Summary
Background
Houses in mild-climate countries, such as Australia, are often ill-equipped to provide occupants protection during cold weather due to their design. As a result, we rely on energy to warm homes, however, energy is becoming increasingly expensive, and evidence is emerging of a sizable burden to population health of being unable to afford to warm homes causing exposure to cold indoor temperatures.
Methods
We use a large longitudinal sample of adult Australians (N = 32,729, Obs = 288,073) collected annually between 2000 and 2019 to estimate the relationship between exposure to energy poverty and mental health (SF-36 mental health score), and a smaller sample from waves collected in 2008–9, 2012–13, and 2016–17 (N = 22,378, Obs = 48,371) to estimate the relationship between energy poverty and onset of asthma, chronic bronchitis or emphysema, hypertension, coronary heart disease, and depression/anxiety. Fixed effects and correlated random-effects regression was used in models. As exposure and outcomes were self-reported, we tested alternative specifications of each to examine bias from measurement error.
Findings
When people can no longer afford to warm their homes, their mental health declines significantly (by 4.6-points on the SF-36 mental health scale, 95% CI −4.93 to −4.24), their odds of reporting depression/anxiety or hypertension increases by 49% (OR 1.49, 95% CI 1.09 to 2.02) and 71% (OR 1.71, 95% CI 1.13 to 2.58) respectively. The findings for the decline in mental health were supported in additional analyses that tested alternative specifications of the exposure measure, including co-resident verification of respondent reporting of being able to afford to warm the home. Support for an effect of energy poverty on hypertension was less clearly supported in these same sensitivity models. There was little evidence of an effect of energy poverty on asthma or chronic bronchitis onset in this adult population noting, however, that we could not examine exacerbation of symptoms.
Interpretation
Reducing exposure to energy poverty should be considered as an intervention with clear benefits for mental health and potential benefits for cardiovascular health.
Funding
National Health and Medical Research Council, Australia.
Keywords: Energy poverty, Health, Longitudinal, Australia
Research in context.
Evidence before this study
Being unable to afford to adequately warm their home, or energy poverty, exposes residents to cold indoor temperatures. The World Health Organisation (WHO) Housing and Health guidelines, published in 2018, recommend that indoor temperatures in people's homes be above 18 °C. This recommendation is based on systematic reviews of the research evidence relating to indoor temperature and its effect on health including excess mortality and cardiovascular health. In addition to the research synthesis generated by WHO that underpins these guidelines, we searched google scholar for recent evidence published after the Guidelines on the health effects of indoor temperature across a range of outcomes – spanning both physical and mental health. We found two additional papers based on the Japanese Smart Wellness Housing Survey linking cold indoor temperature to cholesterol and cardiovascular health. Despite this guidance, gaps in evidence remain in our understanding of energy poverty on depression and mental health, on cardiovascular disease beyond the risk factor of changes in blood pressure from being in a cold indoor environment.
Added value of this study
This study examines a wide range of health outcomes (asthma, bronchitis, hypertension, coronary heart disease, depression, mental health and anxiety) in a large, national cohort of Australian adults who report that they cannot keep their homes warm. Using a causal analytical framework, we compare the effect of changes in their exposure to energy poverty on health over time. We use a range of exposure measures to examine possible bias generated by misspecification of the exposure. We use the observations of co-residents in the household to verify exposure classification and reduce the likelihood that respondent health status affects the reporting of exposure to energy poverty. We also estimate a negative control model with cancer as an outcome.
Implications of all the available evidence
By demonstrating a negative health effect from the inability to keep the home warm, this study provides evidence that housing-focussed health interventions are likely to be effective in improving mental health. Furthermore, given that lower income households are more likely to experience energy poverty, this study confirms that strategies to reduce exposure are likely to also reduce health inequalities in mental health and depression and, likely, hypertension.
Introduction
International research suggests that cold residential living environments are a determinant of cardiovascular disease,1, 2, 3 high blood pressure,4, 5, 6 cholesterol,7 diabetes,8 asthma and COPD,9, 10, 11 and depression.12, 13, 14 There is also evidence that cold and damp homes have a negative impact on mental health and wellbeing13, 15, 16, 17, 18 and that energy poverty (being unable to afford to heat one's home) negatively impacts on self-assessed general health.19 Recent evidence examining the contribution of exposure to cold indoor home environments on cardiovascular disease suggests that this preventable housing condition makes a sizeable contribution to disease burden.20
While dwelling design, climatic conditions, construction materials, and overall housing quality are determinants of indoor residential temperature, each household's relative financial resources enable them to mediate these factors, and to keep their dwellings warm. The lack of sufficient financial resources to keep homes warm is broadly referred to in policy and research as ‘fuel poverty’, ‘energy poverty’ or ‘energy hardship’.21 We use the term energy poverty henceforth.
Energy poverty is an area of concern for public health for many reasons. First, it is correlated with high and low indoor temperature, both of which are negatively associated with health. Second, it is experienced by the most disadvantaged communities and households within a society.21,22 For example, low-income households, single person households, residents of the private rental sector, people with disabilities and First Nations people.23 Finally, with our changing climate, countries like Australia will face more temperature extremes and natural disasters testing the capacity of our housing and housing systems to protect our health.
Apart from published randomised trials in Japan24,25 and community trials in New Zealand,26 the available evidence on the casual relationship between energy poverty, cold housing exposure and health outcomes is limited by a lack of robust data, and the cost and complexity of accessing it. While Japan has the Smart Wellness Housing Study,27 there is currently no large-scale monitoring data for in–home temperature in Australia. Not only is indoor temperature data rarely collected but it also varies by season, time of day, location within home (i.e., bedroom, living area), residents’ individual thermal sensitivity, and capacity to pay for heating.
In the absence of large-scale temperature monitoring data in most settings, a valuable baseline understanding can be gained from national longitudinal survey data, which can utilise changes over time to assess how much of an impact living in homes that the occupants cannot afford to heat, and regard as cold, has on their health.
To advance research in this field beyond our current knowledge, and complement existing evidence from trials, studies are required that examine effects of being unable to heat homes due to financial constraints on chronic health conditions (e.g., asthma, bronchitis, hypertension, coronary heart disease, depression, and anxiety) within a causal framework. In this paper, we use a nationally representative, longitudinal survey of Australians to examine the relationship between energy poverty and onset of health conditions (asthma, chronic bronchitis or emphysema, hypertension, coronary heart disease, depression and anxiety) identified in the WHO Housing and Health Guidelines as being related to unhealthy housing.28 We examine the association between being unable to afford to keep housing warm and health (study objective 1). First, we use fixed effects regression models to estimate the size of effect of exposure to energy poverty on self-reported mental health. Second, for a range of chronic health conditions (asthma, chronic bronchitis or emphysema, hypertension, coronary heart disease, depression and anxiety) we estimate their increased odds of incidence with a change in exposure to energy poverty – and thereby their ability to warm their homes. To explore dynamics of exposure to energy poverty, we utilised the longitudinal nature of the data to estimate the health effects of varying time spent in energy poverty (objective 2). Correlated random effects regression models examine exposure over more than one wave of data collection, as well as changes in exposure into and out of energy poverty. We hypothesis that exposure to energy poverty will reduce mental health and increase the risk of chronic disease (i.e., respiratory, cardiovascular and depression/anxiety).
Methods
Data source
Initiated in 2001, the Household, Income and Labour Dynamics in Australia Survey (HILDA) is a household-based longitudinal social and economic survey.29 The baseline sample was a national probability sample of 7,682 households in private dwellings (where household was defined as co-residence). The survey collects information on demographic, social, economic and health conditions of individuals through interviews and questionnaires, with a focus on family formation, income and work. In addition to a household level data collection, all household members completed the survey individually generating an individual level dataset. This included information on their health. Individuals were followed up every year and the sample has been gradually extended to include any new household members resulting from changes in the composition of the original households. We used data from wave 1 to wave 19, leading to a total sample of 32,729 individuals (i.e., each person who participated in the survey) aged 15 years and over culiminating in 288,073 observations (i.e., the item responses of individuals over the waves in which they participated in the survey). This sample was used to examine the relationship between energy poverty and self-reported mental health. To examine the relationship between energy poverty and asthma, bronchitis, hypertension, heart disease and depression, we restricted the sample to years in which these outcomes were collected (waves 2009, 2013 and 2017) and the year prior (waves 2008, 2012 and 2016). The analytical sample sizes for these models are described in Table 1 under the heading's asthma, bronchitis, hypertension, heart disease and depression.
Table 1.
Summary of derivation of analytical sample including missing observations on each outcome.
| Mental health component score (SF-36) | Asthma | Chronic bronchitis | Hypertension | Heart disease | Depression | |
|---|---|---|---|---|---|---|
| Eligible sample (individuals/obs) | 32,729/288,073 | 22,378/48,371 | 22,378/48,371 | 22,378/48,371 | 22,378/48,371 | 22,378/48,371 |
| Objective 1 | ||||||
| Missing observations | Exposure:37,203 | Exposure:6817 | Exposure:6817 | Exposure:6817 | Exposure:6817 | Exposure:6817 |
| Outcome:30,440 | Outcome:30 | Outcome:30 | Outcome:30 | Outcome:30 | Outcome:30 | |
| Covariate:9115 | Covariate:1785 | Covariate:1785 | Covariate:1785 | Covariate:1785 | Covariate:1785 | |
| Total excluded missing observations | 45,024 | 8139 | 8139 | 8139 | 8139 | 8139 |
| No change in outcome (therefore dropped from logistic fixed effect models) (individuals/obs) | n.a. | 18,886/37,291 | 19,674/39,330 | 18,357/35,808 | 19,367/38,502 | 18,103/35,272 |
| Analytical sample (individuals/obs) | 30,457/243,049 | 1135/2941 | 347/902 | 1664/4424 | 654/1730 | 1918/4960 |
| Objective 2 | ||||||
| Missing observations | Exposure:85,260 | Exposure:13,075 | Exposure:13,075 | Exposure:13,075 | Exposure:13,075 | Exposure:13,075 |
| Outcome:30,440 | Outcome:30 | Outcome:30 | Outcome:30 | Outcome:30 | Outcome:30 | |
| Covariates:9115 | Covariates:1785 | Covariates:1785 | Covariates:1785 | Covariates:1785 | Covariates:1785 | |
| Total excluded missing observations | 91,064 | 14,155 | 14,155 | 14,155 | 14,155 | 14,155 |
| Analytical sample (individuals/obs) | 24,517/197,009 | 17,539/34,216 | 17,539/34,216 | 17,539/34,216 | 17,539/34,216 | 17,539/34,216 |
Note: Missing observations on exposure, outcome, and covariates overlap. The total excluded missing obs is the union of the three sets (not the sum). Missing observations refers to cases where data were not recorded for an item. Exposure refers to a measure of energy poverty. Outcome refers to a measure of health. Covariates are the variables used to adjust the analyses for confounding.
Exposure – energy poverty
At each survey wave, respondents were asked whether they were unable to heat their home because of a shortage of money (0-No; 1-Yes), which represents a consensual measure of energy poverty.30 In addition to this binary variable, we created several measures to describe the dynamics of exposure over time including 1) exposure contemporaneous to outcome measurement that is referred to as current exposure; 2) a categorical variable describing exposure patterns over two consecutive years as being either a) two years of exposure to energy poverty referred to as consistent exposure, b) one year without exposure followed by one year of exposure referred to as recent exposure, c) one year of exposure followed by one year without exposure referred to as past exposure or d) no exposure in any of the years under consideration.
Health outcomes – onset of asthma, chronic bronchitis or emphysema, hypertension, coronary heart disease, depression, mental health
Respondents were asked if they had “…ever been told by a doctor or nurse that you have any of the long-term health conditions listed below?” Listed conditions included asthma, chronic bronchitis and emphysema, high blood pressure/hypertension, coronary heart disease, and depression or anxiety. These data are available for three recent waves of the dataset (9,13 and 17). They were used to generate a series of dummy variables (0-No; 1-Yes) indicating the diagnosis of each condition. If this question is correctly answered by respondents, then a change in their response from one wave to the next from not having a particular condition to having it, indicates condition onset. To harness this strength of the longitudinal data, we have used an analytical regression strategy that models changes in the outcome variable within people over time, noting that there should be one change only.
In addition, the Medical Outcomes Study Short Form (SF-36) was used to measure respondents’ health status at every wave. Scaled SF-36 mental health ranged from 0 to 100 and was used as a continuous variable.
Covariates
Confounders selected for adjustment were based on the literature and included age (in years), gender (male/female, except in fixed-effects regression models that make within person comparisons), household equivalised disposable income (centred on the mean), Indigenous status (Yes/No), presence of children in the household (Yes/No), number of adults in household, and if the household was in Housing Affordability Stress (HAS) (Yes/No).
Statistical analyses
In the descriptive phase of the analyses, the prevalence of energy poverty overall and by income quintiles were estimated. These estimates were adjusted for population weights at baseline using ‘aweights’ in Stata.
In the first analytic phase, responding to study objective 1, we used longitudinal regression analyses on complete case data to estimate the effect of exposure to energy poverty on health. Where possible, we used fixed effects regression models in order to reduce time invariant confounding.31 These models estimate the effects of changes in exposures on changes in health status within each person's set of responses across survey waves.31 For models estimating the effect of energy poverty on mental health all waves of data were used (2000–2019). For models estimating the odds of chronic disease onset, analyses were restricted to waves where this information was collected (2009, 2013, 2017).
In the second analytic stage, responding to study objective 2, we used Correlated Random Effects models (CRE) on complete case data to estimate the effect of prolonged and changing exposure to energy poverty on health.32, 33, 34 Compared to fixed effects models, CRE models include time-constant variables in a parametric form.
To test our models for bias, we selected a negative control outcome35 which we would not expect to be causally associated with exposure to energy poverty. Cancer was selected as there is no strong evidence of an association between energy poverty exposure and prevalent cancer (a function of incidence and survivorship, neither of which we expect to be strongly associated with energy poverty). As for the other chronic health conditions defined as outcomes in these analyses, cancer status was defined by how respondents answered the questions asking if they had “…ever been told by a doctor or nurse that you have any of the long-term health conditions listed below?” Listed amongst the response options to this question was cancer.
Table 2 summarises the models used in this study. Table 1 describes the derivation of the analytical sample from the eligible sample. There were no exclusion criteria and analyses were undertaken on complete case data. Stata software was used to estimate all models.
Table 2.
Summary of the models estimated including study objective, exposure, outcome, type of model and data waves utilised.
| Exposure | Outcome(s) | Type of model | Waves of data used | Study objective (results) |
|---|---|---|---|---|
| Unable to heat home | Mental health and wellbeing (SF-36) | Fixed effects regression | Annual waves between 2000 and 2019 | 1 (Fig. 2) |
| Unable to heat home | Diagnosis of asthma, chronic bronchitis, hypertension, heart disease, depression | Fixed effects logistic regression | Waves 2009, 2013, 2017 | 1 (Fig. 3) |
| Unable to heat home in two waves | Mental health and wellbeing (SF-36) | Correlated Random Effects regression | Annual waves between 2000 and 2019 | 2 (Fig. 4a) |
| Unable to heat home in two waves | Diagnosis of asthma, chronic bronchitis, hypertension, heart disease, depression | Correlated Random Effects logistic regression | Waves 2008, 2009, 2012, 2013, 2016, 2017 | 2 (Fig. 5a) |
| Moving into being unable to heat home between two waves | Mental health and wellbeing (SF-36) | Correlated Random Effects regression | Annual waves between 2000 and 2019 | 2 (Fig. 4b) |
| Moving into being unable to heat home between two waves | Diagnosis of asthma, chronic bronchitis, hypertension, heart disease, depression | Correlated Random Effects logistic regression | Waves 2008, 2009, 2012, 2013, 2016, 2017 | 2 (Fig. 5b) |
| Moving out of being unable to heat home between two waves | Mental health and wellbeing (SF-36) | Correlated Random Effects regression | Annual waves between 2000 and 2019 | 2 (Fig. 4c) |
| Moving out of being unable to heat home between two waves | Diagnosis of asthma, chronic bronchitis, hypertension, heart disease, depression | Correlated Random Effects logistic regression | Waves 2008, 2009, 2012, 2013, 2016, 2017 | 2 (Fig. 5c) |
| Unable to heat home | Diagnosis of cancer | Fixed effects logistic regression – negative control model | Waves 2008, 2009, 2012, 2013, 2016, 2017 | 1 (Table 8) |
In addition to the main analysis, we estimated a series of additional models that examined the sensitivity of our estimates of effect to exposure measurement:
-
a.
Sensitivity analysis 1 - We used an alternative survey question that asked respondents about their ability to warm at least one room in their house: “When it is cold, are you able to keep at least one room of the house adequately warm”. This question was asked in waves 14 and 18 and analysed in relation to health information collected in 2017. A negative response at both waves 14 and 18 was considered evidence of exposure to energy poverty whereas a positive response in at least one wave (either 14 or 18) was regarded as energy security.
-
b.
Sensitivity analysis 2 - We used information from other household members to validate the self-reported energy poverty exposure. By linking respondents to their cohabiting partners within the same household, we created an exogenously constructed indicator of exposure. All household members provided independent responses to the question of whether “they were unable to heat their homes because of a shortage of money”. Use of partner responses, rather than primary respondent responses to this question, removes the potential for the primary respondents' mental health to influence their perception and reporting of ‘adequately warm’ housing, which may bias estimates obtained from the longitudinal data.
-
c.
Sensitivity analysis 3 - We used a subsample of respondents who had not moved house during the study period increasing the consistency of exposure to their home environments.
-
d.
Sensitivity analysis 4 – For models of disease onset (i.e., not the models of self-reported mental health), we censored the dataset to remove people who indicated in 2009 or 2013 that they had a chronic health condition, and then in subsequent waves (2013 or 2017) that they did not. This additional model tested if measurement error in the outcome variable changed the findings of our analyses.
Sensitivity models 1 to 4 were used to test the main effects estimated for objective 1. Sensitivity models 2 to 4 were used to test models relating to objective 2 -- noting the first sensitivity analyses did not contain enough information to test changes in exposure over time.
Role of the funding source
Funders had no role in study design, data collection, data analysis, interpretation, writing of the report).
Results
Descriptive
Table 3 shows that at baseline, 2.3% of respondents reported that they could not heat their house due to financial constraints and 1.3% of respondents reported being unable to heat at least one room in their home. This average varied greatly by quintile of household income with 6.3% of low-income households reporting that they could not afford to adequately warm their home.
Table 3.
Prevalence of exposure to cold housing in the Household, Income and Labour Dynamics in Australia survey.
| Exposure measures | Baseline prevalence |
Baseline prevalence by household income |
||||
|---|---|---|---|---|---|---|
| Total | Quintile 1 (Lowest) | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 (Highest) | |
| Cannot afford to adequately warm homea | 2.3 | 6.3 | 3.5 | 1.9 | 0.9 | 0.3 |
| (n = 253/11,283) | (n = 103/1645) | (n = 68/1939) | (n = 49/2641) | (n = 26/2787) | (n = 7/2271) | |
| Individuals with co-resident validation | 1.5 | 4.2 | 2.8 | 1.1 | 0.7 | 0.3 |
| (n = 98/6770) | (n = 34/810) | (n = 31/1108) | (n = 17/1561) | (12/1794) | (5/1497) | |
| Individuals who do not move in subsequent waves | 1.9 | 5.1 | 3.0 | 1.4 | 1.0 | 0.3 |
| (n = 183/9500) | (n = 73/1413) | (n = 48/1619) | (n = 32/2251) | (n = 23/2324) | (n = 6/1892) | |
| Unable to heat at least one roomb | 1.3 | 3.4 | 1.4 | 2.7 | 0.5 | 0.4 |
| (n = 232/17,279) | (n = 56/1637) | (n = 45/3197) | (n = 89/3239) | (n = 21/4160) | (n = 21/5045) | |
Baseline was 2009.
Baseline was 2014.
There was variation in exposure by type of dwelling (with apartment dwellers reporting a higher proportion of those sampled who were exposed), region (with regional/remote areas reporting a higher rate of those sampled who were exposed) and State and Territory (with the highest estimated proportion located in the Southern-most state of Tasmania) (Table 4).
Table 4.
Prevalence at baseline (wave 2009) of households reporting that they could not afford to adequately warm their home by housing type, regional status and State and Territory of Australia from the Household, Income and Labour Dynamics in Australia survey.
| Cannot afford to adequately warm home | Prevalence (95% Confidence Intervals) | Exposed/Number of individuals (weighted to the population) |
|---|---|---|
| Type of dwelling | ||
| Free-standing | 1.9 (1.6–2.1) | 174/9361 |
| Semi-detached | 2.1 (1.1–3.1) | 15/712 |
| Apartment/unit/flat | 5.3 (4.0–6.6) | 62/1173 |
| Other (e.g. caravan, houseboat) | 6.7 (0.0–13.6) | 2/33 |
| Region | ||
| Urban | 2.1 (1.8–2.4) | 166/7969 |
| Regional/rural | 2.6 (2.1–3.1) | 87/3314 |
| State or Territory | ||
| NSW | 2.4 (1.8–2.9) | 83/3505 |
| Victoria | 1.6 (1.1–2.1) | 45/2862 |
| Queensland | 1.9 (1.4–2.5) | 43/2236 |
| South Australia | 2.3 (1.4–3.3) | 21/886 |
| Western Australia | 3.5 (2.4-4.5) | 43/1235 |
| Tasmania | 6.2 (3.7–8.7) | 17/276 |
| Northern Territory | 0.0 (0.0-0.0) | 0/84 |
| Australian Capital Territory | 0.4 (0.0–2.1) | 1/198 |
In relation to the health outcomes considered in these analyses, the prevalence of each chronic condition apart from asthma increased with age (Table 5) and, apart from heart disease, were more prevalent in women within the sample than men. There were clear socio-economic gradients by education and income such that the highest prevalence of each condition was observed in the lowest socio-economic categories. All health conditions were more prevalent amongst households experiencing housing affordability stress.
Table 5.
Describes the baseline sociodemographic characteristics of individuals in the Household, Income and Labour Dynamics in Australia sample by each health outcome.
| Asthma (%) | Chronic bronchitis or emphysema (%) | High Blood Pressure (%) | Heart diseases (%) | Depression or Anxiety (%) | SF36 Mental Health (average)a | |
|---|---|---|---|---|---|---|
| Age (years) | ||||||
| <20 | 14.0 | 0.4 | 0.6 | 0.4 | 6.7 | 73.8 |
| 20 to 39 | 11.6 | 0.6 | 3.4 | 0.2 | 11.0 | 73.3 |
| 40 to 59 | 9.1 | 1.9 | 18.4 | 3.9 | 11.0 | 74.1 |
| >60 | 11.0 | 5.9 | 45.0 | 14.2 | 10.1 | 76.8 |
| Total number of people | 13,296 | 13,296 | 13,296 | 13,296 | 13,296 | 11,444 |
| Sex | ||||||
| Male | 9.0 | 2.0 | 15.7 | 4.9 | 7.8 | 75.6 |
| Female | 12.7 | 2.2 | 17.9 | 4.0 | 12.8 | 73.3 |
| Total number of people | 13,296 | 13,296 | 13,296 | 13,296 | 13,296 | 11,444 |
| Education | ||||||
| Year 11 or below | 9.3 | 0.9 | 11.6 | 2.3 | 7.8 | 73.1 |
| Diploma, certificate or Year 12 | 10.2 | 2.0 | 13.9 | 3.3 | 10.5 | 74.6 |
| Degree or higher | 12.8 | 3.0 | 24.0 | 7.2 | 11.8 | 76.1 |
| Total number of people | 13,296 | 13,296 | 13,296 | 13,296 | 13,296 | 11,444 |
| Household income (Quintiles) | ||||||
| 1 (Lowest) | 13.0 | 4.9 | 29.6 | 9.7 | 17.4 | 70.0 |
| 2 | 12.2 | 3.1 | 20.3 | 5.9 | 12.3 | 73.3 |
| 3 | 10.5 | 1.2 | 13.5 | 2.9 | 10.0 | 74.0 |
| 4 | 10.6 | 1.2 | 12.2 | 2.8 | 8.2 | 75.7 |
| 5 (Highest) | 8.8 | 1.0 | 13.4 | 2.7 | 6.2 | 77.6 |
| Total number of people | 13,296 | 13,296 | 13,296 | 13,296 | 13,296 | 11,444 |
| Housing Affordability Stress | ||||||
| No | 10.8 | 2.1 | 16.9 | 4.4 | 9.9 | 74.8 |
| Yes | 15.2 | 3.2 | 17.1 | 5.4 | 20.7 | 67.9 |
| Total number of people | 12,754 | 12,754 | 12,754 | 12,754 | 12,754 | 11,043 |
A higher score on this scale correlates with better mental health.
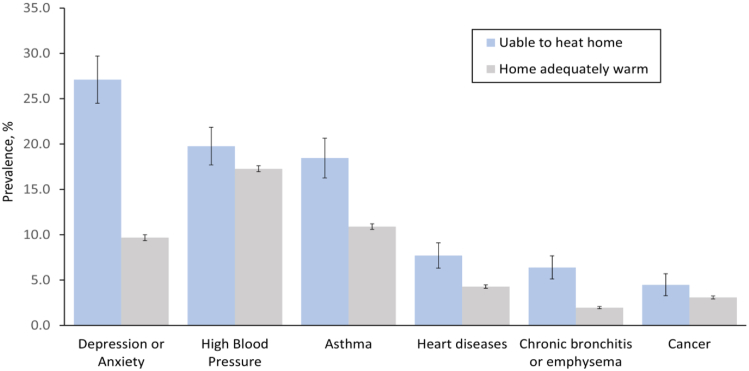
Notably, people with chronic health conditions—across all conditions considered as either outcomes or negative control outcomes (i.e., cancer) in these analyses (Fig. 1)— were more likely to report living in houses that they could not afford to keep warm.
Fig. 1.
Prevalence of chronic health problems by being able to afford to heat home. Note. Estimates are adjusted for age and population weights. Population weights were applied using STATA command ‘aweight’. Measures of health conditions are self-reported doctor diagnosis of each condition. Estimate based on sample described in Table 5.
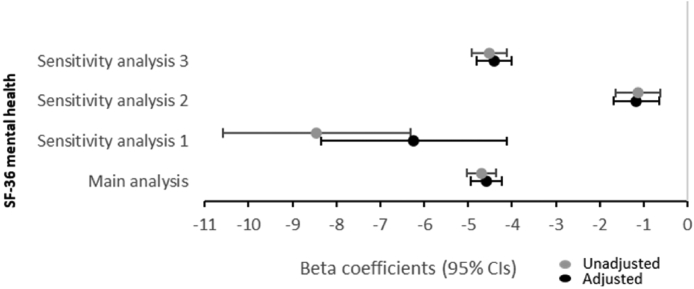
Exposure to cold housing and poor self-reported mental health
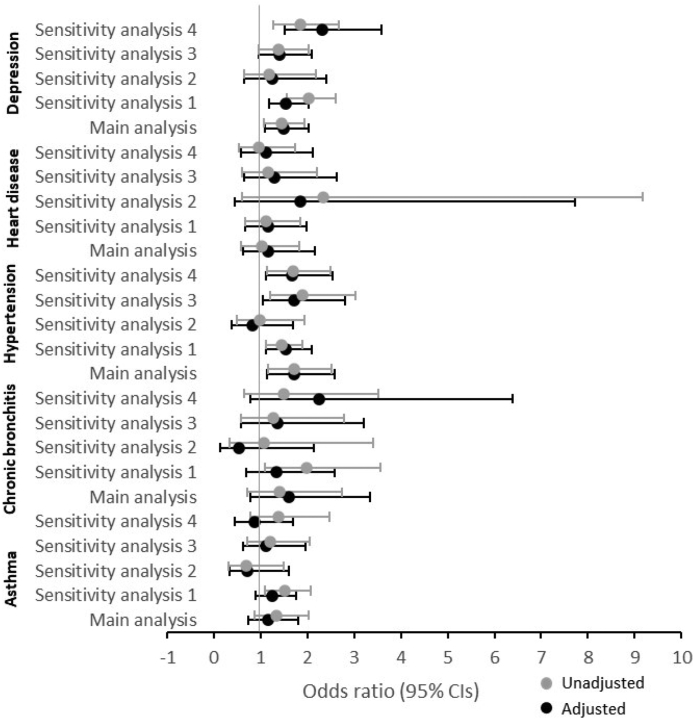
Fixed effects regression models give us insight into the likely causal effects of changes in energy poverty on change in health conditions. In adjusted model of the SF-36 mental health score we find evidence that when people can no longer afford to warm their homes, their mental health declines by 4.6 points (95% CI −4.93 to −4.24) - the estimated beta coefficient for the main analyses adjusted for confounders plotted in Fig. 2. Related to this, fixed effects models adjusted for confounding also provide support for an effect of energy poverty on the odds of reporting depression/anxiety (OR 1.49 95% CI 1.09 to 2.02) (see Fig. 3, main analysis).
Fig. 2.
Results from longitudinal regression analysis analyses summarising the effect of being unable to warm the house on self-reported mental health (SF-36). Note: Beta coefficients with 95% Confidence Intervals were estimated from fixed effects models for the main analysis and sensitivity analyses 2 and 3. Beta coefficients with 95% Confidence Intervals were estimated from regression models for sensitivity analyses 1. All adjusted models included age, household equivalised disposable income, Indigenous status, presence of children, number of adults and housing affordability stress. Sensitivity analysis 1 was additionally adjusted for gender. Main analysis included 30,457 people and 243,049 observations, sensitivity analysis 1 included 12,944 people, sensitivity analysis 2 included 19,351 people and 145,145 observations and sensitivity analysis 3 included 26,484 people and 189,884 observations.
Fig. 3.
Results from longitudinal regression analyses summarising the effect of being unable to warm the house on the odds of reporting chronic health conditions. Note: Beta coefficients with 95% Confidence Intervals were estimated from fixed effects models for the main analysis and sensitivity analyses 2 and 4. Beta coefficients with 95% Confidence Intervals were estimated from regression models for sensitivity analyses 1. All adjusted models included age, household equivalised disposable income, Indigenous status, presence of children, number of adults and housing affordability stress. Sensitivity analysis 1 was additionally adjusted for gender.
As we have used a self-reported exposure measure in these analyses, we designed three sensitivity analyses to test the robustness of our measure. First, (sensitivity analysis 1) we estimated CRE models using an exposure measure based on an alternative question in the survey (“When it is cold, are you able to keep at least one room of the house adequately warm”) asked in 2014 and 2018. Noting that because this question was asked in only two waves, we were unable to use fixed-effects regression and relied on a random-effects models (which is more prone to confounding from differences between people). Comparable with the main analyses indicating a 4.6 point decline in mental health with exposure to energy poverty, these models estimated a (greater than) 6-point decline on the SF-36 mental health scale for exposed people with Confidence Intervals overlapping with the estimates generated in the main analysis.
The second sensitivity analysis (sensitivity analysis 2) aimed to reduce bias from people's outcomes status affecting their reporting of exposure by incorporating the self-report of other people living in the house (specifically their co-resident partner). Findings support the direction of effect estimated in the main analysis reported in Fig. 2, although the estimated effect size is smaller. Specifically, the effect size indicates a reduction in SF-36 of just over one point on average compared to 4.6 points in the main analysis. Additionally, confidence intervals do not overlap with the main analysis for these models.
The third sensitivity analysis (sensitivity analysis 3) sought to reduce the likelihood of residual confounding from changes in housing due to relocation in intervening years between health outcome measurement. By restricting the sample to people who did not move from their home throughout the study period any change to householder's ability to keep their home warm is due to improved financial wellbeing and/or home modifications. These models support our observation of a causal effect of being unable to afford to keep homes warm on worsening mental health on the SF-36 mental health scale providing very similar estimates to the main analysis.
Exposure to cold housing and asthma, chronic bronchitis, hypertension, heart disease and depression
Looking across a range of chronic diseases, we found strong evidence of an effect of energy poverty on hypertension (OR 1.71, 95% CI 1.13 to 2.58) and depression (OR 1.49, 95% CI 1.09 to 2.02) in our main analyses that is adjusted for confounding (Fig. 3). For the remaining health conditions (including asthma, bronchitis/emphysema and depression) 95% confidence intervals crossed the null. The sample sizes used in the models reported in this Figure are summarised in Table 6.
Table 6.
Samples sizes used in analyses reported for exposure to cold housing and asthma, chronic bronchitis, hypertension, heart disease and depression.
| Asthma |
Chronic bronchitis or emphysema |
High Blood Pressure |
Heart diseases |
Depression or Anxiety |
|
|---|---|---|---|---|---|
| People/Obs | People/Obs | People/Obs | People/Obs | People/Obs | |
| Main Analysis | 1135/2941 | 347/902 | 1664/4424 | 664/1730 | 650/1655 |
| Sensitivity Analysis 1 | 13,943/13,943 | 13,943/13,943 | 13,943/13,943 | 13,943/13,943 | 13,943/13,943 |
| Sensitivity Analysis 2 | 650/1655 | 178/469 | 1067/2826 | 414/1094 | 967/2477 |
| Sensitivity Analysis 3 | 850/2137 | 307/779 | 1437/3738 | 598/1531 | 1411/3512 |
| Sensitivity analysis 4 | 615/1482 | 229/572 | 1600/4247 | 583/1526 | 1287/3184 |
In addition to sensitivity analysis 1 to 3 reported above, a fourth check (sensitivity analysis 4) was conducted for model's estimating onset of chronic disease. This involved excluding respondents who previously reported being diagnosed with the condition of interest to ensure new cases of each condition were being modelled. Generally, sensitivity analyses 1, 3 and 4 support the findings of the main analysis for hypertension and depression; noting however that the confidence intervals estimated in sensitivity analyses 3 cross the null for depression. Notably, estimates generated in sensitivity analysis 2 – where other household members reporting of exposure status was ascertained to verify respondent self-report – did not support associations observed in the main analysis for hypertension and depression suggesting reporting bias in our main analysis (Fig. 3).
Dynamics of exposure
To meet our objective of exploring the effects of exposure over time, we modelled exposure consistency and change over time in relation to each of the outcomes under consideration.
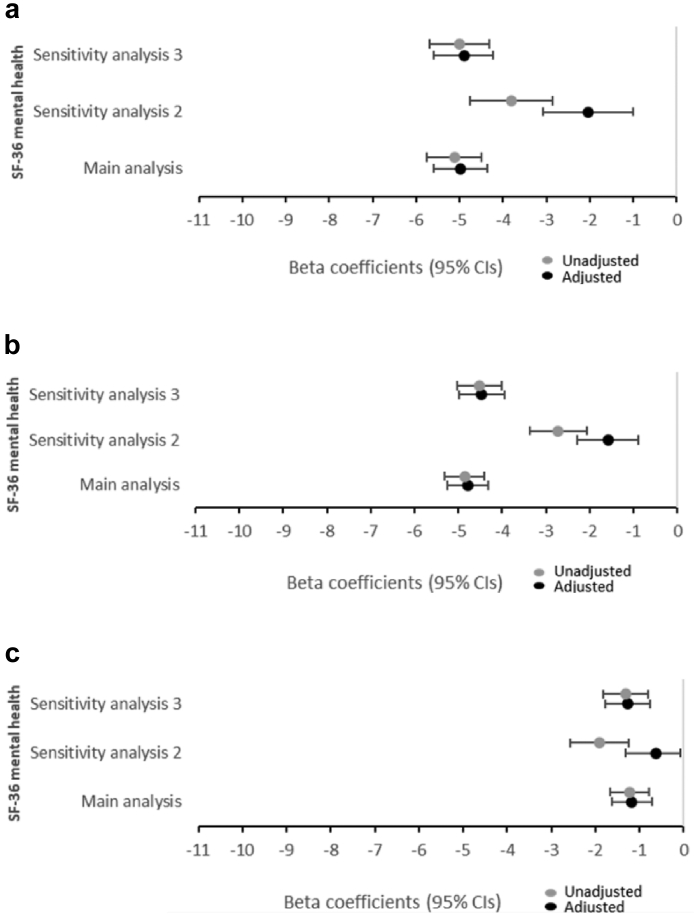
In models examining exposure to energy poverty over longer durations of time (two waves of measurement), we observed that mental health was on average around 5-points lower on the SF-36 mental health subscale in adjusted models (and about 2 points lower for sensitivity analysis 2) (Fig. 4a). People who could afford to warm their homes, after having difficulty doing so in past waves, recorded lower scores on the SF-36 than the reference group (OR −1.17, 95% CI −1.62 to −0.72) (Fig. 4c), however, this was not as low as for people who had reported energy poverty consistently in two consecutive waves of the survey (OR −4.97 95% CI −5.60, −4.35) (Fig. 4a) or shifted into energy poverty over the study period (OR −4.79 95% CI −5.24 to −4.33) (Fig. 4b).
Fig. 4.
Results from longitudinal regression analyses summarising the effect of being unable to warm the house on self-reported mental health (SF-36): a) consistently (i.e., for two consecutive waves of exposure) b) recently (newly reporting energy poverty) c) in the past (reporting energy poverty in past waves, but not the most recent wave). Note: Beta coefficients with 95% Confidence Intervals were estimated from correlated random effects models for the main analysis and sensitivity analyses 2. All adjusted models included age, gender, household equivalised disposable income, Indigenous status, presence of children, number of adults and housing affordability stress. Main analysis included 24,517 people and 197,009 observations.
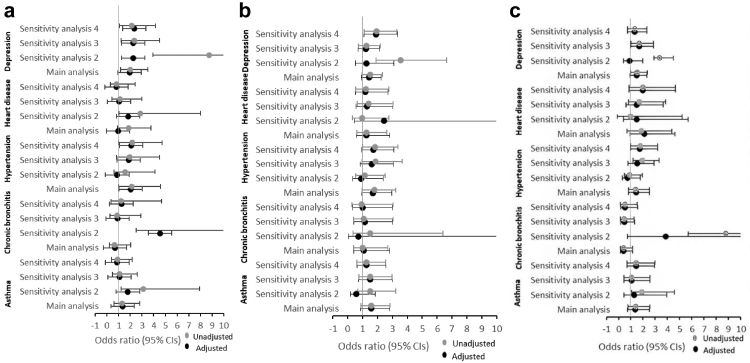
In relation to estimating the increased odds of chronic disease onset, the main analyses found people who reported two consecutive waves of exposure had increased odds of hypertension (OR 2.04, 95% CI 1.01 to 4.22) and depression (OR 1.95, 95% CI 1.12 to 3.41) (Fig. 5a). While the findings for hypertension were not strongly supported by sensitivity analyses, more consistent findings were observed for depression. In addition, there was little evidence that exposure to energy poverty either recently or in the past was associated with the onset of chronic health conditions (Fig. 5b and c).
Fig. 5.
The results from longitudinal regression analyses summarising the estimated effect of being unable to warm the home on the odds of reporting chronic health conditions a) consistently (i.e., for two consecutive waves of exposure) b) recently (newly reporting energy poverty) c) in the past (reporting energy poverty in past waves, but not the most recent wave). Note: Odd ratios with 95% Confidence Intervals were estimated from correlated random effects models for the main analysis and sensitivity analyses 2 and 3. All adjusted models included age, gender, household equivalised disposable income, Indigenous status, presence of children, number of adults and housing affordability stress.
The samples size for the analyses presented in Fig. 5 is reported in Table 7.
Table 7.
Samples sizes used in analyses reported for dynamics of exposure to cold housing and asthma, chronic bronchitis, hypertension, heart disease and depression.
| Asthma People/Obs |
Chronic bronchitis or emphysema People/Obs |
High Blood Pressure People/Obs |
Heart diseases People/Obs |
Depression or Anxiety People/Obs |
|
|---|---|---|---|---|---|
| Main Analysis | 17,539/34,216 | 17,539/34,216 | 17,539/34,216 | 17,539/34,216 | 17,539/34,216 |
| Sensitivity Analysis 2 | 12,562/23,762 | 12,562/23,764 | 12,562/23,764 | 12,562/23,764 | 12,562/23,764 |
| Sensitivity Analysis 3 | 16,095/29,389 | 16,095/29,389 | 16,095/29,389 | 16,095/29,389 | 16,095/29,389 |
| Sensitivity analysis 4 | 16,936/32,790 | 17,402/33,894 | 17,316/33,674 | 16,947/32,771 | 16,812/32,498 |
Negative control models
In addition to exploring the robustness of our findings by testing measurement of the exposure, we estimated the effect of being in energy poverty on cancer diagnosis as a negative control outcome (Table 8). That is, an outcome we would not expect to see significantly associated with the exposure. The negative control outcome models were not significant, suggesting that the observed relationships in our models are not likely to be severely biased.
Table 8.
The results from longitudinal regression analyses summarising the estimated effect of being unable to heat home on cancer diagnosis.
| The effect of changes in exposure on healtha | Odds Ratio (95% CI) |
|---|---|
| Energy poverty | 1.01 (0.58,1.76) |
| Exposure dynamicsb | |
| …into energy poverty | 1.01 (0.44,2.33) |
| …out of energy poverty | 1.45 (0.65,3.22) |
| …2 consecutive waves of energy poverty | 1.67 (0.64,4.32) |
Fixed effects regression models. Models adjusted for household income, presence of children, number of adults, housing affordability stress. Includes 731 people and 1938 observations.
Correlated random effect regression model. Models adjusted for age, gender, household income, ethnicity, presence of children, number of adults, housing affordability stress. Includes 17,539 people and 34,216 observations.
Discussion
The strongest finding of our analysis was the relationship between being exposure to energy poverty and mental health on the SF-36 validated mental health scale (examined in analyses relating to objective one) and dynamic patterns of exposure to energy poverty (objective two). This finding was observed in the main analysis and supported in our sensitivity analyses with alternative specifications of the exposure measure. This represents a relatively sizeable average decline in this measure and similar in scale to the difference in being in the lowest versus middle quintile of household income (see Table 5) and larger than has been previously reported for housing affordability stress on mental health.36 In addition, most models indicated an increased odds of reporting depression and anxiety onset upon energy poverty exposure. Based on this, we conclude that exposure to energy poverty negatively effects mental health and wellbeing, and likely increases the odds of depressive symptoms and anxiety.
We found little evidence of an association between energy poverty and respiratory conditions such as asthma and chronic bronchitis. This is likely a function of the questions used in the survey to determine health status. Importantly, the question (have you been told by a doctor or nurse that you have asthma/chronic bronchitis/emphysema) does not measure or indicate symptom exacerbation, only onset, giving a limited perspective of the association of this exposure with chronic respiratory illness. Importantly evidence of the role of thermal insulation in reducing use of medications for asthma in New Zealand37 suggests this exacerbation pathway is significant.
There was weak to moderate evidence of a relationship between energy poverty and hypertension onset in fixed effects models and in models that considered exposure over two measurement periods. This is consistent with findings from the WHO (2018) and well-executed randomised controlled trials that have examined temperature change in relation to elevated blood pressure and found evidence of a direct effect.25 We note, however, that an association between being unable to heat one's home and hypertension was not replicated in models where other household members reporting of this exposure was used to validate the main respondent's self-reported exposure measurement.
Our analyses have important policy and research implications. The finding of a strong mental health effect of energy poverty contributes a better understanding of the negative health impacts of being unable to heat homes. This compliments existing research evidence on the health effects of cold housing on cardiovascular and respiratory health conditions. Given this strong mental health effect, our findings support a role for energy poverty and cold housing remediation though social prescribing initiatives that provide energy subsidies. This has been effective in the United Kingdom, see for example the ‘Boiler on Prescription’ initiative38 and in interventions to improve housing conditions in New Zealand such as the Well Homes initiative.39 The broader health and wellbeing utility of improving housing conditions needs to be considered in evaluations of the efficacy of these initiatives.
Our findings also highlight the important role of energy security as a protector of human health as our climate changes. With extremes in temperature set to be greater and more frequently changing this century, our housing stock needs to be upgraded (and in some cases retired) to enable people to maintain a healthy indoor temperature efficiently, sustainably, and cost-effectively in their homes. Policy initiatives to reduce energy costs and improve housing conditions will be of increasing importance and need to be considered together. Our research adds weight and momentum to this pressing concern for Australian government and citizens and has implications relevant across the Western Pacific region.
Our analysis benefits from being based on a large, nationally representative longitudinal dataset, and the use of robust estimation techniques. It has several limitations, however. First, all the measures of exposure are based on self-report. This reporting is subject to bias – for example, people with lower mental health may be more likely to report negatively on their home environments. To ameliorate this potential source of bias, we have used alternative measures of energy poverty (using an alternative survey question), restricted exposure definition to cases validated by another household member and, also, considered alternative specifications (i.e., examining exposure over two waves of data collection rather than one alone). In each of these alternative models, the negative mental health effect of being unable to warm homes remained, which suggests this is a robust finding.
Second, the measures of asthma, chronic bronchitis, hypertension, heart disease and depression and anxiety are measured at intervals of four years. We cannot ascertain if changes in health status occurred directly after changes reported in exposure. While we acknowledge this as a limitation, we also note that the strongest direction of effect is likely to run from exposure to energy poverty to poorer health and that additional analyses of the sample where more than one occupant needs to have recorded that their home cannot be heated goes some way to verifying that the extent to which this aspect of the analyses has biased study findings is small.
Third, our sensitivity analysis 2 – that used the alternative question relating to indoor warmth was only available for waves 14 and 18 whereas outcome measurement was only available at wave 17. This resulted in a temporal mismatch between exposure and outcome in these models. We have assumed that if waves 14 and 18 recorded no energy poverty, then we regarded the household to be unexposed. Otherwise, exposure was assumed.
Fourth, we have not taken the spatial distribution of exposure to energy poverty into account in our models. The extent to which this exposure is concentrated in specific parts of Australia remains an important research question for future study.
Fifth, we have not accounted for the potential for attrition from the longitudinal sample to introduce selection bias. We note that selection bias occurs when attrition is associated with both the exposure and outcome. For fixed effects analyses to be biased by selection, attrition would need to be associated with both change in energy poverty status and change in outcome—dependently.40 Past modelling of dependence in change in an Australian longitudinal cohort examining poverty and health suggests that it is unlikely for fixed effects models (i.e., the models used to examine study objective one)41; however results from the CRE models may be affected to an unknown extent (i.e., the models used to examine study objective two).
Finally, and importantly, we did not have measure of the condition of people's homes and, consequently, could not assess if this was a source of residual confounding in the study. Moreover, we did not have information on climatic or environment conditions at the time of the survey. Future studies should examine the extent to which these factors explain associations observed in this study.
Conclusion
Our study highlights how exposure to energy poverty, or being unable to adequately warm homes, reduces occupants’ mental health. Specifically, people living in housing they cannot afford to warm report poorer mental health and are more likely to report depression/anxiety. These findings suggest a considerable and preventable mental health burden, alongside the more widely researched cardiovascular and respiratory disease pathways from living in homes that cannot be adequately warmed. Both energy poverty and housing temperature are important priorities for action to protect health and reduce health inequities in the face of rising energy costs and our changing climate.
Contributors
Rebecca Bentley: Conceptualization, Methodology, Investigation, Writing – original draft, Writing – review & editing. Lyrian Daniel: Conceptualization, Investigation, Writing – review & editing. Yuxi Li: Methodology, Investigation, Writing – review & editing. Emma Baker: Conceptualization, Writing – review & editing. Ang Li: Methodology, Investigation, Writing – review & editing.
Data sharing statement
The data used are available free of charge to researchers through the National Centre for Longitudinal Data Dataverse at the Australian Data Archive (https://dataverse.ada.edu.au/dataverse/ncld). Access is subject to approval by the Australian Government Department of Social Services and is conditional on signing a license specifying terms of use.
Declaration of interests
We declare no competing interests.
Acknowledgments
This study was funded by a grant from the NHMRC Centre of Research Excellence in Healthy Housing (APP1196456; principal investigator [CI] Rebecca Bentley, Melbourne School of Population and Global Health, University of Melbourne) and NHMRC Ideas Grant (APP2004466; principal investigator [CI] Rebecca Bentley, Melbourne School of Population and Global Health, University of Melbourne). This study uses unit record data from the HILDA Survey, conducted by the Melbourne Institute of Applied Economic and Social Research on behalf of the Australian Government Department of Social Services (release 20; https://doi.org/10.26193/PI5LPJ). The findings and views reported in this Article, however, are those of the authors and should not be attributed to the Australian Government, the Department of Social Services, or the Melbourne Institute.
References
- 1.Saeki K., Obayashi K., Kurumatani N. Platelet count and indoor cold exposure among elderly people: a cross-sectional analysis of the HEIJO-KYO study. J Epidemiol. 2017;27(12):562–567. doi: 10.1016/j.je.2016.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lloyd E.L., McCormack C., McKeever M., Syme M. The effect of improving the thermal quality of cold housing on blood pressure and general health: a research note. J Epidemiol Community Health. 2008;62(9):793–797. doi: 10.1136/jech.2007.067835. [DOI] [PubMed] [Google Scholar]
- 3.Umishio W., Ikaga T., Kario K., et al. Electrocardiogram abnormalities in residents in cold homes: a cross-sectional analysis of the nationwide Smart Wellness Housing survey in Japan. Environ Health Prev. 2021;26(1) doi: 10.1186/s12199-021-01024-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shiue I., Shiue M. Indoor temperature below 18 degrees C accounts for 9% population attributable risk for high blood pressure in Scotland. Int J Cardiol. 2014;171(1):e1–e2. doi: 10.1016/j.ijcard.2013.11.040. [DOI] [PubMed] [Google Scholar]
- 5.Shiue I. Cold homes are associated with poor biomarkers and less blood pressure check-up: English Longitudinal Study of Ageing, 2012-2013. Environ Sci Pollut Res Int. 2016;23(7):7055–7059. doi: 10.1007/s11356-016-6235-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Umishio W., Ikaga T., Kario K., et al. Cross-sectional analysis of the relationship between home blood pressure and indoor temperature in winter a nationwide smart wellness housing survey in Japan. Hypertension. 2019;74(4):756–766. doi: 10.1161/HYPERTENSIONAHA.119.12914. [DOI] [PubMed] [Google Scholar]
- 7.Umishio W., Ikaga T., Kario K., et al. Association between indoor temperature in winter and serum cholesterol: a cross-sectional analysis of the smart wellness housing survey in Japan. J Atherosclerosis Thromb. 2022 doi: 10.5551/jat.63494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shaw M. Housing and public health. Annu Rev Public Health. 2004;25:397–418. doi: 10.1146/annurev.publhealth.25.101802.123036. [DOI] [PubMed] [Google Scholar]
- 9.Free S., Howden-Chapman P., Pierse N., Viggers H. More effective home heating reduces school absences for children with asthma. J Epidemiol Commun Health. 2010;64(5):379–386. doi: 10.1136/jech.2008.086520. [DOI] [PubMed] [Google Scholar]
- 10.Donaldson G.C., Wedzicha J.A. The causes and consequences of seasonal variation in COPD exacerbations. Int J Chronic Obstr Pulm Dis. 2014;9:1101. doi: 10.2147/COPD.S54475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.D'Amato M., Molino A., Calabrese G., Cecchi L., Annesi-Maesano I., D'Amato G. The impact of cold on the respiratory tract and its consequences to respiratory health. Clin Transl Allergy. 2018;8(1):1–8. doi: 10.1186/s13601-018-0208-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hyndman S. Housing dampness and health amongst British Bengalis in East London. Soc Sci Med. 1990;30(1):131–141. doi: 10.1016/0277-9536(90)90336-q. [DOI] [PubMed] [Google Scholar]
- 13.Liddell C., Guiney C. Living in a cold and damp home: frameworks for understanding impacts on mental well-being. Publ Health. 2015;129(3):191–199. doi: 10.1016/j.puhe.2014.11.007. [DOI] [PubMed] [Google Scholar]
- 14.Mohan G. The impact of household energy poverty on the mental health of parents of young children. J Public Health. 2022;44(1):121–128. doi: 10.1093/pubmed/fdaa260. [DOI] [PubMed] [Google Scholar]
- 15.Sawyer A., Sherriff N., Bishop D., Darking M., Huber J.W. It's changed my life not to have the continual worry of being warm" - health and wellbeing impacts of a local fuel poverty programme: a mixed-methods evaluation. BMC Publ Health. 2022;22(1):786. doi: 10.1186/s12889-022-12994-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chimed-Ochir O., Ikaga T., Ando S., et al. Effect of housing condition on quality of life. Indoor Air. 2021;31(4):1029–1037. doi: 10.1111/ina.12819. [DOI] [PubMed] [Google Scholar]
- 17.Poortinga W., Rodgers S.E., Lyons R.A., et al. The health impacts of energy performance investments in low-income areas: a mixed-methods approach. Public Health Res. 2018;6(5):1–182. [PubMed] [Google Scholar]
- 18.Clair A., Baker E. Cold homes and mental health harm: evidence from the UK household longitudinal study. Soc Sci Med. 2022;314 doi: 10.1016/j.socscimed.2022.115461. [DOI] [PubMed] [Google Scholar]
- 19.Churchill S.A., Smyth R. Energy poverty and health: panel data evidence from Australia. Energy Econ. 2021;97 [Google Scholar]
- 20.Singh A., Mizdrak A., Daniel L., et al. Estimating cardiovascular health gains from eradicating indoor cold in Australia. Environ Health. 2022;21(1):54. doi: 10.1186/s12940-022-00865-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daniel L., Baker E., Beer A., Pham N.T.A. Cold housing: evidence, risk and vulnerability. Hous Stud. 2021;36(1):110–130. [Google Scholar]
- 22.Riva M., Makasi S.K., Dufresne P., O'Sullivan K., Toth M. Energy poverty in Canada: prevalence, social and spatial distribution, and implications for research and policy. Energy Res Social Sci. 2021;81 [Google Scholar]
- 23.MacArthur J.L., Hoicka C.E., Castleden H., Das R., Lieu J. Canada's Green New Deal: forging the socio-political foundations of climate resilient infrastructure? Energy Res Social Sci. 2020;65 [Google Scholar]
- 24.Saeki K., Obayashi K., Iwamoto J., et al. Influence of room heating on ambulatory blood pressure in winter: a randomised controlled study. J Epidemiol Community Health. 2013;67(6):484–490. doi: 10.1136/jech-2012-201883. [DOI] [PubMed] [Google Scholar]
- 25.Saeki K., Obayashi K., Kurumatani N. Short-term effects of instruction in home heating on indoor temperature and blood pressure in elderly people: a randomized controlled trial. J Hypertens. 2015;33(11):2338–2343. doi: 10.1097/HJH.0000000000000729. [DOI] [PubMed] [Google Scholar]
- 26.Howden-Chapman P., Matheson A., Crane J., et al. Effect of insulating existing houses on health inequality: cluster randomised study in the community. BMJ. 2007;334(7591):460. doi: 10.1136/bmj.39070.573032.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Umishio W., Ikaga T., Fujino Y., et al. Disparities of indoor temperature in winter: a cross-sectional analysis of the Nationwide Smart Wellness Housing Survey in Japan. Indoor Air. 2020;30(6):1317–1328. doi: 10.1111/ina.12708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization . World Health Organization; 2018. WHO housing and health guidelines. [Google Scholar]
- 29.Nicole W., Mark W. The household, income and labour dynamics in Australia (HILDA) survey. J Econom Statistics. 2021;241(1):131–141. [Google Scholar]
- 30.Bosch J., Palència L., Malmusi D., Marí-Dell'Olmo M., Borrell C. The impact of fuel poverty upon self-reported health status among the low-income population in Europe. Hous Stud. 2019;34(9):1377–1403. [Google Scholar]
- 31.Gunasekara F.I., Richardson K., Carter K., Blakely T. Fixed effects analysis of repeated measures data. Int J Epidemiol. 2014;43(1):264–269. doi: 10.1093/ije/dyt221. [DOI] [PubMed] [Google Scholar]
- 32.Schunck R. Within and between estimates in random-effects models: advantages and drawbacks of correlated random effects and hybrid models. STATA J. 2013;13(1):65–76. [Google Scholar]
- 33.Fay R., Authier M., Hamel S., et al. Quantifying fixed individual heterogeneity in demographic parameters: performance of correlated random effects for Bernoulli variables. Methods Ecol Evol. 2022;13(1):91–104. [Google Scholar]
- 34.Wooldridge J.M. Correlated random effects models with unbalanced panels. J Econom. 2019;211(1):137–150. [Google Scholar]
- 35.Arnold B.F., Ercumen A. Negative control outcomes: a tool to detect bias in randomized trials. JAMA. 2016;316(24):2597–2598. doi: 10.1001/jama.2016.17700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bentley R., Baker E., Mason K., Subramanian S., Kavanagh A.M. Association between housing affordability and mental health: a longitudinal analysis of a nationally representative household survey in Australia. Am J Epidemiol. 2011;174(7):753–760. doi: 10.1093/aje/kwr161. [DOI] [PubMed] [Google Scholar]
- 37.Fyfe C., Barnard L.T., Douwes J., Howden-Chapman P., Crane J. Retrofitting home insulation reduces incidence and severity of chronic respiratory disease. Indoor Air. 2022;32(8) doi: 10.1111/ina.13101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Burns P., Coxon J. Gentoo Group; Sunderland: 2016. Boiler on Prescription Trial Closing Report. [Google Scholar]
- 39.Pierse N., White M., Ombler J., et al. Well homes initiative: a home-based intervention to address Housing-Related ill health. Health Educ Behav. 2020;47(6):836–844. doi: 10.1177/1090198120911612. [DOI] [PubMed] [Google Scholar]
- 40.Lash T.L., Fox M.P., Fink A.K. Springe; NewYork: 2009. Applying Quantitative Bias Analysis to Epidemiologic Data. [Google Scholar]
- 41.Bentley R., Simons K., Kvalsvig A., Milne B., Blakely T. Short-run effects of poverty on asthma, ear infections and health service use: analysis of the Longitudinal Study of Australian Children. Int J Epidemiol. 2021;50(5):1526–1539. doi: 10.1093/ije/dyab059. [DOI] [PubMed] [Google Scholar]