Abstract
Background
Adverse Childhood Experiences (ACEs) have been shown to contribute to a litany of mental and physical health problems, including several chronic diseases and death, via a model known as the ACE pyramid. Many of the results of ACEs in the ACE pyramid are known contributors to poor perceived health, which has significant health implications. Despite these results, a possible link between ACEs and perceived health has not been examined to date. Based on the temporal order of the ACE pyramid, we believe any relationship between ACEs and perceived health will be mediated by other components of the model.
Methods
We conducted an analysis of the 2010 Behavioral Risk Factor Surveillance System (BRFSS) data for 4 states (Hawaii, Nevada, Vermont and Wisconsin).The Adverse Childhood Experiences Scale (11 questions) and Physical Health Days (days out of the last 30 where physical health was not good) were the primary predictor and outcome variables, respectively. The PHQ-8, a depression measure, served as a first-level mediator, while body mass index, Sleep Days (days out of the last 30 that sleep was poor) and average monthly alcohol consumption served as second-level mediators. We conducted a multiply-mediated regression using PROCESS (Hayes, 2018).
Results
The analysis included 6,060 respondents. ACEs were associated with an increase of 0.28 additional days of poor perceived health days per ACE through increases in depression and poor sleep.
Conclusions
Adverse childhood experiences may influence perceived health through multiple intermediary factors, including depression and poor sleep quality. We discuss several theoretical and clinical implications, and future directions are proposed that take advantage of the multiply-mediated model.
Keywords: adverse childhood experiences, perceived health, depression, mediation, sociological factors, child abuse, domestic violence, health behavior, psychological stress
Introduction
Adverse Childhood Experiences (ACEs) refer to distressing, often traumatic, events that could happen in a child’s life, such as physical, sexual and emotional abuse, neglect and family environment factors, such as domestic abuse and divorce.1 Unfortunately, ACEs are not an uncommon phenomenon. The 2016 National Survey of Children’s Health found that 45% of children have experienced at least one ACE, while 20% of children have experienced two or more.2 Children who experience one or more ACE are at risk for a variety of negative health outcomes.1,3–5
The ACE Pyramid
The ACE pyramid, originally proposed in 1998, is a theoretical model that demonstrates the path by which the health of a child who has experienced ACEs may be significantly diminished.1 The model proposes that ACEs lead to the development of biopsychosocial abnormalities, which increase the likelihood of health risk behaviors, contributing to the onset of chronic disease and ultimately culminating in death.1 In the time since the initial ACE study, much work has been done to examine and support the stages of the ACE pyramid. Regarding psychosocial abnormalities, ACEs have been linked with an increased risk of coincident and future depression and suicide.6–12 The lasting effects of ACEs can later be seen through the development of risky health behaviors, including the use of alcohol, tobacco and illicit substances, such as prescription opioids.7,11,13,14 Other health risk factors, including poor sleep and an unhealthy body mass index (BMI), have been linked to ACEs as well.15–18 Finally, ACEs have been linked to countless chronic health conditions, such as autoimmune disease, heart disease, liver disease and cancer.19–22 In total, the existing literature provides ample evidence to support the ACE pyramid as a theoretical model and to demonstrate that ACEs affect a wide range of mental and physical health outcomes. However, no study to date has examined the impact of ACEs on perceived health.
ACEs and Perceived Health
Perceived physical health refers to an individual’s thoughts regarding their own health. While understandably associated with objective health, perceived health is distinct in that it is a subjective experience that can differ from measures of objective health. Some studies suggest that objective health may not even be the primary determinant of perceived health, with other factors such as life satisfaction, spirituality and close relationships playing a larger role in determining perceived health.23–25 Perceived health is also associated with mortality independently from objective health, as patients who perceive their health as being poor experience health declines faster than their peers who are of similar objective health.23,26,27 For example, studies have shown that the impact of poor perceived health has a substantial impact on survival rates for cancer patients.28 This influence on survival lends itself to including poor perceived health in the ACE pyramid model, as the capstone for the pyramid is death.1 While the traditional focus of the ACE pyramid has been on the chronic health conditions that directly contribute to mortality, it stands to reason that a factor shown to have a pronounced impact on mortality beyond chronic illness may also be an important component of the ACE pyramid model. Furthermore, many of the factors that are commonly included as early outcomes in the ACE pyramid are associated with increases in poor perceived health. There is an established link between depression and poor perceived physical health.25,29,30 Other studies have shown that poor perceived health is associated with poor sleep,31–33 excess alcohol consumption34–36 and BMI.24,37,38 With many of the very risk factors that ACEs increase also being associated with poor perceived health, it reasons then that ACEs may indirectly contribute to poor perceived health as mediated by those factors.
Multiple-Mediation Model
When examining the ACE pyramid and the effects of ACEs on health outcomes, much of the work conducted has been done using a single-mediation model.39,40 While more thorough than a non-mediational model, the use of a single mediation pathway fails to account for the complexity involved in the intersection of biological and psychological phenomena. Using a single-mediation does not provide sufficient explanation of the underlying mechanisms of the ACE pyramid model as it was proposed as a single-mediation collapses several of the model’s casual layers into one, reducing the depth of knowledge gained from the study. We propose that the unique levels of the ACE pyramid, when available, should be used as additional mediation levels in order to capture the nature of the phenomena in question more fully.
This Study
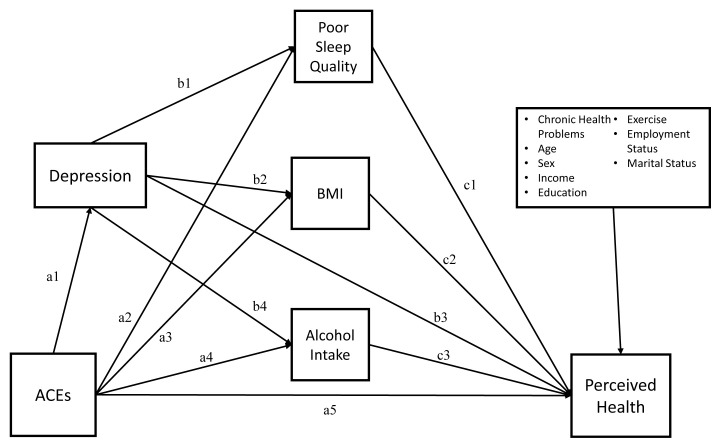
The ACE pyramid conceptually outlines how ACEs contribute to depression, health risk behaviors and chronic disease. We aim to expand this theoretical model to include a psychological component of health by examining the association between the ACE pyramid model and perceived health. Previous work on ACEs has only used single-mediated models primarily aimed at assessing the effects of ACEs on chronic health problems. The current study examines the ACE pyramid model with a multiple-mediation model to further expand the understanding of the wide-reaching influences of ACEs. (Figure 1) Specifically, we expect that ACEs will be indirectly associated with an increase in poor perceived health as mediated by depression and health-related risk factors.
Figure 1.
Theoretical Multiple-Mediation Model for Poor Perceived Physical Health. Proposed theoretical model linking Adverse Childhood Experiences to Perceived Health. Paths can be combined to describe mediating paths. For example, ACEs to BMI (Path a3) and BMI to Perceived Health (c2) shows ACEs’ effect on Perceived Health through Path a3c2.
Methods
Participants and the Procedure
Data from the 2010 Behavioral Risk Factor Surveillance Survey (BRFSS) was used, as this was the most recent year in which questions relating to both ACEs and depression were included. The BRFSS is an annual telephone survey conducted by the CDC designed to be representative of the United States population.41 The BRFSS includes core health questions administered to every participant, as well as optional modules on a per-state basis.41 The modules assessing ACEs and depression are both optional modules, and were last administered together in the 2010 BRFSS across four states (Hawaii, Nevada, Vermont and Wisconsin). As a result, data for this study was limited to those 4 states (Possible n = 6,081, 62% female).
Measures
The Adverse Childhood Experiences Scale was used as a measure of challenges during childhood.41 The ACEs Scale consists of 11 questions related to the 8 ACEs defined in the original ACE study.1,41 While there are various validated methods that can be used to score and subscale the ACEs Scale,1,21 we have opted to use the entirety of the scale as a 1-factor “child maltreatment” scale as demonstrated by Ford and colleagues.42 The reliability of the ACEs Scale was good (Cronbach’s α = 0.78).
Perceived poor physical health (PPPH) was assessed by a single-item from the Healthy Days portion of the HRQOL-4:41,43 “Now thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good?” While perceived health is commonly assessed on a likert-type question, such as “How would you rate your health?”, a review by the CDC found that the HRQOL-4’s Physical Healthy Days had strong construct validity as a measure of perceived health, as well as offering several advantages over the more traditional likert-type question.43
Depression was assessed via the Patient Health Questionnaire-8 (PHQ-8), which is an 8-question screening tool that has been repeatedly validated and is derived from the PHQ-9 frequently used in clinical settings.44 Questions are scored from 0 to 14, indicating the number of days out of the last 2 weeks the participant has experienced each of the 8 symptoms, resulting in a score ranging from 0 to 112 symptom days. The reliability of the PHQ-8 was good (Cronbach’s α = 0.86).
The remaining mediating variables were assessed with single-item measures. Sleep quality was measured by the question, “How many days did you not get enough sleep in the past 30 days?”41 BMI is a calculated variable in the BRFSS derived from self-reported height and weight. Average monthly alcohol consumption was assessed with the question, “During the last 30 days, on days when you drank, about how many drinks did you drink on average?”41
In addition to our primary measurers, several covariates were included to account for known health risk factors. The covariates included age, income, education, sex, exercise, employment and marital status, all of which were categorical with the exception of age (continuous) and sex (binary). Additionally, a cumulative measure of chronic health problems was included to account for several indicators of objective poor health, including diabetes, heart attack, heart disease, stroke and current asthma as reported to the patient by their doctor. Objective health measures were included as a covariate as a means to further isolate the impact of ACEs on the perception of health rather than the existence of health conditions.
Statistical Analysis
As a preliminary analysis, we conducted bivariate correlations between ACEs, depression, sleep quality, BMI, alcohol consumption, chronic health problems and perceived poor physical health (PPPH). Out of the total sample of 6,081, 21 participants were excluded from the main analysis due to missing data (Final n= 6,060, 0.5% missing). For the main analysis, we analyzed a multiple mediation model using the PROCESS v3 macro in SAS 9.4 under the current assumptions for mediation.45–47 As we used observational data without a pre-existing temporal relationship between the variables, we selected the direction of the proposed paths in the model based on the theoretical flow of the ACE pyramid.1 The PROCESS v3 procedure uses bootstrapping (k= 5,000) to create 95% confidence intervals for the estimated indirect effects as a measure of significance instead of the Sobel test, as is recommended in current mediation literature.45–47 Finally, in preparation for our OLS regression-based analyses, we conducted an assessment of multicollinearity that revealed no multicollinearity concerns between the variables and covariates based on all variance inflation factors (VIFs) being below 2.5.
Results
Participants ranged in age from 18–99 (M = 56.3, SD = 16.05). The sample was primarily White (72.4%) with 3.5% Black, 7.8% Multiracial, 3.85% Hispanic and 11.6% other. The mean ACE score was 2.0 (SD = 2.29). For all descriptive statistics, see Table 1. In our preliminary analysis of correlations, ACEs were associated with increases in all mediating variables (p < 0.0001) as well as increases in PPPH (r = 0.08, p < 0.0001). Additionally, almost all mediating variables were associated with increases in PPPH (Table 2) with alcohol consumption being the only exception; it was associated with a decrease in PPPH (r = −0.08, p < 0.0001). All covariates were significantly correlated with the outcome measure (p < 0.05) and were, therefore, included in the final model.
Table 1.
Descriptive Statistics of Primary Variables and Demographics
| N= 6,081 | |
|---|---|
| Primary Variables, Mean (SD) | |
| Poor Perceived Health | 10.75 (10.83) |
| ACEs | 2.01 (2.29) |
| Depression | 19.78 (23.01) |
| Sleep Quality | 9.64 (10.69) |
| BMI | 27.95 (6.52) |
| Alcohol Intake* | 1.12 (1.99) |
| Age, Mean (SD) | 56.28 (16.1) |
| Sex = Female, N (%) | 3770, (62.0) |
| Chronic Health Problems, Mean (SD) | 0.37 (0.69) |
| Race/Ethnicity, N (%) | |
| White | 4,403 (72.4) |
| Black | 210 (3.5) |
| Other | 704 (11.6) |
| Multiracial | 474 (7.8) |
| Hispanic | 234 (3.9) |
| Education Level, N (%) | |
| Education < HS | 419 (6.9) |
| Education > HS | 5,662 (93.1) |
| Monthly Exercise, N (%) | |
| Yes | 4,394 (72.3) |
| No | 1,687 (27.77) |
| Income, N (%) | |
| Income < 35K | 1,738 (28.6) |
| Income ≥ 35K | 4,343 (71.4) |
| Employment Status**, N (%) | |
| Employed | 3,278 (54.0) |
| Unemployed | 1,053 (17.34) |
| Retired | 1,740 (28.66) |
| Marital Status***, N (%) | |
| Married | 3,244 (53.42) |
| Previously Married | 1,795 (29.56) |
| Single/Never Married | 847 (13.95) |
| Currently Dating | 187 (3.08) |
For Alcohol Intake, N = 6,077
For Employment Status, N = 6,071
For Marital Status, N= 6,073
Table 2.
Bivariate Correlations Between Primary Variables
| ACE | Depression | Sleep Quality | BMI | Alcohol Intake | Perceived Health | |
|---|---|---|---|---|---|---|
| ACE Scale | 1 | |||||
| Depression | 0.34*** | 1 | ||||
| Sleep Quality | 0.20*** | 0.52*** | 1 | |||
| BMI | 0.08*** | 0.13*** | 0.12*** | 1 | ||
| Alcohol Intake | 0.08*** | 0.01 | 0.02 | −0.02 | 1 | |
| Perceived Health | 0.08*** | 0.35*** | 0.20*** | 0.09*** | −0.08*** | 1 |
Note:
p < 0.05
p < 0.001,
p < 0 .0001,
ACE= Adverse Childhood Experience Scale
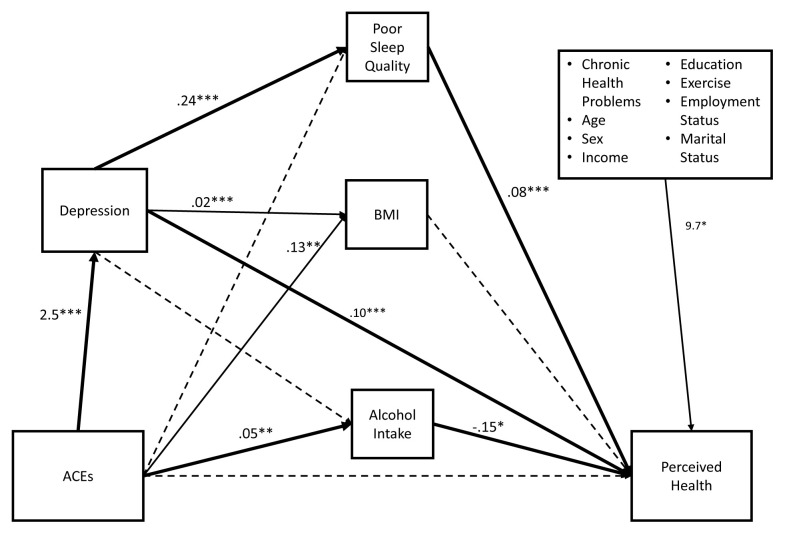
In the main analysis, the number of ACEs experienced were significantly associated with increases in depression scores (Path a1 = 2.5, p < 0.0001), BMI (Path a3 = 0.13, p = 0.0009) and alcohol consumption (Path a4 = 0.05, p = 0.0002). However, the number of ACEs experienced were not related to poor sleep (path a2, p = 0.59). The first mediator, the depression score, was associated with increases in both poor sleep (Path b1 = 0.24, p < 0.0001) and BMI (Path b2 = 0.02, p < 0.0001), but it was not related to alcohol consumption (Path b3, p = 0.61).
The multiple-mediation model for PPPH was significant (F16,6043 = 129.4, p < 0.0001) and accounted for 26% of the variance in PPPH. The direct effect of ACEs on PPPH was not significant (Path a5 = 0.026, p = 0.66). However, the total indirect effect of ACEs was significantly associated with an increase in PPPH (Total Indirect Effect = 0.28, 95%CI = 0.238–0.333) via 2 mediation paths (Figure 2). For the first mediation path, ACEs were associated with an increase in depression score, which were then associated with an increase in PPPH (Path a1b3 = 0.24, 95%CI = 0.200–0.293). In the second path, the significant ACEs-depression path was associated with an increase in poor sleep, which was then associated with an increase in PPPH (Path a1b1c1 = 0.049, 95% CI= 0.032–0.067). Additionally, ACEs were also indirectly associated with a decrease in PPPH mediated by alcohol consumption (Path a4c3 = −0.007, 95% CI = −0.013–−.0002). (Table 3)
Figure 2.
Computed Multiple-Mediation Model for Poor Physical Health.
Note: *p < 0.05, **p < 0.01, ***p < 0.001; Dashed lines indicate paths that are not statistically significant. Bolded paths indicate paths of mediation. Total indirect effect of ACEs = 0.28 (95% CI = 0.238–0.333). Significant Covariates includes chronic health problems, age, education > HS, sex = F, did not exercise in the past month, being unemployed and being retired.
Table 3.
Regression Estimates for Poor Perceived Health
| Estimate | SE | t | p | Lower CI (95%) | Upper CI (95%) | |
|---|---|---|---|---|---|---|
| Intercept | −2.20 | 1.13 | −1.91 | 0.06 | −4.37 | 0.05 |
| Primary Variables | ||||||
| ACEs | 0.03 | 0.06 | 0.44 | 0.66 | −0.09 | 0.14 |
| Depression | 0.10 | 0.01 | 14.40 | <.0001 | 0.09 | 0.11 |
| Poor Sleep Quality | 0.08 | 0.01 | 6.17 | 0.0001 | 0.06 | 0.11 |
| BMI | 0.00 | 0.02 | 0.12 | 0.91 | −0.03 | 0.04 |
| Alcohol Intake | −0.15 | 0.06 | −2.41 | 0.02 | −0.27 | −0.03 |
| Demographics | ||||||
| Age | 0.12 | 0.01 | 10.43 | <.0001 | 0.09 | 0.14 |
| Sex = Female | −1.01 | 0.26 | −3.90 | <.0001 | −1.51 | −0.50 |
| Education < HS | -- | -- | -- | -- | -- | -- |
| Education > HS | −1.20 | 0.49 | −2.47 | 0.01 | −2.16 | −0.25 |
| Exercise | -- | -- | -- | -- | -- | -- |
| No Monthly Exercise | 3.95 | 0.28 | 13.90 | <.0001 | 3.40 | 4.51 |
| Chronic Health Problems | 0.96 | 0.19 | 5.15 | <.0001 | 0.59 | 1.32 |
| Income <35K | -- | -- | -- | -- | -- | -- |
| Income ≥ 35K | −0.54 | 0.31 | −1.75 | 0.08 | −1.14 | 0.06 |
| Employment Status | ||||||
| Employed | -- | -- | -- | -- | -- | -- |
| Unemployed | 5.10 | 0.38 | 13.41 | <.0001 | 4.36 | 5.85 |
| Retired | 1.78 | 0.37 | 4.86 | <.0001 | 1.06 | 2.49 |
| Marital Status | ||||||
| Married | -- | -- | -- | -- | -- | -- |
| Previously Married | 0.13 | 0.31 | 0.41 | 0.68 | −0.48 | 0.73 |
| Single/Never Married | 0.30 | 0.39 | 0.78 | 0.43 | −0.46 | 1.07 |
| Currently Dating | 0.76 | 0.71 | 1.07 | 0.28 | −0.63 | 2.16 |
Note: Parameter estimates for the model predicting days of poor perceived health. Reference groups for categorical variables signified by --.
Discussion
This study aimed to support and expand upon the ACE pyramid model by demonstrating that ACEs exhibit a multiply-mediated association with perceived physical health. We found that ACEs were indirectly associated with poor perceived health via associated increases in the depression score followed by an associated increased in poor sleep. The lack of a significant direct association between ACEs and poor perceived health suggests that this association is fully mediated, which is consistent with the ACE pyramid model.1 While it is plausible that ACEs could have directly altered an individuals’ later perceptions, the implication of mediation allows for a more gradual, natural progression from experiencing ACEs to altered health perception.
Our results provide novel support for the ACE pyramid model by expanding upon prior findings in several key ways. First, this study provides evidence that ACEs are associated with perceived physical health, a construct known to increase mortality rates, but as of yet unexamined in ACEs research. This evidence suggests that ACEs may be a clinically significant factor to consider, even in late-life healthcare, due to the known impact of poor perceived health on decreased survival rates. Second, our study highlights the intertwining of psychosocial and physiological health by demonstrating that components of the ACE pyramid model can have an impact beyond biological health in the form of health perception. Finally, this study empirically demonstrates support for the ACE pyramid functioning as a model of multiple-mediation, and future studies should seek to use models that reflect the multi-layered nature of the ACE pyramid. These novel contributions provide several new avenues for ACEs research and interventions.
Perceived Physical Health
From a clinical perspective, this finding provides support for utilizing ACE scores in 2 new ways. First, ACE screening holds potential as an additional intervention area for pre-existing chronic health problems. As it stands, ACE screenings are used primarily as an aid in preventing poor health outcomes. Our findings suggest that ACE screenings can be used after the poor health outcome has occurred as a means to inform treatments targeted at improving perceived health. Second, our findings suggest an alternative avenue for prevention using ACE screenings for patients who do not yet have chronic health problems. In addition to the standard practice of using ACE scores to understand and address risky health behaviors, clinicians should also offer evidence-based interventions designed to improve perceived health, such as the use of mindfulness meditation.48,49 Future studies should seek to further examine the proposed link between ACEs, poor perceived health and survival rates as well as the efficacy of interventions, such as mindfulness for decreasing the effect of ACEs on perceived health.
We believe the link between ACEs and perceived health is troubling and worth serious consideration from a theoretical perspective as well. This finding, in conjunction with the existing body of literature, suggests that ACEs may pose a dual threat to the health of an individual. Much research has demonstrated that ACEs increase the likelihood that an individual develops one or more chronic health problems.1,3,4 Our findings suggest that ACEs are associated with increases in the likelihood that those same individuals perceive their health as poor. Given that perceived poor health is a risk factor known to decrease survival rates,23,26–28 it is plausible that ACEs may first contribute to making someone sick and then reduce their odds of survival by diminishing their perception of their health. Future research is needed to evaluate the role of perceived health in the ACE pyramid model as it relates to mortality.
Multiple-Mediation and ACEs
Our results showed that the relationship between ACEs and perceived health is multiply mediated via several associative pathways. ACEs were associated with an increase in the number of drinks a person has on average per month and their depression score. The increased depression score was then associated with the increase of days a person sleeps poorly. The increased depression score and the elevated incidence of poor sleep were associated with an increase in the number of days per month that person perceives their health to be poor. Additionally, the increased average number of drinks per month was associated with a slight decrease in the perceived poor health days per month. While the first 2 pathways are congruent with our hypotheses and the ACE pyramid in general, we believe the counterintuitive relationship between alcohol consumption and perceived health requires further examination and may be due in large part to 2 factors. First, our sample had a relatively low average number of drinks per month (M = 1.1, SD = 2.0), indicating that a strong majority of our sample did not drink with great frequency. This low number may indicate that the majority are using alcohol in social settings or as a self-care coping strategy, both of which could serve as protective factors for perceived health.50–54 Second, our sample’s drinking habits fall within the acceptable moderate drinking range of the United States dietary guidelines.55 We believe that individuals who engage in healthy drinking practices may also be mindful of other dietary guidelines, resulting in greater perceived health. Additionally, mild to moderate drinking has been shown to have a protective effect against a myriad of health problems.52,56–58 Future studies should seek to examine this link in further detail.
We propose that the multiply-mediated nature of ACEs provides several potential opportunities for intervening between when an individual experiences ACEs and their development of poor health. For instance, several school-level interventions have been shown to be effective at reducing depression rates,59 but our results suggest such interventions have the potential to offer long-term health benefits as well. In addition to interventions targeted at adolescents, we believe our findings support an opportunity to mitigate the increased health risks associated with ACEs in elderly patients. We propose that counseling or psychotherapy may be beneficial for the elderly as a means to boost their longevity, especially as their health declines, as it could serve to sever the mediation between ACEs and perceived health.
Future ACEs studies should seek to examine alternative, multiple-mediation avenues, such as the mediating roles of anxiety and nutrition. Multiple-mediation analysis provides an enhanced understanding of the mechanisms that underlie the relationship between ACEs and poor health that are otherwise left to conjecture. This enhanced understanding is crucial for developing new approaches to preventing chronic illness as well as aiding in the continued understanding of the relationships between mental and physical health.
Limitations
Our study had multiple limitations. First, our sample was a cross-sectional epidemiological survey, which limited our ability to make causal inferences. Specifically, while we attempted to control for a myriad of confounding factors, the potential for confounding factors cannot be ruled out in our study. Other factors that were unaccounted for may have a significant impact on both ACEs and PPPH, such as the parenting style the individual was raised with, the neighborhood they live in and various policy-level factors. Furthermore, most of the data was categorical in nature due to the formatting of the survey, and, therefore, we were limited in the level of specificity we could achieve with several measures. Finally, while we do not believe the impact of ACEs to be changing over time, it is worth noting that our data was somewhat older.
Second, while our use of the PROCESS methodology provided many advantages, it was unable to accommodate the weighting variables provided by the BRFSS.47 The BRFSS uses a complex survey design, including raking by strata, and they include several weights to account for the potential design effects of the survey.41 We were not able to adjust for these design effects, meaning our sample was biased in its construction. As a result, caution must be used in generalizing our findings to the general population.
Third, our application of the multiple-mediation methodology relies heavily on the theoretical assumptions of the ACE pyramid. For example, we modeled the effect of depression on poor sleep as the ACE Pyramid dictates that poor psychosocial health is the antecedent of problematic health behaviors. As a result, our proposed model does not accommodate the potential for reciprocal relationships, such as depression increasing poor sleep and poor sleep exacerbating depressive symptoms. While our model is informed by theory, it is plausible that misspecification of the mediational pathways occurred, resulting in biased estimates. Future studies should seek to further examine the proposed pathways using a longitudinal study.
Conclusion
Adverse childhood experiences are related to perceived health through multiple intermediary factors, including depression and poor sleep quality. Given the protective role of perceived health in patients with chronic conditions, screening for ACEs in those patients may be of clinical value. Furthermore, the mediational components of our model provide new insight for intervention opportunities relating to ACEs. Future research should further explore the integration of perceived health into the ACE pyramid.
Footnotes
Conflicts of Interest
The authors declare they have no conflicts of interest.
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
References
- 1. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 2.Child and Adolescent Health Measurement Initiative. 2016–2017 National Survey of Children’s Health (NSCH) data query. [Accessed August 28, 2019]. www.childhealthdata.org Published online 2019.
- 3. Foege WH. Adverse childhood experiences. A public health perspective. Am J Prev Med. 1998;14(4):354–355. doi: 10.1016/s0749-3797(98)00016-6. [DOI] [PubMed] [Google Scholar]
- 4. Gould DA, Stevens NG, Ward NG, Carlin AS, Sowell HE, Gustafson B. Self-reported childhood abuse in an adult population in a primary care setting. Prevalence, correlates, and associated suicide attempts. Arch Fam Med. 1994;3(3):252–256. doi: 10.1001/archfami.3.3.252. [DOI] [PubMed] [Google Scholar]
- 5. Weiss MJ, Wagner SH. What explains the negative consequences of adverse childhood experiences on adult health? Insights from cognitive and neuroscience research. Am J Prev Med. 1998;14(4):356–360. doi: 10.1016/s0749-3797(98)00011-7. [DOI] [PubMed] [Google Scholar]
- 6. Anda RF, Brown DW, Felitti VJ, Bremner JD, Dube SR, Giles WH. Adverse childhood experiences and prescribed psychotropic medications in adults. Am J Prev Med. 2007;32(5):389–394. doi: 10.1016/j.amepre.2007.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Anda RF, Whitfield CL, Felitti VJ, et al. Adverse childhood experiences, alcoholic parents, and later risk of alcoholism and depression. Psychiatr Serv. 2002;53(8):1001–1009. doi: 10.1176/appi.ps.53.8.1001. [DOI] [PubMed] [Google Scholar]
- 8. Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord. 2004;82(2):217–225. doi: 10.1016/j.jad.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 9. Cheong EV, Sinnott C, Dahly D, Kearney PM. Adverse childhood experiences (ACEs) and later-life depression: perceived social support as a potential protective factor. BMJ Open. 2017;7(9):e013228. doi: 10.1136/bmjopen-2016-013228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brodsky BS, Malone KM, Ellis SP, Dulit RA, Mann JJ. Characteristics of borderline personality disorder associated with suicidal behavior. Am J Psychiatry. 1997;154(12):1715–1719. doi: 10.1176/ajp.154.12.1715. [DOI] [PubMed] [Google Scholar]
- 11. Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA. 2001;286(24):3089–3096. doi: 10.1001/jama.286.24.3089. [DOI] [PubMed] [Google Scholar]
- 12. Kingree JB, Thompson MP, Kaslow NJ. Risk factors for suicide attempts among low-income women with a history of alcohol problems. Addict Behav. 1999;24(4):583–587. doi: 10.1016/s0306-4603(98)00109-9. [DOI] [PubMed] [Google Scholar]
- 13. Dube SR, Anda RF, Felitti VJ, Edwards VJ, Croft JB. Adverse childhood experiences and personal alcohol abuse as an adult. Addict Behav. 2002;27(5):713–725. doi: 10.1016/s0306-4603(01)00204-0. [DOI] [PubMed] [Google Scholar]
- 14. Strine TW, Dube SR, Edwards VJ, et al. Associations between adverse childhood experiences, psychological distress, and adult alcohol problems. Am J Health Behav. 2012;36(3):408–423. doi: 10.5993/ajhb.36.3.11. [DOI] [PubMed] [Google Scholar]
- 15. Chapman DP, Wheaton AG, Anda RF, et al. Adverse childhood experiences and sleep disturbances in adults. Sleep Med. 2011;12(8):773–779. doi: 10.1016/j.sleep.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 16. Chapman DP, Liu Y, Presley-Cantrell LR, et al. Adverse childhood experiences and frequent insufficient sleep in 5 U.S. States, 2009: a retrospective cohort study. BMC Public Health. 2013;13:3. doi: 10.1186/1471-2458-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Thomas C, Hyppönen E, Power C. Obesity and type 2 diabetes risk in midadult life: the role of childhood adversity. Pediatrics. 2008;121(5):e1240–e1249. doi: 10.1542/peds.2007-2403. [DOI] [PubMed] [Google Scholar]
- 18. Williamson DF, Thompson TJ, Anda RF, Dietz WH, Felitti V. Body weight and obesity in adults and self-reported abuse in childhood. Int J Obes Relat Metab Disord. 2002;26(8):1075–1082. doi: 10.1038/sj.ijo.0802038. [DOI] [PubMed] [Google Scholar]
- 19. Brown MJ, Thacker LR, Cohen SA. Association between adverse childhood experiences and diagnosis of cancer [published correction appears in PLoS One. 2014;9(1). https://doi.org/10.1371/annotation/bd99c401-8d86-465a-a930-bd84bb662657 ] PLoS One. 2013;8(6):e65524. doi: 10.1371/journal.pone.0065524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dong M, Dube SR, Felitti VJ, Giles WH, Anda RF. Adverse childhood experiences and self-reported liver disease: new insights into the causal pathway. Arch Intern Med. 2003;163(16):1949–1956. doi: 10.1001/archinte.163.16.1949. [DOI] [PubMed] [Google Scholar]
- 21. Dong M, Anda RF, Felitti VJ, et al. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse Negl. 2004;28(7):771–784. doi: 10.1016/j.chiabu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 22. Dube SR, Fairweather D, Pearson WS, Felitti VJ, Anda RF, Croft JB. Cumulative childhood stress and autoimmune diseases in adults. Psychosom Med. 2009;71(2):243–250. doi: 10.1097/psy.0b013e3181907888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wu S, Wang R, Zhao Y, et al. The relationship between self-rated health and objective health status: a population-based study. BMC Public Health. 2013;13:320. doi: 10.1186/1471-2458-13-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Al-Windi A. The relations between symptoms, somatic and psychiatric conditions, life satisfaction and perceived health. A primary care based study. Health Qual Life Outcomes. 2005;3:28. doi: 10.1186/1477-7525-3-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mulsant BH, Ganguli M, Seaberg EC. The relationship between self-rated health and depressive symptoms in an epidemiological sample of community-dwelling older adults. J Am Geriatr Soc. 1997;45(8):954–958. doi: 10.1111/j.1532-5415.1997.tb02966.x. [DOI] [PubMed] [Google Scholar]
- 26.Eurostat. Quality of life: Facts and views. Published online 2015 https://ec.europa.eu/eurostat/documents/3217494/6856423/KS-05-14-073-EN-N/742aee45-4085-4dac-9e2e-9ed7e9501f23.
- 27. Ko Y, Boo S. Self-perceived health versus actual cardiovascular disease risks. Jpn J Nurs Sci. 2016;13(1):65–74. doi: 10.1111/jjns.12087. [DOI] [PubMed] [Google Scholar]
- 28. Greer JA, Pirl WF, Jackson VA, et al. Perceptions of health status and survival in patients with metastatic lung cancer. J Pain Symptom Manage. 2014;48(4):548–557. doi: 10.1016/j.jpainsymman.2013.10.016. [DOI] [PubMed] [Google Scholar]
- 29. Han B. Depressive symptoms and self-rated health in community-dwelling older adults: a longitudinal study. J Am Geriatr Soc. 2002;50(9):1549–1556. doi: 10.1046/j.1532-5415.2002.50411.x. [DOI] [PubMed] [Google Scholar]
- 30. Ruo B, Rumsfeld JS, Hlatky MA, Liu H, Browner WS, Whooley MA. Depressive symptoms and health-related quality of life: the Heart and Soul Study. JAMA. 2003;290(2):215–221. doi: 10.1001/jama.290.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep. 1995;18(6):425–432. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- 32. Furihata R, Uchiyama M, Takahashi S, et al. The association between sleep problems and perceived health status: a Japanese nationwide general population survey. Sleep Med. 2012;13(7):831–837. doi: 10.1016/j.sleep.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 33. Roth T, Coulouvrat C, Hajak G, et al. Prevalence and perceived health associated with insomnia based on DSM-IV-TR; International Statistical Classification of Diseases and Related Health Problems, Tenth Revision; and Research Diagnostic Criteria/International Classification of Sleep Disorders, Second Edition criteria: results from the America Insomnia Survey. Biol Psychiatry. 2011;69(6):592–600. doi: 10.1016/j.biopsych.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 34. Atallah N, Adjibade M, Lelong H, et al. How Healthy Lifestyle Factors at Midlife Relate to Healthy Aging. Nutrients. 2018;10(7):854. doi: 10.3390/nu10070854. Published 2018 Jun 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Elliott JC, Hasin DS, Des Jarlais DC. Perceived health and alcohol use in individuals with HIV and Hepatitis C who use drugs. Addict Behav. 2017;72:21–26. doi: 10.1016/j.addbeh.2017.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Peltzer K, Louw J, McHunu G, Naidoo P, Matseke G, Tutshana B. Hazardous and harmful alcohol use and associated factors in tuberculosis public primary care patients in South Africa. Int J Environ Res Public Health. 2012;9(9):3245–3257. doi: 10.3390/ijerph9093245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hassan MK, Joshi AV, Madhavan SS, Amonkar MM. Obesity and health-related quality of life: a cross-sectional analysis of the US population. Int J Obes Relat Metab Disord. 2003;27(10):1227–1232. doi: 10.1038/sj.ijo.0802396. [DOI] [PubMed] [Google Scholar]
- 38. Okosun IS, Choi S, Matamoros T, Dever GE. Obesity is associated with reduced self-rated general health status: evidence from a representative sample of white, black, and Hispanic Americans. Prev Med. 2001;32(5):429–436. doi: 10.1006/pmed.2001.0840. [DOI] [PubMed] [Google Scholar]
- 39. Douglas KR, Chan G, Gelernter J, et al. Adverse childhood events as risk factors for substance dependence: partial mediation by mood and anxiety disorders. Addict Behav. 2010;35(1):7–13. doi: 10.1016/j.addbeh.2009.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Monnat SM, Chandler RF. Long Term Physical Health Consequences of Adverse Childhood Experiences. Sociol Q. 2015;56(4):723–752. doi: 10.1111/tsq.12107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.CDC - BRFSS 2010. Centers for Disease Control and Prevention; [Accessed June 7, 2019]. https://www.cdc.gov/brfss/annual_data/annual_2010.htm. Published online 2010. [Google Scholar]
- 42. Ford DC, Merrick MT, Parks SE, et al. Examination of the Factorial Structure of Adverse Childhood Experiences and Recommendations for Three Subscale Scores. Psychol Violence. 2014;4(4):432–444. doi: 10.1037/a0037723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention. Measuring Healthy Days: Population assessment of health-related quality of life. US Department of Health and Human Services; Published online 2000 https://www.cdc.gov/hrqol/pdfs/mhd.pdf. [Google Scholar]
- 44. Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1–3):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 45. Hayes AF. Beyond Baron and Kenny: Statistical Mediation Analysis in the New Millennium. Commun Monogr. 2009;76(4):408–420. doi: 10.1080/03637750903310360. [DOI] [Google Scholar]
- 46. Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 47.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. 2e. The Guilford Press; 2018. [Google Scholar]
- 48. Roberts KC, Danoff-Burg S. Mindfulness and health behaviors: is paying attention good for you? J Am Coll Health. 2010;59(3):165–173. doi: 10.1080/07448481.2010.484452. [DOI] [PubMed] [Google Scholar]
- 49. Zvolensky MJ, Solomon SE, McLeish AC, et al. Incremental validity of mindfulness-based attention in relation to the concurrent prediction of anxiety and depressive symptomatology and perceptions of health. Cogn Behav Ther. 2006;35(3):148–158. doi: 10.1080/16506070600674087. [DOI] [PubMed] [Google Scholar]
- 50. Haug MR, Wykle ML, Namazi KH. Self-care among older adults. Soc Sci Med. 1989;29(2):171–183. doi: 10.1016/0277-9536(89)90165-2. [DOI] [PubMed] [Google Scholar]
- 51. Heinze JE, Kruger DJ, Reischl TM, Cupal S, Zimmerman MA. Relationships Among Disease, Social Support, and Perceived Health: A Lifespan Approach. Am J Community Psychol. 2015;56(3–4):268–279. doi: 10.1007/s10464-015-9758-3. [DOI] [PubMed] [Google Scholar]
- 52. Koppes LL, Dekker JM, Hendriks HF, Bouter LM, Heine RJ. Moderate alcohol consumption lowers the risk of type 2 diabetes: a meta-analysis of prospective observational studies. Diabetes Care. 2005;28(3):719–725. doi: 10.2337/diacare.28.3.719. [DOI] [PubMed] [Google Scholar]
- 53. Krokavcova M, van Dijk JP, Nagyova I, et al. Social support as a predictor of perceived health status in patients with multiple sclerosis. Patient Educ Couns. 2008;73(1):159–165. doi: 10.1016/j.pec.2008.03.019. [DOI] [PubMed] [Google Scholar]
- 54. Nicholas PK. Hardiness, self-care practices and perceived health status in older adults. J Adv Nurs. 1993;18(7):1085–1094. doi: 10.1046/j.1365-2648.1993.18071085.x. [DOI] [PubMed] [Google Scholar]
- 55.US Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. 8e. Published online December 2015 https://health.gov/dietaryguidelines/2015/guidelines.
- 56. Anstey KJ, Mack HA, Cherbuin N. Alcohol consumption as a risk factor for dementia and cognitive decline: meta-analysis of prospective studies. Am J Geriatr Psychiatry. 2009;17(7):542–555. doi: 10.1097/jgp.0b013e3181a2fd07. [DOI] [PubMed] [Google Scholar]
- 57. Reynolds K, Lewis B, Nolen JD, Kinney GL, Sathya B, He J. Alcohol consumption and risk of stroke: a meta-analysis. JAMA. 2003;289(5):579–588. doi: 10.1001/jama.289.5.579. [DOI] [PubMed] [Google Scholar]
- 58. Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342:d671. doi: 10.1136/bmj.d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Stice E, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: factors that predict magnitude of intervention effects. J Consult Clin Psychol. 2009;77(3):486–503. doi: 10.1037/a0015168. [DOI] [PMC free article] [PubMed] [Google Scholar]