Abstract
Aims
High salt intake is common and contributes to poor cardiovascular health. Urinary sodium excretion correlates directly with glucocorticoid excretion in humans and experimental animals. We hypothesized that high salt intake activates the hypothalamic–pituitary–adrenal axis activation and leads to sustained glucocorticoid excess.
Methods and results
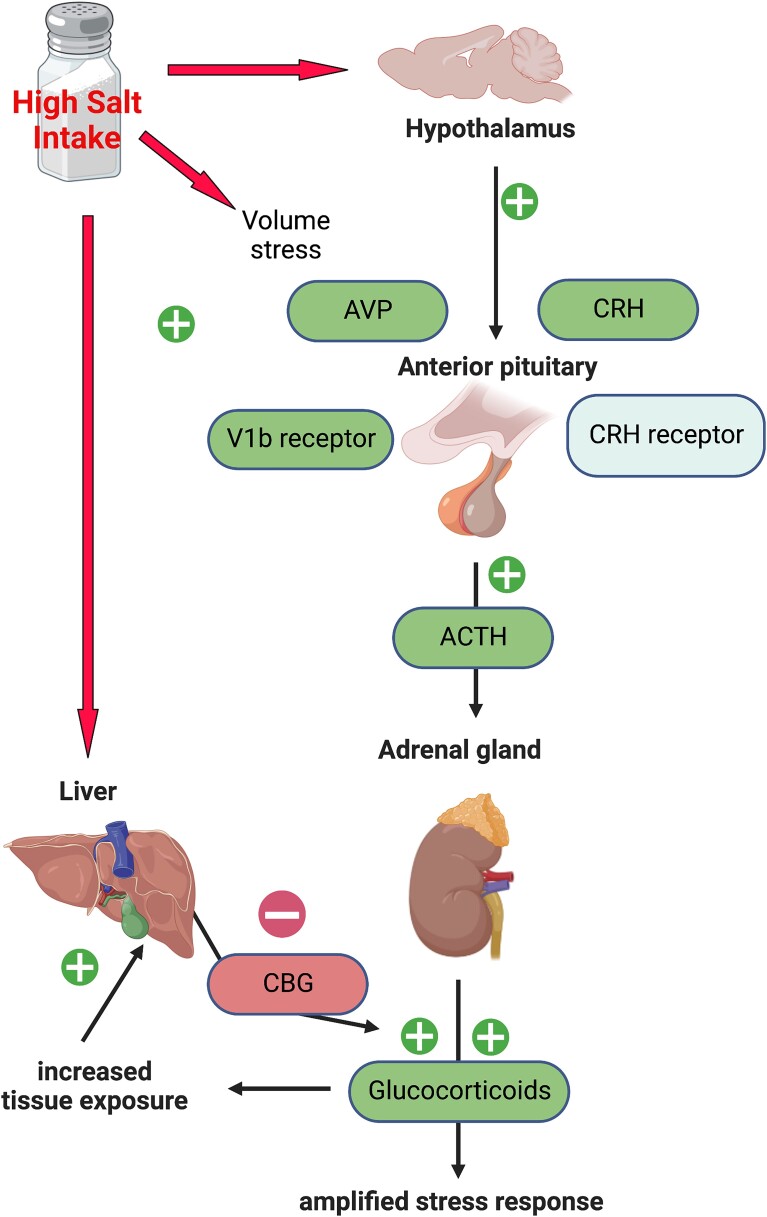
In male C57BL/6 mice, high salt intake for 2–8 weeks caused an increase in diurnal peak levels of plasma corticosterone. After 2 weeks, high salt increased Crh and Pomc mRNA abundance in the hypothalamus and anterior pituitary, consistent with basal hypothalamic–pituitary–adrenal axis activation. Additionally, high salt intake amplified glucocorticoid response to restraint stress, indicative of enhanced axis sensitivity. The binding capacity of Corticosteroid-Binding Globulin was reduced and its encoding mRNA downregulated in the liver. In the hippocampus and anterior pituitary, Fkbp5 mRNA levels were increased, indicating increased glucocorticoid exposure. The mRNA expression of the glucocorticoid-regenerating enzyme, 11β-hydroxysteroid dehydrogenase Type 1, was increased in these brain areas and in the liver. Sustained high salt intake activated a water conservation response by the kidney, increasing plasma levels of the vasopressin surrogate, copeptin. Increased mRNA abundance of Tonebp and Avpr1b in the anterior pituitary suggested that vasopressin signalling contributes to hypothalamic–pituitary–adrenal axis activation by high salt diet.
Conclusion
Chronic high salt intake amplifies basal and stress-induced glucocorticoid levels and resets glucocorticoid biology centrally, peripherally and within cells.
Keywords: Stress, Cortisol, Glucocorticoid excess, Glucocorticoid receptor, Salt
Graphical Abstract
Graphical Abstract.
See the editorial comment for this article ‘Salty secrets of the brain: the link between stress, salt, and hypertension’, by A.H. Ludwig-Słomczyńska and T.J. Guzik, https://doi.org/10.1093/cvr/cvad071.
1. Introduction
The American Heart Association advocates a daily limit of 1500 mg Na (3.75 g salt) for most individuals, particularly those with hypertension.1 Daily salt intake in the United States of America, and most other countries, usually exceeds this threshold.2 In humans and experimental animals high salt intake induces abnormal physiological function of many organ systems and causes a range of poor health outcomes.3 This damaging effect of salt is most clearly seen in ‘salt-sensitive’ experimental models, i.e. those which display an exaggerated hypertensive response to high salt intake. Salt-sensitivity is also found in ∼30% of healthy humans and independently increases cardiovascular risk4 and mortality risk.5 Nevertheless, even in those people categorised as salt-resistant, high salt intake modifies organ function and accrual of incremental deficits over time will cause disease. Thus habitual dietary salt excess causes cardiovascular disease and may contribute to the development of autoimmunity,6 some cancers7 and cognitive impairment.8 High dietary salt clearly exerts a significant global health burden. Interventions to reduce intake improve outcomes.9 However, such reductions are difficult to achieve and sustain in the general population. Understanding how cell and organ physiology responds to chronic high salt intake offers an additional route to improve health across an array of diseases.
Our study focuses on glucocorticoids (cortisol in humans, corticosterone in rodents), powerful hormones which underpin many important cardiovascular, cognitive, immune, and metabolic cell functions. Glucocorticoids are not normally considered key regulators of salt balance. Nevertheless, observational studies in humans show a positive correlation between urinary free cortisol excretion and 24 h sodium excretion, taken to reflect salt intake.3,10–12 A small number of controlled sodium intake studies, typically lasting ∼7 days, have examined the relationship between salt intake and urinary excretion of glucocorticoids. Ranging from 8 to >600 subjects, these studies consistently report a direct relationship between dietary salt intake and urine cortisol excretion.13–19 A long-term balance study also found a positive relationship between salt intake and urinary cortisol excretion in healthy men enrolled in the MARS-500 spaceflight simulation programme.20 The direct association between salt intake and urinary glucocorticoid excretion has also been reported in mice19,21,22 and is exaggerated in mice with reduced expression of the glucocorticoid metabolizing enzyme 11β-hydroxysteroid dehydrogenase Type 2 (11βHSD2), which have salt-sensitive blood pressure.21
Based on these associations, we hypothesized that sustained high salt intake would activate the hypothalamic–pituitary–adrenal (HPA) axis. In male C57BL/6 mice, we find that salt intake increases basal and stress-induced corticosterone levels and alters aspects of peripheral glucocorticoid biology.
2. Methods
Experiments were performed between September 2018 and June 2022. Adult male C57BL/6 mice were commercially sourced (Charles River, UK) at age 10–12 weeks and maintained under controlled conditions of temperature (24 ± 1⁰C), humidity (50 ± 10% humidity) and light (lights on 7am to 7pm local time). Mice had ad libitum access to water and commercial rodent chow. The control diet contained 0.3% sodium and 0.7% potassium by weight [RM1, SDS Diets, United Kingdom (UK)]; the high salt diet contained 3% sodium and 0.6% potassium by weight (RM 3% Na+ SY, SDS Diets, UK). Mice were randomized into treatment groups and experiments performed with a single blinding to group allocations. No anaesthetic agents were used in these experiments and animals were euthanised either by cervical dislocation or by decapitation. All procedures conform to the guidelines from Directive 2010/63/EU of the European Parliament on the protection of animals used for scientific purposes. All experiments were performed in accordance with the UK Animals (Scientific procedures) Act under a UK Home Office Project Licence to the lead investigator (MAB) following ethical review by the University.
See Supplementary material online for Expanded Methods.
2.1. Basal HPA axis activity
Corticosterone was measured at the diurnal nadir (7am) and peak (7pm) in mice fed either high salt or control diet for up to 8 weeks. At the end of these experiments, mice were killed between 7 and 8am, and tissue was taken for mRNA measurements.
2.2. HPA axis response to stress
Each animal mouse was removed from its home cage between 7 and 8am and blood collected by tail venesection to give baseline corticosterone. Each mouse was then restrained in a Plexiglas tube for 15 min and another blood sample taken to measure the peak corticosterone response. Each mouse was then returned to its home cage. The protocol permitted collection of one further blood sample from each mouse, taken at either 30−, 60− or 90-min post-restraint stress.
2.3. Corticosterone, copeptin and aldosterone measurement
Corticosterone was extracted from tail venesection samples and measured by commercial ELISA kit (ADI-900-097; Enzo Life Sciences, UK). For copeptin and aldosterone, mice were euthanized by decapitation (between 7am and 8am), trunk blood was collected on ice, and separated by centrifugation and stored at −20⁰C. After a single thaw of all samples, copeptin (CEA365Mu; Cloud-Clone Corp., USA) and aldosterone (ADI-900-173; Enzo Life Sciences, UK) were measured by commercial ELISA.
2.3.1. Copeptin and aldosterone measurement
Mice were euthanized by decapitation (between 7am and 8am), trunk blood was collected on ice, and separated by centrifugation and stored at −20⁰C. After a single thaw of all samples, copeptin (CEA365Mu; Cloud-Clone Corp., USA) and aldosterone (ADI-900-173; Enzo Life Sciences, UK) were measured by commercial ELISA.
2.4. Corticosterone-binding globulin binding capacity
This was measured using a saturation binding assay, as described,23 with the maximal binding capacity (Bmax), estimated using non-linear regression.
2.5. Quantitative polymerase chain reaction
mRNA abundance in tissues was measured by quantitative RT-PCR using the Universal Probe Library (Roche, UK) or PowerUp SYBR Green (Applied Biosystems, UK). Primer sequences and probe numbers are given in Supplementary material online, Table S1. The results were normalized to the mean concentration of reference genes. These were Actb and Tbp for adrenal, hippocampus and anterior pituitary; Actb and Hprt for liver; Actb and Rn18s for kidney cortex/medulla and aorta; Actb and Gapdh for heart; Gapdh and Tbp for hypothalamus. Before normalization, the concentration of mRNA for reference genes in hypothalamus, liver, kidney and heart from mice fed control diet (n = 8) and mice fed high salt diet for 2 weeks (n = 8) was compared by Mann–Whitney U-test. There was no effect of salt intake: P-values ranged from P = 0.181 to P = 0.993
2.6. Quantification and statistical analysis
Group size estimates were based on pilot experiments demonstrating an increase in peak plasma corticosterone after 2 weeks of high salt intake. Power analysis was performed using G*Power v3.19 Software,24 using a main effect alpha level of P < 0.05 and 90% power. No animals were excluded from study, but some samples subsequently failed quality control in assay (e.g. for RNA quality/abundance; blood sample volume) and retrospective power analysis on data sets was therefore performed. In final data sets, individual points are shown along with group mean ± SD. Statistical analysis was performed using GraphPad Prism v8.4 Software. The distribution of data sets was assessed using the Shapiro–Wilk normality test. Normally distributed data sets were analysed by t-test, one-way ANOVA or two-way ANOVA, with or without repeated measures, as stated in the figure legends. For ANOVA, Holm–Sidak post-tests were used for planned comparisons. For data that did not pass normality testing, non-parametric analysis was carried out using Wilcoxon test. The sample number (n) and statistical analysis details used are stated in the figure legends; absolute P-values for planned comparisons are reported.
3. Results
3.1. High salt activates the HPA axis to increase corticosterone synthesis
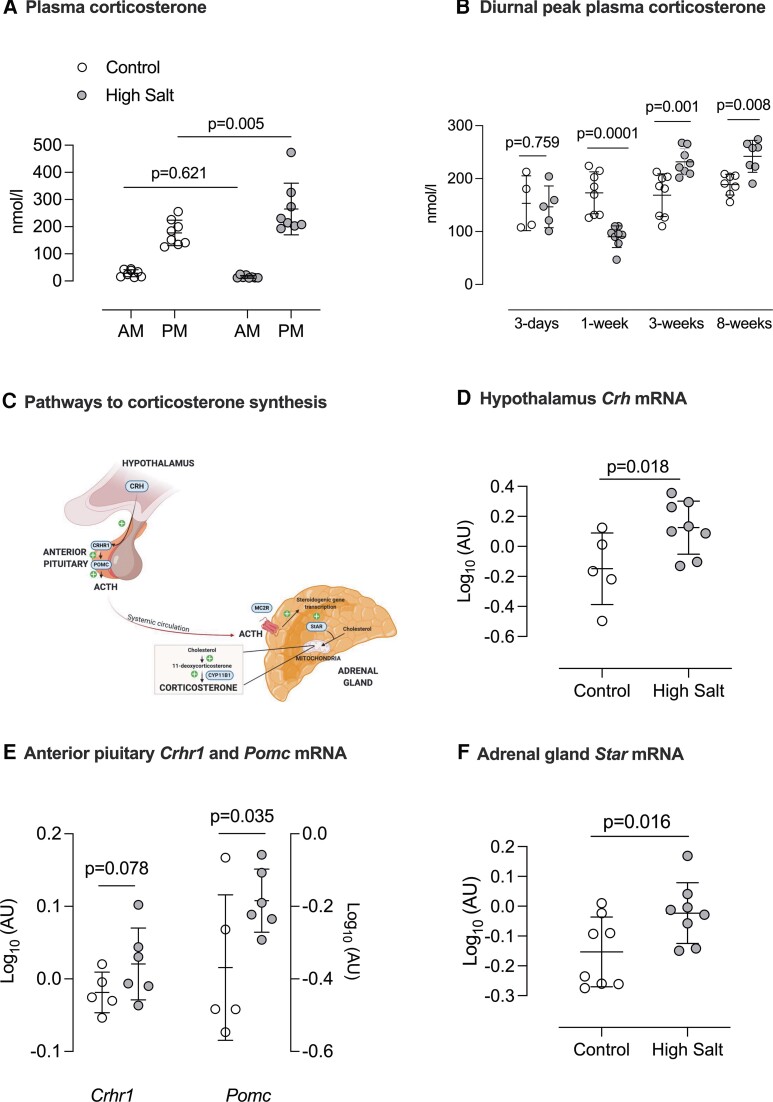
The hypothesis that high salt intake activated the HPA axis was initially tested in n = 8 mice, sampling blood at 7am and 7pm to capture the diurnal nadir and peak of corticosterone. Measurements were made in each mouse on control diet (0.3% Na) and again after 2 weeks of high salt (3% Na). High salt intake significantly increased peak plasma corticosterone, without affecting the nadir (Figure 1A). We next examined the time course, measuring peak corticosterone in separate groups of mice maintained on high salt or control diets for 3 days, 1−, 3−, and 8-weeks (Figure 1B). The effect of salt intake was biphasic: at 1-week, peak corticosterone was suppressed, after which high salt intake increased peak corticosterone levels, and this stimulatory effect was sustained.
Figure 1.
Activation of HPA axis after high salt intake. (A) Plasma corticosterone measured at 7am (diurnal nadir) and 7pm (diurnal peak) in male C57BL/6 mice (n = 8) first on a 0.3% Na diet (control, open circles) and again after 14 days on 3% Na diet (high salt; closed circles). Individual values are shown with group mean ± SD; statistical comparison was two-way repeated measures ANOVA for the main effects of time of day (P < 0.0001) and diet (P = 0.071) and the interaction (P = 0.016); P-values for planned comparisons (Holm–Sidak) are given. (B) The effect of salt diet on diurnal peak plasma corticosterone was measured in separate groups of mice fed either control (open circles) or high salt diet (closed circles) for 3 days (n = 4/5), 1 week (n = 8/8), 3 weeks (n = 8/8) or 8 weeks (n = 8/8) of either. Individual values are shown with group mean ± SD; statistical comparison was two-way ANOVA for the main effects of ‘diet’ (P = 0.476) and ‘duration’ (P < 0.0001) and the interaction (P < 0.0001); P-values for planned comparisons (Holm–Sidak) are shown. (C) Schematic highlighting key components of HPA axis activation that were then measured at mRNA level in tissue taken from different C57BL/6 mice fed either 0.3% Na (open circles n = 8) or 3%Na (closed circles n = 8) for 2 weeks. For hypothalamus and anterior pituitary, n = 5 for control diet and n = 6 for high salt diet following exclusion of samples because of poor mRNA yield/quality. (D) Crh (corticosterone releasing hormone) mRNA in hypothalamus (E) Crhr1 (CRH receptor and Pomc (pro-opiomelanocortin) mRNA in anterior pituitary; and (F) adrenal gland Star (Steroidogenic Acute Regulatory protein) mRNA. Individual values are shown with group mean ± SD; statistical comparison was by unpaired t-test with P-values as indicated.
Using tissue taken from the 2-week high salt group, we examined mRNA expression for key genes leading to increased corticosterone production (Figure 1C). Hypothalamic Crh expression (encoding corticotropin releasing hormone; CRH) was elevated (Figure 1D). The mRNA abundance of the anterior pituitary CRH receptor, Crhr1, tended to be higher in the high salt group and pro-opiomelanocortin, the precursor of adrenocorticotropic hormone (ACTH), was significantly increased by high salt intake (Figure 1E). Adrenal gland weight and the mRNA levels of 11β-hydroxylase and the ACTH receptor were not changed by high salt diet (see Supplementary material online, Figure S1) but mRNA encoding steroidogenic acute regulatory protein (StAR) was increased (Figure 1F). StAR expression, the regulated rate-limiting step for adrenal steroid biosynthesis, is increased chronically by ACTH.25 ACTH can also stimulate aldosterone excretion26 but here we found broad suppression of the renin–aldosterone system by high salt intake: mRNA for hepatic angiotensinogen (Agt), kidney renin (Ren) and adrenal gland aldosterone synthase (Cyp11b2) were all reduced and plasma aldosterone was supressed. Additionally, renal mRNA expression of the mineralocorticoid receptor was significantly downregulated in mice on a high salt diet (see Supplementary material online, Figure S2).
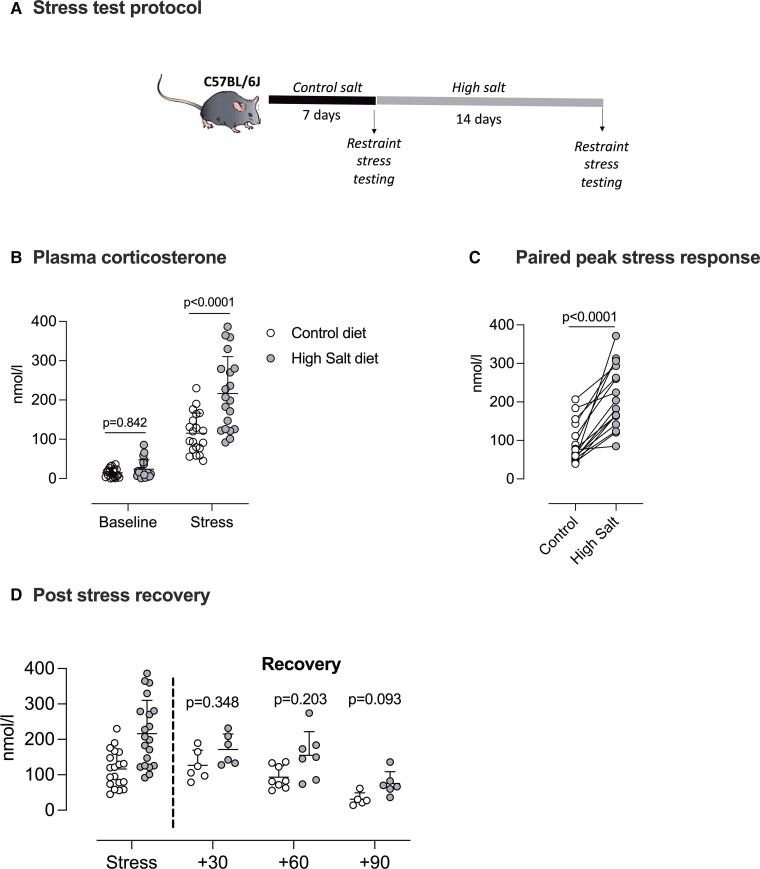
In a different group of mice (n = 20), we assessed the effect of high salt intake on the HPA axis response to a 15 min restraint stress (Figure 2A). On control diet, restraint stress increased plasma corticosterone in all mice, with a group average increase of ∼90 nmol/L (Figure 2B). After 2 weeks of high salt intake, the peak stress response was amplified in 16 of these mice (Figure 2C), and the group mean response approximately doubled.
Figure 2.
High salt intake amplifies the stress response. (A) protocol for measuring the stress response in male C57BL/6 mice (n = 20) fed 0.3% Na diet (control; open circles) and again after 2 weeks on a 3% Na diet (high salt; closed circles). (B) Plasma corticosterone in samples taken at 8am (baseline) and again after 15 min of tube restraint (Stress). Analysis was two-way ANOVA with repeated measures for the main effects of ‘stress-response’ (P < 0.0001) and ‘diet’ (P = 0.0006) and the interaction (P = 0.0014); P-values for planned comparisons (Holm–Sidak) are given. (C) The paired peak stress response in each mouse (n = 20), analysed by paired t-test. (D) The corticosterone recovery from stress was measured at either 30 (n = 6/6), 60 (n = 8/7) or 90 minutes (n = 5/6) following release from the restraint tube. Analysis was two-way ANOVA with repeated measures for the main effects of ‘time’ and ‘diet’ and the interaction; P-values for planned comparisons (Holm–Sidak) are given. Individual measurements are shown with group mean ± SD.
Protocol welfare considerations permitted only one additional blood sample per mouse, and this was drawn by tail venesection at either 30−, 60−, or 90-minutes post-restraint (Figure 2D). Assessed by ANOVA at group level, the main effects of time (P < 0.0001) and salt diet (P = 0.007) were significant, but the interaction was not (P = 0.344), and there were no significant differences in the planned post-hoc comparisons, indicating that the rate of recovery from stress was not affected by salt intake.
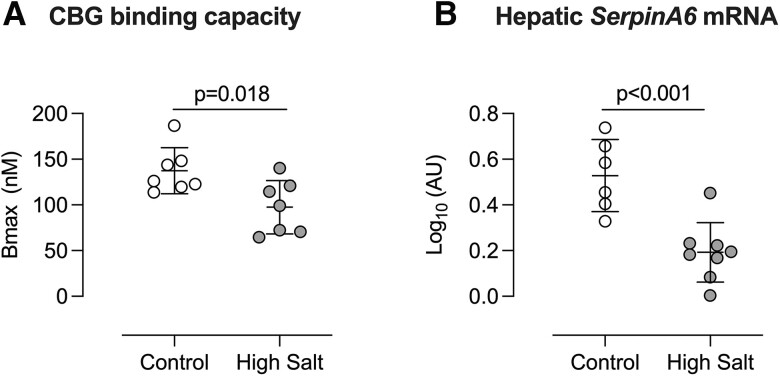
3.2. High salt reduces corticosterone-binding globulin expression and capacity
Although high salt diet increased the total amount of circulating corticosterone at rest and under stress, most glucocorticoid is bound to corticosterone-binding globulin (CBG) and only unbound hormone is active. Thus, CBG has the potential to act as a buffer, stabilising the unbound, active fraction against increased hormone production. We therefore measured CBG binding capacity, which was significantly reduced after 14 days of high salt intake (Figure 3A). Liver mRNA levels of the encoding gene, SerpinA6, was also lower in the high salt group (Figure 3B). SerpinA6 expression was also significantly reduced in mice after 7 days of high salt intake (see Supplementary material online, Figure S3), although CBG binding capacity was not different from the control group at this time point.
Figure 3.
Effect of high salt intake on corticosterone-binding globulin. Male C57BL/6 mice were fed either 0.3% (control; open circles) or 3% (high salt; closed circles), diet for 14 days and blood taken for measurement of (A) Corticosterone-binding globulin binding capacity (n = 7/7). (B) mRNA abundance of SerpinA6, encoding CBG, was measured in liver cDNA (n = 6/8). Expression was normalized to that of reference genes Gapdh and Tbp and log-transformed. Individual measurements are shown with group mean ± SD; statistical comparisons were made with Student’s unpaired t-test and two-tailed P-values are given.
3.3. High salt alters glucocorticoid receptor signalling in tissues
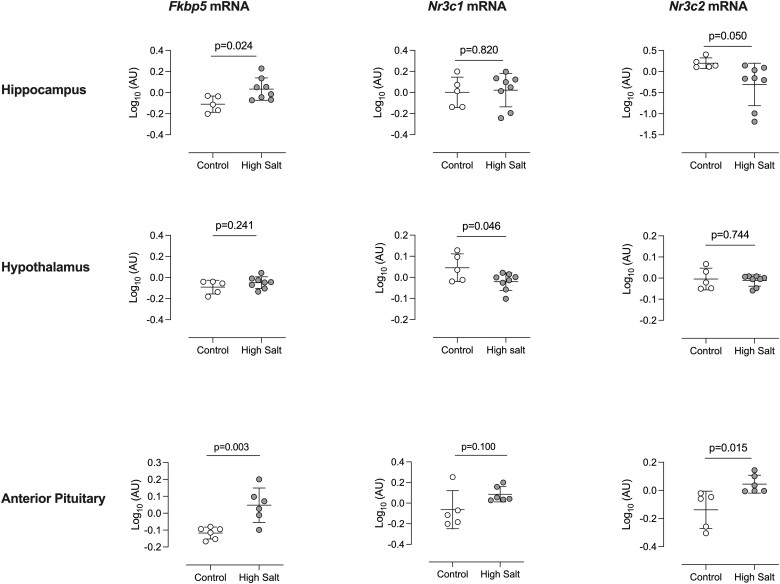
We hypothesised that these effects of high salt diet would combine to increase glucocorticoid signalling within tissues. Glucocorticoid exposure, reported by mRNA encoding FK506-binding protein 5 (Fkbp5)27 was increased in the hippocampus and anterior pituitary but not in the hypothalamus, where mRNA abundance for the glucocorticoid receptor (Nr3c1) was significantly reduced (Figure 4). In the anterior pituitary, mRNA abundance for the glucocorticoid receptor (Nr3c1) tended to be higher in mice fed high salt, but this was not statistically significant; mRNA for the mineralocorticoid receptor (Nr3c2) was increased with high salt. In the hippocampus, receptor expression was not strongly influenced by dietary salt but the enzyme 11β-hydroxysteroid dehydrogenase Type 1 (11βHSD1), which regenerates active glucocorticoid in cells to amplify glucocorticoid signalling,28 was upregulated at mRNA level (see Supplementary material online, Figure S4).
Figure 4.
Effect of high salt intake on mRNA abundance of Fkbp5, Nr3c1 and Nr3c2 in brain regions. Male C57BL/6 mice were fed either 0.3% (control; open circles; n = 8) or 3% (high salt; closed circles; n = 8), diet for 14 days and tissues taken at cull. Excluding samples that failed to yield sufficient material for analysis, mRNA abundance of FK506-binding protein 5 (Fkbp5), glucocorticoid receptor (Nr3c1) and mineralocorticoid receptor (Nr3c2) was measured in hippocampus (n = 5/8), hypothalamus (n = 5/8) and anterior pituitary (n = 5/6) Values were normalized to the expression of reference genes Gapdh and Tbp and log-transformed. Individual measurements for samples that passed QC are shown, along with group mean ± SD. Statistical comparisons were made with Student’s unpaired t-test and P-values are given.
In peripheral tissues, Fkbp5 mRNA was upregulated in the liver, despite downregulation of the glucocorticoid receptor; 11βHSD1 expression was again upregulated (see Supplementary material online, Figure S5). In contrast, kidney Fkbp5 mRNA was downregulated in cortex and medulla, as was mineralocorticoid receptor (Nr3c2) mRNA expression; the glucocorticoid receptor (Nr3c1) was downregulated in only the kidney cortex (see Supplementary material online, Figure S2 and S6). There were no significant changes in these transcripts in the heart, aorta (see Supplementary material online, Figure S7) or adrenal gland (see Supplementary material online, Figure S8) after 2 weeks of high salt intake.
3.4. High salt intake and water conservation
Recent studies indicate that a high salt diet causes a metabolic shift to produce organic osmolytes, which help stabilize body water in the face of salt-induced diuresis.22,29 We examined this in mice fed high salt or control diet for 2 weeks. High salt diet increased food intake but body weight did not change over the 2-week experimental timeframe (Figure 5A). As expected, both urinary sodium, chloride and potassium excretion were significantly increased, but urinary urea excretion was not affected by high salt intake (Figure 5B). Plasma urea concentration was modestly increased by high salt intake but the mRNA abundance for rate-limiting enzymes for ureagenesis and gluconeogenic enzymes (pyruvate carboxylase and phosphoenolpyruvate carboxykinase 1) were not significantly changed in either kidney or liver (see Supplementary material online, Figure S9).
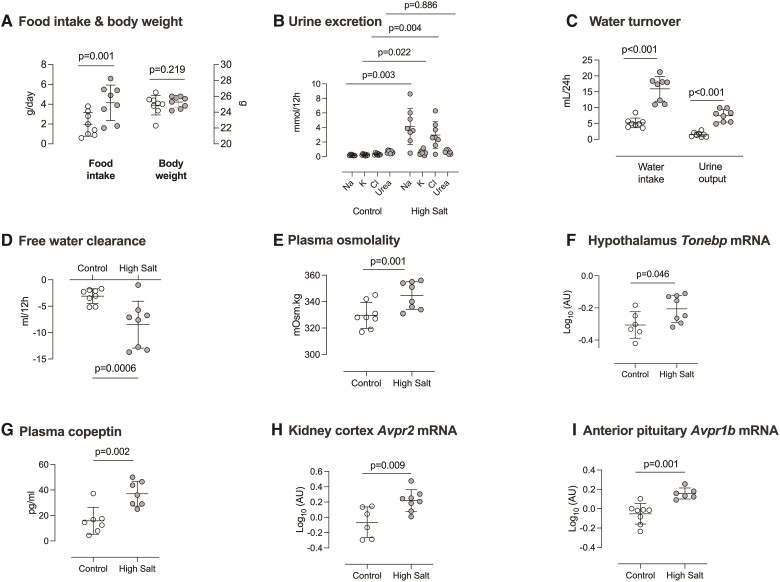
Figure 5.
Effect of high salt intake on fluid volume markers. Male C57BL/6 mice were fed 0.3% (Control; open circles n = 8) diet and then 3% (high salt; closed circles n = 8) diet for 14 days. (A) Food intake and body weight; (B) urine excretion of sodium, potassium, chloride and urea; (C) water turnover; (D) free water clearance and (E) plasma osmolarity. The following measurements were made from samples collected from other experiments: (F) mRNA abundance of tonicity-responsive enhancer-binding protein (Tonebp) in the hypothalamus; (G) plasma copeptin; (H) mRNA abundance of vasopressin V2 receptor (Avpr2) in kidney cortex and (I) mRNA abundance of vasopressin V1b receptor (Avpr1b) in anterior pituitary. Individual measurements are shown with group mean ± SD; statistical comparisons were made with Student’s unpaired t-test and two-tailed P-values are given.
High salt diet induced polyuria and polydipsia (Figure 5C). Free water clearance was significantly reduced (Figure 5D) and sustained high salt intake increased plasma osmolality (Figure 5E) and plasma sodium concentration (see Supplementary material online, Figure S9). Other evidence was indicative of a water conservation response. In the hypothalamus, mRNA encoding Tonicity-responsive enhancer-binding protein (TonEBP), which reflects parallel transcription/translation of vasopressin in response to hypertonicity30 was increased by high salt (Figure 5F). Plasma copeptin, a stable surrogate for vasopressin secretion,31 was also elevated (Figure 5G), as was mRNA abundance of the vasopressin V2 receptor in the kidney (Figure 5H). Vasopressin can also activate V1b receptors in the anterior pituitary to stimulate ACTH release,32 and this receptor was upregulated at the mRNA level in mice fed high salt diet (Figure 5I).
4. Discussion
The main finding of our study is that sustained high dietary salt intake in mice induced multiple abnormalities in glucocorticoid biology. The HPA axis was activated and the response to environmental stress amplified. The capacity of CBG to buffer a rise in blood corticosterone was diminished, and in the hippocampus, anterior pituitary and liver, exposure to glucocorticoids was increased.
Our study provides a mechanistic explanation of the positive correlation between salt intake and urinary cortisol excretion consistently observed in humas,12–18,20 and has two important implications. First, glucocorticoid excess may contribute to the long-term health consequences of high salt intake; second, dietary salt intake becomes an important consideration when diagnosing and managing pre-existing hypercortisolism.
4.1. HPA axis activation at rest and in response to stress
We show functional evidence of a novel, direct connection between dietary salt intake and HPA axis activation. The effect was biphasic: diurnal peak plasma corticosterone was supressed at 1 week and thereafter significantly enhanced. In humans, 1 week of high salt also reduces plasma cortisol, which may reflect an initial phase of enhanced urinary elimination.33 Longer-term, however, our data indicate that high salt intake increases corticosterone production: hypothalamic CRH mRNA was increased and peak plasma levels were elevated. A sustained increase in circulating glucocorticoid, should normally downregulate CRH receptor mRNA expression in the anterior pituitary.34,35 Such downregulation did not happen in our study and Crhr1 mRNA abundance was, overall, higher in the high salt group compared with controls. Combined with significantly increased Pomc mRNA in anterior pituitary, our data indicates enhanced ACTH production/release with sustained high salt intake. Our results suggest two plausible explanations for this phenomenon. First, it is possible that high salt intake disrupts the normal negative feedback control of the HPA axis by corticosterone. In the hippocampus, this negative feedback occurs via the mineralocorticoid receptor because 11HSD2 is not expressed.36 High salt reduced mineralocorticoid receptor mRNA levels, which, on the basis of previous genetic and pharmacological studies, would be expected to enhance basal HPA axis activity.37 That high salt increased anterior pituitary Crh1 mRNA is also consistent with impaired negative feedback.34,35
A second possibility is that vasopressin, a co-regulator of ACTH secretion,32 contributes to enhanced glucocorticoid release. In support of this hypothesis, high salt intake increased serum copeptin, which quantitatively reports hypothalamic synthesis/release of vasopressin.31 High salt also upregulated mRNA for the vasopressin V1b receptor in the anterior pituitary and although this might not fully parallel receptor number,38V1br knockout mice have reduced basal corticosterone and an attenuated response to acute stress.39 Glucocorticoids also directly increase mRNA V1br mRNA abundance and enhance receptor coupling to phospholipase C.40 Overall, a role for vasopressin is a plausible interpretation of our data and is discussed more below.
Amplification of the stress response was found in this study. We do not think this reflects the repeated sampling as the protocol does not itself increase basal corticosterone, cause stress-induced changes in the leukogram or cause stress-associated changes in mouse behaviour.41 We conclude that it is the salt intake itself that enhances the stress response and in this context, we have previously found that high salt diet activates the sympathetic nervous system activation in C57BL/6 mice.42 Indeed, high salt diet is emerging as an important behavioural modifier, at least in rodents.43 This warrants systematic investigation because detrimental changes in brain health in response to high dietary salt intake may have important real-world consequences.
4.2. Peripheral glucocorticoid homeostasis
After two weeks of high salt feeding, total CBG binding capacity for corticosterone was reduced. This reflects early downregulation of Serpina6 mRNA, which after several days reduces the amount of CBG in circulation.44 Whether high salt diet modulates molecular binding affinity of CBG for corticosterone, through altered glycosylation for example45 remains undetermined. The consequences of reduced CBG binding are difficult to gauge. On one hand, CBG is a reservoir for corticosterone in circulation and enhanced glucocorticoid signalling might therefore be anticipated. On the other hand, CBG also contributes to tissue delivery of glucocorticoid46 and CBG-deficient mice are hyporesponsive to corticosterone.47
Our data do not indicate a consistently altered glucocorticoid response after two weeks of high salt intake. Elevated Fkbp5 mRNA suggests glucocorticoid exposure was enhanced in liver, anterior pituitary and hippocampus, reduced in the kidney and unchanged in other tissues examined. The overall picture is complex because changes to the glucocorticoid and mineralocorticoid mRNA expression were accompanied by evidence of altered intracellular glucocorticoid regeneration via 11βHSD1. This granularity is important and shows that high salt intake is influencing glucocorticoid biology at both the systemic and cellular level. Importantly, local changes in glucocorticoid regeneration alter high-level physiological phenotypes.48 For example, transgenic 11βHSD1 overexpression in liver49 and adipose50 cause metabolic abnormalities with salt-sensitive hypertension; overexpression in the hippocampus accelerates age-related cognitive decline.51
4.3. High salt, glucocorticoids, and water homeostasis
Recent studies show that high salt intake engages a water conservation response akin to aestivation, the metabolic torpor induced in diverse species through extended exposure to a hot and arid environment.52 Central to this response is a shift to muscle catabolism, accumulating organic osmolytes such as urea within the body to stabilize fluid volume during extreme challenges to water balance. Thus, in mice facing the dehydrating challenge of high salt diet combined with 0.9% saline as the sole source of fluid, gluconeogenesis and ureagenesis is evident at 2 weeks, associated with an increase in plasma corticosterone.22 This association is also found in humans,19,29 suggesting that glucocorticoids may drive the metabolic reprioritisation, although other clinical studies suggest that the energy demand imposed by glomerular hyperfiltration is more important.12
Our study was not designed to interrogate the metabolic response to high salt intake, but we can make some limited inferences. For example, body weight did not increase despite higher calorific intake and plasma urea was higher in mice fed high salt, suggesting catabolism. On the other hand mRNA abundance of pyruvate carboxylase and phosphoenolpyruvate carboxykinase 1, used to report gluconeogenic flux in liver and kidney53 were not changed by high salt diet, although mRNA levels are not the only factor.54
Certainly, despite free access to water, 2-weeks of high salt diet induced plasma hypertonicity and hypernatremia, indicating compromised fluid balance. Indeed, our observations indicate activation of a water conservation response: hypothalamic mRNA abundance of TonEBP (which parallels vasopressin production in response to hypertonicity30) was increased by high salt intake, as was circulating copeptin (reporting vasopressin synthesis31). Finally, in the kidney, V2 receptor mRNA levels, which parallels protein expression and receptor activity55 were significantly increased, supporting enhanced water reabsorption in the collecting duct when high salt intake is high.56
It is possible that the need to activate an extreme water conservation response underpins the rise in glucocorticoids that will ultimately mobilise organic osmolytes. Increased vasopressin synthesis, upregulation of the V1b receptor in the anterior pituitary39 and CRH in the hypothalamus57 will synergise to activate the HPA axis and elevate circulating glucocorticoid.
4.4. Limitations
Our study aimed to investigate the hypothesis that high salt intake activated the HPA axis. In this, the study was successful and in describing the phenomenon, the data provide a rationale for detailed examination of the consequences for organ function. However, our study is limited. Most experiments provide a snap-shot view at two weeks. Aspects of our study are based on measurements of bulk tissue mRNA abundance for a small number of genes. Given the breadth of the glucocorticoid transcriptome and the challenges of connecting transcriptional changes to altered protein function, our study provides a restricted insight into the potential consequences of salt-induced HPA axis activation. Finally, although the association between urinary salt and glucocorticoid excretion is seen in both women and men, there is well-documented sexual dimorphism in HPA axis function at rest and during the response to stress.58 Our research capability was much reduced during the pandemic and we are not yet able to report a detailed examination of the relationship between salt intake and HPA axis function in female mice.
4.5. Perspectives
We find evidence of accumulated glucocorticoid excess with sustained high salt intake in male C57BL/6 mice. Given that human salt intake is habitually high, our results are relevant to human health. HPA axis induction by high salt intake may serve a critical role in preserving fluid balance but the long-term consequences of this are likely detrimental: glucocorticoid excess typically promotes sodium retention and salt-sensitive blood pressure abnormalities.59–61 HPA activation may also contribute to poor metabolic10,62 and cognitive health when salt intake is high.63
Supplementary material
Supplementary material is available at Cardiovascular Research online.
Author contributions
H.M.C., M.C.H., D.E.W.L., N.D., and M.A.B. contributed to the study design. H.M.C., G.K., C.G., A.C., and M.A.B. performed experiments. J.R.I. and M.N. designed protocols and provided reagents. All authors contributed to data production, statistical analysis, and interpretation. H.M.C., N.D., and M.A.B. wrote the initial draft of the manuscript; all authors reviewed and revised the manuscript.
Supplementary Material
Acknowledgements
We thank David Binnie for supporting animal welfare monitoring, randomisation and blinding. Images in Figure 1 and the graphical abstract were created with BioRender.com.
Contributor Information
Hannah M Costello, Edinburgh Kidney, British Heart Foundation Centre for Cardiovascular Science, The Universtiy of Edinburgh, Edinburgh, EH16 4TJ, United Kingdom.
Georgios Krilis, Edinburgh Kidney, British Heart Foundation Centre for Cardiovascular Science, The Universtiy of Edinburgh, Edinburgh, EH16 4TJ, United Kingdom.
Celine Grenier, Edinburgh Kidney, British Heart Foundation Centre for Cardiovascular Science, The Universtiy of Edinburgh, Edinburgh, EH16 4TJ, United Kingdom.
David Severs, Department of Internal Medicine, Division of Nephrology and Transplantation, Erasmus Medical Center, University Medical Center Rotterdam, 3000 CA Rotterdam, The Netherlands.
Alicja Czopek, Edinburgh Kidney, British Heart Foundation Centre for Cardiovascular Science, The Universtiy of Edinburgh, Edinburgh, EH16 4TJ, United Kingdom.
Jessica R Ivy, Edinburgh Kidney, British Heart Foundation Centre for Cardiovascular Science, The Universtiy of Edinburgh, Edinburgh, EH16 4TJ, United Kingdom.
Mark Nixon, Edinburgh Kidney, British Heart Foundation Centre for Cardiovascular Science, The Universtiy of Edinburgh, Edinburgh, EH16 4TJ, United Kingdom.
Megan C Holmes, Edinburgh Kidney, British Heart Foundation Centre for Cardiovascular Science, The Universtiy of Edinburgh, Edinburgh, EH16 4TJ, United Kingdom.
Dawn E W Livingstone, Edinburgh Kidney, British Heart Foundation Centre for Cardiovascular Science, The Universtiy of Edinburgh, Edinburgh, EH16 4TJ, United Kingdom.
Ewout J Hoorn, Department of Internal Medicine, Division of Nephrology and Transplantation, Erasmus Medical Center, University Medical Center Rotterdam, 3000 CA Rotterdam, The Netherlands.
Neeraj Dhaun, Edinburgh Kidney, British Heart Foundation Centre for Cardiovascular Science, The Universtiy of Edinburgh, Edinburgh, EH16 4TJ, United Kingdom.
Matthew A Bailey, Edinburgh Kidney, British Heart Foundation Centre for Cardiovascular Science, The Universtiy of Edinburgh, Edinburgh, EH16 4TJ, United Kingdom.
Funding
Research funding for this study came from The British Heart Foundation (FS/16/54/32730; PG/16/98/32568; RE/18/5/34216); Kidney Research UK (IN001/2017; INT001/2018) and a Chief Scientist Office Senior Clinical Research Fellowship (SCAF/19/02).
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author
Translational perspective.
The direct connectivity between salt intake and HPA axis function may be relevant for the long-term health consequences of a high salt diet.
References
- 1. Whelton PK, Appel LJ, Sacco RL, Anderson CA, Antman EM, Campbell N, Dunbar SB, Frohlich ED, Hall JE, Jessup M, Labarthe DR, MacGregor GA, Sacks FM, Stamler J, Vafiadis DK, Van Horn LV. Sodium, blood pressure, and cardiovascular disease: further evidence supporting the American heart association sodium reduction recommendations. Circulation 2012;126:2880–2889. [DOI] [PubMed] [Google Scholar]
- 2. Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, Engell RE, Lim SS, Danaei G, Mozaffarian D, Global Burden of Diseases N and Chronic Diseases Expert G . Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open 2013;3:e003733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hunter RW, Dhaun N, Bailey MA. The impact of excessive salt intake on human health. Nat Rev Nephrol 2022;18:321–335. [DOI] [PubMed] [Google Scholar]
- 4. Morimoto A, Uzu T, Fujii T, Nishimura M, Kuroda S, Nakamura S, Inenaga T, Kimura G. Sodium sensitivity and cardiovascular events in patients with essential hypertension. Lancet 1997;350:1734–1737. [DOI] [PubMed] [Google Scholar]
- 5. Weinberger MH, Fineberg NS, Fineberg SE, Weinberger M. Salt sensitivity, pulse pressure, and death in Normal and hypertensive humans. Hypertension 2001;37:429–432. [DOI] [PubMed] [Google Scholar]
- 6. Sigaux J, Semerano L, Favre G, Bessis N, Boissier MC. Salt, inflammatory joint disease, and autoimmunity. Joint Bone Spine 2018;85:411–416. [DOI] [PubMed] [Google Scholar]
- 7. Fang X, Wei J, He X, An P, Wang H, Jiang L, Shao D, Liang H, Li Y, Wang F, Min J. Landscape of dietary factors associated with risk of gastric cancer: a systematic review and dose-response meta-analysis of prospective cohort studies. Eur J Cancer 2015;51:2820–2832. [DOI] [PubMed] [Google Scholar]
- 8. Faraco G, Hochrainer K, Segarra SG, Schaeffer S, Santisteban MM, Menon A, Jiang H, Holtzman DM, Anrather J, Iadecola C. Dietary salt promotes cognitive impairment through tau phosphorylation. Nature 2019;574:686–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Neal B, Wu Y, Feng X, Zhang R, Zhang Y, Shi J, Zhang J, Tian M, Huang L, Li Z, Yu Y, Zhao Y, Zhou B, Sun J, Liu Y, Yin X, Hao Z, Yu J, Li KC, Zhang X, Duan P, Wang F, Ma B, Shi W, Di Tanna GL, Stepien S, Shan S, Pearson SA, Li N, Yan LL, Labarthe D, Elliott P. Effect of salt substitution on cardiovascular events and death. N Engl J Med 2021;385:1067–1077. [DOI] [PubMed] [Google Scholar]
- 10. Baudrand R, Campino C, Carvajal CA, Olivieri O, Guidi G, Faccini G, Vohringer PA, Cerda J, Owen G, Kalergis AM, Fardella CE. High sodium intake is associated with increased glucocorticoid production, insulin resistance and metabolic syndrome. Clin Endocrinol (Oxf) 2014;80:677–684. [DOI] [PubMed] [Google Scholar]
- 11. Torres SJ, Grimes C, Nowson CA, Jayasinghe SU, Bruce CR, Mason SA, He FJ, Turner AI. Urinary sodium is positively associated with urinary free cortisol and total cortisol metabolites in a cross-sectional sample of Australian schoolchildren aged 5–12 years and their mothers. Br J Nutr 2019;121:164–171. [DOI] [PubMed] [Google Scholar]
- 12. Rossitto G, Maiolino G, Lerco S, Ceolotto G, Blackburn G, Mary S, Antonelli G, Berton C, Bisogni V, Cesari M, Seccia TM, Lenzini L, Pinato A, Montezano A, Touyz RM, Petrie MC, Daly R, Welsh P, Plebani M, Rossi GP, Delles C. High sodium intake, glomerular hyperfiltration, and protein catabolism in patients with essential hypertension. Cardiovasc Res 2021;117:1372–1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ehrlich EN. Reciprocal variations in urinary cortisol and aldosterone in response to increased salt intake in humans. J Clin Endocrinol Metab 1966;26:1160–1169. [DOI] [PubMed] [Google Scholar]
- 14. Wambach G, Bleienheuft C, Bonner G. Sodium loading raises urinary cortisol in man. J Endocrinol Invest 1986;9:257–259. [DOI] [PubMed] [Google Scholar]
- 15. Lewicka S, Nowicki M, Vecsei P. Effect of sodium restriction on urinary excretion of cortisol and its metabolites in humans. Steroids 1998;63:401–405. [DOI] [PubMed] [Google Scholar]
- 16. Litchfield WR, Hunt SC, Jeunemaitre X, Fisher ND, Hopkins PN, Williams RR, Corvol P, Williams GH. Increased urinary free cortisol: a potential intermediate phenotype of essential hypertension. Hypertension 1998;31:569–574. [DOI] [PubMed] [Google Scholar]
- 17. Chamarthi B, Kolatkar NS, Hunt SC, Williams JS, Seely EW, Brown NJ, Murphey LJ, Jeunemaitre X, Williams GH. Urinary free cortisol: an intermediate phenotype and a potential genetic marker for a salt-resistant subset of essential hypertension. J Clin Endocrinol Metab 2007;92:1340–1346. [DOI] [PubMed] [Google Scholar]
- 18. Chen AX, Haas AV, Williams GH, Vaidya A. Dietary sodium intake and cortisol measurements. Clin Endocrinol (Oxf) 2020;93:539–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Schutten MT, Kusters YH, Houben AJ, Niessen HE, Op ‘t Roodt J, Scheijen JL, van de Waardenburg MP, Schalkwijk CG, de Leeuw PW, Stehouwer CD. Glucocorticoids affect metabolic but not muscle microvascular insulin sensitivity following high versus low salt intake. JCI Insight 2020;5:e127530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rakova N, Juttner K, Dahlmann A, Schroder A, Linz P, Kopp C, Rauh M, Goller U, Beck L, Agureev A, Vassilieva G, Lenkova L, Johannes B, Wabel P, Moissl U, Vienken J, Gerzer R, Eckardt KU, Muller DN, Kirsch K, Morukov B, Luft FC, Titze J. Long-term space flight simulation reveals infradian rhythmicity in human na(+) balance. Cell Metab 2013;17:125–131. [DOI] [PubMed] [Google Scholar]
- 21. Bailey MA, Craigie E, Livingstone DEW, Kotelevtsev YV, Al-Dujaili EAS, Kenyon CJ, Mullins JJ. Hsd11b2 haploinsufficiency in mice causes salt sensitivity of blood pressure. Hypertension 2011;57:515–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kitada K, Daub S, Zhang Y, Klein JD, Nakano D, Pedchenko T, Lantier L, LaRocque LM, Marton A, Neubert P, Schroder A, Rakova N, Jantsch J, Dikalova AE, Dikalov SI, Harrison DG, Muller DN, Nishiyama A, Rauh M, Harris RC, Luft FC, Wassermann DH, Sands JM, Titze J. High salt intake reprioritizes osmolyte and energy metabolism for body fluid conservation. J Clin Invest 2017;127:1944–1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hammond GL, Lahteenmaki PL. A versatile method for the determination of serum cortisol binding globulin and sex hormone binding globulin binding capacities. Clin Chim Acta 1983;132:101–110. [DOI] [PubMed] [Google Scholar]
- 24. Faul F, Erdfelder E, Lang AG, Buchner A. G*power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39:175–191. [DOI] [PubMed] [Google Scholar]
- 25. Lee J, Yamazaki T, Dong H, Jefcoate C. A single cell level measurement of StAR expression and activity in adrenal cells. Mol Cell Endocrinol 2017;441:22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dunbar DR, Khaled H, Evans LC, Al-Dujaili EA, Mullins LJ, Mullins JJ, Kenyon CJ, Bailey MA. Transcriptional and physiological responses to chronic ACTH treatment by the mouse kidney. Physiol Genomics 2010;40:158–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vermeer H, Hendriks-Stegeman BI, van der Burg B, van Buul-Offers SC, Jansen M. Glucocorticoid-induced increase in lymphocytic FKBP51 messenger ribonucleic acid expression: a potential marker for glucocorticoid sensitivity, potency, and bioavailability. J Clin Endocrinol Metab 2003;88:277–284. [DOI] [PubMed] [Google Scholar]
- 28. Hunter RW, Bailey MA. Glucocorticoids and 11beta-hydroxysteroid dehydrogenases: mechanisms for hypertension. Curr Opin Pharmacol 2015;21:105–114. [DOI] [PubMed] [Google Scholar]
- 29. Rakova N, Kitada K, Lerchl K, Dahlmann A, Birukov A, Daub S, Kopp C, Pedchenko T, Zhang Y, Beck L, Johannes B, Marton A, Muller DN, Rauh M, Luft FC, Titze J. Increased salt consumption induces body water conservation and decreases fluid intake. J Clin Invest 2017;127:1932–1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kim DH, Kim KK, Lee TH, Eom H, Kim JW, Park JW, Jeong JK, Lee BJ. Transcription factor TonEBP stimulates hyperosmolality-dependent arginine vasopressin gene expression in the mouse hypothalamus. Front Endocrinol (Lausanne) 2021;12:627343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Christ-Crain M, Fenske W. Copeptin in the diagnosis of vasopressin-dependent disorders of fluid homeostasis. Nat Rev Endocrinol 2016;12:168–176. [DOI] [PubMed] [Google Scholar]
- 32. Antoni FA. Magnocellular vasopressin and the mechanism of “glucocorticoid Escape”. Front Endocrinol (Lausanne) 2019;10:422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kerstens MN, van der Kleij FG, Boonstra AH, Sluiter WJ, Koerts J, Navis G, Dullaart RP. Salt loading affects cortisol metabolism in normotensive subjects: relationships with salt sensitivity. J Clin Endocrinol Metab 2003;88:4180–4185. [DOI] [PubMed] [Google Scholar]
- 34. Ochedalski T, Rabadan-Diehl C, Aguilera G. Interaction between glucocorticoids and corticotropin releasing hormone (CRH) in the regulation of the pituitary CRH receptor in vivo in the rat. J Neuroendocrinol 1998;10:363–369. [DOI] [PubMed] [Google Scholar]
- 35. Itoi K, Motoike I, Liu Y, Clokie S, Iwasaki Y, Uchida K, Sato T, Aguilera G. Genome-Wide analysis of glucocorticoid-responsive transcripts in the hypothalamic paraventricular region of Male rats. Endocrinology 2019;160:38–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chapman K, Holmes M, Seckl J. 11beta-hydroxysteroid Dehydrogenases: intracellular gate-keepers of tissue glucocorticoid action. Physiol Rev 2013;93:1139–1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Berardelli R, Karamouzis I, D’Angelo V, Zichi C, Fussotto B, Giordano R, Ghigo E, Arvat E. Role of mineralocorticoid receptors on the hypothalamus-pituitary-adrenal axis in humans. Endocrine 2013;43:51–58. [DOI] [PubMed] [Google Scholar]
- 38. Aguilera G, Volpi S, Rabadan-Diehl C. Transcriptional and post-transcriptional mechanisms regulating the rat pituitary vasopressin V1b receptor gene. J Mol Endocrinol 2003;30:99–108. [DOI] [PubMed] [Google Scholar]
- 39. Tanoue A, Ito S, Honda K, Oshikawa S, Kitagawa Y, Koshimizu TA, Mori T, Tsujimoto G. The vasopressin V1b receptor critically regulates hypothalamic-pituitary-adrenal axis activity under both stress and resting conditions. J Clin Invest 2004;113:302–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rabadan-Diehl C, Aguilera G. Glucocorticoids increase vasopressin V1b receptor coupling to phospholipase C. Endocrinology 1998;139:3220–3226. [DOI] [PubMed] [Google Scholar]
- 41. Abatan OI, Welch KB, Nemzek JA. Evaluation of saphenous venipuncture and modified tail-clip blood collection in mice. J Am Assoc Lab Anim Sci 2008;47:8–15. [PMC free article] [PubMed] [Google Scholar]
- 42. Ralph AF, Grenier C, Costello HM, Stewart K, Ivy JR, Dhaun N, Bailey MA. Activation of the sympathetic nervous system promotes blood pressure salt-sensitivity in C57BL/6 mice. Hypertension 2021;77:158–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Beaver JN, Gilman TL. Salt as a non-caloric behavioral modifier: A review of evidence from pre-clinical studies. Neurosci Biobehav Rev 2021;135:104385. [DOI] [PubMed] [Google Scholar]
- 44. Perogamvros I, Ray DW, Trainer PJ. Regulation of cortisol bioavailability–effects on hormone measurement and action. Nat Rev Endocrinol 2012;8:717–727. [DOI] [PubMed] [Google Scholar]
- 45. Chan WL, Carrell RW, Zhou A, Read RJ. How changes in affinity of corticosteroid-binding globulin modulate free cortisol concentration. J Clin Endocrinol Metab 2013;98:3315–3322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Henley D, Lightman S, Carrell R. Cortisol and CBG - getting cortisol to the right place at the right time. Pharmacol Ther 2016;166:128–135. [DOI] [PubMed] [Google Scholar]
- 47. Petersen HH, Andreassen TK, Breiderhoff T, Brasen JH, Schulz H, Gross V, Grone HJ, Nykjaer A, Willnow TE. Hyporesponsiveness to glucocorticoids in mice genetically deficient for the corticosteroid binding globulin. Mol Cell Biol 2006;26:7236–7245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bailey MA. 11beta-Hydroxysteroid Dehydrogenases and hypertension in the metabolic syndrome. Curr Hypertens Rep 2017;19:100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Masuzaki H, Yamamoto H, Kenyon CJ, Elmquist JK, Morton NM, Paterson JM, Shinyama H, Sharp MG, Fleming S, Mullins JJ, Seckl JR, Flier JS. Transgenic amplification of glucocorticoid action in adipose tissue causes high blood pressure in mice. J Clin Invest 2003;112:83–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Paterson JM, Morton NM, Fievet C, Kenyon CJ, Holmes MC, Staels B, Seckl JR, Mullins JJ. Metabolic syndrome without obesity: hepatic overexpression of 11beta-hydroxysteroid dehydrogenase type 1 in transgenic mice. Proc Natl Acad Sci U S A 2004;101:7088–7093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Holmes MC, Carter RN, Noble J, Chitnis S, Dutia A, Paterson JM, Mullins JJ, Seckl JR, Yau JL. 11beta-hydroxysteroid Dehydrogenase type 1 expression is increased in the aged mouse hippocampus and parietal cortex and causes memory impairments. J Neurosci 2010;30:6916–6920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Staples JF. Metabolic flexibility: hibernation, torpor and estivation. Compr Physiol 2016;6:737–771. [DOI] [PubMed] [Google Scholar]
- 53. Chakravarty K, Cassuto H, Reshef L, Hanson RW. Factors that control the tissue-specific transcription of the gene for phosphoenolpyruvate carboxykinase-C. Crit Rev Biochem Mol Biol 2005;40:129–154. [DOI] [PubMed] [Google Scholar]
- 54. Burgess SC, He T, Yan Z, Lindner J, Sherry AD, Malloy CR, Browning JD, Magnuson MA. Cytosolic phosphoenolpyruvate carboxykinase does not solely control the rate of hepatic gluconeogenesis in the intact mouse liver. Cell Metab 2007;5:313–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Hasler U, Nielsen S, Feraille E, Martin PY. Posttranscriptional control of aquaporin-2 abundance by vasopressin in renal collecting duct principal cells. Am J Physiol Renal Physiol 2006;290:F177–F187. [DOI] [PubMed] [Google Scholar]
- 56. Graffe CC, Bech JN, Pedersen EB. Effect of high and low sodium intake on urinary aquaporin-2 excretion in healthy humans. Am J Physiol Renal Physiol 2012;302:F264–F275. [DOI] [PubMed] [Google Scholar]
- 57. Katan M, Morgenthaler N, Widmer I, Puder JJ, Konig C, Muller B, Christ-Crain M. Copeptin, a stable peptide derived from the vasopressin precursor, correlates with the individual stress level. Neuro Endocrinol Lett 2008;29:341–346. [PubMed] [Google Scholar]
- 58. Leistner C, Menke A. Hypothalamic-pituitary-adrenal axis and stress. Handb Clin Neurol 2020;175:55–64. [DOI] [PubMed] [Google Scholar]
- 59. Bailey MA, Mullins JJ, Kenyon CJ. Mineralocorticoid and glucocorticoid receptors stimulate epithelial sodium channel activity in a mouse model of cushing syndrome. Hypertension 2009;54:890–896. [DOI] [PubMed] [Google Scholar]
- 60. Mu S, Shimosawa T, Ogura S, Wang H, Uetake Y, Kawakami-Mori F, Marumo T, Yatomi Y, Geller DS, Tanaka H, Fujita T. Epigenetic modulation of the renal beta-adrenergic-WNK4 pathway in salt-sensitive hypertension. Nat Med 2011;17:573–580. [DOI] [PubMed] [Google Scholar]
- 61. Ivy JR, Oosthuyzen W, Peltz TS, Howarth AR, Hunter RW, Dhaun N, Al-Dujaili EA, Webb DJ, Dear JW, Flatman PW, Bailey MA. Glucocorticoids induce nondipping blood pressure by activating the thiazide-sensitive cotransporter. Hypertension 2016;67:1029–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Lanaspa MA, Kuwabara M, Andres-Hernando A, Li N, Cicerchi C, Jensen T, Orlicky DJ, Roncal-Jimenez CA, Ishimoto T, Nakagawa T, Rodriguez-Iturbe B, MacLean PS, Johnson RJ. High salt intake causes leptin resistance and obesity in mice by stimulating endogenous fructose production and metabolism. Proc Natl Acad Sci U S A 2018;115:3138–3143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Ouanes S, Popp J. High cortisol and the risk of dementia and Alzheimer’s disease: a review of the literature. Front Aging Neurosci 2019;11:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author