Abstract
Introduction
To evaluate patient–physician communication and patients’ understanding of treatment goals in rheumatoid arthritis (RA).
Methods
A cross-sectional online survey of patients with RA and physicians treating RA was conducted between 16 and 30 June 2021. Participants were asked to rate the importance of 17 goals on a 6-point Likert scale, and mean scores were compared between patients and physicians by the Wilcoxon rank sum test. Patients’ satisfaction with physician communication and their understanding of treatment goals were also assessed.
Results
The responses of 502 patients and 216 physicians were analyzed. The most common patient age group was 50–59 years (28.5%), and the mean disease duration was 10.3 years. Physicians had a mean of 19.2 years of treatment experience and were treating a mean of 44.3 patients. Among the 17 goals assessed, patients placed significantly more importance on drug tapering or discontinuation as short-term goals (3–6 months) and on performing basic activities of daily living, being able to engage in daily tasks, achieving and maintaining remission, maintaining better laboratory values, and drug tapering or discontinuation as long-term goals (5–10 years; all adjusted p < 0.05). Patient treatment satisfaction was significantly associated with disease activity, a feeling of treatment effectiveness, satisfaction with physician communication, and agreement with physician goals.
Conclusion
Differences exist among patients with RA and physicians treating RA regarding the importance of short- and long-term treatment goals. Good patient–physician communication appears to be important for improving patient satisfaction.
Trial registration
University Hospital Medical Information Network identifier: UMIN000044463.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40744-023-00560-2.
Keywords: Rheumatoid arthritis, Treatment goals, Patient–physician communication, Patient satisfaction, Online survey
Key Summary Points
| Why carry out this study? |
| The inconsistency of patient and physician attitudes towards treatment goals in rheumatoid arthritis (RA) is a potential obstacle to achieving appropriate treatment effects, but the differences in patient and physician opinions on the importance of treatment goals and the associated causes and impacts of these differences are unclear. |
| The aim of this study was to evaluate the differences in patient and physician opinions on the importance of treatment goals and to understand the associated causes and impacts. |
| What was learned from this study? |
| The results of this survey showed that both patients and physicians place importance on pain and laboratory values and that treat-to-target (T2T) strategy, which aims to achieve clinical remission, is routinely implemented in the treatment of RA; however, they also show that tapering or discontinuing therapies appears to be more important to patients than to physicians and that there is inadequate communication between patients and physicians on joint destruction and anxiety. |
| Our results suggest a need to improve mutual understanding on treatment goals to inhibit joint destruction and maintain good mental health in patients. |
Introduction
Many drugs with various mechanisms of action and modalities were newly marketed between 2000 and 2018 to treat rheumatoid arthritis (RA), and these led to remarkable improvements in the proportion of patients attaining low disease activity or remission, with the proportion of patients achieving this target increasing from about 20% to about 70% [1]. The most recent Japanese RA treatment guidelines recommend the treat-to-target (T2T) strategy and are in line with the 2019 update of the European Alliance of Associations for Rheumatology (EULAR) RA management recommendations [2]. In particular, the Japanese guidelines provide specific information that supports adopting the T2T strategy in clinical practice. This latest update of the Japanese guidelines (published in 2020) [3] focused on the opinion of patients and their families regarding RA treatment strategies and included the results of a survey on the association between the T2T strategy and patient treatment satisfaction, conducted in response to suggestions by an RA patient advocacy group [4].
Although the T2T management strategy has greatly improved the prognosis of RA, certain patients still have difficult-to-treat RA (D2T RA) [5]. A recent study reported on some causes of D2T RA, which included difficulty implementing appropriate treatment because of comorbidities and risks of adverse events and inconsistent attitudes of patients and physicians regarding treatment intensification [6]. Economic factors related to ability to pay have also been reported as one of the patient-related causes of D2T RA [7]. Another study found that the typical characteristics of patients with D2T RA are poor adherence and clinical characteristics such as pain, obesity, and history of relapsing [8].
The results of several studies indicated that patients and physicians have different opinions on the importance of treatment goals. Kaneko et al. [9] reported differences even in the most important treatment goals; for example, 40% of their patients placed importance on the goal of achieving a life unbothered by RA versus only 15% of physicians. Studenic et al. [10] showed that > 70% of patients placed importance on pain relief versus < 5% of physicians. In another study, after a 1-year follow-up period, the joint destruction score on a visual analog scale was higher in patients than in physicians, with this difference being larger than at diagnosis; the researchers reported their view that the patient score reflected disease activity [11]. Taken together, these findings suggest that differences in treatment goals may hamper the treatments aimed at inhibiting joint destruction in RA. Moreover, the lack of shared treatment goals may decrease patient satisfaction with the chosen treatment; for example, the authors of one study reported higher disease activity and a lower remission rate in patients whose satisfaction with treatment was inconsistent with physician satisfaction [12]. Another study identified communication with physicians about treatment strategies and disease activity as factors that contribute to patient satisfaction [13].
From the above, it is evident that not only is the inconsistency of patient and physician attitudes towards treatment goals in RA a potential limitation to achieving appropriate treatment effects, but also that the differences in attitudes in clinical settings are unclear. Consequently, the current communication and treatment goals of patients with RA and physicians treating patients with RA need to be clarified. Therefore, in this study we aimed to evaluate the differences in patient and physician opinions on the importance of treatment goals and to understand the associated causes and impacts.
Methods
Study Design
This study was an online cross-sectional survey of patients with RA and physicians treating RA. The study protocol was registered in the University Hospital Medical Information Network Clinical Trial Registry (UMIN ID number: UMIN000044463). The study was approved by the ethics committee of the Japanese Association for the Promotion of State-of-the-Art in Medicine (ID number: Tokyo, Japan; 2021-36) and followed the ethical principles of medical research involving human subjects of the 1964 Declaration of Helsinki (and its later amendments). All participants provided written informed consent prior to participate in the study, and all patient data was anonymized.
Population
We conducted the survey between 16 and 30 June 2021 among eligible patients and physicians from research panels, i.e., groups of candidates as provided by Japanese research companies. All candidates had provided informed consent to the panel providers for use of their anonymized and aggregated data. For the present study, the research companies recruited new individuals as candidates and asked them to provide additional written informed consent to enroll in this study. Patients were recruited from research panels of two third-party companies(Cross Marketing Group, Inc. [14] and Rakuten Insight, Inc. [15]); eligible patients had to have a diagnosis of RA and to have received treatment for RA at the time of the survey. Physicians treating patients with RA were recruited from a research panel of Nikkei Business Publications, Inc. [16]; physicians were eligible to participate if they were working in any department of rheumatology and connective tissue disease (internal medicine), rheumatology (orthopedic surgery), internal medicine, or orthopedic surgery. It should be noted here that Japan has a unique system in which not only internists but also orthopedic surgeons are involved in the treatment of RA; both of these are able to prescribe disease-modifying antirheumatic drugs [DMARDs], including biologics and Janus kinase [JAK] inhibitors). In addition, to be eligible for inclusion, physicians had to be treating ≥ 5 patients with RA at the time of the survey.
Study Outcomes
The primary outcome was the difference in treatment goals between patients with RA and physicians managing RA in patients, and was assessed by comparing the importance of 17 treatment goals of interest (see Fig. 1). Both patients and physicians rated the importance of each goal on a 6-point Likert scale ranging from 1 (not important at all) to 6 (extremely important).
Fig. 1.
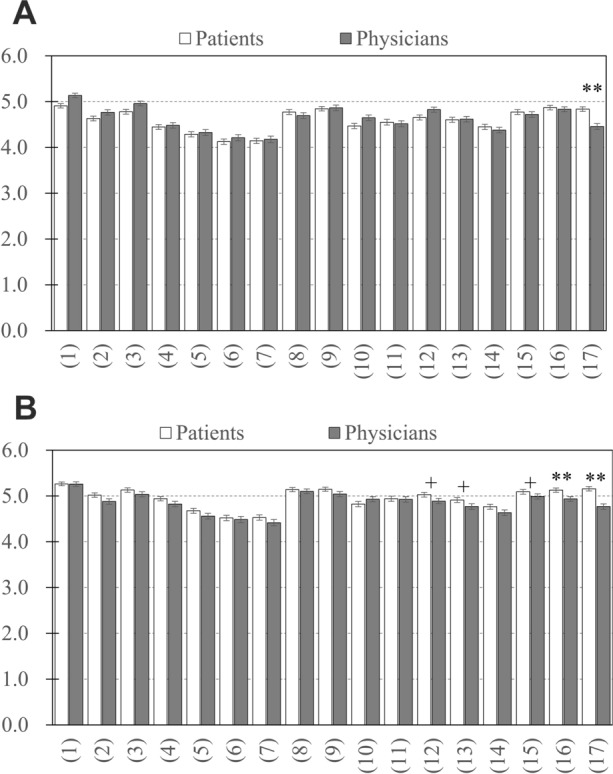
Importance of treatment goals for patients with rheumatoid arthritis and physicians in the short term (a) and long term (b). The numbers in parentheses under each bar graph represent the assessed treatment goal: (1) feel relief from pain or any improvement; (2) less stiffness (frequency and duration); (3) swelling of joints goes away; (4) maintain muscular and grip strength; (5) feel less fatigue and tiredness; (6) feel less anxiety; (7) have good quality sleep; (8) have no joint destruction in fingers and toes or no progression; (9) have no decrease in the mobility of fingers or toes or have better mobility than before; (10) do not feel conscious of changes in appearance due to joint destruction in fingers and toes and have no hesitation in exposing fingers and toes; (11) do not require surgery for joints; (12) perform basic activities of daily living, such as dressing, eating, bathing, and using the toilet without assistance; (13) able to engage in work, studying, housekeeping, childcare, and nursing care; (14) able to engage in hobbies and sports; (15) achieve and maintain rheumatoid arthritis remission; (16) maintain better laboratory values (e.g., C-reactive protein); and (17) taper or discontinue drugs. Cross and double asterisks indicate a significant difference at +p < 0.05; **p < 0.001
To consider the impact of the length of time to achieve the treatment goals, we asked participants to rate these 17 items over both the short (within 3–6 months) and the long term (within 5–10 years). In addition, physicians were asked to estimate the importance of all 17 goals to patients by using a 6-point Likert scale (ranging from 1, not important at all, to 6, extremely important) and patients were asked to rate their agreement with any goal proposed by their primary physicians by using a 6-point Likert scale (ranging from 1, do not agree at all, to 6, completely agree).
The secondary outcomes were patient satisfaction with treatment and the difference in score for communication topics between patients and physicians. Patient satisfaction with current treatment was rated on a 6-point Likert scale ranging from 1 (not satisfied at all) to 6 (extremely satisfied). To assess the communication topics discussed in daily clinical practice, we showed patients a list of 20 topics (see Fig. 2) and asked them to select all those that they want to mention or have mentioned to their primary physicians and that they have been asked about by their primary physicians.
Fig. 2.
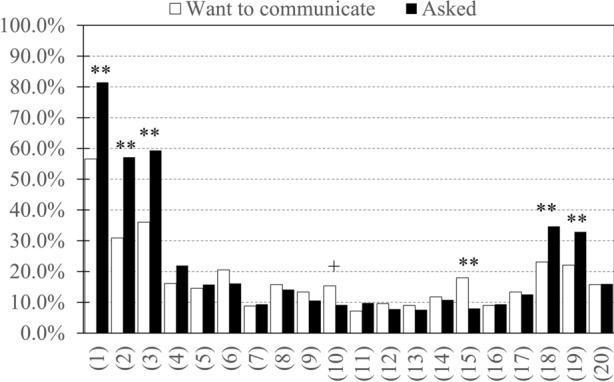
Proportion of patients with rheumatoid arthritis who want to mention topics to their physician and the proportion of patients who have been asked about topics by their physician. The numbers in parentheses under the bar graph represent the assessed topics: (1) pain; (2) stiffness; (3) swelling of joints; (4) muscle and grip strength; (5) fatigue and tiredness; (6) concerns and anxiety; (7) quality and length of sleep; (8) current or future mobility and range of motion; (9) current or future changes in appearance due to joint destruction; (10) anxiety about current or future joint destruction; (11) basic activities of daily living, such as dressing, eating, bathing, and using the bathroom; (12) work, studying, housekeeping, childcare, and nursing care; (13) hobbies and sports; (14) current complications; (15) my treatment goals; (16) whether or not I understand goals proposed by my current physician; (17) receiving information to increase my knowledge about rheumatoid arthritis; (18) current drug treatment situation; (19) presence or absence of drug side effects; (20) costs of treatment and drugs. Cross and double asterisks indicate a significant difference at +p < 0.05; **p < 0.001
Information was collected on the demographic, clinical, and other characteristics of patients with RA, including sex, age, body mass index, clinical department visited, disease duration, Multidimensional Health Assessment Questionnaire (MDHAQ)/Routine Assessment of Patient Index Data 3 (RAPID3) [17], MDHAQ/Psychological Index 3 (PSYCH3) [18, 19], presence of a treatment mentor, procedures for determining treatment success, factors associated with feeling that treatment is going well (including 17 treatment goals, positive explanation by the current physician, and positive explanation by nurses or pharmacists), existence of pain, experience with a biologic or JAK inhibitor, experience of the explanation about joint destruction, and disease activity (remission, mild, moderate, or severe). In addition, we recorded the following information on physician characteristics: clinical department, duration caring for patient with RA (in years), status of rheumatology board certification, implementation of T2T, and number of patients with RA.
Statistical Analysis
As the primary outcome, the 17 treatment goals were compared between patients and physicians by Wilcoxon rank sum test; the results are presented as mean (standard deviation [SD]). p-Values were adjusted by Bonferroni correction. Post hoc analyses were conducted to explore factors associated with the importance of treatment goals to physicians by using linear mixed multivariate regression analyses. In each analysis, the explained variable was the importance of each treatment goal and the explanatory variables were physician characteristics (e.g., status of rheumatology board certification, implementation of T2T strategy), adjusted for the type of treatment goals, with clustering by physician as a random effect. Separate analyses were performed for the short- and long-term goals.
Secondary outcomes were assessed by multivariate linear regression analyses. To confirm factors associated with patient satisfaction, we included all patient characteristics and perceptions as explanatory variables, i.e., sex, age, clinical department visited; disease duration, BMI, MDHAQ/RAPID3, MDHAQ/PSYCH3, treatment mentors, procedures for determining treatment, factors associated with feeling that treatment is going well, existence of pain, experience with a biologic or JAK inhibitor, experience of the explanation about joint destruction, disease activity, satisfaction with communications with the primary physician, and agreement with goals proposed by primary physician. Factors associated with the level of patient agreement with goals proposed by primary physicians in the short- and long-term were also assessed by multivariate linear regression analyses with the following explanatory variables: sex, age, disease duration, BMI, MDHAQ/RAPID3, MDHAQ/PSYCH3, and the importance of the 17 treatment goals. The variables were selected stepwise with Akaike’s information criterion.
For the 20 items related to communication between patients and physicians, McNemar’s exact test was used to compare: (1) the proportion of patients who want to mention the items to physicians with the proportion of patients who have mentioned them, and (2) the proportion of patients who want to mention the items with the proportion of patients who have been asked about the items by their physicians. p-Values were adjusted by Bonferroni correction.
All statistical analyses were performed with R statistical analysis software version 4.1.1 ® Foundation for Statistical Computing, Vienna, Austria). Two-sided tests were used for all comparisons, and p-values < 0.05 were considered to indicate statistically significant differences.
Results
Respondent Characteristics
A total of 502 patients and 216 physicians met the eligibility criteria and completed the survey.
The baseline characteristics of patients are shown in Table 1. The most common age group was 50–59 years, and almost two thirds of patients were female. The mean disease duration was 10.3 years, and more than half the patients were being treated at a department of rheumatology and connective tissue disease (internal medicine).
Table 1.
Characteristics of patients
| Patient characteristics (N = 502) | Values |
|---|---|
| Sex, n (%) | |
| Female | 325 (64.7) |
| Age group (years), n (%) | |
| 20–39 | 45 (9.0) |
| 40–49 | 102 (20.3) |
| 50–59 | 143 (28.5) |
| 60–69 | 132 (26.3) |
| 70+ | 80 (15.9) |
| Type of department where primary physician works, n (%) | |
| Rheumatology and connective tissue disease (internal medicine) | 265 (52.8) |
| Rheumatology (orthopedic surgery) | 160 (31.9) |
| Internal medicine | 20 (4.0) |
| Orthopedic surgery | 49 (9.8) |
| Other/unknown | 8 (1.6) |
| Disease duration (years), n (%) | |
| < 3 | 50 (10.0) |
| 3–4 | 82 (16.3) |
| 5–9 | 105 (20.9) |
| 10–19 | 119 (23.7) |
| 20+ | 61 (12.2) |
| Unknown | 85 (16.9) |
| MDHAQ, mean (SD) | |
| RAPID3 | 6.39 (5.4) |
| PSYCH3 | 1.03 (1.6) |
| Disease activity, n (%) | |
| Remission | 174 (34.7) |
| Mild | 117 (23.3) |
| Moderate | 125 (24.9) |
| Severe | 86 (17.1) |
Values in table are given as the mean (standard deviation [SD]) or as a count (%)
MDHAQ Multidimensional Health Assessment Questionnaire, PSYCH3 Psychological Index 3, RAPID3 Routine Assessment of Patient Index Data 3
The baseline characteristics of physicians are shown in Table 2. The clinical department with the highest proportion of physicians was internal medicine, followed by orthopedic surgery, rheumatology and connective tissue disease (internal medicine), and rheumatology (orthopedic surgery). The mean years of experience in RA treatment was 19.2, and the mean number of patients with RA being treated at the time of the survey was 44.3. Half of physicians were board-certified rheumatologists, and more than half consciously implemented T2T.
Table 2.
Characteristics of physicians
| Physician characteristics (N = 216) | Values |
|---|---|
| Type of department, n (%) | |
| Rheumatology and connective tissue disease (internal medicine) | 47 (21.8) |
| Rheumatology (orthopedic surgery) | 18 (8.3) |
| Internal medicine | 89 (41.2) |
| Orthopedic surgery | 62 (28.7) |
| Experience of RA treatment (years), n (%) | |
| < 10 | 36 (16.7) |
| 10–19 | 54 (25.0) |
| 20–29 | 95 (44.0) |
| 30+ | 31 (14.4) |
| Board-certified rheumatologist, n (%) | |
| Yes | 108 (50.0) |
| No | 108 (50.0) |
| Delivery status of T2T, n (%) | |
| Always deliver | 124 (57.4) |
| Aim to deliver but sometimes cannot/do not aim to deliver | 92 (42.6) |
| Number of patients with RA, n (%) | |
| 5–9 | 49 (22.7) |
| 10–19 | 37 (17.1) |
| 20–39 | 47 (21.8) |
| 40–79 | 45 (20.8) |
| 80+ | 38 (17.6) |
Values in table are given as a count (%)
RA Rheumatoid arthritis, T2T treat to target
Difference in Treatment Goals Between Patients and Physicians
We compared the importance of 17 treatment goals between patients and physicians and calculated the adjusted p values. In the short term (3–6 months), goal (17) taper or discontinue drugs, was significantly more important to patients than to physicians (adjusted p < 0.05; Fig. 1a). In the long term (5–10 years), goals (12) perform basic activities of daily living, such as dressing, eating, bathing, and using the toilet without assistance, (13) able to engage in work, studying, housekeeping, childcare, and nursing care, (15) achieve and maintain RA remission, (16) maintain better laboratory values (e.g., C-reactive protein [CRP]), and (17) taper or discontinue drugs were significantly more important to patients than to physicians (adjusted p < 0.05). The results are presented in Fig. 1b and also as scatter plots in Electronic Supplementary Material (ESM) Fig. 1a, b.
Among the 17 treatment goals, seven were consistently more important than others to both patients and physicians, regardless of whether in the short or long term; these were (1) feel relief from pain or any improvement, (3) swelling of joints goes away, (9) have no decrease in the mobility of fingers or toes or have better mobility than before, (15) achieve and maintain RA remission, and (16) maintain better laboratory values (e.g., CRP). In the long term, the most important goal to patients was (17) taper or discontinue drugs, but physicians rated the most important one as (10) do not feel conscious of changes in appearance due to joint destruction in fingers and toes and have no hesitation in exposing fingers and toes (ESM Table 1).
Patient Satisfaction and Agreement with Goals
By using a generalized linear model and assuming a Gaussian distribution (p < 0.05), we derived nine factors that were significantly associated with patient satisfaction, presented here in descending order of standard partial regression coefficients: satisfaction with communication with primary physicians (β = 0.520); no decrease in the mobility of joints in fingers and toes or better mobility than before (β = 0.140); agreement with any goals proposed by primary physicians (β = 0.133); able to engage in work, studying, housekeeping, childcare, and nursing care (β = 0.101); MDHAQ/RAPID3 (β = − 0.036); positive explanation by nurses or pharmacists (β = − 0.093); no need of any surgery for RA (β = − 0.094); family as treatment mentor (β = − 0.155); and pain (β = − 0.303) (Table 3).
Table 3.
Factors associated with patient satisfaction with rheumatoid arthritis treatment
| Parameter | Coefficient | Standard error | t | p |
|---|---|---|---|---|
| (Intercept) | 1.346 | 0.301 | 4.472 | < 0.001 |
| Sex (reference = men) | 0.138 | 0.076 | 1.826 | 0.068 |
| MDHAQ/RAPID3 | − 0.036 | 0.008 | − 4.400 | < 0.001 |
| Satisfaction with communication with primary physicians | 0.520 | 0.042 | 12.279 | < 0.001 |
| Treatment mentor | ||||
| (1) Family member | − 0.155 | 0.073 | − 2.130 | 0.034 |
| (2) Current physician treating RA | − 0.142 | 0.098 | − 1.443 | 0.150 |
| (9) Other | 0.450 | 0.244 | 1.845 | 0.066 |
| Agreement with any goals proposed by primary physicians | 0.133 | 0.041 | 3.257 | 0.001 |
| Factors that make patients realize that current treatments are working well | ||||
| (1) Feel relief from pain or any improvement | 0.091 | 0.056 | 1.624 | 0.105 |
| (2) Have less stiffness (frequency and duration) | − 0.073 | 0.052 | − 1.410 | 0.159 |
| (6) Feel less anxiety | 0.107 | 0.058 | 1.855 | 0.064 |
| (7) Have good quality sleep | − 0.100 | 0.059 | − 1.713 | 0.087 |
| (9) No decrease in the mobility of joints in fingers and toes or better mobility than before | 0.140 | 0.051 | 2.749 | 0.006 |
| (11) No need of any surgery for RA | − 0.094 | 0.038 | − 2.480 | 0.013 |
| (13) Able to engage in work, studying, housekeeping, childcare, and nursing care | 0.101 | 0.046 | 2.167 | 0.031 |
| (14) Able to engage in hobbies and sports | − 0.075 | 0.042 | − 1.790 | 0.074 |
| (15) Achieve and maintain RA remission | 0.058 | 0.040 | 1.472 | 0.142 |
| (17) Taper or discontinue drugs | − 0.055 | 0.038 | − 1.422 | 0.156 |
| (18) Positive explanation by primary physicians | 0.103 | 0.054 | 1.917 | 0.056 |
| (19) Positive explanation by nurses or pharmacists | − 0.093 | 0.045 | − 2.088 | 0.037 |
| With pain (reference = without pain) | − 0.303 | 0.115 | − 2.637 | 0.009 |
| Received explanation about joint destruction (reference = no explanation) | − 0.118 | 0.085 | − 1.390 | 0.165 |
MDHAQ Multidimensional Health Assessment Questionnaire, RAPID3 Routine Assessment of Patient Index Data 3
By using a generalized linear model and assuming a Gaussian distribution, we also derived five factors that were significantly associated with patients’ agreement with treatment goals in the short term (p < 0.05): the importance of having good quality sleep (β = 0.175); the importance of maintaining better laboratory values (β = 0.170); MDHAQ/RAPID3 (β = − 0.042); MDHAQ/PSYCH3 (β = − 0.074); and the importance of feeling less anxiety (β = − 0.158) (Table 4). In the long term, three factors were significantly associated with patients’ agreement with treatment goals: the importance of maintaining better laboratory values (β = 0.161); MDHAQ/RAPID3 (β = − 0.044); and MDHAQ/PSYCH3 (β = − 0.071; Table 4).
Table 4.
Factors associated with patient agreement with short- and long-term goals proposed by current physician
| (Intercept)Parameter | Short-term goals | Long-term goals | ||||||
|---|---|---|---|---|---|---|---|---|
| Coefficient | Standard error | t | p | Coefficient | Standard error | t | p | |
| 3.893 | 0.313 | 12.452 | < 0.001 | 3.484 | 0.250 | 13.920 | < 0.001 | |
| Sex (reference = men) | − 0.167 | 0.099 | − 1.681 | 0.093 | ||||
| Age | − 0.050 | 0.028 | − 1.758 | 0.079 | ||||
| MDHAQ/RAPID3 | − 0.042 | 0.010 | − 4.356 | < 0.001 | − 0.044 | 0.010 | − 4.576 | < 0.001 |
| MDHAQ/PSYCH3 | − 0.074 | 0.032 | − 2.308 | 0.021 | − 0.071 | 0.032 | − 2.222 | 0.027 |
| Goal | ||||||||
| (6) Feel less anxiety | − 0.158 | 0.078 | − 2.028 | 0.043 | ||||
| (7) Have good quality sleep | 0.175 | 0.075 | 2.344 | 0.019 | ||||
| (12) Perform basic activities of daily living, such as dressing, eating, bathing, and using the toilet without assistance | 0.083 | 0.049 | 1.693 | 0.091 | ||||
| (13) Able to engage in work, studying, housekeeping, childcare, and nursing care | 0.067 | 0.047 | 1.415 | 0.158 | ||||
| (16) Maintain better laboratory values (e.g., CRP) | 0.170 | 0.054 | 3.152 | 0.002 | 0.161 | 0.055 | 2.939 | 0.003 |
CRP C-reactive protein, MDHAQ Multidimensional Health Assessment Questionnaire, PSYCH3 Psychological Index 3, RAPID3 Routine Assessment of Patient Index Data 3
Communication Between Patients and Physicians About Treatment Goals
Among the 20 communication items, there were five for which the proportion of patients asked about these by their primary physicians was significantly higher than the proportion of patients who wanted to mention these items to their physician: (1) pain, (2) stiffness, (3) joint swelling, (18) current treatment adherence, and (19) presence or absence of drug side effects (adjusted p < 0.05 for all comparisons). We found only two items for which the proportion of patients who were asked about the items by primary physicians was significantly lower than the proportion of patients who wanted to mention them: (10) anxiety about current or future joint destruction and (15) my treatment goals (adjusted p < 0.05). The other items, including information about joint destruction and quality of life, e.g., quality and length of sleep, daily living, and social life, were infrequently selected as communication-related items by patients or physicians (Fig. 2; the same results are shown as scatter plots in ESM Fig. 2).
Discussion
In the present study, we showed that both patients and physicians place importance on pain and laboratory values and found that the T2T strategy, which aims to achieve clinical remission, is routinely implemented in the treatment of RA. On the other hand, we also demonstrated that tapering and discontinuing appear to be more important to patients than to physicians and that there is a lack of sufficient communication between patients and physicians on joint destruction and anxiety, suggesting a need to improve mutual understanding about treatment goals to inhibit joint destruction and maintain good mental functioning in patients.
Compared to previous studies performed in Japan, the eligible patients in our study were younger and included a lower proportion of women: the proportion of patients aged ≥ 60 years was around 30% lower than that in earlier studies based on Japanese health insurance data, and the proportion of females was around 10% lower [20, 21]. The clinical characteristics of participants in the present study also differed from those in previous epidemiological studies, with the participants of the present study having higher disease activity and a longer disease duration (a higher proportion of patients had a disease duration of ≥ 5 years). Regarding patients with a long disease duration, it is possible that the present survey was conducted a long time after the period of communication between patients and physicians when patients set treatment goals with their physicians, which may explain the low proportion of patients who mentioned treatment goals to their physician and/or were asked about them. In addition, many patients visited a department of rheumatology and connective tissue disease (internal medicine), whereas many physicians worked in internal medicine. Only about half of physicians were board-certified rheumatologists, but we found no significant association between being a board-certified rheumatologist and the importance of treatment goals.
In the short and long term, both patients and physicians placed importance on the following six goals: (1) feeling relief from pain or any improvement; (9) having no decrease in joint mobility or better mobility; (3) having no joint swelling; (8) having no joint destruction; (15) achieving and maintain RA remission; and (16) maintaining better laboratory values. These goals are consistent with endpoints emphasized in RA treatment guidelines [2, 22]. The present study confirms that treatment goals as defined in treatment guidelines are shared by patients and physicians and suggests that both groups undertake treatment with the aim to achieve the same goals. In contrast, a previous study found that patients value the goal of living life without being bothered by RA but that physicians value the goal of preventing joint destruction and improving the number of swollen joints [9]. Other studies reported a discrepancy in the proportion of patients and physicians who placed importance on pain and the result of pain assessments [10, 11]. However, our results may have differed from those of these previous studies because more physicians now follow the T2T strategy, in which clinical remission is the primary goal and decision-making is shared with patients.
One short-term goal, (17) drug tapering or discontinuation, was more important to patients than to physicians. In addition, as long-term goals, (12) ability to perform basic activities of daily living, (13) ability to engage in everyday activities, (15) achieving RA remission, and (16) maintaining better laboratory values were more important to patients than to physicians. We assume that patients place more value than physicians realize on being treated with the smallest dose and at the lowest frequency of administration. Patients likely place high priority on dosage reduction because it is a visible and easily understandable index that reflects treatment effects and is associated with a reduction in the economic burden of treatment. Reducing the dosage may also help improve adherence and reduce the risk of adverse events, so it can be expected to enhance patient quality of life. In addition to these benefits, dosage reduction or drug discontinuation may improve overall patient satisfaction. On the other hand, continuing to take drugs as prescribed is important for inhibiting joint destruction and achieving remission in the long term. Relapse of RA has been reported as a result of drug tapering and discontinuation [23]. In addition, Benham et al. showed that the T2T strategy cannot be achieved when patients do not agree with a dose increase [24]. To achieve the long-term goal of being able to perform daily activities, patients and physicians must share the opinion that early discontinuation or dose reduction is not necessarily a good treatment option if clinical remission is achieved without structural remission.
The results of the present study suggest that patients’ treatment satisfaction is associated with their satisfaction in communicating with physicians, the presence of pain, noticing treatment effects on impaired joint function, agreement with goals proposed by physicians, and MDHAQ/RAPID3. We believe that several of these factors may be also associated with differences in treatment goals between patients and physicians. First, patients who had no deterioration in the mobility of finger and toe joints or better mobility than before treatment and had a low MDHAQ/RAPID3 reported higher satisfaction, suggesting the importance of maintaining and improving joint functions and maintaining low disease activity. To maintain joint functions, it is critical to control both disease activity and joint destruction [25]. Thus, inhibiting joint destruction appears to be an important factor in patient satisfaction. Next, patients with higher treatment satisfaction demonstrated better agreement with goals proposed by physicians. The agreement levels were significantly lower in patients with higher MDHAQ/RAPID3 and those who placed higher importance on the goal of reducing feelings of anxiety, suggesting that any improvement of mental health aspects, such as anxiety about RA, can enhance patient agreement with physician goals and help to bridge gaps between patients and physicians.
Regarding the communication between patients and physicians, ≥ 50% of patients mentioned subjective symptoms such as pain, stiffness, and swelling to physicians, whereas ≤ 20% of patients expressed views about joint destruction and mental function. A previous questionnaire survey revealed that 62% of patients share their view of treatment with primary physicians and that 76% of them ask to discuss treatment goals [26]. In the present study, 17.9% of patients wanted to mention treatment goals to physicians, 7.8% had mentioned treatment goals, and 8.0% were asked by physicians about treatment goals, suggesting that either such goals are not sufficiently discussed in the clinical setting or—as mentioned above—a high proportion of patients in the study had been treated for such a long time that they rarely discussed treatment goals with their physician. We assume that some issues in the communication between patients and physicians were related to the short consultation time and a lack of patient health literacy. One characteristic of Japanese clinical settings is the collaboration between internal medicine doctors and orthopedic surgeons. Therefore, we expect that patient education based on the perspectives of patients or physicians could improve health literacy more effectively.
Previous studies also reported that the communication between patients and physicians partially covers treatment strategies and quality of life [9, 27]. In our study, only 15% of patients wanted to mention their view on joint destruction, i.e., all three of the respective items [(8) current or future mobility and range of motion, (9) current or future changes in appearance due to joint destruction, and (10) anxiety about current or future joint destruction]; although this was a higher percentage than the patients who were asked about these items, the difference was not significant. Inhibition of joint destruction is important for achieving functional remission, so we suggest that this goal is not discussed often enough by patients and physicians. To preserve range of motion, maintenance of both clinical remission to suppress inflammation and functional remission to inhibit joint destruction is critical [25]. If patients and physicians discuss and share the goal of inhibiting joint destruction, patients may develop a deeper understanding of the significance of their current treatment, which may in turn help to achieve treatment goals and improve patient satisfaction.
In our study, both patients and physicians placed less importance on goals of reducing anxiety and sleeplessness than on other goals. A previous report revealed that most patients felt uncomfortable talking about concerns and anxiety with physicians [28]. In contrast, other studies demonstrated an association of disease activity with the severity of sleeplessness and depression and demanded routine care for those symptoms [28–30].
The limitations of the present study are related to the general features of online-based questionnaire surveys. Such surveys are based only on spontaneous reporting by patients and do not facilitate the collection of detailed clinical information. Furthermore, the study did not match patients and physicians, which could have caused inconsistencies in responses between the two groups. However, these limitations are believed to have had little impact on the study conclusions because the study collected views and conditions in everyday clinical settings. We did not create patient–physician pairs in the present study, and our results showed that the proportion of each type of department was different in terms of patients and physicians. Although a physician’s specialty might influence their communication skills and styles, we found no association between being a board-certified rheumatologist and the amount of importance placed on treatment goals. Consequently, we believe that our unpaired design had a limited or no impact on our conclusions.
Conclusions
In conclusion, our survey revealed that patients and physicians share treatment goals that are primarily related to clinical remission and suggested that most physicians apply the T2T strategy, which aims to improve the acute inflammation associated with joint pain and swelling. Our results also demonstrated that communication between patients and physicians is insufficient on the topics of joint destruction and mobility associated with functional remission. These findings suggest two important conclusions: (1) patients need to have a better understanding of the importance of treatment adherence for achieving and maintaining functional remission, even after achieving clinical remission, with the goal to inhibit joint destruction, and (2) shared decision-making in long-term goals, such as improved quality of life, has improved.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank the participants of the study. The authors also thank Medilead Inc. for their assistance with the online survey, with funding from Eisai Co., Ltd. and Gilead Sciences K.K.
Funding
This study was funded by Eisai Co., Ltd., and Gilead Sciences K.K.; this funding also covered publication, including the journal’s Rapid Service Fee.
Medical Writing/Editorial Assistance
The authors also thank Yamada Translation Bureau, Inc., (www.ytrans.com/home.html) for editorial assistance with funding from Eisai Co., Ltd.
Author Contributions
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication. Shigeki Momohara had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study conception and design: Shigeki Momohara, Kei Ikeda, Masahiro Tada, Toshiaki Miyamoto, Mitsumasa Kishimoto, Takanori Mito. Acquisition of data: Eriko Wakita and Ayako Shoji. Analysis and interpretation of data: Shigeki Momohara, Kei Ikeda, Masahiro Tada, Toshiaki Miyamoto, Mitsumasa Kishimoto, Takanori Mito, Keita Fujimoto, and Ayako Shoji.
Disclosures
Shigeki Momohara has participated in speakers’ bureaus for AbbVie Inc., Astellas Pharma Inc., Chugai Pharmaceutical Co. Ltd., Eisai Co., Ltd., Eli Lilly Japan K.K., Mitsubishi-Tanabe Pharma Corporation, Ono Pharmaceutical Co. Ltd, and Pfizer Inc. Kei Ikeda has participated in speakers’ bureaus for AbbVie Inc., Eli Lilly Japan K.K., Asahi-Kasei Pharma Corporation., Gilead Sciences, Inc., Eisai Co., Ltd., and Pfizer Inc.; and received a research grant from Mitsubishi-Tanabe Pharma Corporation. Masahiro Tada has nothing to declare. Toshiaki Miyamoto has participated in speakers’ bureaus for AbbVie Inc., Asahi-Kasei Pharma Corporation., Eisai Co., Ltd., Eli Lilly Japan K.K., and Gilead Sciences, Inc. Takanori Mito and Keita Fujimoto are employees of Eisai Co., Ltd. Ayako Shoji and Eriko Wakita are employees of Medilead, Inc., which was commissioned to perform this work by Eisai Co., Ltd. Mitsumasa Kishimoto has received consulting fees and/or honoraria from AbbVie Inc., Amgen-Astellas BioPharma, Asahi-Kasei Pharma Corporation., Astellas Pharma Inc., AYUMI Pharmaceutical Corporation, Bristol-Myers Squibb K.K., Celgene Corporation, Chugai Pharmaceutical Co. Ltd., DAIICHI SANKYO COMPANY, LIMITED, Eisai Co., Ltd., Eli Lilly Japan K.K., Gilead Sciences, Inc., Janssen Pharmaceutical K.K., Kyowa Kirin Co., Ltd., Novartis Pharma K.K., Ono Pharmaceutical Co. Ltd, Pfizer Inc., Mitsubishi-Tanabe Pharma Corporation, TEIJIN PHARMA LIMITED, and UCB Japan Co. Ltd. Mitsumasa Kishimoto was also supported by AMED under Grant Number [JP21ek0410086]. Two authors changed their affiliation during the study, as follows: Kei Ikeda moved from the Department of Allergy and Clinical Immunology, Chiba University Hospital, Chiba, to the Department of Rheumatology, Dokkyo Medical University, Tochigi, Japan and Ayako Shoji moved from Medilead Inc., Tokyo, to Healthcare Consulting Inc., Tokyo, Japan.
Compliance with Ethics Guidelines
This study was an online cross-sectional survey of patients with RA and physicians treating RA. The study protocol was registered in the University Hospital Medical Information Network Clinical Trial Registry (UMIN ID number: UMIN000044463). The study was approved by the ethics committee of the Japanese Association for the Promotion of State-of-the-Art in Medicine (ID number: Tokyo, Japan; 2021-36) and followed the ethical principles of medical research involving human subjects of the 1964 Declaration of Helsinki (and its later amendments). All participants provided written informed consent prior to participate in the study, and all patient data was anonymized.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request; subject to approval by the study sponsor.
References
- 1.Yamanaka H, Tanaka E, Nakajima A, et al. A large observational cohort study of rheumatoid arthritis, IORRA: providing context for today's treatment options. Mod Rheumatol. 2020;30(1):1–6. doi: 10.1080/14397595.2019.1660028. [DOI] [PubMed] [Google Scholar]
- 2.Smolen JS, Landewé RBM, Bijlsma JWJ, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 2020;79(6):685–699. doi: 10.1136/annrheumdis-2019-216655. [DOI] [PubMed] [Google Scholar]
- 3.Japan College of Rheumatology. Guidelines for the management of rheumatoid arthritis: diagnosis and treatment. Tokyo: Japan College of Rheumatology; 2020 (in Japanese).
- 4.Kojima M, Hasegawa M, Hirata S, et al. Patients’ perspectives of rheumatoid arthritis treatment: a questionnaire survey for the 2020 update of the Japan college of rheumatology clinical practice guidelines. Mod Rheumatol. 2022;32:307–312. doi: 10.1080/14397595.2021.1913276. [DOI] [PubMed] [Google Scholar]
- 5.Buch MH. Defining refractory rheumatoid arthritis. Ann Rheum Dis. 2018;77(7):966–969. doi: 10.1136/annrheumdis-2017-212862. [DOI] [PubMed] [Google Scholar]
- 6.Nagy G, Roodenrijs NMT, Welsing PM, et al. EULAR definition of difficult-to-treat rheumatoid arthritis. Ann Rheum Dis. 2021;80(1):31–35. doi: 10.1136/annrheumdis-2020-217344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Takanashi S, Kaneko Y, Takeuchi T. Characteristics of patients with difficult-to-treat rheumatoid arthritis in clinical practice. Rheumatology (Oxford) 2021;60(11):5247–5256. doi: 10.1093/rheumatology/keab209. [DOI] [PubMed] [Google Scholar]
- 8.Roodenrijs NMT, van der Goes MC, Welsing PMJ, et al. Difficult-to-treat rheumatoid arthritis: contributing factors and burden of disease. Rheumatology (Oxford) 2021;60(8):3778–3788. doi: 10.1093/rheumatology/keaa860. [DOI] [PubMed] [Google Scholar]
- 9.Kaneko Y, Sato M, Cai Z, Sato M. Assessment of discordance of treatment satisfaction between patients with rheumatoid arthritis in low disease activity or in remission and their treating physicians: a cross-sectional survey. Mod Rheumatol. 2021;31(2):326–333. doi: 10.1080/14397595.2020.1775945. [DOI] [PubMed] [Google Scholar]
- 10.Studenic P, Radner H, Smolen JS, Aletaha D. Discrepancies between patients and physicians in their perceptions of rheumatoid arthritis disease activity. Arthritis Rheum. 2012;64(9):2814–2823. doi: 10.1002/art.34543. [DOI] [PubMed] [Google Scholar]
- 11.Kaneko Y, Kondo H, Takeuchi T. American College of Rheumatology/European League Against Rheumatism remission criteria for rheumatoid arthritis maintain reliable performance when evaluated in 44 joints. J Rheumatol. 2013;40(8):1254–1258. doi: 10.3899/jrheum.130166. [DOI] [PubMed] [Google Scholar]
- 12.Alves Pereira I, Maldonado Cocco J, Feijó Azevedo V, et al. Levels of satisfaction with rheumatoid arthritis treatment and associated alignment between physicians and patients across Latin America. Clin Rheumatol. 2020;39(6):1813–1822. doi: 10.1007/s10067-019-04858-x. [DOI] [PubMed] [Google Scholar]
- 13.Jiang N, Yang P, Liu S, et al. Satisfaction of patients and physicians with treatments for rheumatoid arthritis: a population-based survey in China. Patient Prefer Adher. 2020;14:1037–1047. doi: 10.2147/PPA.S232578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cross Marketing Inc. Internet research (Internet-based research, web surveys). 2022. https://www.cross-m.co.jp/en/service/netresearch/. Accessed 12 Dec 2022
- 15.Rakuten Insight, Inc. To have a meaningful impact. 2022. https://insight.rakuten.co.jp/en/aboutus.html (in Japanese). Accessed 12 Dec 2022
- 16.Nikkei BP Marketing, Inc. Custom research services. 2022. https://www.nikkeibpm.co.jp/item/1100/1100/index.html (in Japanese). Accessed 12 Dec 2022
- 17.Pincus T, Yazici Y, Bergman MJ. RAPID3, an index to assess and monitor patients with rheumatoid arthritis, without formal joint counts: similar results to DAS28 and CDAI in clinical trials and clinical care. Rheum Dis Clin North Am. 2009;35(4):773–778. doi: 10.1016/j.rdc.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 18.Pincus T, Swearingen C, Wolfe F. Toward a multidimensional health assessment questionnaire (MDHAQ): assessment of advanced activities of daily living and psychological status in the patient-friendly health assessment questionnaire format. Arthritis Rheum. 1999;42(10):2220–2230. doi: 10.1002/1529-0131(199910)42:10<2220::AID-ANR26>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 19.Pincus T, Hassett AL, Callahan LF. Criterion contamination of depression scales in patients with rheumatoid arthritis: the need for interpretation of patient questionnaires (as all clinical measures) in the context of all information about the patient. Rheum Dis Clin North Am. 2009;35(4):861–864. doi: 10.1016/j.rdc.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 20.Nakajima A, Sakai R, Inoue E, Harigai M. Prevalence of patients with rheumatoid arthritis and age-stratified trends in clinical characteristics and treatment, based on the National Database of Health Insurance Claims and Specific Health Checkups of Japan. Int J Rheum Dis. 2020;23(12):1676–1684. doi: 10.1111/1756-185X.13974. [DOI] [PubMed] [Google Scholar]
- 21.Yamanaka H, Sugiyama N, Inoue E, Taniguchi A, Momohara S. Estimates of the prevalence of and current treatment practices for rheumatoid arthritis in Japan using reimbursement data from health insurance societies and the IORRA cohort (I) Mod Rheumatol. 2014;24(1):33–40. doi: 10.3109/14397595.2013.854059. [DOI] [PubMed] [Google Scholar]
- 22.Kameda H, Fujii T, Nakajima A, et al. Japan College of Rheumatology guideline for the use of methotrexate in patients with rheumatoid arthritis. Mod Rheumatol. 2019;29(1):31–40. doi: 10.1080/14397595.2018.1472358. [DOI] [PubMed] [Google Scholar]
- 23.Lillegraven S, Paulshus Sundlisæter N, Aga AB, et al. Effect of half-dose vs stable-dose conventional synthetic disease-modifying antirheumatic drugs on disease flares in patients with rheumatoid arthritis in remission: the ARCTIC REWIND randomized clinical trial. JAMA. 2021;325(17):1755–1764. doi: 10.1001/jama.2021.4542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Benham H, Chiu H, Tesiram J, et al. A patient-centered knowledge translation tool for treat-to-target strategy in rheumatoid arthritis: patient and rheumatologist perspectives. Int J Rheum Dis. 2021;24(3):355–363. doi: 10.1111/1756-185X.14051. [DOI] [PubMed] [Google Scholar]
- 25.Welsing PM, van Gestel AM, Swinkels HL, Kiemeney LA, van Riel PL. The relationship between disease activity, joint destruction, and functional capacity over the course of rheumatoid arthritis. Arthritis Rheum. 2001;44(9):2009–2017. doi: 10.1002/1529-0131(200109)44:9<2009::AID-ART349>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 26.Strand V, Wright GC, Bergman MJ, Tambiah J, Taylor PC. Patient expectations and perceptions of goal-setting strategies for disease management in rheumatoid arthritis. J Rheumatol. 2015;42(11):2046–2054. doi: 10.3899/jrheum.140976. [DOI] [PubMed] [Google Scholar]
- 27.McInnes IB, Combe B, Burmester G. Understanding the patient perspective—results of the rheumatoid arthritis: insights, strategies & expectations (RAISE) patient needs survey. Clin Exp Rheumatol. 2013;31:350–357. [PubMed] [Google Scholar]
- 28.Lwin MN, Serhal L, Holroyd C, Edwards CJ. Rheumatoid arthritis: the impact of mental health on disease: a narrative review. Rheumatol Ther. 2020;7(3):457–471. doi: 10.1007/s40744-020-00217-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taylor P, Manger B, Alvaro-Gracia J, et al. Patient perceptions concerning pain management in the treatment of rheumatoid arthritis. J Int Med Res. 2010;38:1213–1224. doi: 10.1177/147323001003800402. [DOI] [PubMed] [Google Scholar]
- 30.Hughes M, Chalk A, Sharma P, Dahiya S, Galloway J. A cross-sectional study of sleep and depression in a rheumatoid arthritis population. Clin Rheumatol. 2021;40(4):1299–1305. doi: 10.1007/s10067-020-05414-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request; subject to approval by the study sponsor.


