Abstract
Background:
The Emergency Department (ED) has increasingly been recognized as an important site of care for older adults with unmet palliative care needs. Despite this, no clear model of care delivery has emerged.
Aim:
To assess the acceptability and feasibility of a scripted palliative care communication intervention in the ED directed by social workers. We hypothesized that the intervention would be feasible, acceptable to patients and ED social workers, and that the collection of patient outcomes would be possible.
Design:
A prospective, unblinded, pilot randomized clinical trial of older adults with serious illness presenting to the ED. Patients were randomized to either receive a social worker-directed palliative care intervention (n-65), which consisted of a conversation focused on patients' goals, values, hopes and worries, or to usual care (n-52). The intervention was evaluated for feasibility and acceptability.
Results:
Of patients randomized to the intervention arm, 66% (43/65) completed a conversation with the social worker. Focus group feedback with the social workers further demonstrated the feasibility of these conversations. There was minimal (12%) loss to follow-up. Of the patients who received the intervention, the majority reported that they appreciated the social workers bringing up their goals for the future (77%), their social workers asking about their fears and worries (72%), and they liked the way the conversation was set up (81%). Social workers administered 95% of the conversation components.
Conclusions:
This pilot trial demonstrated the feasibility and acceptability of a social worker-directed, scripted palliative care communication intervention in a single urban, academic ED.
Keywords: emergency medicine, palliative care, end-of-life care, goals of care, palliative medicine, patient care planning, social work
Introduction
The Emergency Department (ED) commonly serves as a portal of entry to the hospital for patients with serious illness and at the end of life,1–9 with over half of older adults visiting the ED in their last month of life.2 As such, treatment decisions made in the ED have been demonstrated to impact patients' trajectories and subsequent care.2,10
Delivering goal-concordant care, or medical care that aligns with patients' personal goals and values regarding their health care, is complicated by the ED culture of aggressive care,11,12 and that most patients present without any goals of care discussions having taken place.13 When these discussions have taken place, the ED rarely has documentation of it.14 The result is that the care is not always aligned with patients' goals and values.15–17 Ultimately, although many patients with serious illness may not value invasive therapies that are unlikely to improve quality of life,18 most patients who present in the last months of life are admitted to the hospital and die there.2 As such, overall outcomes are likely to be impacted by better understanding patients' goals and values during their emergency visit.19,20
One method that has been shown to facilitate the discussion of patients' goals and values is the Serious Illness Conversation (SIC).21,22 This method has been tested in many care settings and has been shown to effectively and efficiently facilitate such discussions without causing worsening anxiety or depression.23 Designed to be held by different providers on the interprofessional care team, SICs are nondecisional explorations that focus on what the patient's hopes, worries, and priorities are and not specifically to address whether or not to pursue a specific treatment. Hence, these discussions open a window to allow medical providers to better understand how to make sure the care options they offer patients align with the patient's wishes.
Despite the clear need for this understanding in the setting of acutely ill patients presenting to the ED, limited progress has been made toward improving access to palliative care services there. ED clinicians and administrators cite a lack of access to palliative care consults, the ED culture, limited knowledge about how and when to engage palliative care, and competing priorities as limiting their ability to deliver this care.24–26
There has also been limited evidence of long-term outcomes with palliative care in the ED setting, although this is complicated by the many coexisting issues occurring in the relatively short time course of most ED visits relative to the trajectory of a patient's health care experience. Research related to palliative care delivery models in the ED has largely comprised small pilot studies often exploring disease-specific consult models,19,20,27–31 and those assessing the training and education of ED providers in targeted palliative care skills.27,32–38 These models do not take into account the variable access that hospitals have to inpatient palliative care consultation, the competing demands of ED providers and the demonstrated barriers to having ED providers primarily deliver this care.24–26
We initially sought to identify commonly available clinicians in the ED with existing advanced communication skills and a deep understanding of the psychosocial needs of patients to help elicit patients' goals and values in an effort to promote goal-concordant care and address the limited access to palliative care in the ED.
Social workers who are commonly embedded in, or available to, EDs in the United States support the ED assessment of patients' psychosocial needs, serve as a patient advocates, offer counseling, and help patients navigate issues such as housing, substance use, and domestic violence.39–41 Their presence in EDs, training, and advanced communication skills uniquely position them to explore patients' goals and values, using a holistic approach to patient care that relies on their skills at navigating the complex landscape of patients' individual, family, and sociocultural needs, including at end of life.42,43 In this capacity, working at the top of their license, social workers can assist the rest of the interprofessional care team in better understanding the goals and values patients share with them. If this finding is verified, social workers may prove invaluable at expanding the capacity of EDs across the country to understand the priorities of patients facing serious illness with the ultimate goal of providing goal-concordant care.
Given the novelty of employing ED social workers in this capacity and the nuances of the ED culture and setting, we first strived to ensure this novel social work-led palliative care communications' intervention was acceptable to patients and social workers and that the intervention, pragmatically, was feasible to accomplish in a busy ED setting. Secondarily, we sought to establish the effect size of the intervention on patient-centered outcomes. These secondary outcomes will be reported elsewhere.
Methods
Study design and study setting
This is a prospective, single-center, unblinded pilot clinical trial of the feasibility and acceptability of a social work-directed palliative care communication intervention in older adults with potential palliative care needs presenting to the ED. This study was conducted with existing ED social workers without additional dedicated time for their effort to assess if the goals and value discussions could be conducted within existing workflow. The study design was developed through discussions with the hospital's social work leadership who was also a coinvestigator and author on this study (M.E.G.), and the three ED social workers.
This study was conducted at a 1000-bed urban academic medical center in the United States with ∼120,000 annual ED visits, a Division of Palliative Care and training programs in both palliative care and emergency medicine. The study was approved by the Massachusetts General Hospital Institutional Review Board. This study was not supported by external funding.
Participants
Population
We studied patients presenting to the ED who were 75 years or older and were triaged to the Acute or Urgent parts of the ED, the two highest acuity areas in the ED. Exclusion criteria included non-English speaking or inability to consent (due to condition acuity or inability to participate in informed consent).
Sample
Given staff limitations, research assistants screened the ED track board seven hours a day Monday–Friday for patients who were 75+ years of age. Successive patients meeting the entry criteria were enrolled up to four patients per day in an effort not to overburden the ED social workers who had all of their usual duties to complete. Older adults were chosen as a population who we anticipated would have more palliative care needs, including establishing goals and values.
Recruitment
For patients meeting this criterion, research assistants approached the physician caring for the patient and asked them the surprise question (SQ: “Would you be surprised if this patient died in the next 12 months?”). The SQ has been previously identified as a tool for identifying patients that would benefit from a palliative care intervention in the ED.44–46 Patients screening “positive” to the SQ (“No, I would not be surprised if the patient died in the next 12 months”) were eligible for inclusion. Patients were then approached for consent and enrolled.
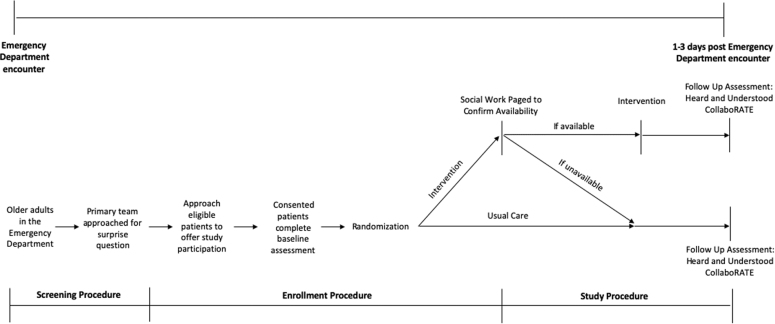
Randomization
After enrollment, a baseline demographic survey was completed with each patient. Thereafter, 1:1 randomization occurred using a randomization schema from Random.org. If the patient was assigned to the intervention group, the research assistant paged the ED social worker with the patient information. Patients randomized to the control group received no further study activity on day 1 (Fig. 1).
FIG. 1.
Study flow diagram.
Intervention group
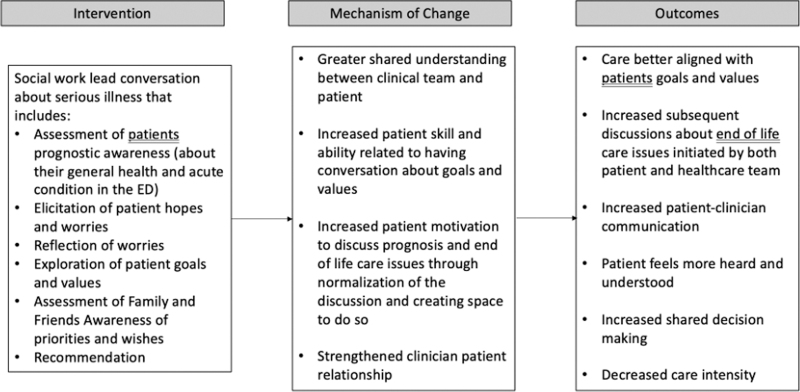
Informed by an ecological model of patient-centered care, we developed a conceptual model for a social work-led intervention (Fig. 2). This model guides the design of this study and projects into future studies of our intervention, which will critically address issues of patient outcomes. Intervention group patients received an SIC in the ED, facilitated by an ED social worker. This single conversation explored the patients' goals and values, and included their hopes and worries. It was adapted for use by social workers in the ED through the modified Delphi approach previously described47 and is in the form of a script social workers follow during the conversation to ensure fidelity of the conversation content. Live SICs were held at the bedside using the script and tailored to the patient's circumstances. Postconversation, the social worker documented the conversation content in the medical record using a structured note template modeled on the conversation guide and communicated their impressions with the ED clinical team verbally. The patient was then contacted by a research assistant the following day to complete three follow-up surveys. If they could not be reached, attempts were made again on days two and three.
FIG. 2.
Conceptual model. ED, Emergency Department.
Social workers received structured training on the script's content and use, followed by a simulation with a palliative care physician with expertise in communication training. The social workers then did an additional simulation with a patient actor. Before study start, each social worker administered the conversation with one patient volunteer. Weekly or biweekly meetings with the ED social workers and research staff, including an ED physician, an expert in serious illness communications, and a palliative care social worker, were ongoing during the study period to help troubleshoot logistics and concerns that arose about SIC interactions. Of note, due to concerns about scope of work, social workers were instructed when medical decisions, prognosis, or code status type issues arose during their SICs to encourage the patient to either talk with their medical provider in the ED about the issues or to allow the social worker to inform the medical provider about their concerns.
Control group
The control group completed the same baseline survey as the intervention group and two surveys in follow-up. They did not receive the social work-led SIC and, as such, did not complete the survey assessing the quality of the SIC. The follow-up protocol was otherwise the same as the intervention group.
Study variables and outcome measures
Feasibility of the intervention and assessment was determined by overall study accrual, the percentage of patients randomized to the intervention that received a conversation, the lost to follow-up rate, and the duration of the conversation that was recorded by the ED social workers, and was also informed by a focus group of social workers, facilitated by a nonstudy staff, audiorecorded, and professionally transcribed.
Acceptability to patients was assessed using the Quality of Serious Illness Conversation (QSIC), a five-item tool designed to assess the degree to which patients find these conversations acceptable, and previously employed for inpatients.48 Acceptability to social workers was assessed through a focus group as noted above.
Baseline characteristics were collected through a questionnaire previously designed by the Palliative Care Communication Initiative,49 and abstracted from the medical record. This questionnaire allowed patients to self-report their quality of life and their physical, emotional, and spiritual symptom burden as well as their self-reported race, gender, education, financial security, and religious affiliation. Participant age, insurance, and specific components of the past medical history were collected from the medical record.
To ensure all study clinicians delivered the intervention consistently, we assessed intervention through chart abstraction, using a fidelity checklist, which outlined the essential components of the conversation, including: (1) assessment of prognostic awareness, (2) disclosure of worry, (3) exploration of what is important, and (4) recommendation. High fidelity was defined as a mean adherence of >70% to the fidelity checklist components, which is consistent with expert consensus for behavioral intervention studies.50
Data analysis
The primary endpoints were feasibility and acceptability. Based on prior work related to palliative care interventions, and informed by our recognition of social worker work load, we determined that the intervention would be feasible if completed in ≥60% of patients randomized to receive it. Study feasibility was also determined by a lost to follow-up rate of <15% in both groups, and the ability to meet a study accrual goal of 10 patients/month. To evaluate acceptability to patients, we calculated intervention participants' response to the acceptability survey.
To evaluate acceptability to social workers, we conducted a thematic analysis of the transcript of the three social workers who participated in the focus group. Qualitative data from the focus group were thematically analyzed using an inductive approach. Two researchers individually read the transcripts and a provisional coding tree was drafted. The transcript was then independently coded by the two researchers using Dedoose (SocioCultural Research Consultants, LLC, Manhattan Beach, CA). Codes were adapted as necessary, resulting in a modified code tree. Multiple codes could be applied to a single response as appropriate. Coding disagreements were resolved by discussion. Themes were identified by reviewing relevant sections of transcripts.
In the comparisons shown in Table 2, we used chi-square test or Fisher's exact test whenever appropriate. SAS version 9.4 (SAS Institute, Inc., Cary, NC) was used for statistical analyses.
Table 2.
Lost to Follow-Up Versus Not Lost to Follow-Up
| Characteristic | All, n (%) | Not lost to follow-up, n (%) | Lost to follow-up, n (%) | p |
|---|---|---|---|---|
| Full sample | 117 | 103 | 14 | |
| Gender | ||||
| Male | 62 (54) | 56 (54) | 7 (50) | 0.807 |
| Female | 51 (45) | 46 (45) | 7 (500) | |
| Other | 1 (1) | 1 (1) | 0 (0) | |
| Age | ||||
| 75–80 | 42 (37) | 36 (35) | 6 (43) | 0.841 |
| 81–85 | 39 (34) | 36 (35) | 5 (36) | |
| 86–90 | 19 (17) | 19 (18) | 1 (7) | |
| 91–95 | 13 (11) | 11 (11) | 2 (14) | |
| 96 and older | 1 (1) | 1 (1) | 0 (0) | |
| Race | 94 (82) | |||
| White | 14 (12) | 84 (82) | 12 (86) | 0.641 |
| Black | 3 (3) | 13 (13) | 1 (7) | |
| Native Hawaiian | 1 (1) | 2 (2) | 1 (7) | |
| Other | 2 (2) | 2 (2) | 0 (0) | |
| Education | ||||
| Did not graduate high school | 16 (14) | 14 (14) | 2 (14) | 0.873 |
| High school or GED | 36 (32) | 31 (30) | 6 (43) | |
| 1–3 Year college or technical school | 18 (16) | 16 (16) | 2 (14) | |
| Bachelor's degree | 15 (13) | 15 (15) | 2 (14) | |
| Masters or doctorate degree | 29 (25) | 27 (26) | 2 (14) | |
| Financial security | ||||
| Secure | 81 (71) | 76 (74) | 7 (50) | 0.132 |
| Partially secure | 23 (19) | 19 (18) | 4 (29) | |
| Insecure | 11 (10) | 8 (8) | 3 (21) | |
| Religious affiliation | ||||
| Yes | 88 (76) | 79 (77) | 12 (86) | 0.67 |
| No | 26 (23) | 24 (23) | 2 (14) | |
| Quality of life | ||||
| High (7–10) | 58 (51) | 56 (54) | 2 (29) | 0.174 |
| Medium | 33 (29) | 28 (27) | 6 (43) | |
| Low (0–3) | 23 (20) | 19 (18) | 4 (28) | |
| Emotional distress | ||||
| Yes | 59 (52) | 52 (50) | 9 (64) | 0.401 |
| No | 55 (48) | 51 (50) | 5 (36) | |
| Physical distress | ||||
| Yes | 86 (75) | 76 (74) | 11 (79) | 1.00 |
| No | 28 (25) | 27 (26) | 3 (21) | |
| Spiritual distress | ||||
| Yes | 21 (18) | 17 (22) | 5 (45) | 0.136 |
| No | 93 (82) | 59 (78) | 6 (55) | |
| Distress related to prognostic uncertainty | ||||
| Yes | 70 (61) | 64 (62) | 8 (57) | 0.774 |
| No | 44 (39) | 39 (38) | 6 (43) | |
Results
Baseline characteristics were collected in 100% of patients and well matched between the two groups (Table 1).
Table 1.
Patient Characteristics
| Characteristic | All, n (%) | Usual care, n (%) | Intervention, n (%) |
|---|---|---|---|
| Full sample | 117 | 52 | 65 |
| Gender | |||
| Male | 63 (54) | 28 (54) | 35 (54) |
| Female | 53 (45) | 23 (44) | 30 (46) |
| Other | 1 (1) | 1 (2) | 0 |
| Age | |||
| 75–80 | 42 (36) | 17 (33) | 25 (38) |
| 81–85 | 41 (35) | 22 (42) | 19 (29) |
| 86–90 | 20 (17) | 8 (15) | 12 (18) |
| 91–95 | 13 (11) | 5 (10) | 8 (12) |
| 96 and older | 1 (1) | 0 (0) | 1 (2) |
| Race | |||
| White | 96 (83) | 41 (80) | 55 (85) |
| Black | 14 (12) | 8 (16) | 6 (10) |
| Native Hawaiian | 3 (3) | 1 (2) | 2 (3) |
| Asian | 1 (1) | 1 (2) | 0 (0) |
| Other | 2 (2) | 0 (0) | 2 (3) |
| Education | |||
| Did not graduate high school | 16 (14) | 7 (13) | 9 (14) |
| High school or GED | 37 (32) | 17 (33) | 20 (31) |
| One to three year college or technical school | 18 (15) | 7 (13) | 11 (17) |
| Bachelors degree | 17 (15) | 6 (12) | 11 (17) |
| Masters or doctorate degree | 29 (25) | 15 (29) | 14 (22) |
| Financial security | |||
| Secure | 83 (71) | 40 (77) | 43 (66) |
| Partially secure | 23 (20) | 7 (13) | 16 (24) |
| Insecure | 11 (9) | 5 (10) | 6 (10) |
| Religious affiliation | |||
| Yes | 91 (78) | 39 (75) | 52 (80) |
| No | 26 (22) | 13 (25) | 13 (20) |
| Quality of life | |||
| High (7–10) | 60 (51) | 28 (53) | 32 (49) |
| Medium | 34 (29) | 13 (25) | 21 (32) |
| Low (0–3) | 23 (20) | 11 (22) | 12 (18) |
| Emotional distress | |||
| Yes | 61 (52) | 29 (56) | 32 (49) |
| No | 56 (48) | 23 (44) | 33 (51) |
| Physical distress | |||
| Yes | 87 (75) | 42 (81) | 45 (69) |
| No | 30 (25) | 10 (19) | 20 (31) |
| Spiritual distress | |||
| Yes | 22 (19) | 9 (17) | 13 (20) |
| No | 95 (81) | 43 (83) | 52 (80) |
| Distress related to prognostic uncertainty | |||
| Yes | 72 (62) | 33 (63) | 39 (60) |
| No | 45 (38) | 19 (37) | 26 (40) |
| History of coronary artery disease | |||
| Yes | 52 (44) | 26 (50) | 26 (40) |
| No | 65 (56) | 26 (50) | 39 (60) |
| History of hypertension | |||
| Yes | 104 (89) | 46 (88) | 58 (89) |
| No | 13 (11) | 6 (12) | 7 (11) |
| History of diabetes | |||
| Yes | 36 (31) | 19 (37) | 17 (27) |
| No | 80 (69) | 33 (63) | 47 (73) |
| History of dementia | |||
| Yes | 5 (4) | 1 (98) | 4 (6) |
| No | 110 (96) | 50 (2) | 60 (94) |
Feasibility
A total of 211 patients were approached for participation during the study period (December 7, 2020–March 5, 2021 and May 3–May 20, 2021), among whom 117 were enrolled in the study and randomized (55%). We had a recruitment interruption due to COVID-19 pandemic-related issues. We enrolled an average of 31 patients per month. Of the 65 patients randomized to the intervention group, social workers were able to complete a SIC for 43 (66.1%) of them. In intervention patients for whom the conversation was not completed (22), the most frequent reasons included social worker work load in other areas of the ED (45%), the patient was discharged or admitted to the hospital before the social worker could arrive (20%), the patient refused the conversation (10%), or the patient was unable to participate secondary to acuity or confusion (10%).
We achieved an 88% follow-up rate combined across both study groups, with 14 patients unable to complete the follow-up surveys despite three attempts (5 in the intervention arm, 9 in the control). These patients did not differ in their baseline characteristics when compared with the overall cohort, except as it relates to quality of life (Table 2). The conversations took an average of 33 minutes.
Fidelity
Social workers consistently administered 95% of the intervention components. Within the conversation categories, assessment of prognostic awareness, exploration of what is important, and recommendations were complete 95% of the time. Disclosure of worry was completed 93% of the time.
Acceptability to patients
Of patients who received the intervention (43) and had completed follow-up assessments (38), 77% reported that they appreciated the social worker bringing up their personal goals for the future; 72% reported they appreciated the social worker asking about their fears and worries; and 81% reported they liked the way the conversation about their illness was set up. While not specifically measuring acceptability as the aforementioned questions from the QSIC tool do, the survey also revealed that 44% reported that the conversation would influence how they prepared for the future, and 48% reported that that discussing their illness with the social worker increased their understanding of what might happen in the future.
Acceptability to social workers
In the focus group with the three social workers, themes emerged related to the work being gratifying, meaningful, and thought provoking, and a scope of work that aligned well with their training:
It's a lot closer to what people think of when they think about social work, really getting to sit with someone and understand how their upbringing and their beliefs and general views of life impact their views about what kind of treatment they want
It's really meaningful work. I feel like these conversations are really interesting
I don't feel at all uncomfortable having these conversations. I really enjoy these conversations
I've sat with them through them thinking that [content of the serious illness conversation] out, which has been really profound
They've been more thought-provoking for patients, and I have enjoyed the opportunity to sit with patients during that time
I would say that these conversations have been good for me
The importance of their training and preparation emerged as a theme in the discussion, along with areas where more training would have been helpful:
The training that we received felt rigorous with the actors. And that I thought was really helpful
The woman who came in from a patient-family perspective - hearing her perspective and what their conversations were looking like, I found really valuable
I do think that having more information or training around code status and the nuances… even if we ourselves aren't getting into that… just to have a knowledge base around it… would've been helpful for me
A theme related to the intervention's reception, both from patients and ED clinicians, also emerged. From the patient perspective, a theme of openness, and willingness to engage become apparent:
[the patients] want us to come.
Patients are really open to sharing and getting into deep thought with us
Patients were really receptive to social work coming in and having these conversations
Related to the ED providers, there was concern about pushback:
Those pushback moments stuck with me, more than the positive reactions, which were more than the pushback
I just don't know that the information that we got from patients were as respected or given as much as if [a physician] went to the provider and said, “I had this conversation”
With respect to feasibility of conducting SICs, there was a recognition that there were challenges associated with doing this work. These themes were related to the content around code status, the challenges of the ED environment, competing priorities and to the lack of clear follow-up:
I feel a little bit of discomfort towards the last two questions when we're talking about, “Have you been someone that's talked to your provider about being on breathing machines?” I don't feel super comfortable with that part of the conversation
[there are] times in which we get the page. We're going to go to the patient, but the patient is at scans or the provider is with the patient or the patient's going upstairs immediately
It's always hard to balance when there's more work
The ED is unpredictable. So it could be fine when we agree to meet with a patient. And then in the duration of that time we're meeting we get three other serious pages and get backed up
[it is hard when] we've related the information and having to sit with knowing that nothing might come of it
Themes related to areas that represented opportunities for improvements in the program included the desire for a closed-loop system to communicate recommendations to the team, a way to integrate family into the discussions, scripted language that facilitates social workers building on conversations that have already been started with other members of their care team (e.g., oncologists or primary care physicians), and tools that could help patients continue these conversations with other caregivers:
Any way that the work could be integrated into rounds conversations might be helpful
I would also think I would have added a piece of communicating with the patient's PCP
Giving a card to the patient… that says, “I've had a serious illness conversation, I'm ready to talk about my code status,” or something like that that they could then hand to a provider that they trusted
Discussion
In this pilot randomized control trial, we assessed the feasibility and acceptability of a social worker-led palliative care intervention in the ED. We demonstrated the ability to enroll the majority of patients that were approached, and that two-thirds of patients assigned to the intervention actually received it. Additionally, most patients found the intervention acceptable. To our knowledge, this study is the first to assess the feasibility of a social work-directed palliative care intervention in the ED.
Nonpalliative care social workers in Oncology and General Internal Medicine have demonstrated success in leading conversations about patients' goals, values, hopes, and worries.51,52 Their involvement in goals of care discussions is in keeping with an international consensus of experts that recommends nonphysician facilitators participate in these conversations.53 Despite these recommendations, to our knowledge, EDs have not engaged ED social workers in ED-based palliative care. In the focus group, the social workers reported that they felt this work was meaningful and felt well within their scope of practice.
Additionally, we found that the majority of patients identified as eligible for the intervention were able to receive it, without altering the social workers' current responsibilities. Given that social workers are already embedded in many EDs, this may offer a feasible option for the provision of aspects of palliative care in the ED. This is especially important given that there is limited access to subspecialized palliative care providers in many EDs, and may also serve to address some of the previously discussed cultural and structural issues related to ED providers having these discussions.
Although related work has demonstrated the acceptability of code status conversations in the ED, it has not previously been known how amenable patients would be to having broader conversations about goals, values, hopes, and worries. It was also not previously known how these conversations would be received when facilitated by social workers, who were not addressing code status directly.
Compared with an inpatient study of a similar serious illness conversation facilitated by physicians,48 acceptability was similar: 77% of patients in this study (vs. 86% in the inpatient study) appreciated the clinician bringing up their personal goals for the future; 72% versus 77% reported they appreciated the clinician asking about their fears and worries; 81% versus 70% reported they liked the way the conversation about their illness was set up.
Notably, this study also demonstrates the need for palliative care in the ED. Over half of the patients in the sample experienced either physical or emotional distress and almost half of patients (49%) reported a moderate or low quality of life. Additionally, 89% of patients had at least one comorbid condition. With such a high rate of physical and emotional distress among older ED patients, and in the setting of significant medical complexity, this study demonstrates the need for palliative care in the ED. This finding also reinforces previous work that examined the efficacy of the SQ in the ED,44,45 suggesting that this is a useful screen to identify seriously ill older adults in the ED. Related to ongoing integration of ED providers in identifying patients that would benefit from palliative care engagement, following this study the SQ has been hardwired in the electronic medical record (EMR) at the study site as a best practice alert on a subset of patients.
In our study, a lower percentage of patients (44%) reported that the conversation helped with their prognostic understanding (compared with 76% in the prior inpatient study). This is not surprising since the content related to prognostic disclosures was removed47 in an effort to better align the conversation guide with the clinical scope of social workers, and the environment of the ED in which prognostication may be more challenging, given that information is often still being collected.
In the social work focus group, the clinicians did identify some key areas to help improve the intervention. These included a system to ensure that the conversations are seen, and continued, by the inpatient team or outpatient primary care physician (PCP). This has the potential to increase the efficacy of the intervention, and will require a solution that is likely both process based and technology enabled. The social workers also noted a need to identify how best to engage families. Given this study was conducted during COVID when visitor restrictions were in place, this represents an important insight and consideration for future intervention improvement.
Limitations
As a pilot study, the ED social workers voluntarily participated and were involved in the intervention's development. They also participated in weekly meetings with emergency medicine, SIC, and palliative care social work experts to continue to refine the intervention and their skills. This may have contributed to the intervention's acceptability and it will be important to continue to test this as the intervention is evaluated at scale. Additionally, this study was conducted at an academic medical center with limited sociodemographic diversity. To that end, although some demographic characteristics are similar to national samples54,55 (Gender, African American Race, Education), other characteristics are significantly underrepresented (Hispanic Race). Although there is no national benchmark for self-reported financial security, our sample (with <10% of the sample reporting financial insecurity), is not generalizable to all areas. Additionally, the focus group only included the three ED social workers, thereby limiting our ability to achieve thematic saturation. Subsequent trials should re-explore issues of acceptability with social work participants.
Conclusions
This study demonstrates that a social worker-led serious illness conversation may be feasible in the ED and acceptable to patients and social workers. It also demonstrates that conducting a randomized controlled trial of this intervention is possible in the ED. This study provides an important first step toward rigorously evaluating the impact that a novel model of a social worker-led ED intervention can have in providing palliative care. We believe this model has the potential to offer a scalable model for identifying patients' goals and values early in their hospitalization and as a result, allow patients' care to be better aligned with their wishes. More research will be needed to explore feasibility and acceptability in EDs with a different patient mix and with different access to ED-based social workers.
Funding Information
No funding was received for this article.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Kangovi S, Barg FK, Carter T, et al. Understanding why patients of low socioeconomic status prefer hospitals over ambulatory care. Health Aff (Millwood) 2013;32(7):1196–1203; doi: 10.1377/hlthaff.2012.0825 [DOI] [PubMed] [Google Scholar]
- 2. Smith AK, McCarthy E, Weber E, et al. Half of older Americans seen in emergency department in last month of life; most admitted to hospital, and many die there. Health Aff 2012;31:1277–1285; doi: 10.1377/hlthaff.2011.0922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. 2017 NHAMCS micro-data file. National Center for Health Statistics. 2019. Available from: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Datasets/NHAMCS [Last accessed: January 1, 2021.]
- 4. Rosenwax LK, McNamara BA, Murray K, et al. Hospital and emergency department use in the last year of life: A baseline for future modifications to end-of-life care. Med J Aust 2011;194:570–573; doi: 10.5694/j.1326-5377.2011.tb03232.x [DOI] [PubMed] [Google Scholar]
- 5. Lee YH, Chu D, Yang NP, et al. Emergency visits among end-of-life cancer patients in Taiwan: A nationwide population-based study. BMC Palliat Care 2015;14:25; doi: 10.1186/s12904-015-0016-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kompanje EJO. Editorial: The worst is yet to come. Many elderly patients with chronic terminal illnesses will eventually die in the emergency department. Intensive Care Med 2010;36(5):732–734; doi: 10.1007/s00134-010-1803-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mayer DK, Travers D, Wyss A, et al. Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. J Clin Oncol 2011;29(19):2683–2688; doi: 10.1200/JCO.2010.34.2816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Smith AK, Schonberg MA, Fisher J, et al. Emergency department experiences of acutely symptomatic patients with terminal illness and their family caregivers. J Pain Symptom Manage 2010;39(6):972–981; doi: 10.1016/j.jpainsymman.2009.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hanchate AD, Dyer KS, Paasche-Orlow MK, et al. Disparities in emergency department visits among collocated racial/ethnic Medicare enrollees. Ann Emerg Med 2019;73(3):225–235. doi: 10.1016/j.annemergmed.2018.09.007 [DOI] [PubMed] [Google Scholar]
- 10. Zalenski RJ, Compton S. Death trajectories of emergency department patients and palliative care service utilization. Ann Emerg Med 2004;44(4):S68; doi: 10.1016/j.annemergmed.2004.07.225 [DOI] [Google Scholar]
- 11. Connors AF, Dawson NV, Desbiens NA, et al. A controlled trial to improve care for seriously ill hospitalized patients: The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). J Am Med Assoc 1995; doi: 10.1001/jama.274.20.1591 [DOI] [Google Scholar]
- 12. Barnato AE, Herndon MB, Anthony DL, et al. Are regional variations in end-of-life care intensity explained by patient preferences? A study of the US Medicare population. Med Care 2007;45(5):386–393; doi: 10.1097/01.mlr.0000255248.79308.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Smith AK, Fisher J, Schonberg MA, et al. Am I doing the right thing? Provider perspectives on improving palliative care in the emergency department. Ann Emerg Med 2009;54(1):86–93.e1 doi: 10.1016/j.annemergmed.2008.08.022 [DOI] [PubMed] [Google Scholar]
- 14. Oulton J, Rhodes SM, Howe C, et al. Advance directives for older adults in the emergency department: A systematic review. J Palliat Med 2015;18(6):500–505; doi: 10.1089/jpm.2014.0368 [DOI] [PubMed] [Google Scholar]
- 15. Aldridge MD, Bradley EH. Epidemiology and patterns of care at the end of life: Rising complexity, shifts in care patterns and sites of death. Health Aff 2017;36(7):1175–1183; doi: 10.1377/hlthaff.2017.0182 [DOI] [PubMed] [Google Scholar]
- 16. Field MJ, Cassel CK. Approaching death: Improving care at the end of life. Health Prog 2011; doi: 10.7326/0003-4819-128-11-199806010-00034 [DOI] [PubMed] [Google Scholar]
- 17. Teno JM, Gozalo PL, Bynum JPW, et al. Change in end-of-life care for medicare beneficiaries: Site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA 2013;309(5):470–477; doi: 10.1001/jama.2012.207624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Goodman DC, Morden NE, Chang C-H, et al. Trends in cancer care near the end of life. A Dartmouth Atlas of Health Care Brief. A Rep Darthmouth Atlast Proj 2013:1–8. [PubMed] [Google Scholar]
- 19. Wu FM, Newman JM, Lasher A, et al. Effects of initiating palliative care consultation in the emergency department on inpatient length of stay. J Palliat Med 2013;16(11):1362–1367; doi: 10.1089/jpm.2012.0352 [DOI] [PubMed] [Google Scholar]
- 20. Grudzen CR, Richardson LD, Johnson PN, et al. Emergency department-initiated palliative care in advanced cancer a randomized clinical trial. JAMA Oncol 2016;2(5):591–598; doi: 10.1001/jamaoncol.2015.5252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jacobsen J, Bernacki R, Paladino J. Shifting to Serious Illness Communication. JAMA 2022;327(4):321–322; doi: 10.1001/jama.2021.23695 [DOI] [PubMed] [Google Scholar]
- 22. Bernacki R, Paladino J, Neville BA, et al. Effect of the serious illness care program in outpatient oncology: A cluster randomized clinical trial. JAMA Intern Med 2019;179(6):751–759; doi: 10.1001/jamainternmed.2019.0077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mack JW, Weeks JC, Wright AA, et al. Prigerson HG. End-of-life discussions, goal attainment, and distress at the end of life: Predictors and outcomes of receipt of care consistent with preferences. J Clin Oncol 2010;28(7):1203–1208; doi: 10.1200/JCO.2009.25.4672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lamba S, Nagurka R, Zielinski A, et al. Palliative care provision in the emergency department: Barriers reported by emergency physicians. J Palliat Med 2013;16(2):143–147; doi: 10.1089/jpm.2012.0402 [DOI] [PubMed] [Google Scholar]
- 25. Grudzen CR, Richardson LD, Major-Monfried H, et al. Hospital administrators' views on barriers and opportunities to delivering palliative care in the emergency department. Ann Emerg Med 2013;61(6):654–660; doi: 10.1016/j.annemergmed.2012.06.008 [DOI] [PubMed] [Google Scholar]
- 26. Stone SC, Mohanty S, Grudzen CR, et al. Emergency medicine physicians' perspectives of providing palliative care in an emergency department. J Palliat Med 2011;14(12):1333–1338; doi: 10.1089/jpm.2011.0106 [DOI] [PubMed] [Google Scholar]
- 27. Kistler EA, Sean Morrison R, Richardson LD, et al. Emergency department-triggered palliative care in advanced cancer: Proof of concept. Acad Emerg Med 2015;22(2):237–239; doi: 10.1111/acem.12573 [DOI] [PubMed] [Google Scholar]
- 28. Mahony SO, Blank A, Simpson J, et al. Preliminary report of a palliative care and case management project in an emergency department for chronically ill elderly patients. J Urban Health 2008;85(3):443–451; doi: 10.1007/s11524-008-9257-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ting SM, Li P, Lau FL, et al. Acute bereavement care in the emergency department: Does the professional-supported volunteers model work? Eur J Emerg Med 1999;6(3):237–243; doi: 10.1097/00063110-199909000-00012 [DOI] [PubMed] [Google Scholar]
- 30. Rosenberg M, Rosenberg L. Integrated model of palliative care in the emergency department. West J Emerg Med 2013;14(6):633–666 doi: 10.5811/westjem.2013.5.14674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Carron P-N, Dami F, Diawara F, et al. Palliative care and prehospital emergency medicine: Analysis of a case series. Medicine (Baltimore) 2014;93(25):e128; doi: 10.1097/MD.0000000000000128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gisondi MA, Lu DW, Yen M, et al. Adaptation of EPEC-EM curriculum in a residency with asynchronous learning. West J Emerg Med 2010;11(5):491–499. [PMC free article] [PubMed] [Google Scholar]
- 33. Lamba S, Desandre PL, Todd KH, et al. Integration of palliative care into emergency medicine: The Improving Palliative Care in Emergency Medicine (IPAL-EM) collaboration. J Emerg Med 2014;46(2):264–270; doi: 10.1016/j.jemermed.2013.08.087 [DOI] [PubMed] [Google Scholar]
- 34. Shoenberger JM, Yeghiazarian S, Rios C, et al. Death notification in the emergency department: Survivors and physicians. West J Emerg Med 2013;14(2):181–185; doi: 10.5811/westjem.2012.10.14193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lamba S, Pound A, Rella JG, et al. Emergency medicine resident education in palliative care: A needs assessment. J Palliat Med 2012;15(5):516–520; doi: 10.1089/jpm.2011.0457 [DOI] [PubMed] [Google Scholar]
- 36. Goldonowicz JM, Runyon MS, Bullard MJ. Palliative care in the emergency department: An educational investigation and intervention. BMC Palliat Care 2018;17(1):43; doi: 10.1186/s12904-018-0293-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Da Silva Soares D, Nunes CM, Gomes B. Effectiveness of emergency department based palliative care for adults with advanced disease: A systematic review. J Palliat Med 2016;19(6);601–609; doi: 10.1089/jpm.2015.0369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Quest T, Herr S, Lamba S, et al. Demonstrations of clinical initiatives to improve palliative care in the emergency department: A report from the IPAL-EM Initiative. Ann Emerg Med 2013;61(6):661–667; doi: 10.1016/j.annemergmed.2013.01.019 [DOI] [PubMed] [Google Scholar]
- 39. Fusenig E. The Role of Emergency Room Social Worker: An Exploratory Study. Retrieved from Sophia, the St. Catherine University repository website: https://sophia.stkate.edu/msw_papers/26. 2012. [Last accessed: January 3, 2022].
- 40. Van Pelt J. Making caring connections, cutting costs: Social work in the emergency department. Soc Work Today 2010;10(6). [Google Scholar]
- 41. Gordon JA. Cost-benefit analysis of social work services in the emergency department: A conceptual model. Acad Emerg Med 2001;8(1):54–60; doi: 10.1111/j.1553-2712.2001.tb00552.x [DOI] [PubMed] [Google Scholar]
- 42. Bosma H, Johnston M, Cadell S, et al. Creating social work competencies for practice in hospice palliative care. Palliat Med 2010;24(1):79–87; doi: 10.1177/0269216309346596 [DOI] [PubMed] [Google Scholar]
- 43. Cicely Saunders D. Social Work and Palliative Care—The Early History. Br J Soc Work 2001;31(5):791–799. [Google Scholar]
- 44. Ouchi K, Jambaulikar G, George NR, et al. The “Surprise Question” asked of emergency physicians may predict 12-month mortality among older emergency department patients. J Palliat Med 2018;21(2):236–240 doi: 10.1089/jpm.2017.0192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Aaronson EL, George N, Ouchi K, et al. The surprise question can be used to identify heart failure patients in the emergency department who would benefit from palliative care. J Pain Symptom Manage 2019;57(5):944–951; doi: 10.1016/j.jpainsymman.2019.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ouchi K, Strout T, Haydar S, et al. Association of emergency clinicians' assessment of mortality risk with actual 1-month mortality among older adults admitted to the hospital. JAMA Netw Open 2019;2(9):e1911139; doi: 10.1001/jamanetworkopen.2019.11139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Aaronson EL, Greenwald JL, Krenzel LR, et al. Adapting the serious illness conversation guide for use in the emergency department by social workers. Palliat Support Care 2021:1–5; [Epub ahead of print]; doi: 10.1017/S1478951521000821 [DOI] [PubMed] [Google Scholar]
- 48. Gace D, Sommer RK, Daubman BR, et al. Exploring Patients' Experience with Clinicians Who Recognize Their Unmet Palliative Needs: An Inpatient Study. J Palliat Med 2020;23(11):1493–1499; doi: 10.1089/jpm.2020.0043 [DOI] [PubMed] [Google Scholar]
- 49. Gramling R, Gajary-Coots E, Stanek S, et al. Design of, and enrollment in, the palliative care communication research initiative: A direct-observation cohort study. BMC Palliat Care 2015;14(1):1–14; doi: 10.1186/s12904-015-0037-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Borrelli B. The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. J Public Health Dent 2011;71(s1):S52–S63; doi: 10.1111/j.1752-7325.2011.00233.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. O'Donnell AE, Schaefer KG, Stevenson LW, et al. Social worker-aided palliative care intervention in high-risk patients with heart failure (SWAP-HF). A pilot randomized clinical trial. JAMA Cardiol 2018;3(6):516–519; doi: 10.1001/jamacardio.2018.0589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lakin JR, Arnold CG, Catzen HZ, et al. Early serious illness communication in hospitalized patients: A study of the implementation of the Speaking About Goals and Expectations (SAGE) program. Healthcare 2021;9(2):100510; doi: 10.1016/j.hjdsi.2020.100510 [DOI] [PubMed] [Google Scholar]
- 53. Rietjens JAC, Sudore RL, Connolly M, et al. Definition and recommendations for advance care planning: An international consensus supported by the European Association for Palliative Care. Lancet Oncol 2017;18(9):e543–e551; doi: 10.1016/S1470-S2045(17)30582-X [DOI] [PubMed] [Google Scholar]
- 54. Ryan CL, Bauman K. Educational Attainment in the United States. US Census Bur Cust Serv Cent 2016;P20–P578. Available from: https://www.census.gov/content/dam/Census/library/publications/2016/demo/p20-p578.pdf [Last accessed: December 1, 2021]. [Google Scholar]
- 55. Population Distribution by Race/Ethnicity. Kaiser Family Foundation. 2019. Available from: https://www.kff.org/other/state-indicator/distribution-by-raceethnicity/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D [Last accessed: October 19, 2021]