Purpose of review
To highlight the peculiarity of skin and soft tissue infections (SSTIs) in elderly patients and to provide useful elements for their optimal management.
Recent findings
In the COVID-19 era, early discharge from the hospital and implementation of outpatient management is of key importance.
Summary
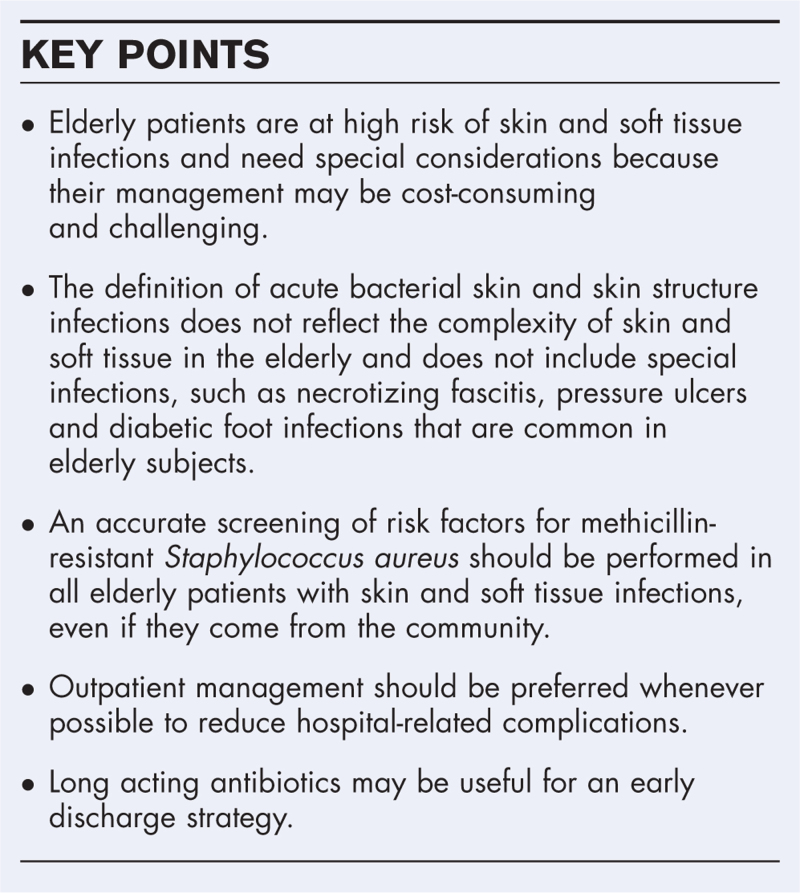
Elderly patients are at high risk of SSTIs due to several factors, including presence of multiple comorbidities and skin factors predisposing to infections. Clinical presentation may be atypical and some signs of severity, such as fever and increase in C-reactive protein, may be absent or aspecific in this patients population. An appropriate diagnosis of SSTIs in the elderly is crucial to avoid antibiotic overtreatment. Further studies should explore factors associated with bacterial superinfections in patients with pressure ulcers or lower limb erythema. Since several risk factors for methicillin-resistant Staphylococcus aureus (MRSA) may coexist in elderly patients, these subjects should be carefully screened for MRSA risk factors and those with high risk of resistant etiology should receive early antibiotic therapy active against MRSA. Physicians should aim to several objectives, including clinical cure, patient safety, early discharge and return to community. SSTIs in the elderly may be managed using long-acting antibiotics, but clinical follow-up is needed.
Keywords: atypical presentation, elderly, long-acting antibiotics, methicillin-resistant Staphylococcus aureus, skin and soft tissue infections, pressure ulcer
INTRODUCTION
The World Health Organization (WHO) predicts that the number of people aged >60 years will rise from 900 million to 2 billion between 2015 and 2050 [1]. Moreover, the Review on Antimicrobial Resistance, commissioned by the UK Government, argued that infections caused by antimicrobial resistance could kill 10 million people per year by 2050, more than the number of deaths caused by cancer [2]. Considering these two statements, it is easy to understand that in the next future elderly will represent the population at highest risk of infections and poor outcome from infectious diseases. Elderly patients have specific peculiarities that influence the presentations of infectious diseases and the response to treatments. Multiple comorbidities, changes in drug pharmacokinetics (PK) and pharmacodynamics (PD), and the presence of polypharmacy with the inherent risk of adverse drug reactions and drug–drug or drug–disease interactions make the management of infections very challenging in elderly patients [3▪]. Skin and soft tissue infections (SSTIs) are common in these subjects [4]. An increase of 22% of ambulatory care and a 40% of Emergency Department visits for SSTIs has been reported from 2000 to 2012 [5]. More specifically, SSTIs increased almost two-fold in older adults (>65 years of age) [5]. Moreover, the prevalence of SSTIs as cause of healthcare-associated infections ranges from less than 1% to about 20% according to different hospital settings [6], with the highest prevalence reported in acute care hospitals and long-term care facilities (10.9% and 17%, respectively) [7,8].
The clinical spectrum of skin infections is highly variable and ranges from mild infections to life-threatening diseases. The new definition of acute bacterial skin and skin structure infections (ABSSSI) has been released to allow homogeneity in patients included in clinical trials. However, some important disease entities are excluded from this definition. As a matter of fact, the guidance about ABSSSI management from Food and Drug Administration (FDA) does not address infections needing more complex treatment regimens, such as those resulting from animal or human bites, necrotizing fasciitis, diabetic foot infection, decubitus ulcer infection, myonecrosis, and ecthyma gangrenosum [9]. Some of these manifestations, such as decubitus ulcer infections are frequent in elderly patients. Moreover, elderly are usually excluded from randomized controlled trials [10]. Thus, in this category of patients using the term ABSSSI may have limitations and may be not appropriate. In this review we use the term SSTIs and discuss all type of skin infections, including those not included in the definition of ABSSSI.
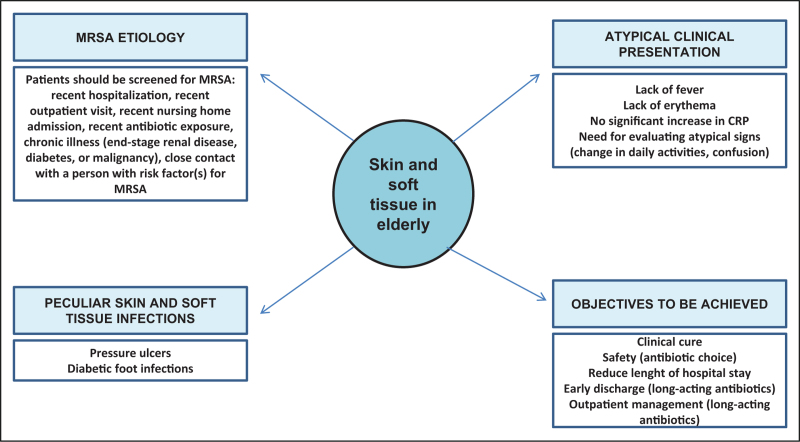
The aim of this document is to highlight the peculiarity of SSTIs in elderly patients and to provide useful elements for their optimal management. Figure 1 summarizes peculiar elements of elderly patients with skin and soft tissue infection highlighted in this review.
FIGURE 1.
Peculiar considerations in elderly patients with skin and soft tissue infections. CRP, C-reactive protein; MRSA, methicillin-resistant Staphylococcus aureus.
Box 1.
no caption available
PECULIAR RISK FACTORS
Elderly patients have several risk factors for SSTIs. Changes in skin consistence and immunosenescence predispose to SSTIs in elderly subjects. Dermal matrix alterations, atrophy, senescence of dermal cells such as fibroblasts, and decreased synthesis and accelerated break down of dermal collagen fibers are factors that contribute to an increased susceptibility to skin infections [11]. Elderly patients have a high frequency of conditions associated with skin fragility, such as edema and trauma.
Moreover, the presence of multiple comorbidities may impact on the progression and the course of SSTIs and represents a prognostic factor in elderly patients. Among comorbidities, the presence of heart failure, one of the most common conditions in the elderly, may be associated with peripheral edema that increases the risk of erisypela and cellulitis. It has been estimated that one third of adults aged 65 or older have diabetes mellitus [12]. A retrospective study conducted in the United States from 2005 to 2010 showed that abscesses, cellulitis, and other skin infections were more frequent in patients with diabetes mellitus [13]. Moreover, patients with diabetes mellitus had a fourfold risk of skin complications compared to nondiabetic patients. Several mechanisms, such as hyperglycemia, nonenzymatic glycation of proteins, impairment of the immune response and generation of reactive oxygen species are involved in the relationship between SSTIs and diabetes mellitus [14▪]. Elderly patients with diabetes are more likely to develop diabetes-related complications that further complicate the management of these patients and reduce the probabilities to achieve a clinical cure from a SSTI.
Finally, the presence of malnutrition plays a crucial role in elderly patients and increases the risk of SSTIs. Malnutrition is a very common problem that affects approximately 30–50% of all hospitalized patients. Among the elderly residents in long-term care facilities, malnutrition ranges from 12.5% to 78.9% [15]. Of note, among patients who are not malnourished on admission, about one third may become malnourished while in the hospital. This evenience increases the risk of SSTIs during the hospitalization of elderly patients and may represent a challenge since elderly with malnutrition have low chances of survive and recover from an infectious disease episode.
DIFFERENT ETIOLOGY COMPARED TO ADULTS?
Skin and soft tissue infections are usually caused by Streptococcus pyogenes and Staphylococcus aureus, including methicillin-resistant Staphylococcus aureus (MRSA) strains [16–19]. Less commonly identified bacteria include other Streptococcus species, Enterococcus faecalis, and Gram-negative bacteria [20,21]. MRSA has become a significant healthcare problem, especially in hospital settings. In the past decade, this organism has emerged in the community known as community-associated MRSA (CA-MRSA). Outbreaks of CA-MRSA infections have been increasingly reported worldwide with skin and soft tissue as the most common manifestation [22,23]. In the United States, the prevalence of SSTIs caused by CA-MRSA has been reported to range from 15% to 74% of all SSTIs [24]. Thus, the first consideration is to understand whether elderly patients have higher risk to have a SSTI caused by MRSA compared to adults. As a matter of fact, identification of risk factors is important in initial decisions about antibiotic selection. Risk factors for MRSA acquisition included the following factors: recent hospitalization, recent outpatient visit (within 12 months), recent nursing home admission (within 12 months), recent antibiotic exposure (range, 1–12 months), chronic illness (such as end-stage renal disease, diabetes, or malignancy), injection drug use, and close contact with a person with risk factor(s) for MRSA acquisition [25]. Living in an area with a high prevalence of CA-MRSA or admission to a hospital with a high prevalence of hospital acquired-MRSA is also considered a significant risk factor for MRSA colonization. Advancing age by itself is not considered a risk factor for MRSA infection. A study from UK studied the prevalence of MRSA in a general practice in London [26]. Among 258 older subjects living in their own home, MRSA was found in two participants (0.78%) and past history of MRSA was the only significant risk factor for MRSA colonization. However, elderly patients may have more frequently other risk factors for MRSA. Moreover, age >65 years is a significant risk factor for hospitalization and poor outcome due to a MRSA infection [27]. Hence, advancing age is indirectly linked to MRSA acquisition. Interestingly, a recent retrospective study conducted in patients >60 years old in Poland showed that the prevalence of MRSA is significantly different in categories of patients: 14.1% in young old (60–74 years), 19.5% in old old (75–85 years) and 26.7% in longevity (≥85 years old) [28].
Moreover, elderly patients residing in nursing homes appear to be at increased risk of colonization and infection by antibiotic resistant pathogens (such as MRSA). Marwick et al.[29] showed that the incidence of resistant bacteria is higher in nursing home patients compared to those reported in the control group (70% versus 36%, P = 0.026), and isolation of any resistant organism and receipt of initial inadequate antibiotic therapy are both factors independently associated with death.
These findings highlight some important considerations: first, elderly patients admitted to the hospital for SSTIs should be carefully screened for risk factors for CA-MRSA; second, the knowledge of updated epidemiological data about the CA-MRSA prevalence in elderly patients in specific areas is crucial to better decide empirical treatment for severe SSTIs; third, studies evaluating the prevalence of MRSA colonization and infections in nursing home residents are needed.
CLINICAL PRESENTATION
The clinical presentation of SSTIs in the elderly may differ from that of adults. Systemic symptoms and signs that are typically associated with infections in younger adults, such as fever, might be absent in older people [30]. Poor vascular supply, more common in elderly, can reduce the presence of erythema, warmth and tenderness that are typically associated with skin infections. Moreover, increase in C-reactive protein may be less pronounced in this category of patients due to impaired immune system and low capacity to respond to external stressors. Unfortunately, there is a paucity of guidance to help clinicians in illuminating these nonclassical presentations [31]. A systematic review of studies assessing the diagnostic accuracy of symptoms and signs of bacterial skin infections in subjects aged over 65 years showed that the presence of pressure sores, wounds and ulcers are helpful predictors of skin infections in these patients, while other skin manifestations such as warmth and erythema were not explored in clinical studies [31]. The diagnosis of bacterial skin infections based only on the presence of wounds, pressure sores or skin ulcers may increase the risk of unnecessary antimicrobial treatment and inducing antibiotic resistance. Similarly, positive blood cultures may be misleading and should be performed in selected patients to avoid overtreatment when potential contaminants are detected [32]. Clinical presentation of skin infections in the elderly should be further explored and the occurrence of atypical signs, such as confusion and changes in activities of daily living, should be studied in this patients’ population.
Another challenge in the management of SSTIs in the elderly is to efficiently differentiate cases that are potentially lifethreatening and warrant prompt hospitalization from those that are less severe and can be managed in an outpatient setting. The Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) scoring system has been developed to discriminate necrotizing fascitis from other severe soft-tissue infections [33]. However, its sensitivity ranges from 43.2% to 80.0% in different studies. This heterogeneity may be due to several factors, including differences in race, region or area, demographics (age, sex, body mass index), comorbid medical conditions (diabetes, immunosuppressant status) [34]. In elderly patients, some items of the LRINEC score may be not present (increase in C-reactive protein or white blood cell) while other items may be altered due to other conditions (hyponatremia, increase in creatinine and glucose values). Further studies are needed to validate existing scores or develop new dedicated scores for elderly with severe skin infections.
DON’T FORGET SPECIAL SKIN AND SOFT TISSUE INFECTIONS
Pressure ulcers are common in elderly patients, especially in those who live in long-term facilities. In community settings there is a lower rate of pressure ulcers occurrence due to less immobility and malnutrition from advanced chronic illness. The reported prevalence of pressure ulcers in the community is less than 2% of elderly individuals but progressively increase with age (4.2% in patients ≥85 years old) [35]. In the hospital setting, this data significantly increases with prevalence as high as 50% [36]. The majority of pressure ulcers occurring in hospitals develop during the initial 5 days of hospitalization and have an adverse impact on patient outcome, quality of life, length of hospital stay and healthcare costs. The management of this type of infections in the elderly is challenging. Etiology of infections of pressure ulcers differ from that of other type of skin infections. Most pressure ulcer infections are polymicrobial. Gram negative bacilli and anaerobes, such as such as Bacteroides fragilis, Peptostreptococcus, and Clostridium spp., are common causes of infections of sacral pressure ulcers.
Another specific type of SSTIs that may frequently occur in elderly patients is diabetic foot infections (DFIs). Diabetes mellitus is a common condition in elderly patients. The management of DFIs in elderly patients may be challenging because of specific etiology, increase in resistant organisms, need for frequent medications and challenge in antibiotic treatment. The presence of concomitant clinical conditions, such as kidney failure, and the polypharmacy should be carefully evaluated in the selection of the optimal antibiotic treatment in these patients.
SPECIAL CONSIDERATIONS FOR TREATMENT: CURRENT CHALLENGES AND FUTURE RESEARCH
Antibiotic treatment of elderly patients with SSTIs may be challenging and the therapeutic choice may differ from that of adult patients. Special considerations should be done.
The choice of antibiotic treatment in elderly patients needs special attention considering the presence of multiple comorbidities and the high risk of toxicity. Changes in drug PK/PD and the presence of polypharmacy with the inherent risk of adverse drug reactions and drug–drug or drug–disease interactions make the choice of the optimal antibiotic very challenging in these patients [3▪]. Appropriate antibiotic prescription, either in terms of drug choice or dosage, is of paramount importance among elderly, but balancing efficacy, safety, tolerability and development of antimicrobial resistance is difficult [3▪]. Table 1 summarizes antibiotics for SSTIs and their potential limitations in elderly patients. Some oral antibiotics, including fluoroquinolones and linezolid, are associated with high risk of adverse events in the elderly: fluoroquinolones may induce cardiac adverse events and delirium in the elderly, while linezolid may cause bone marrow suppression and thrombocytopenia. Intravenous antibiotics against MRSA should be carefully selected in these patients. Vancomycin is associated with high risk of kidney failure and should be avoided in patients with chronic kidney disease.
Table 1.
Antibiotics for skin and soft tissue infections and their use in elderly patients
| Antibiotic | Coverage | Route of administration | Considerations in elderly patients |
| Minocycline/doxicycline | Gram-positive bacteria | Oral | No adjustment for renal function |
| Clindamycin | Gram-positive bacteria, anaerobes | i.v. or oral | High risk of C. difficile infection |
| Fluoroquinolones | Gram-positive bacteria, Pseudomonas aeruginosa | i.v. or oral | Risk of cardiac side effects (prolonged QT, arrythmias) and risk of neurological adverse event (confusion, delirium) |
| Linezolid | Staphylococci (incl. MRSA) Enterococci (incl. VRE), Streptococci |
i.v. or oral | Risk of thrombocytopenia and myelosuppression |
| Glycopeptides (vancomycin/teicoplanin) | Gram-positive bacteria, Staphylococci (incl. MRSA), Enterococci (exl. VRE) | i.v. | Risk of kidney injury (vancomycin) |
| Daptomycin | Gram-positive bacteria | i.v. | Risk of rhabdomyolysis (consider drug-drug interactions) |
| Tigecycline | Active against many Gram-positive bacteria, Gram-negative bacteria (no Pseudomonas) and anaerobes | i.v. | Less tolerated (nausea, vomiting) |
| Ceftaroline | Active against Gram-positive bacteria, Enterobacteriaceae (no ESBL) No activity vs. Pseudomonas |
i.v. | |
| Dalbavancin | Active against Gram-positive bacteria Staphylococci (incl. MRSA) | i.v. | Advantage: Long acting, single administration |
| Oritavancin | Active against Gram-positive bacteria Staphylococci (incl. MRSA), Enterococci incl VRE |
i.v. | Advantage: Long acting, single administration |
i.v., intravenous; MRSA, methicillin-resistant S. aureus; VRE, vancomycin resistant Enterococci.
Another important aspect is the objective to be achieved. Two important objectives in these patients are early discharge and early switch-therapy. A short duration of antibiotic course may be favorable due to a potential reduction of adverse events and antibiotic resistance, and the opportunity to enhance patients’ compliance and to decrease healthcare costs. Early discharge is particularly important in elderly patients to allow return to common activities. Hospitalization in elderly patients may be associated with several complications. These conditions may include worsening of preexisting issues such as mobility and cognitive impairment, but may be also be represented by new onset complication developing during hospitalization, such as delirium, hospital-acquired incontinence, falls, pressure injuries and new functional impairments [37]. Moreover during the COVID-19 pandemic, avoiding hospitalization is important to guarantee patients’ safety and reduce hospital overcrowding [38,39].
Long-acting antibiotics, including dalbavancin and oritavancin, may be useful in these patients to avoid hospital admission and its related complications. Moreover, in patients with polypharmacy the use of single administration of dalbavancin or oritavancin increases the compliance and reduces the risk of failure. A recent study described the efficacy and safety of dalbavancin among elderly patients with different type of infections, including bones and joint infections, surgical site infection, and infective endocarditis. Clinical cure was confirmed for 79% of old patients at 1, 3, and 6 months. Six adverse events (9%) were reported after dalbavancin's administration, but each time in combination with other antibiotics [40,41].
The therapeutic management of an elderly patient with SSTIs should be individualized according to the patient's profile. Patients with clinical stability, stable comorbid illness and stable social situations may be early discharged and considered for a switch to oral therapy with an antimicrobial agent with a good safety profile and simple route of administration. Conversely, in a patient, who may be defined as “complex enough,’ ’ with multiple comorbidities, polypharmacy, need for intravascular devices for drug administration, the objective should be treatment simplification [42▪▪]. These patients may be candidates to long-acting antibiotics also in the Emergency Department to allow early return to community. Outpatients management with the possibility to complete the follow-up of patients who received long-acting antibiotics and are early discharged should be implemented.
CONCLUSION
Elderly patients have peculiar characteristics and the management of infectious diseases may be challenging in this patients population. The term ABSSSIs does not reflect the complexity of skin infections in elderly patients. Some entities, such as pressure ulcers and decubitus, occur frequently in these patients and need special awareness. Most elderly patients are characterized by multiple comorbidities and high risk for polypharmacy interactions. An accurate identification of patients at risk for infections caused by difficult-to-treat microorganisms such as MRSA is necessary, as well as a correct management including the early empirical administration of an active antibiotic therapy. The choice of antibiotic therapy should take in account various factors, including safety of the delivered drugs, interactions, patient profile, and possibility of permitting an early discharge, thus minimizing the costs of hospitalization. The use of long-acting antibiotics should be evaluated in these patients to avoid hospitalization and its related complications. Future research should focus on atypical presentation of SSTIs in the elderly and on the identification of patients who need antibiotic therapy and avoid antibiotic misuse. The discrimination of contamination or colonization and the presence of bacterial superinfection in patients with special SSTI such as pressure ulcers, is crucial in these cases and specific diagnostic work-up should be developed. Moreover, outpatient management should be strengthened and stakeholders and institution should be involved to implement this outpatient care.
Acknowledgements
None.
Financial support and sponsorship
None.
Conflicts of interest
Giusy Tiseo declare honoraria for educational meetings by Shionogi. Marco Falcone received unconditional grants/or speaker honoraria from MSD, Angelini, Shionogi, Pfizer, Menarini, Termo-Fisher, Gilead and Nordic Pharma. Declared conflicts of interest are outside the submitted work and did not affect the scientific objectivity of this review.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.World Health Organization (WHO). 10 facts on ageing and the life course. Geneva, Switzerland: WHO; 2012. Available at: https://www.who.int/news-room/fact-sheets/detail/10-facts-on-ageing-and-health [Accessed 6 December 2022]. [Google Scholar]
- 2.O’Neill J. Tackling drug-resistant infections globally: final report and recommendations. London: Review on Antimicrob Resistance; 2016. [Google Scholar]
- 3▪.Falcone M, Paul M, Tiseo G, et al. Considerations for the optimal management of antibiotic therapy in elderly patients. J Glob Antimicrob Resist 2020; 22:325–333. [DOI] [PubMed] [Google Scholar]; This review summarized special considerations that should be done in elderly patients who need antibiotics.
- 4.Laube S. Skin infections and ageing. Ageing Res Rev 2004; 3:69–89. [DOI] [PubMed] [Google Scholar]
- 5.Tun K, Shurko JF, Ryan L, Lee GC. Age-based health and economic burden of skin and soft tissue infections in the United States, 2000 and 2012. PLoS One 2018; 13:e0206893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cristina ML, Spagnolo AM, Giribone L, et al. Epidemiology and prevention of healthcare-associated infections in geriatric patients: a narrative review. Int J Environ Res Public Health 2021; 18:5333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cairns S, Reilly J, Stewart S, et al. The prevalence of healthcare-associated infection in older people in acute care hospitals. Infect Control Hosp Epidemiol 2011; 32:763–767. [DOI] [PubMed] [Google Scholar]
- 8.Serrano M, Barcenilla F, Limón E, et al. Prevalence of healthcare-associated infections in long-term care facilities in Catalonia. VINCat Program. Enferm. Infect Microbiol Clin 2017; 35:505–510. [DOI] [PubMed] [Google Scholar]
- 9.Guidance for industry acute bacterial skin and skin structure infections: developing drugs for treatment. Available at: https://www.fda.gov/files/drugs/published/Acute-Bacterial-Skin-and-Skin-Structure-Infections---Developing-Drugs-for-Treatment.pdf [Accessed 6 December 2022]. [Google Scholar]
- 10.Prendki V, Tau N, Avni T, et al. A systematic review assessing the under-representation of elderly adults in COVID-19 trials. BMC Geriatr 2020; 20:538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee H, Hong Y, Kim M. Structural and functional changes and possible molecular mechanisms in aged skin. Int J Mol Sci 2021; 22:12489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Menke A, Casagrade S, Geiss L, Cowie CC. Prevalence and trends in diabetes among adults in the United States, 1988−2012. JAMA 2015; 314:1021–1029. [DOI] [PubMed] [Google Scholar]
- 13.Suaya JA, Eisenberg DF, Fang C, Miller LG. Skin and soft tissue infections and associated complications among commercially insured patients aged 0–64 years with and without diabetes in the US. PLoS One 2013; 8:e60057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14▪.Falcone M, Meier JJ, Marini MG, et al. Diabetes and acute bacterial skin and skin structure infections. Diabetes Res Clin Pract 2021; 174:108732. [DOI] [PubMed] [Google Scholar]; This study is of special interest because it discusses about the mutual relationship between diabetes and acute bacterial skin and skin structure infections. The complex management of patients with diabetes mellitus and skin infections is highlighted and practical suggestions provided to clinicians.
- 15.Neloska L, Damevska K, Nikolchev A, et al. The association between malnutrition and pressure ulcers in elderly in long-term care facility. Open Access Maced J Med Sci 2016; 4:423–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Venditti M, Falcone M, Micozzi A, et al. Staphylococcus aureus bacteremia in patients with hematologic malignancies: a retrospective case–control study. Haematologica 2003; 88:923–930. [PubMed] [Google Scholar]
- 17.Kaye KS, Petty LA, Shorr AF, Zilberberg MD. Current epidemiology, etiology, and burden of acute skin infections in the United States. Clin Infect Dis 2019; 68:S193–S199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Campanile F, Bongiorno D, Falcone M, et al. Changing Italian nosocomial-community trends and heteroresistance in Staphylococcus aureus from bacteremia and endocarditis. Eur J Clin Microbiol Infect Dis 2012; 31:739–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Falcone M, Serra P, Venditti M. Serious infections due to methicillin-resistant Staphylococcus aureus: an evolving challenge for physicians. Eur J Intern Med 2009; 20:343–347. [DOI] [PubMed] [Google Scholar]
- 20.Giuliano S, Rubini G, Conte A, et al. Streptococcus anginosus group disseminated infection: case report and review of literature. Infez Med 2012; 20:145–154. [PubMed] [Google Scholar]
- 21.Falcone M, Tiseo G, Durante-Mangoni E, et al. Risk factors and outcomes of endocarditis due to nonhacek gram-negative bacilli: data from the prospective multicenter Italian endocarditis study cohort. Antimicrob Agents Chemother 2018; 62:e02208–e2217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miller LG, Perdreau-Remington F, Bayer AS, et al. Clinical and epidemiologic characteristics cannot distinguish community-associated methicillin-resistant Staphylococcus aureus infection from methicillin-susceptible S. aureus infection: a prospective investigation. Clin Infect Dis 2007; 44:471–482. [DOI] [PubMed] [Google Scholar]
- 23.Zetola N, Francis JS, Nuermberger EL, Bishai WR. Community-acquired meticillin-resistant Staphylococcus aureus: an emerging threat. Lancet Infect Dis 2005; 5:275–286. [DOI] [PubMed] [Google Scholar]
- 24.Moran GJ, Krishnadasan A, Gorwitz RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med 2006; 355:666–667. [DOI] [PubMed] [Google Scholar]
- 25.Salgado CD, Farr BM, Calfee DP. Community-acquired methicillin-resistant Staphylococcus aureus: a meta-analysis of prevalence and risk factors. Clin Infect Dis 2003; 36:131–139. [DOI] [PubMed] [Google Scholar]
- 26.Maudsley J, Stone SP, Kibbler CC, et al. The community prevalence of methicillin-resistant Staphylococcus aureus (MRSA) in older people living in their own homes: implications for treatment, screening and surveillance in the UK. J Hosp Infect 2004; 57:258–262. [DOI] [PubMed] [Google Scholar]
- 27.Cuervo G, Gasch O, Shaw E, et al. Clinical characteristics, treatment and outcomes of MRSA bacteraemia in the elderly. J Infect 2016; 72:309–316. [DOI] [PubMed] [Google Scholar]
- 28.Pomorska-Wesołowska M, Różańska A, Natkaniec J, et al. Longevity and gender as the risk factors of methicillin-resistant Staphylococcus aureus infections in southern Poland. BMC Geriatr 2017; 17:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marwick C, Santiago VH, McCowan C, et al. Community acquired infections in older patients admitted to hospital from care homes versus the community: cohort study of microbiology and outcomes. BMC Geriatr 2013; 13:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.van Duin D. Diagnostic challenges and opportunities in older adults with infectious diseases. Clin Infect Dis 2012; 54:973–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gbinigie OA, Ordóñez-Mena JM, Fanshawe T, et al. Limited evidence for diagnosing bacterial skin infections in older adults in primary care: systematic review. BMC Geriatr 2019; 19:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tiseo G, Mazzone A, Falcone M. Identifying patients with acute bacterial skin and skin structure infection who need blood cultures. Intern Emerg Med 2019; 14:203–206. [DOI] [PubMed] [Google Scholar]
- 33.Wong CH, Khin LW, et al. The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: a tool for distinguishing necrotizing fasciitis from other soft tissue infections. Crit Care Med 2004; 32:1535–1541. [DOI] [PubMed] [Google Scholar]
- 34.Wu H, Liu S, Li C, Song Z. Modified Laboratory Risk Indicator for Necrotizing Fasciitis (m-LRINEC) score system in diagnosing necrotizing fasciitis: a nested case–control study. Infect Drug Resist 2021; 14:2105–2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Margolis DJ, Knauss J, Bilker W, Baumgarten M. Medical conditions as risk factors for pressure ulcers in an outpatient setting. Age Ageing 2003; 32:259–264. [DOI] [PubMed] [Google Scholar]
- 36.Jaul E, Barron J, Rosenzweig JP, Menczel J. An overview of co-morbidities and the development of pressure ulcers among older adults. BMC Geriatr 2018; 18:305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mudge AM, McRae P, Hubbard RE, et al. Hospital-associated complications of older people: a proposed multicomponent outcome for acute care. J Am Geriatr Soc 2019; 67:352–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Prendki V, Tiseo G, Falcone M. ESCMID Study Group for Infections in the Elderly (ESGIE). Caring for older adults during the COVID-19 pandemic. Clin Microbiol Infect 2022; 28:785–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Andreoni M, Bassetti M, Corrao S. The role of dalbavancin for Gram positive infections in the COVID-19 era: state of the art and future perspectives. Expert Rev Anti Infect Ther 2021; 19:1125–1134. [DOI] [PubMed] [Google Scholar]
- 40.Wackenheim C, Le Maréchal M, Pluchart H, et al. Dalbavancin in clinical practice: a particular place for the elderly? Eur J Clin Microbiol Infect Dis 2022; 41:977–979. [DOI] [PubMed] [Google Scholar]
- 41.Cacopardo B, Cattaneo D, Cortese F, et al. Role of dalbavancin as combination therapy: evidence from the literature and clinical scenarios. Expert Rev Anti Infect Ther 2022; 20:997–1004. [DOI] [PubMed] [Google Scholar]
- 42▪▪.Falcone M, Concia E, Giusti M, et al. Acute bacterial skin and skin structure infections in internal medicine wards: old and new drugs. Intern Emerg Med 2016; 11:637–648. [DOI] [PubMed] [Google Scholar]; In this review, the authors proposed a clinical approach to patients with multiple comorbidities hospitalized for skin infections, providing two different approach for two patients profiles: the good enough and the complex enough patient.