NSAIDs (ibuprofen or naproxen) is recommended as the initial pharmacological intervention. Alternatively, acetaminophen can be used if NSAIDs are contraindicated.18 (Figure 2) Patients often report a trial of these over-the-counter medications at home without significant relief; however, the dose and frequency are often suboptimal. Therefore, it is worthwhile reviewing and prescribing NSAIDs with a therapeutic dose and frequency.27 A different class of NSAIDs or combination of NSAIDs and acetaminophen can be considered, unless contraindicated.28 Muscle relaxants can also be used for a short period with significant pain relief for acute LBP.29 Spinal manipulation and massage can also be considered initially for acute LBP if resources are available.18
Figure 2.
Pharmacological management for acute and chronic low back pain.18
Management of Chronic Low Back Pain
Patients with CLBP, defined as greater than 12 weeks of duration, can be a challenge to PCPs at an initial encounter. Sometimes, the patient has been in the care of other providers and has had some or even extensive work up and interventions. In this case, it is important to review if the prior assessment was appropriate and then find any missing information (e.g., red flags or yellow flags).
Setting realistic goals of pain management, to reduce pain rather than complete resolution, and addressing function to improve daily activities will be paramount to better patient compliance. It is important to remind the patient that mild pain should not warrant total rest. For nonspecific CLBP without red flags or focal neurological deficits, early referral to multidisciplinary rehabilitation, i.e., a physiatrist, will be efficacious for CLBP. If not accessible, encouragement of physical activity (walking and gentle stretching) and mindfulness-based stress reduction can be useful. For pharmacological treatment of CLBP, NSAIDs are the first-line therapy followed by duloxetine and tramadol as second-line therapy.30 Standing doses of NSAIDs are not recommended more than a week continuously as they can be related to acute kidney injury or gastrointestinal ulcers. It is important to explain that tramadol, an opioid agonist, can be associated with opioid-related adverse events including misuse and abuse. Anticonvulsants such as gabapentin, pregabalin and topiramate are increasingly utilized to treat low back pain and/or radiating leg pain, colloquially known as “sciatica”. However, these medications lack high-quality evidence for efficacy, although the associated adverse effects are relatively mild.31 Another commonly prescribed medication for CLBP is muscle relaxants, although their efficacy in treating CLBP is not clear.
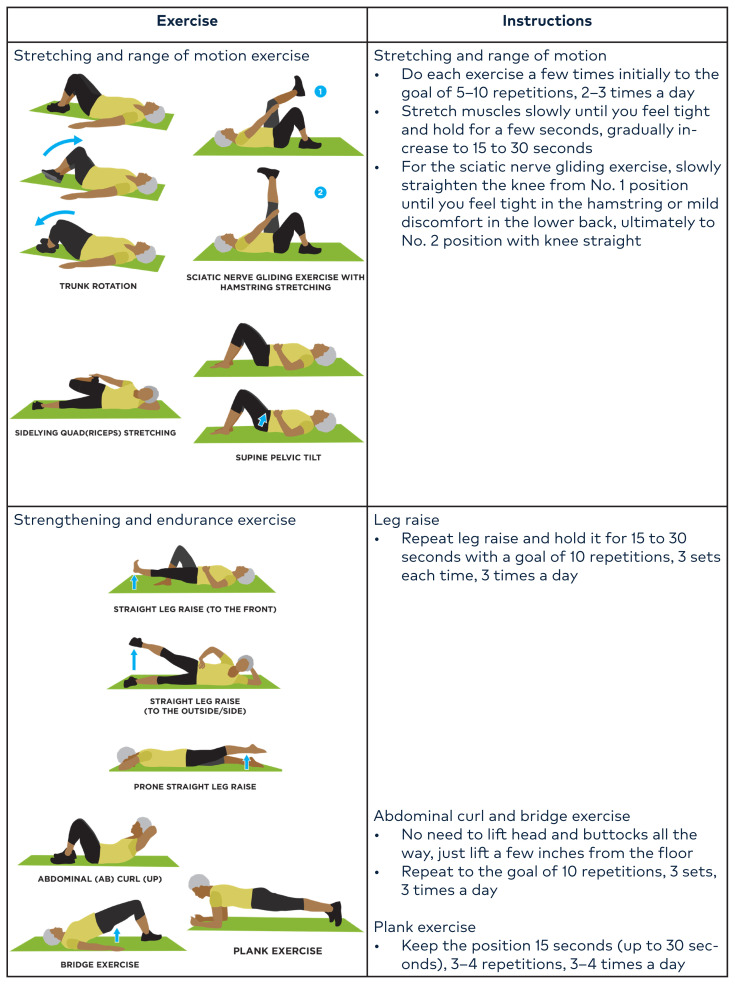
Home Exercise Program
A home exercise program is a long-term, effective and economic solution to improve LBP and has been shown to prevent recurrence. Specific exercises vary based on the individual patient. Common exercises include stretching/range of motion exercise, strengthening, endurance exercise of core muscles, balance exercise and functional activities. The details of these exercises are illustrated in Figure 3. The biggest challenge is adherence, which can vary from 30–84% depending on multiple factors such as age, motivation, pain level, complexity and number of exercises, supervision, follow-up, and communication with health care providers.33,34 To improve adherence, PCPs can review some exercises with the patient or a trained medical assistant can review them during the encounter. A few sessions of PT focusing on home exercise education can be an option as well.
Figure 3.
Illustration of commonly done home exercises for patients with low back pain. Source: Nevada Interprofessional Healthy Aging Network (NIHAN), ©2021 by NIHAN.32
Physical Therapy
In the context of interdisciplinary management, an experienced therapist can adopt different therapeutic exercises while the referring physician sets overall goals with specific precautions. The communication between interdisciplinary team members is key to a successful outcome.
PT should be considered if the patient shows persistent (more than 6 weeks) pain and dysfunction despite education and a self-directed home exercise program. It can also be extended if the patient is not ready to perform home exercise independently. It is important to remind the patient of the limited duration of physical therapy and importance of establishing an independent and self-directed home exercise program. It can also be useful to know several names of common therapeutic exercise interventions for LBP.35
Common physical therapy protocols for LBP include stretching/flexibility/neurodynamic therapy, manual therapy, core muscle stabilization exercise, postural/balance exercise, direction-based therapeutic exercise, heating modalities and education/review of home exercise programs. Iliopsoas/rectus femoris stretching can be very useful if there is a significantly tight hip flexor leading to anterior pelvic rotation, which, in turn, promotes lumbar lordosis therefore aggravating symptoms of spinal stenosis and facet arthropathy. The reverse mechanism can also develop with significant hamstring tightness. Modifications of the hamstring tendon stretching can be used to promote sciatic nerve mobility such as with neurodynamic therapy (e.g., slump stretching exercise).36 Manual therapy includes lumbopelvic mobilization, muscle energy techniques, manipulation and occasionally traction.37 Direction-based therapeutic exercises such as McKenzie exercises are commonly used to address sciatic pain and to restore lumbar lordosis using extension, flexion and lateral directional movements depending on the individual patient.38 Williams exercises are used in patients with spinal stenosis emphasizing flexion-based movement such as pelvic tilt, knee to chest, partial sit up, hip flexor stretches and squats.39
Core stabilization exercises are also frequently utilized and include neuromuscular control exercises, strengthening exercises of specific muscles and dynamic stability exercises that are frequently underutilized. Some physical examinations (such as the prone instability test) can be useful to predict the response to core muscle stabilization exercises.40 Lower limb strengthening exercises can add to core muscle exercise and are shown to improve LBP and mobility.41 Postural rehabilitation through muscle strengthening, flexibility and stretching also has been shown to be an effective exercise for CLBP.42
Complementary medicine such as massage, yoga and Pilates can be considered with some proven benefit for CLBP.43 Yoga can provide some improvement in back related pain and function, but it is uncertain if there is any significant improvement compared to other exercises.44 Pilates can also be considered as an adjunct treatment option using isometric contractions of the core muscles while moving or at rest.45
In addition to these therapeutic interventions, if there are yellow flags present, it may be important to engage CBT early in management.46 CBT can decrease catastrophizing and increase self-efficacy for managing pain. Similarly, mindfulness-based intervention can increase pain acceptance and mindfulness.47
Follow-Up Visit
On the follow-up visit, the physician should evaluate the interval changes in pain and functional level as reported by the patient (with or without using specific scales as described in the initial evaluation section above), the compliance and efficacy of the intervention from the first visit and any new symptoms. Non-pharmacological intervention, particularly therapeutic exercise, is typically associated with less compliance than pharmacological intervention as it places more burden on the patient.33
If LBP is improving, the PCP can start transitioning or weaning off the pharmacological pain management while increasing physical activities. “Back schools,” a combination of exercises and education often done during PT sessions, can be discussed with the patient. Evidence is limited for efficacy due to the low number of studies and widely varying protocols. It may be useful to some patients with psychological risks, as education in “back schools” has evolved over the years from negative messaging (strict restriction) to more positive messaging (what and how to do) to support psychological well-being.48
If LBP is not improving despite initial pharmacological and non-pharmacological interventions, referral to a multidisciplinary pain service can be an option. Opioid medications (other than short term tramadol [≤ 7 days]) should only be considered in a multidisciplinary pain clinic if the aforementioned interventions failed to improve the pain. However, it is important to note that opioid analgesics have not been shown to improve functional outcomes of acute LBP and there is scarce evidence of efficacy in CLBP. In fact, long term use of opioid analgesics in CLBP can cause drug tolerance, emergence of drug induced hyperalgesia and an increase in medication-related adverse events including opioid use disorders such as addiction and overdose-related mortality.28
Bracing, such as lumbosacral orthosis (LSO), can be considered in CLBP as an adjunct to improve physical activity. Different types of lumbosacral orthoses are available. These range from over-the-counter options including lumbosacral belts and lumbosacral corsets as well as rigid LSOs such as the William, Chairback, or Warm and Foam LSOs, each of which requires a prescription. Bracing is not usually effective in preventing LBP and it remains unclear whether it is more effective than no or other intervention; therefore, utilization should be judicious in selected patients who failed other previously mentioned conservative treatments.49
Conclusion
Conservative management can be effective in most patients with LBP. Understanding factors for unfavorable prognosis and atypical course can be useful in treatment planning. Conservative management options, including education, psychological intervention, different therapeutic exercises and bracing, eventually lead to an independent and self-directed home exercise program. Understanding the details of these conservative management options by the PCP can lead to better utilization of these options.
Funding Statement
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity.
Footnotes
Conflicts of Interest
The authors declare they have no conflicts of interest.
Drs. Doddy, Lee and Nguyen are employees of Sunrise Health GME Consortium, an organization affiliated with the journal’s publisher.
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
References
- 1. Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344(5):363–370. doi: 10.1056/nejm200102013440508. [DOI] [PubMed] [Google Scholar]
- 2. Finley CR, Chan DS, Garrison S, et al. What are the most common conditions in primary care? Systematic review. Can Fam Physician. 2018;64(11):832–840. [PMC free article] [PubMed] [Google Scholar]
- 3. Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24(6):769–781. doi: 10.1016/j.berh.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 4. GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–1259. doi: 10.1016/s0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Theis KA, Steinweg A, Helmick CG, Courtney-Long E, Bolen JA, Lee R. Which one? What kind? How many? Types, causes, and prevalence of disability among U.S. adults. Disabil Health J. 2019;12(3):411–421. doi: 10.1016/j.dhjo.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 6. Kelly GA, Blake C, Power CK, O’keeffe D, Fullen BM. The association between chronic low back pain and sleep: a systematic review. Clin J Pain. 2011;27(2):169–181. doi: 10.1097/ajp.0b013e3181f3bdd5. [DOI] [PubMed] [Google Scholar]
- 7. Foster NE, Anema JR, Cherkin D, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018;391(10137):2368–2383. doi: 10.1016/s0140-6736(18)30489-6. [DOI] [PubMed] [Google Scholar]
- 8. Axén I, Leboeuf-Yde C. Trajectories of low back pain. Best Pract Res Clin Rheumatol. 2013;27(5):601–612. doi: 10.1016/j.berh.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 9. Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet. 2018;391(10137):2356–2367. doi: 10.1016/s0140-6736(18)30480-x. [DOI] [PubMed] [Google Scholar]
- 10. Bratton RL. Assessment and management of acute low back pain. Am Fam Physician. 1999;60(8):2299–2308. [PubMed] [Google Scholar]
- 11. Glattacker M, Heyduck K, Jakob T. Yellow flags as predictors of rehabilitation outcome in chronic low back pain. Rehabil Psychol. 2018;63(3):408–417. doi: 10.1037/rep0000200. [DOI] [PubMed] [Google Scholar]
- 12. Ikemoto T, Miki K, Matsubara T, Wakao N. Psychological treatment strategy for chronic low back pain. Spine Surg Relat Res. 2018;3(3):199–206. doi: 10.22603/ssrr.2018-0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chou R, Shekelle P. Will this patient develop persistent disabling low back pain? JAMA. 2010;303(13):1295–1302. doi: 10.1001/jama.2010.344. [DOI] [PubMed] [Google Scholar]
- 14. Polomano RC, Galloway KT, Kent ML, et al. Psychometric Testing of the Defense and Veterans Pain Rating Scale (DVPRS): a new pain scale for military population. Pain Med. 2016;17(8):1505–1519. doi: 10.1093/pm/pnw105. [DOI] [PubMed] [Google Scholar]
- 15. Wygant DB, Arbisi PA, Bianchini KJ, Umlauf RL. Waddell non-organic signs: new evidence suggests somatic amplification among outpatient chronic pain patients. Spine J. 2017;17(4):505–510. doi: 10.1016/j.spinee.2016.10.018. [DOI] [PubMed] [Google Scholar]
- 16. Kongsted A, Kent P, Jensen TS, Albert H, Manniche C. Prognostic implications of the Quebec Task Force classification of back-related leg pain: an analysis of longitudinal routine clinical data. BMC Musculoskelet Disord. 2013;14:171. doi: 10.1186/1471-2474-14-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. AANEM. AANEM’s top five choosing wisely recommendations. Muscle Nerve. 2015;51(4):617–619. doi: 10.1002/mus.24628. [DOI] [PubMed] [Google Scholar]
- 18. Qaseem A, Wilt TJ, McLean RM, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice cuideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–530. doi: 10.7326/m16-2367. [DOI] [PubMed] [Google Scholar]
- 19. Petersen T, Laslett M, Juhl C. Clinical classification in low back pain: best-evidence diagnostic rules based on systematic reviews. BMC Musculoskelet Disord. 2017;18(1):188. doi: 10.1186/s12891-017-1549-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fairbank J, Gwilym SE, France JC, et al. The role of classification of chronic low back pain. Spine (Phila Pa 1976) 2011;36(21 Suppl):S19–S42. doi: 10.1097/brs.0b013e31822ef72c. [DOI] [PubMed] [Google Scholar]
- 21. Gianola S, Frigerio P, Agostini M, et al. Completeness of outcomes description reported in low back pain rehabilitation interventions: a survey of 185 randomized trials. Physiother Can. 2016;68(3):267–274. doi: 10.3138/ptc.2015-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Henschke N, Maher CG, Refshauge KM, et al. Prevalence of and screening for serious spinal pathology in patients presenting to primary care settings with acute low back pain. Arthritis Rheum. 2009;60(10):3072–3080. doi: 10.1002/art.24853. [DOI] [PubMed] [Google Scholar]
- 23. Chou R, Deyo RA, Jarvik JG. Appropriate use of lumbar imaging for evaluation of low back pain. Radiol Clin North Am. 2012;50(4):569–585. doi: 10.1016/j.rcl.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 24.Imaging Tests fo Lower-Back Pain. Choosing Wisely Published; Apr, 2012. https://www.choosingwisely.org/patient-resources/imaging-tests-for-back-pain/ [Google Scholar]
- 25. Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36(4):811–816. doi: 10.3174/ajnr.a4173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. French SD, Cameron M, Walker BF, Reggars JW, Esterman AJ. A Cochrane review of superficial heat or cold for low back pain. Spine (Phila Pa 1976) 2006;31(9):998–1006. doi: 10.1097/01.brs.0000214881.10814.64. [DOI] [PubMed] [Google Scholar]
- 27. Chou R, Deyo R, Friedly J, et al. Systemic pharmacologic therapies for low back pain: a systematic review for an American College of Physicians Clinical Practice Guideline. Ann Intern Med. 2017;166(7):480–492. doi: 10.7326/m16-2458. [DOI] [PubMed] [Google Scholar]
- 28. Deyo RA, Von Korff M, Duhrkoop D. Opioids for low back pain. BMJ. 2015;350:g6380. doi: 10.1136/bmj.g6380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Abdel Shaheed C, Maher CG, Williams KA, McLachlan AJ. Efficacy and tolerability of muscle relaxants for low back pain: systematic review and meta-analysis. Eur J Pain. 2017;21(2):228–237. doi: 10.1002/ejp.907. [DOI] [PubMed] [Google Scholar]
- 30. Kamper SJ, Apeldoorn AT, Chiarotto A, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ. 2015;350:h444. doi: 10.1136/bmj.h444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Enke O, New HA, New CH, et al. Anticonvulsants in the treatment of low back pain and lumbar radicular pain: a systematic review and meta-analysis. CMAJ. 2018;190(26):E786–E793. doi: 10.1503/cmaj.171333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mobility: Home Exercises of Low Back. NIHAN Published; 2020. https://www.nihan.care/wp-content/uploads/2020/08/Mob-BACK-red.pdf . [Google Scholar]
- 33. Nicolson PJA, Bennell KL, Dobson FL, Van Ginckel A, Holden MA, Hinman RS. Interventions to increase adherence to therapeutic exercise in older adults with low back pain and/or hip/knee osteoarthritis: a systematic review and meta-analysis. Br J Sports Med. 2017;51(10):791–799. doi: 10.1136/bjsports-2016-096458. [DOI] [PubMed] [Google Scholar]
- 34. Medina-Mirapeix F, Escolar-Reina P, Gascón-Cánovas JJ, Montilla-Herrador J, Jimeno-Serrano FJ, Collins SM. Predictive factors of adherence to frequency and duration components in home exercise programs for neck and low back pain: an observational study. BMC Musculoskelet Disord. 2009;10:155. doi: 10.1186/1471-2474-10-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hayden JA, Cartwright JL, Riley RD, Vantulder MW. Chronic Low Back Pain IPD Meta-Analysis Group. Exercise therapy for chronic low back pain: protocol for an individual participant data meta-analysis. Syst Rev. 2012;1:64. doi: 10.1186/2046-4053-1-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Pourahmadi M, Hesarikia H, Keshtkar A, et al. Effectiveness of slump stretching on low back pain: a systematic review and meta-analysis. Pain Med. 2019;20(2):378–396. doi: 10.1093/pm/pny208. [DOI] [PubMed] [Google Scholar]
- 37. Sipko T, Paluszak A, Siudy A. Effect of sacroiliac joint mobilization on the level of soft tissue pain threshold in asymptomatic women. J Manipulative Physiol Ther. 2018;41(3):258–264. doi: 10.1016/j.jmpt.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 38. Karlsson M, Bergenheim A, Larsson MEH, Nordeman L, van Tulder M, Bernhardsson S. Effects of exercise therapy in patients with acute low back pain: a systematic review of systematic reviews. Syst Rev. 2020;9(1):182. doi: 10.1186/s13643-020-01412-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sukmajaya W, Alkaff FF, Oen A, Sukmajaya AC. Williams flexion exercise for low back pain: a possible implementation in rural areas. Open Access Maced J Med Sci. 2020;8(B):1–5. [Google Scholar]
- 40. Chang WD, Lin HY, Lai PT. Core strength training for patients with chronic low back pain. J Phys Ther Sci. 2015;27(3):619–622. doi: 10.1589/jpts.27.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. de Sousa CS, de Jesus FLA, Machado MB, et al. Lower limb muscle strength in patients with low back pain: a systematic review and meta-analysis. J Musculoskelet Neuronal Interact. 2019;19(1):69–78. [PMC free article] [PubMed] [Google Scholar]
- 42. Paolucci T, Attanasi C, Cecchini W, Marazzi A, Capobianco SV, Santilli V. Chronic low back pain and postural rehabilitation exercise: a literature review. J Pain Res. 2018;12:95–107. doi: 10.2147/jpr.s171729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Whitehead A, Gould Fogerite S. Yoga treatment for chronic non-specific low back pain (2017) Explore (NY) 2017;13(4):281–284. doi: 10.1016/j.explore.2017.04.018. [DOI] [PubMed] [Google Scholar]
- 44. Saper RB, Lemaster C, Delitto A, et al. Yoga, physical therapy, or education for chronic low back pain: a randomized noninferiority trial. Ann Intern Med. 2017;167(2):85–94. doi: 10.7326/m16-2579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Yamato TP, Maher CG, Saragiotto BT, et al. Pilates for low back pain: complete republication of a Cochrane review. Spine (Phila Pa 1976) 2016;41(12):1013–1021. doi: 10.1097/brs.0000000000001398. [DOI] [PubMed] [Google Scholar]
- 46. Hill JC, Whitehurst DG, Lewis M, et al. Comparison of stratified primary care management for low back pain with current best practice (STarT Back): a randomised controlled trial. Lancet. 2011;378(9802):1560–1571. doi: 10.1016/s0140-6736(11)60937-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Turner JA, Anderson ML, Balderson BH, Cook AJ, Sherman KJ, Cherkin DC. Mindfulness-based stress reduction and cognitive behavioral therapy for chronic low back pain: similar effects on mindfulness, catastrophizing, self-efficacy, and acceptance in a randomized controlled trial. Pain. 2016;157(11):2434–2444. doi: 10.1097/j.pain.0000000000000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Parreira P, Heymans MW, van Tulder MW, et al. Back schools for chronic non-specific low back pain. Cochrane Database Syst Rev. 2017;8(8):CD011674. doi: 10.1002/14651858.cd011674.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. van Duijvenbode IC, Jellema P, van Poppel MN, van Tulder MW. Lumbar supports for prevention and treatment of low back pain. Cochrane Database Syst Rev. 2008;1823;2008(2):CD00. doi: 10.1002/14651858.cd001823.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]