Abstract
Description
Health-system pharmacy leaders are tasked with determining key staffing decisions based on evolving patient care needs and present-day staffing capacity. A systematic approach to evaluate patient care needs, current model and potential gaps enables leaders to allocate resources in patient care need expansions or sudden fluctuations of patient volumes. Resource management, preparedness and ongoing maintenance form principles used by pharmacy leaders to create an optimal operational environment and elevate clinical pharmacy services. Use of this approach for multiple sites of care across a large network of health systems resulted in identification and improvement in pharmacist coverage and retention of clinical pharmacy services in a critical time of economic uncertainty. Hospitals working toward expanding to 24/7 pharmacist coverage may also consider this systematic approach to elucidate their needs.
Keywords: linical pharmacy service, pharmacists, personnel staffing, administration, leadership, health-system management, work schedule, efficiency
Health-system pharmacy leaders are tasked with determining key staffing decisions based on evolving patient care needs and present-day staffing capacity. A recent article by Gill and colleagues discussed the importance of having a staffing model that can progress to meet these needs.1 The COVID-19 pandemic is challenging pharmacy leaders to determine optimal staffing model plans in anticipation of fluctuating patient volumes and changing care demands. A critical step in the decision-making process is to understand the current pharmacy services staffing model. Systematically evaluating the current model and potential gaps enables leaders to allocate resources in patient care areas that need expansions or have sudden fluctuations of patient volumes.
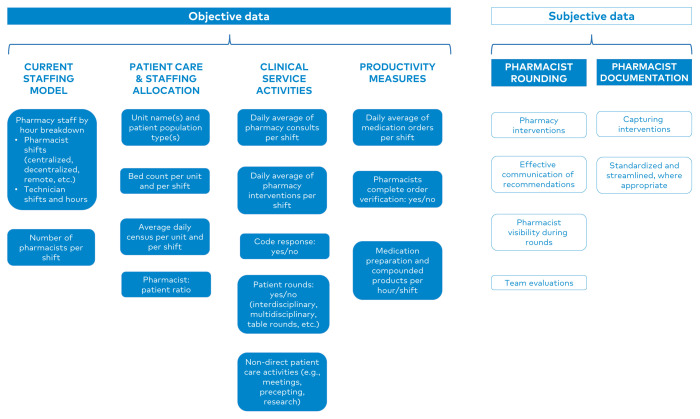
Resource management—through an ongoing review of people, processes and performance—is a key principle used by pharmacy leaders to create an optimal operational environment and elevate clinical pharmacy services. Consider using a data organization tool to map all components listed in Figure 1.
Figure 1.
A systematic approach for evaluating pharmacy services model. Evaluate all components for each shift type on weekdays and weekends.
Current Staffing Model
Operational and clinical pharmacy support can readily be identified by utilizing an organized approach to map out all pharmacy department shifts for each hour of weekdays and weekends. The next step is to create a new section for each category of shift type and catalogue all technician and pharmacist shifts with the scope of services provided for each shift. For example, a section describing weekday coverage may outline the number of pharmacists and technicians working during each hour of the day. Additional details can be added to designate specific shift types (e.g., day shift, overnight shift) and role types, such as operations, pharmacist or ICU pharmacist, as applicable.
Assessment of Patient Care And Staffing Allocation
The next key element of this approach entails understanding patient volume and populations. Consider including the items listed in Figure 1. Assess the patient census for all units and pharmacy team shifts, recognizing that a higher bed turnover rate in some units may provide additional insight on volumes not captured by a daily census. Determine the pharmacist-to-patient ratio, and evaluate its appropriateness relative to the patient acuity level per unit. Such ratios have been previously reported in the literature, including a recent cross-sectional electronic survey analysis by Newsome and colleagues. The authors found 1:16–20 to be the most common ratio in critical care settings based on responses from 185 critical care pharmacists.2
Clinical Service Activities
Apart from order verification, the scope of clinical pharmacy services may include activities such as consults, patient counseling, attending multidisciplinary rounds, answering drug information questions and other interventions. Reviewing non-direct patient care activities (e.g., committee or department meetings, teaching, precepting, research, quality improvement or other departmental projects) further illustrates a well-rounded picture of daily pharmacist duties. To develop a comprehensive depiction of the current staffing model, it may help to describe staff coverage for all activities such as clinical (including specialty coverage), operational and non-direct patient care activities in terms of an objective measurement, such as full-time equivalent (FTE) allocation. When evaluating each shift and unit, consider what, if any, ideal clinical pharmacy program elements are not being provided. In uncovering these gaps, staffing models can be enhanced to expand departmental service capacity.
Productivity Measures
Electronic health record systems, compounding software and clinical pharmacy workflow programs can provide a wealth of objective data on medication orders, verification, preparation and delivery. Evaluating the number of medication orders, clinical pharmacy interventions and compounded medication orders per shift can help leaders to understand the distribution of technician and pharmacist workload. Time-to-order verification or completion of medication orders, consults and clinical pharmacy interventions per unit can further provide context regarding the amount of time required of pharmacists and provision of timely delivery of care.
Pharmacist Rounding
Given that pharmacists are medication experts and serve as essential members of the patient care team, developing and maintaining collegial relationships is crucial. Pharmacy leaders should evaluate satisfaction with communication and services provided to the care team through periodic rounding. This element of performance may also be captured through informal discussions and team evaluations. Pharmacists who are readily accessible to providers, nurses and patients are able to build and maintain rapport.
Pharmacist Documentation
In addition to rounding, reviewing pharmacist documentation may provide insight on opportunities for optimization. Consider evaluation of a sample of patient care notes or consult notes to assess for alignment with appropriate standards and local policies. Identify opportunities to standardize and streamline documentation where appropriate. Evaluate whether any clinical pharmacy services provided are not being captured by current information systems. If so, determine whether current systems can be adapted to capture such activities. These interventions build upon the story that leaders can articulate to demonstrate pharmacy impact in improved patient safety, clinical excellence and unparalleled quality.
Leadership Review of the People, Processes and Performance
A comprehensive assessment of the aforementioned items should be performed with pharmacy leadership to identify opportunities and uncover where the current model can adapt to potential changes. Furthermore, an action plan should be developed in anticipation of decisions needed for evolving patient care needs. In an effort to elevate pharmacy services, this assessment can form the basis of a strategic plan to optimize, expand or better align staffing models with a future strategy.
Use of this systematic approach for multiple sites of care across a large health-system resulted in identification and improvement in pharmacist coverage and retention of clinical pharmacy services in a critical time of economic uncertainty. Such an approach may also serve as a framework for communicating a strategic vision in which pharmacy leaders are seeking to expand staffing models to meet the needs of a new service line or hospital expansion. Hospitals working towards expanding to 24/7 pharmacist coverage as recommended by the American Society of Health-System Pharmacists (ASHP)’s Practice Advance Initiative for 2030 may also consider this systematic approach to elucidate their needs.3
Funding Statement
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity.
Footnotes
Conflicts of Interest
The authors declare they have no conflicts of interest.
Drs. Burgess and Zambrano are employees of HCA Healthcare Clinical Operations Group, an organization affiliated with the journal’s publisher.
Dr. Heath is an employee of TriStar Centennial Medical Center, a hospital affiliated with the journal’s publisher.
This research was supported (in whole or in part) by HCA Healthcare and/or an HCA Healthcare affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
References
- 1. Gill TK, Thornton LM, Schroeder TR, et al. Implementation and evaluation of a team-based pharmacy practice model in a community health system. Am J Health Syst Pharm. 2019;76(7):470–477. doi: 10.1093/ajhp/zxy082. [DOI] [PubMed] [Google Scholar]
- 2. Newsome AS, Smith SE, Jones TW, Taylor A, Van Berkel MA, Rabinovich M. A survey of critical care pharmacists to patient ratios and practice characteristics in intensive care units. J Am Coll Clin Pharm. 2020;3(1):68–74. doi: 10.1002/jac5.1163. [DOI] [Google Scholar]
- 3. ASHP Practice Advancement Initiative 2030: new recommendations for advancing pharmacy practice in health systems. Am J Health Syst Pharm. 2020;77(2):113–121. doi: 10.1093/ajhp/zxz271. [DOI] [PubMed] [Google Scholar]