Abstract
Introduction
Acute pulmonary embolism (PE) is a common diagnosis that can lead to death if left untreated. Computerized tomography pulmonary angiogram scan (CTPA) is the gold standard for diagnosis of PE. Utilization of CTPA is increasing in the emergency setting even when suspicion for PE is very low. While CTPA is helpful, radiation exposure, contrast reactions, and cost must be considered. D-dimer is a well-established, high sensitivity and low specificity laboratory test that can effectively rule out PE in low-risk patients when negative. The ADJUST-PE trial showed that there is a natural rise of D-dimer levels with age. This age adjusted D-dimer level is meant to prevent unnecessary CTPA exams in low suspicion patients. We hypothesize that there are a significant amount of unwarranted CTPA exams ordered at our community hospital that would not have been performed if the age adjusted D-dimer level were implemented.
Methods
During a four-month period we collected a list of patients 18 years of age and older who received a CTPA exam for initial evaluation of possible acute PE at our institution. The primary outcome was to evaluate the percentage of patients who received an imaging study despite a negative D-dimer collected prior to the study, using the age adjusted upper limit of normal based on the ADJUST-PE study.
Results
There were 734 CTPA exams that met our criteria in a four-month period. D-dimer levels were checked in 30.38% (223 of 734) of cases prior to imaging. Out of these 223 cases, 21.08% (47 of 223) were found to have negative age adjusted D-Dimer levels yet still received an imaging study. Out of these 47 cases, 44% (21 of 47) would have been positive using the traditional D-dimer threshold.
Conclusion
This study demonstrates that by adherence to the guideline-based pre-test algorithm and also utilizing the recommendations set forth by the ADJUST-PE study, approximately 21% of patients who undergo D-dimer testing would avoid unwarranted CT imaging. In addition to decreased radiation and contrast exposure, a significant amount of health care expense would be saved.
Keywords: pulmonary embolism, CTPA, D-dimer, diagnostic imaging, health expenditures
Introduction
Acute pulmonary embolism (PE) is the third most common cause of cardiovascular death, following acute coronary syndrome and stroke, attributing to approximately 100,000 deaths per year in the United States (US). PE is also the second most common cause of sudden unexpected death following acute coronary syndrome in outpatients.1,2 The incidence rate for the first episode of acute PE is 1 to 2 per 1,000 each year, with a rising incidence correlating directly to age, reaching 5 per 1,000 each year by the age of 80.3
The diagnosis of PE has more than doubled with the advent of the readily available computerized tomography pulmonary angiogram (CTPA) scan,3 which is considered the gold standard technique.4 As the greatest fraction of imaging services is performed for older patients,5 this upward trend can be expected to further increase as the baby-boomer generation enters retirement. To contribute further to the rising incidence of CTPA scans, studies have found that emergency clinicians hold a low threshold when deciding to order a CTPA even when the suspicion for PE is low in very low risk populations, possibly due to the legal consequences of missing a diagnosis.6–9
However helpful CTPA scans may be, they are not without their limitations including cost, contrast exposure and radiation exposure. Along with the increased frequency of imaging, the cost has also risen at about twice the rate of other health care technologies.10 Contrast reactions must be taken into consideration when ordering a PE protocol. Acute reactions to contrast varies from 15% for mild reactions to 0.2% for severe reactions.11,12 Additionally, radiation exposure is always of concern as it carries with it an increased risk of developing neoplasms.9,13 Medical imaging contributes to over 50% of the average total radiation dose to US residents today compared to less than 25% in 1980.14 Given the rising incidence, increasing cost, increased imaging utilization, medical side effects and an aging population with significant associated morbidity/mortality rates, this diagnosis has an ever-increasing health care burden.
Dr. Philip Wells, of the University of Ottawa, developed a validated algorithm called the “Wells Criteria” that differentiates patients suspected to have acute PE based on low or high probability, utilizing a negative D-dimer level to effectively rule out PE in the low probability group without the need for CTPA.15,16 However, studies have shown that the D-dimer increases with age due to comorbid conditions,16–20 thus limiting the yield and cost-effectiveness of the test in older patients while simultaneously promoting the overuse of CT imaging.15,21
Subsequently, the ADJUST-PE study demonstrated that due to the natural rise of D-dimer levels with age, an adjusted upper limit of normal (age ×10 ug/L with a lower limit of 500 ug/L) was equally effective in ruling out PE without further imaging in patients over the age of 50, safely excluding a larger percentage of at risk patients from undergoing unnecessary imaging.15,16
The goal of this retrospective study is to improve imaging stewardship by utilizing the age adjusted D-dimer to effectively rule out pulmonary emboli without the need for imaging in a community-based hospital. We hypothesize that there are a significant amount of unwarranted CT angiography-pulmonary embolism (CTA-PE) protocols ordered based on a D-dimer that is within normal limits based on the ADJUST-PE study.
Methods
At Memorial Health University Medical Center, a 612-bed academic medical center, we collected a list of all patients requiring CTA chest-PE protocols for a four-month period drawn between January 1 and April 30, 2017. Based on medical record numbers, all CTA chest-PE protocols from this time period were reviewed utilizing the picture archiving and communication system (PACS) (n=768). If the radiologist’s original final read was not clearly positive or negative, these studies were independently reviewed by an additional board-certified radiologist at the time of data collection (n=99). Additionally, if the exam quality was commented upon (i.e., body habitus, poor bolus timing, motion artifact), these were also submitted for independent review. The primary outcome was to evaluate the percentage of patients who received an imaging study despite a negative D-dimer collected prior to the study, using the age adjusted upper limit of normal based on the ADJUST-PE study.
Inclusion Criteria
All patients 18 years and older who were admitted to the hospital and received a CTA-PE protocol for initial evaluation of possible acute PE at MHUMC from January 1 to April 30, 2017 were included in the study.
Exclusion Criteria
The following patients were excluded from the study: patients who were undergoing imaging to re-evaluate a recent diagnosis of an acute PE (within the last 6 months), patients 17 years or younger and patients with known thrombus (i.e., DVT, upper extremity thrombus, etc.). Additionally, patients with non-diagnostic exams were excluded.
An exam was deemed to be non-diagnostic for this study if the central or segmental pulmonary branches were unable to be cleared of PE; this decision was made based on the 2016 CHEST guidelines, which determined that sub-segmental PEs are not typically clinically significant and anticoagulation treatment is argued against.22
Results
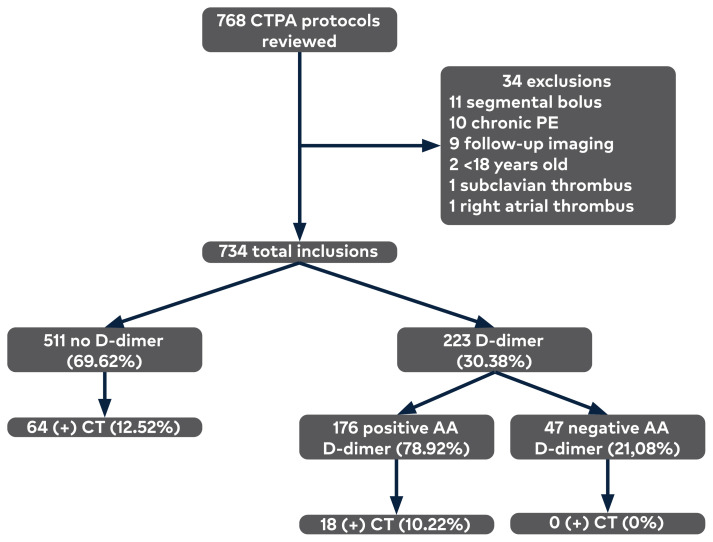
Overall, there were 768 CTA chest-PE protocols obtained in the initial study. Of these, 99 (13.48%) were reviewed by a second board-certified diagnostic radiologist and 34 were excluded, making the final included patient count 734. (Figure 1) The average age of patients undergoing CTA-chest PE protocol was 55.45 years old. Of the total CTPA scans, 11.17% (82 of 734) were positive for acute PE. Of the positive acute PE cases, the average D-dimer was 6475 ug/L. D-dimer levels were checked in 30.38% (223 of 734) of cases prior to imaging. Of these 223 cases, 21.08% (47 of 223) were found to have negative age-adjusted D-dimer levels yet still received an imaging study. Out of these 47 cases, 44% (21 of 47) would have been positive using the traditional threshold of 500ug/L without utilizing the age-adjusted D-dimer criteria. There were no false negative D-dimer cases in this study.
Figure 1.
Results showing a reduction in CT scans using age-adusted D-dimer levels.
AA=age adjusted
Discussion
Our study found that 44% of patients (n=21) with a positive D-dimer would have otherwise been negative if providers utilized the age-adjusted D-dimer as set forth by the ADJUST-PE trial, ultimately avoiding unwarranted imaging and improving health care savings. Furthermore, there were 26 cases that received a CTPA despite having a negative D-dimer based on the traditional cutoff of 500ug/L. This represents a total of 47 patients, or 21% of patients in a 4-month period who still received diagnostic CTPA imaging despite being screened negative with the age-adjusted D-dimer, a highly sensitive screening tool.
This study demonstrates the contrast between the well-studied, guideline-based algorithms and the actual clinical practice of diagnosing PE. By improving the adherence to the guideline–based pre-test algorithm, and also utilizing recommendations set forth according to the ADJUST-PE study, approximately 21% of patients who undergo D-dimer testing would avoid unwarranted CT imaging and contrast exposure. Additionally, a significant amount of health care expense would be saved. As of 2020, a CTA chest at this institution is priced at $4,851 according to MHUMC’s publically available detailed price report, not including specialist fees that are billed separately. Extrapolating these 47 patients with a negative AA D-dimer who underwent imaging over 12 months, this represents $911,988 in potential annual health care savings not including specialist fees.
There are several limitations of this study. This study could not determine a patient’s pre-test probability; therefore, patients were not stratified into risk groups based upon clinical suspicion by risk stratification tools such as the Wells criteria or PERC rule. This also is a retrospective study and did not prospectively enroll patients; only a subset of patients underwent D-dimer testing who underwent diagnostic imaging. This study also didn’t evaluate patients with clinical suspicion of PE who did not undergo CTPA imaging
Conclusion
Despite multiple extensive studies that validate pre-test probability, the utilization of CTPA remains high. This study illustrates that 21% of patients underwent unwarranted imaging based on the ADJUST-PE analysis. When this data is extrapolated over 12 months, approximately 188 patients at our community hospital will undergo unwarranted imaging with potential annual healthcare waste upwards of $900,000. With rising health care burden, limiting unnecessary imaging has strong implications when accounting for cost of imaging, length of stay, complication rates and incidental findings. The application of this study is to raise awareness to improve imaging stewardship and overall patient care in the local setting. As an example, The European Respiratory Journal has updated their guidelines for diagnosis and management of acute PE to include use of age adjusted D-dimer cut-offs.23 In the future, we hope that there will be widespread adherence to a clinical decision making algorithm that uses the age-adjusted D-dimer that will aid physicians in navigating the increasingly complex diagnostic work up and accurate ordering of appropriate imaging modalities.
Funding Statement
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity.
Footnotes
Conflicts of Interest
The authors declare they have no conflicts of interest.
The authors are employees of Memorial Health University Medical Center, a hospital affiliated with the journal’s publisher.
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
References
- 1. Kürkciyan I, Meron G, Sterz F, et al. Pulmonary embolism as a cause of cardiac arrest: presentation and outcome. Arch Intern Med. 2000;160(10):1529–1535. doi: 10.1001/archinte.160.10.1529. [DOI] [PubMed] [Google Scholar]
- 2. Manfredini R, Portaluppi F, Grandi E, Fersini C, Gallerani M. Out-of-hospital sudden death referring to an emergency department. J Clin Epidemiol. 1996;49(8):865–868. doi: 10.1016/0895-4356(96)00114-X. [DOI] [PubMed] [Google Scholar]
- 3.Cecil RL, Goldman L, Schafer AI. Goldman’s Cecil Medicine. 24th ed. Elsevier; 2012. [DOI] [Google Scholar]
- 4. Alderson PO, Martin EC. Pulmonary embolism: diagnosis with multiple imaging modalities. Radiology. 1987;164(2):297–312. doi: 10.1148/radiology.164.2.3299482. [DOI] [PubMed] [Google Scholar]
- 5. Keehan S, Sisko A, Truffer C, et al. Health spending projections through 2017: the baby-boom generation is coming to Medicare. Health Aff (Millwood) 2008;27(2):w145–w155. doi: 10.1377/hlthaff.27.2.w145. [DOI] [PubMed] [Google Scholar]
- 6. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293(21):2609–2617. doi: 10.1001/jama.293.21.2609. [DOI] [PubMed] [Google Scholar]
- 7.Taylor H. Doctors and other health professionals report that fear of malpractice has a big and mostly negative effect on clinical practice, uneccessary defensive medicine and openness to discussing medical errors. In: Taylor H, Leitman R, editors. Harris Interactive, Health Care News. 3. Vol. 2. 2003. pp. 1–5. [Google Scholar]
- 8. Kabrhel C, Matts C, McNamara M, Katz J, Ptak T. A highly sensitive ELISA D-dimer increases testing but not diagnosis of pulmonary embolism. Acad Emerg Med. 2006;13(5):519–524. doi: 10.1197/j.aem.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 9. Kline JA, Courtney DM, Kabrhel C, et al. Prospective multicenter evaluation of the pulmonary embolism rule-out criteria. J Thromb Haemost. 2008;6(5):772–780. doi: 10.1111/j.1538-7836.2008.02944.x. [DOI] [PubMed] [Google Scholar]
- 10. Iglehart JK. The new era of medical imaging--progress and pitfalls. N Engl J Med. 2006;354(26):2822–2828. doi: 10.1056/NEJMhpr061219. [DOI] [PubMed] [Google Scholar]
- 11. Namasivayam S, Kalra MK, Torres WE, Small WC. Adverse reactions to intravenous iodinated contrast media: a primer for radiologists. Emerg Radiol. 2006;12(5):210–215. doi: 10.1007/s10140-006-0488-6. [DOI] [PubMed] [Google Scholar]
- 12. Shujaat A, Shapiro JM, Eden E. Utilization of CT pulmonary angiography in suspected pulmonary embolism in a major urban emergency department. Pulm Med. 2013;2013:915213. doi: 10.1155/2013/915213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 14. Hendee WR, Becker GJ, Borgstede JP, et al. Addressing overutilization in medical imaging. Radiology. 2010;257(1):240–245. doi: 10.1148/radiol.10100063. [DOI] [PubMed] [Google Scholar]
- 15. Righini M, Van Es J, Den Exter PL, et al. Age-adjusted D-dimer cutoff levels to rule out pulmonary embolism: the ADJUST-PE study. JAMA. 2014;311(11):1117–1124. doi: 10.1001/jama.2014.2135. [DOI] [PubMed] [Google Scholar]
- 16. Righini M, Robert-Ebadi H. Diagnosis of acute Pulmonary Embolism. Diagnose der akuten Lungenembolie. Hamostaseologie. 2018;38(1):11–21. doi: 10.5482/HAMO-17-07-0023. [DOI] [PubMed] [Google Scholar]
- 17. Cadroy Y, Pierrejean D, Fontan B, Sié P, Boneu B. Influence of aging on the activity of the hemostatic system: prothrombin fragment 1+2, thrombin-antithrombin III complexes and D-dimers in 80 healthy subjects with age ranging from 20 to 94 years. Nouv Rev Fr Hematol. 1992;34(1):43–46. [PubMed] [Google Scholar]
- 18. Ginsberg JS, Brill-Edwards PA, Demers C, Donovan D, Panju A. D-dimer in patients with clinically suspected pulmonary embolism. Chest. 1993;104(6):1679–1684. doi: 10.1378/chest.104.6.1679. [DOI] [PubMed] [Google Scholar]
- 19. Perrier A, Desmarais S, Goehring C, et al. D-dimer testing for suspected pulmonary embolism in outpatients. Am J Respir Crit Care Med. 1997;156(2 Pt 1):492–496. doi: 10.1164/ajrccm.156.2.9702032. [DOI] [PubMed] [Google Scholar]
- 20. Righini M, Goehring C, Bounameaux H, Perrier A. Effects of age on the performance of common diagnostic tests for pulmonary embolism. Am J Med. 2000;109(5):357–361. doi: 10.1016/S0002-9343(00)00493-9. [DOI] [PubMed] [Google Scholar]
- 21. Ortiz J, Saeed R, Little C, Schaefer S. Age-adjusted D-dimer in the prediction of pulmonary embolism: does a normal age-adjusted D-dimer rule out PE? Biomed Res Int. 2017;2017:4867060. doi: 10.1155/2017/4867060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kearon C, Akl EA, Ornelas J, et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest. 2016;149(2):315–352. doi: 10.1016/j.chest.2015.11.026. [DOI] [PubMed] [Google Scholar]
- 23. Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS): The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC) Eur Respir J. 2019;54(3):1901647. doi: 10.1183/13993003.01647-2019. [DOI] [PubMed] [Google Scholar]