Abstract
Background and Objective
Adolescence is a critical period for human psychological and social development. Mental illness during this time can cause long-lasting damage on both individual and social levels. A growing body of psychological treatments has been employed to treat psychopathology; however, no reviews of these psychological interventions have been conducted. To fill the gap, this study reviewed articles published within the last decade that focused on the efficacy of psychological treatments of adolescent psychopathology.
Methods
Peer-reviewed, original studies published between January 1, 2012, and June 1, 2022 were identified using the PubMed/MEDLINE, PsycINFO, and Google Scholar databases. After reasonable deletion following the exclusion criteria, a total of 50 articles focusing on clinical and subclinical psychopathology were finally reviewed.
Key Content and Findings
Psychological treatments are widely used in treating psychopathology and exhibit efficacy for adolescent psychopathology. Cognitive behavior therapy and family-based therapy are the most commonly used therapies. Many treatments in the review were conducted in the family and school contexts. Although the recent literature is encouraging, future studies with rigorous experimental designs regarding the samples and methodology are required. Future studies should also pay more attention to unsolved psychopathology and identify the effective elements for improvements in interventions and outcomes.
Conclusions
This review provides a full view of studies on the efficacy of psychological treatments for adolescent psychopathology. It can be utilized to inform recommendations for healthcare services to improve treatment outcomes.
Keywords: Adolescents, psychopathology, psychological treatment
Introduction
Adolescence is a critical period for significant psychological and social development, during which a child gradually becomes an adult, and is generally characterized as the period from 10 to 21 years old (1). In this period, adolescents begin to build their self-identity, interpersonal relationships, and professional careers, which substantially influences their later lives. However, psychopathology in adolescence can disrupt or severely impede the development process and cause long-lasting damage.
Adolescent psychopathology is broadly defined in this review, including both clinical and subclinical psychopathology, as well as internalizing and externalizing problems. Left untreated, adolescent psychopathological problems have been proved to lead to poor social functioning, impaired academic achievement, unemployment, and greater risk of suicide and self-harm (2). Furthermore, children and adolescents with psychopathology may put added pressure on their families and society. Families of adolescents with psychopathology need to spend considerable time and energy taking care of them. These adolescents also need more educational and social healthcare services, imposing costs on society (3). The World Economic Forum has projected that mental ill-health will account for more than half of the global economic burden attributable to non-communicable diseases by 2030, at US $6 trillion (4). Collectively, these observations suggest the urgency of establishing effective intervention programs for adolescent psychopathology.
Social context and psychological characteristics play significant roles in adolescent psychopathology. Academic stress, relationship issues, and socioeconomic and social challenges are common environmental stressors for youth vulnerability, while connectedness and social support are protective factors (5). The family and school, as the primary agents of socialization for adolescents, are crucial contexts influencing psychopathology (6-9). Specifically, family risk factors include physical abuse (6), parental psychopathology (7,8), and poor family function (8). At school, bullying is a significant risk factor; anxiety, depression, substance use, eating disorders, and psychosomatic symptoms are frequent among both the culprits and the victims of bullying (9). Poor interpersonal relationships at school can also impede adolescent mental health (10), whereas high-quality relationships can reduce psychopathology induced by interpersonal trauma (11).
Psychological characteristics, such as low self-esteem, are observed in depression and anxiety and eating disorders (12-15). Specifically, depressive and anxious individuals tend to perceive themselves as worthless, incompetent, and inadequate (13). Individuals with eating disorders usually show low levels of self-acceptance and high levels of self-blame (15). Lack of coping skills is another risk factor for mental disorders. Adolescents with maladaptive coping strategies may not be able to effectively manage stress, thereby increasing the risk of depression and anxiety (16-18). Cognitive risk factors have received considerable attention with respect to adolescent psychopathology (19). Threat bias, intolerance of uncertainty, and learned avoidance behavior are extensively found in anxiety and depression disorders (20). As such, cognitive bias has been the main target for treatments to improve emotional distress and problematic behaviors. Emotional regulation has been studied as a protective individual factor and as a promising treatment target in a broad range of mental disorders (21). The two most commonly used strategies are cognitive reappraisal, which refers to re-evaluating a situation to diminish its emotional impact, and expressive suppression, which refers to inhibiting the outward expression of inner emotions. These strategies are critical for adolescents to regulate their distress and feelings (22,23).
Psychological treatments are defined as interventions wherein verbal communication between a therapist and a client is the core element, or a systematic psychological method is written in book format or on a website, and the client works through it more or less independently with some personal support from a therapist. Psychological treatments for adolescent psychopathology have many advantages. First, they are non-invasive and have no side effects compared with pharmacotherapy (24). Second, psychological interventions are evidenced to increase adherence to pharmacotherapy for better treatment effects (25). Third, psychological treatments can reduce symptoms and help adolescents improve their cognitive and behavioral patterns, increasing their ability to face challenges.
Many challenges exist in the treatment of adolescent mental disorders (26). First, stigma about mental health and lack of education and awareness of mental disorders discourage parents from seeking psychological treatment for their children (27). Moreover, a professional mental health treatment is generally inadequate, especially in rural areas (28). Finally, more effective, feasible treatments for adolescent psychopathology are required.
A growing body of psychological treatments, such as cognitive behavior therapy (CBT), psychoanalytic therapy, and family-based treatment (FBT), has been employed to treat psychopathology. CBT theory suggests that our thoughts, emotions, body sensations, and behavior are all connected; therefore, what we think and do affects the way we feel. CBT helps people identify and change thinking and behavior patterns that are harmful or ineffective, replacing them with more accurate thoughts and functional behaviors. Some CBT-based programs are specifically created for certain psychopathological problems. For example, CBT for insomnia (CBTI) is recommended as the first-line treatment for insomnia. It generally comprises stimulus control therapy, relaxation training, and restriction of time in bed, each of which is an effective intervention individually, combined with sleep hygiene education, psychoeducation, and cognitive therapy. Psychoanalytic therapy is a form of talk therapy based on psychoanalysis (29). Psychoanalysis suggests that everyone is subject to a flux of internal conditions, which, to some extent, are always going to be difficult for individuals to deal with or fully acknowledge (30). With the help of psychoanalysts, clients can obtain detailed familiarity with the nature of these internal states and more control of their problems (30). FBT is based on family systems theory (31,32), which emphasizes the relational and contextual nature of human behavior and holds the idea that individual functioning is reciprocally interconnected to that of other individuals within one’s primary relational context—the family (33). This system-oriented approach aims at changing family patterns with the goal of contributing to improvements in adolescents’ mental health.
Many clinical studies have examined the efficacy of various therapeutic interventions in the last decade; however, no reviews of these psychological interventions have been conducted. A comprehensive review can contribute to an overall understanding of the advances of psychological treatments for adolescent psychopathology. Specifically, it could clarify (I) the main treatments for different adolescent psychopathology; (II) the efficacy of those treatments; and (III) the problems existing in current treatment. This review can provide direction for future clinical research aimed at developing more effective interventions and help clinicians improve treatment outcomes. The articles in this review focused on treatment efficacy and integrated programs for adolescents with diagnosed or sub-threshold psychopathology to provide a comprehensive view of the field. Subsequently, suggestions regarding the direction of future treatment research are offered herein. We present this article in accordance with the Narrative Review reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-589/rc).
Methods
In line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (34), a systematic search was undertaken on PubMed/MEDLINE, PsycINFO, and the first 10 pages of Google Scholar for peer-reviewed, original publications between January 1, 2012, and June 1, 2022. The primary search terms used were “adolescent,” “psychopathology,” “treatment,” and “intervention.” The detailed research strategy summary is shown in Table 1.
Table 1. Summary of the search strategy.
| Items | Specification |
|---|---|
| Date of search | 2022.6.30 |
| Databases and other sources searched | PubMed/MEDLINE, PsycINFO, Google Scholar |
| Search terms used | “adolescent” and “psychopathology” and “treatment” or “intervention” |
| Timeframe | 2012.1.1–2022.6.1 |
| Inclusion and exclusion criteria | Inclusion: focus on the efficacy of psychological treatment; subjects aged between 10 and 21 years; English language |
| Exclusion: contains no data, contains duplicate data, contains data that is non-relevant, review study, not focused on the efficacy of psychological treatment | |
| Selection process | Yu Li searched the three databases with the terms “adolescent” and “psychopathology” and “treatment” or “intervention”. The article types were constrained to either “clinical trial” and “randomized controlled trial” on PubMed, PsycINFO, and the first 10 pages of Google Scholar. All authors reviewed these articles and came to a consensus |
Exclusion criteria
As shown in Figure 1, 906 articles were first identified; 708 were excluded because they contained no data or were duplicates, reviews, or considered not relevant. Three additional articles were excluded because they did not focus on the efficacy of psychological treatments. Furthermore, participants’ age was constrained to adolescence (10–21 years old), excluding another 145 articles. A total of 50 articles were finally included in the review.
Figure 1.
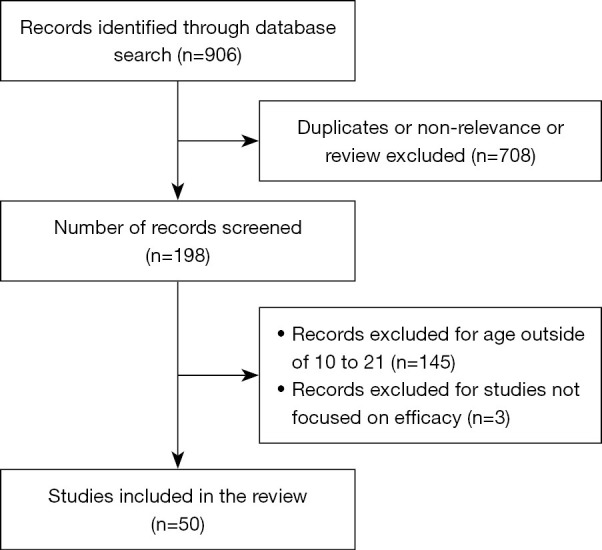
Processing of records.
The reviewed articles included 10 kinds of psychopathology: anxiety, depression, eating disorders, attention deficit hyperactivity disorder (ADHD), externalizing problems, autism spectrum disorder, substance use, insomnia, borderline personality disorder, and psychosis. The studies were reviewed based on which psychopathology they discussed; studies that did not target specific types of psychopathology are summarized in the general Mental Health section. Studies considering already-diagnosed adolescent patients were defined as clinical research, whereas those targeting a community sample were defined as subclinical research. Information regarding the sample, methodology, and effect size from all reviewed articles is presented in Table S1.
Discussion
Anxiety
Subclinical
Cognition-based interventions, such as CBT and cognitive bias modification (CBM), were common for treating anxiety in adolescents. CBT included psychoeducation, task concentration training, cognitive restructuring, exposure, and relapse prevention, whereas CBM included tasks to modify interpretation and attention bias. Capron et al. (35) examined the efficacy of computer-based CBM for interpretation bias interventions to reduce adolescents’ sensitivity to anxiety. In this intervention, individuals were presented with ambiguous information, following which they had to make a decision facilitating the interpretation of this ambiguity. Bias was shaped by structuring feedback to reward one style of interpretation over another (usually positive/benign over negative/threatening). Results showed that CBM can reduce adolescent sensitivity to anxiety. de Hullu et al. (36) compared the efficacy of CBM via the Internet and CBT in reducing adolescent social and test anxiety. The results indicated that neither intervention was superior to the control condition; social and test anxiety declined at the two-year follow-up in all three groups.
Several new programs have been developed recently, such as Dojo (22) and Anxiety Sensitivity Amelioration Programs for Youth (37). Dojo is an emotional-management video game comprising two strategies: emotion regulation training and heart rate variability biofeedback. Emotion regulation training encompasses a wide range of processes that affect the occurrence, duration, intensity, and expression of emotion. Heart rate variability biofeedback is a technique that teaches adolescents a way to alter physiological activity to improve health, performance, and learning. Scholten et al. (22) found that the anxiety symptoms in both Dojo and control conditions significantly decreased; however, no difference was observed between the two conditions. The Anxiety Sensitivity Amelioration Programs for Youth include psychoeducation regarding the nature of anxiety/fear and anxiety sensitivity, and parental training in conducting exposure exercises. Knapp et al. (37) found that this program could significantly decrease anxiety sensitivity.
Clinical
A computer-based Attention Bias Modification Treatment (ABMT) was used as an adjuvant for adolescents with anxiety disorders who did not respond to CBT (38). This treatment focused on weakening threat-related attention bias. ABMT is based on the idea that attention bias can be shaped via repetitive computer-based training methods. The intervention was based on the attention bias assessment task. Participants were presented with a unique set of paired angry and neutral faces on the top and bottom of the screen; a probe replaced the neutral face on 100% of the trials and the participants were required to identify the direction of the probe. The probe remained on screen until the participant responded, and then the next trial began immediately. Reaction time differences of incongruent minus congruent trials provided a measure of attention bias, such that positive values indicated bias toward angry faces and negative values indicated bias away from angry faces. The results showed that it could reduce anxiety and depression symptoms in adolescents who exhibited poor response to CBT.
Depression
Subclinical
CBT was found to significantly reduce adolescent depression compared with non-specific and no-intervention control conditions (39). Kindt et al. (40) combined CBT, social problem-solving, and coping skills to create a depression prevention program called Op Volle Kracht. They tested its effectiveness in adolescents from low-income households whose parents had psychopathology and found that adolescents exhibited a moderate decrease in depressive symptoms in the Op Volle Kracht group compared with those in the control condition. Gest et al. focused on chronotherapeutic treatments on adolescents with moderate to severe depressive symptoms (41). Chronotherapeutic treatments are based on circadian principles and are conducted by the manipulation of “external zeitgebers” to influence patients’ circadian rhythm. It consists of bright light therapy (i.e., exposing patients to bright light in the morning) and wake therapy (i.e., sleep deprivation). Results showed that chronotherapeutic treatments reduced depressive symptoms and improved sleep quality, with the bright light therapy being more effective than the one-night wake therapy.
Eating disorders
Clinical
Treatments for eating disorders primarily focus on adolescents with anorexia nervosa, which is often treated with FBT. FBT tends to work with both parents and children to encourage parental control of children’s eating-related behaviors. Trainor et al. (42) found that FBT could decrease the incidence of comorbid psychiatric conditions (i.e., major depressive disorder, generalized anxiety disorder, and panic disorder/agoraphobia) in adolescents with anorexia nervosa. Lock et al. (43) compared the efficacy of FBT with systemic family therapy. In their study, FBT focused on facilitating weight gain, whereas systemic family therapy addressed family processes. The results showed that FBT reduced hospitalization compared with systemic family therapy. Lock et al. (44) added direct coaching at meal times to FBT to create Intensive Parental Coaching for adolescents with anorexia nervosa who are poor early responders to FBT. They found that this improved intervention was equally effective with FBT and could help poor early responders achieve full weight restoration. Herscovici et al. (45) combined FBT with a family meal intervention. The intervention focused on fostering parents’ ability to assist and/or encourage their children to consume food or beverages within an agreed time. The intervention takes a non-blaming stance to externalize the problem and explores the merits and disadvantages for the patients during recovery. Results showed that combined therapy is equally effective with FBT.
Four studies compared the efficacy of FBT and adolescent focus therapy (AFT). AFT focuses on ameliorating eating disorder symptoms in the context of examining common themes in adolescent development. Accurso et al. (46) found that both FBT and AFT improved most psychological symptoms in adolescents with anorexia nervosa. Moreover, adolescents with more severe, complex, and enduring clinical presentations tended to benefit more from the treatments. Le Grange et al. (47) found that adolescents with more severe eating disorder-related psychopathology had better outcomes with FBT than AFT. Furthermore, maternal and paternal expressed emotions may impact treatment outcomes in FBT and AFT, highlighting the attendance of parental expressed emotion in clinical settings (48). Ciao et al. (49) explored the differences between FBT and AFT’s effect on family functioning, which is related to remission in anorexia nervosa families. The results showed that FBT had a more positive impact than AFT.
Eisler et al. (50) compared the efficacy of single- and multifamily therapy for adolescents with anorexia nervosa. Both interventions focus on helping families overcome their sense of isolation and stigmatization and maximize their own resources. However, multifamily therapy includes five to seven families and is provided in a more intensive form that allows families to gain support from each other. Results showed that both treatments improved anorexia nervosa symptoms, but multifamily therapy was more effective.
Philipp et al. (51) recently created a caregivers’ skill training program known as “Supporting Carers of Children and Adolescents with Eating Disorders in Austria” to alleviate caregivers’ distress and burden. This program provides parents with coping and communication strategies, whether in the form of a workshop or online, to help them support their children with anorexia nervosa. Both forms are equally effective in improving symptoms.
Some programs to improve cognitive weakness in adolescents with anorexia nervosa have been implemented. For example, Biney et al. (52) used a CBT approach to provide psychoeducation targeted at raising girls’ self-esteem. The intervention group showed greater improvement in anorexia nervosa symptoms than the control group. Similarly, Herbrich et al. (53) examined the efficacy of cognitive remediation therapy, a specialized treatment approach targeting cognitive weaknesses in anorexia nervosa; however, no significant differences were observed between the intervention and control groups. Glashouwer et al. (54) designed a computer-based evaluative conditioning intervention to improve the body image of 51 adolescent girls with eating disorders. Participants in this intervention were trained to select pictures of their own and other people’s bodies, with their own pictures systematically followed by friendly smiling faces. However, this treatment showed no effects.
Giel et al. (55) created a lifestyle intervention for obese adolescents comprising three parts: increasing physical activity, nutritional recommendations, and close surveillance by one physician. The results showed that a six-month lifestyle intervention can reduce weight in adolescents.
ADHD
Clinical
Boyer et al. (56) compared the efficacy of two kinds of CBT on adolescents with ADHD: a planning-focused treatment and a solution-focused treatment. The planning-focused treatment involves providing planning and organizational skills on a fixed subject, whereas solution-focused treatment involves guiding the adolescents toward a solution with fixed questions about the encountered problem. Adolescents in the planning-focused treatment had a significantly higher alliance score than those in the less-structured solution-focused treatment. Alliance was related to treatment outcomes in the solution-focused treatment, but not in the planning-focused treatment.
The efficacy of school-based interventions targeting homework problems for adolescents with ADHD has been evaluated (57). The authors focused on two brief interventions: the Homework, Organization, and Planning Skills intervention, and the Completing Homework by Improving Efficiency and Focus intervention. The former intervention covers three main skill areas: school materials organization and management, homework recording, and planning/time management. Based on the former, the latter intervention also implements a behavior management and points system, sets work completion goals, and has the student complete homework and prepare for tests. The results showed that both intervention groups showed improvements in homework problems and organizational skills compared with the waitlist group. Moreover, the Homework, Organization, and Planning Skills intervention was superior to Completing Homework by Improving Efficiency and Focus in adolescents with more severe psychopathology and behavioral dysregulation.
Recently, two versions of a manualized parent–teen psychosocial treatment program were designed (58). The first comprises ten 60-min weekly group sessions of parent and adolescent skills training, and the second comprises eight 90-min weekly sessions of dyadic skills training blended with motivational interviewing. Results showed that both groups had equivalent overall outcomes, but the latter had superior effectiveness when parents had elevated ADHD or depression symptoms or showed high levels of conflict with teens.
Externalizing problems
Subclinical
Weiss et al. (59) used multisystemic therapy to treat adolescent conduct problems. The therapy focuses on multiple systems, targeting behavior disturbances in individuals, family, peers, and dyadic relationships. The goal is to empower parents to help manage their adolescent’s social and personal life more adaptively. Results showed that both the multisystemic therapy group and the usual-services control group showed a decelerating decrease in symptoms, but improvement was greater in the intervention group. Caldwell et al. (60) implemented a specialized intensive treatment program for 127 male adolescents with delinquent behaviors. This program focused on improving their daily interpersonal functioning and creating conventional social bonds to displace delinquent associations and activities. Results showed that callous/unemotional, narcissistic, and impulsive traits changed significantly over the course of treatment, and the decrease in these traits could predict positive institutional behavior. This effect was observed even in adolescents with severe behavioral disorders.
Van Ryzin et al. (61) created a family-based program called the Social Ecology of Family Check-up for adolescent antisocial behavior. The program was designed to support parents’ accurate appraisal of their child’s risk status and their own parenting practices, and to help parents identify appropriate services and reasonable change strategies. Over time, results showed that the program significantly reduced adolescent antisocial behaviors.
Autism spectrum disorder
Clinical
Recently, Idris et al. (62) created the Program for the Education and Enrichment of Relational Skills (PEERS®) for adolescents with autism spectrum disorder. The program involves manualized social-skills interventions involving parents for how to best coach their children socially. PEERS® group was found to increase adolescents’ social skills compared with the control group, from both adolescent self-report and parental-report.
Substance use
Clinical
Hendriks et al. (63) compared the effectiveness of multidimensional family therapy and CBT in adolescents with cannabis abuse or dependence disorders. They found that both were equally effective in reducing cannabis use; however, older adolescents (17–18 years old) benefited considerably more from CBT, and younger adolescents (13–16 years old) benefited considerably more from multidimensional family therapy.
Subclinical
Lammers et al. (64,65) carried out a coping skills intervention at school that used motivational interviewing strategies and cognitive behavioral skills training and aimed to improve symptoms by targeting personality-based risk factors for alcohol misuse in adolescents. The intervention provided pupils with personalized feedback on their results from a personality assessment. Although no treatment effect was found on alcohol use in the whole sample (64), this intervention could reduce alcohol use in adolescents with higher anxiety sensitivity and reduce binge drinking and its frequency in those with higher sensation seeking (65).
Lindenberg et al. (66) created the PROTECT intervention to reduce symptom severity and prevent the full syndrome and sub-threshold onset of gaming disorder and unspecified Internet use disorder in at-risk adolescents. PROTECT was based on CBT and targets changes in addictive reward processing and pathological cognitive mechanisms. Results showed a significant symptom reduction over 12 months in both the PROTECT and control groups, but the intervention was superior in reducing symptom severity compared with the control group.
Chaplin et al. (67) compared the efficacy of two parent-based interventions: the Parenting Mindfully (PM) intervention and brief parental education (PE) on substance use. PM focused on encouraging mindfulness in daily life and parenting, whereas PE educated parents on adolescent development and risk behaviors. Compared with PE, PM prevented increments of substance use in adolescents over time.
Insomnia
Clinical
De Bruin et al. (68) conducted a study to explore the efficacy of CBTI on adolescents diagnosed with insomnia and found that psychopathology symptoms, insomnia, and sleep problems decreased significantly in both the Internet and face-to-face CBTI groups compared with the waitlist group at 2-month follow-up, with effects lasting for at least 12 months.
Subclinical
Dong et al. (69) created a program called Trans-diagnostic Sleep and Circadian Intervention to improve psychosocial, behavioral, and cognitive processes that maintain sleep and circadian problems. Results showed treatment effects on evening circadian preference and sleep quality, but not on the overall health risk.
Borderline personality disorder
Clinical
Jørgensen et al. (70) explored the long-term effectiveness of mentalization-based treatment in 111 adolescents with borderline personality disorder or borderline personality disorder features. The treatment included introductory sessions, individual case formulation sessions, group sessions, and parent sessions. This program aimed to increase patients’ capacity for “making sense of each other and ourselves, implicitly and explicitly in terms of subjective states and mental processes.” The results showed that adolescents in the treatment group were not superior to those in the control group, with both groups showing improvement in clinical and social outcomes.
Schuppert et al. (23) evaluated the effectiveness of Emotion Regulation Training among 109 adolescents. The training focused on improving feelings of control over intense, strong emotions by enhancing cognitive, social, and behavioral coping skills. Both intervention and control groups showed improvements, with no significant difference between the two.
Psychosis
Clinical
She et al. (71) explored the efficacy of structural group therapy in treating inpatients diagnosed with schizophrenia. The structural group therapy included 12 one-hour sessions with different themes and types of activities based on recommendations from an expert panel. These activities aimed to increase adolescents’ self-awareness, positive self-cognition, and self-acceptance. The results showed that structural group therapy could help improve the self-consistency and reduce positive symptoms and general psychopathology in adolescents with schizophrenia.
Subclinical
Poulton et al. (72) created a family-based intervention called Multidimensional Treatment Foster Care aimed at psychotic symptom trajectories in 166 adolescent girls with delinquent behaviors. The girls were placed in homes with foster parents trained to implement a behavioral reinforcement program, with a series of individual therapy sessions. The sessions emphasized assisting the girls in identifying particular stressors, monitoring symptom occurrence, normalizing symptom presence, and role-playing coping mechanisms. Results showed that the girls in the intervention group had a significantly steeper decline in psychotic symptoms compared with the usual-services group.
Adolescent mental health
Subclinical
In addition to specific psychological disorders, several studies have been conducted on the prevention of general mental health problems. The most commonly investigated sample is adolescents with depression and anxiety, due to their high comorbidity in adolescence. Mindsets are core beliefs on the malleability of people’s traits. By providing an interpretative lens, they help shape judgments and reactions to life events and others’ behavior. Mindset interventions focus on teaching the belief that personal traits are malleable. Schleider et al. (73,74) used a mindset intervention for adolescents at risk for depression and anxiety. Results showed that the intervention reduced internalizing distress and strengthened participants’ perceived control. Osborn et al. (75) recently used the “Shamiri” group intervention in adolescents with depression and anxiety. Shamiri includes exercises on growth mindset, gratitude, and value affirmation, and has been shown to reduce depression and anxiety and improve academic performance in adolescents. Johnson et al. (76) tested the efficacy of a school-based mindfulness program in improving depression and anxiety symptoms; however, the program showed no treatment effect.
The efficacy of mindfulness interventions in various aspects of mental health has been widely examined (77-79). Bluth et al. (77) found that mindfulness interventions can improve adolescent mindfulness, self-compassion, perceived stress, and life satisfaction. Bluth et al. (78) found that a mindful self-compassion program has the potential to decrease stress and increase resilience and positive risk-taking in adolescents. Bei et al. (79) combined mindfulness therapy and CBT to improve sleep quality and found significant improvements.
Bierman et al. (80) tested the effectiveness of a school-based enrichment program on reducing psychopathological symptoms in adolescents from low-income families. The program aimed to promote students’ social skills, emotional understanding, self-regulation, and social problem-solving. The results showed that the program significantly reduced conduct problems and emotional symptoms. Shoshani et al. (81) evaluated a school-based intervention based on positive psychology, which included teacher training workshops and teachers’ administration of a parallel program to students. The results showed that adolescents in the intervention group reported significant reductions in general distress, anxiety, and depression symptoms. Manicavasagar et al. (82) examined the efficacy of another positive psychology program, Bite Back, among 235 adolescents. Bite Back is a website for adolescents that uses a combination of interactive exercises and positive psychology information. The program was effective in reducing depression and stress and improving well-being, especially in adolescents with continuous adherence to the program.
Conclusions
This narrative review of intervention studies from the last ten years provides a complete perspective on the efficacy of psychological treatments for adolescent psychopathology. This review can be utilized to make appropriate recommendations for healthcare spending and services, as well as to improve treatment outcomes.
Clinical implications
CBT and programs that are based on it were the most widely-studied therapies for treating adolescent psychopathology. Clinicians should be aware of the growing evidence demonstrating that CBT is effective for treating anxiety (36), depression (39,40), eating disorders (51,52), ADHD (56), substance use (63-66), insomnia (68) and other psychological problems (79). Additionally, researchers have developed programs that combine the intervention approach of CBT with other approaches, such as social problem-solving and coping skills (38) and other therapies, such as mindfulness-based therapy (79), for specific disorders. Researchers also attempted to computerize CBT interventions to make them more convenient for patients (35,36,68), and results suggest that the computerized interventions have treatment effects equal to those of face-to-face CBT (68).
The current findings suggest that families and schools could be good contexts for conducting psychological treatment for adolescent psychopathology. FBT was found to be effective in treating eating disorders (42-50), ADHD (58), conduct problems (59), antisocial behaviors (61), autism spectrum disorder (62), substance use (63,67), and psychosis (72). This might be because family and how parents treat their children are the most influential elements in adolescent daily life (83). Moreover, multifamily therapy was found to be more effective than single-family therapy for anorexia nervosa (50), as parents can benefit from therapists and learn from specific details shared by other parents. School-based programs have also been conducted for the prevention and treatment of many disorders including ADHD (57), substance use (64,65), and general mental health (76,80,81) in adolescents, most of whom present good improvement of symptoms (57,64,65,80,81). One possible reason for this is that providing psychological knowledge and skills through teachers in the school setting allows adolescents to relieve their psychological symptoms through creating a supportive environment (84).
Limitations and future directions
Although the literature in the last decade is encouraging, limitations and future directions need to be highlighted. In terms of sample and methodology, many studies have small sample sizes and restricted ages and focus on only one gender. The samples from certain studies are also quite variable in the severity of psychological symptoms, and severity has been shown to modulate intervention effects (46,57). Further, different measurements were used for the same kind of psychopathology. The sample and measurement variations reduce comparability among study conclusions. Moreover, some of the existing intervention studies lack rigor, such as failing to implement pre- and post-intervention fitness assessments or including a control group. Alternatively, the design of the control condition may contain therapeutic factors similar to the intervention condition, or none of them may contain therapeutic factors. It is also possible that some participants may have characteristics that maintain symptoms that weaken or intensify the treatment effect, such as comorbidities, severe symptoms, and certain personalities. A lack of strict experimental controls may lead to spurious valid or invalid conclusions. As such, further studies with a clear description of methods and restricted intervention design are required to address these gaps.
In terms of psychopathology, certain mental health concerns, such as self-harm, post-traumatic stress disorder, and learning difficulties, are not well-characterized. They are shown as prominent psychopathologic disorders in adolescence (85,86); thus, it is of great importance for future research to examine those conditions. Moreover, borderline personality disorder shows poor treatment efficacy with psychological interventions in our review (23,71), which is probably because a low dosage and intensity of treatment may be insufficient to deal with severe mental disorders. Borderline personality disorder is considered a relatively severe mental disorder associated with high suicide rates, serious functional impairments, and extensive comorbid mental disorders (87). Although these studies focus on adolescence, which is considered the early period for mental disorders to arise, symptoms in this period may have already become persistent and severe; thus, a relatively short intervention cannot work. Finally, these interventions may be too heterogeneous or fragmented to contribute to specific topics in adolescent mental health (23). Thus, new programs with a longer duration, higher intensity, and clearer targets are needed to treat borderline personality disorder.
Regarding therapy, the effectiveness of psychoanalytic treatment on externalizing problems and depression has been proven in previous studies (88,89). However, the age range in these studies is very large, spanning childhood and adolescence; thus, the corresponding results were not included in this review. Future research should narrow the view only to adolescents to investigate the efficacy of psychoanalytic therapy on psychopathology. In addition, only two studies in this review focused on treatments for those who did not respond to the first-line treatment (38,44). More programs prioritizing these patients need to be implemented. Future research should also examine the influential or intermediate factors in treatments, as they could clarify which elements are effective for improvement.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: This study was supported by the National Natural Science Foundation of China (No. 32130045) and the Scientific Foundation of Institute of Psychology, Chinese Academy of Sciences (No. E2CX3815CX).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Footnotes
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-22-589/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-589/coif). XL serves as an unpaid editorial board member of Translational Pediatrics from March 2022 to February 2024. The other authors have no conflicts of interest to declare.
References
- 1.Steinberg L. Adolescence, 12th ed. New York: McGraw-Hill; 2018. [Google Scholar]
- 2.Patafio B, Miller P, Baldwin R, et al. A systematic mapping review of interventions to improve adolescent mental health literacy, attitudes and behaviours. Early Interv Psychiatry 2021;15:1470-501. 10.1111/eip.13109 [DOI] [PubMed] [Google Scholar]
- 3.Knapp M, Wong G. Economics and mental health: the current scenario. World Psychiatry 2020;19:3-14. 10.1002/wps.20692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bloom DE, Cafiero ET, Jané-Llopis E et al. The global economic burden of noncommunicable diseases. Geneva: World Economic Forum, 2011. [Google Scholar]
- 5.Kok JK, Low SK. Risk factors contributing to vulnerability of mental health disorders and the protective factors among Malaysian youth. Int J Sch Educ Psychol 2019;7:102-12. 10.1080/21683603.2018.1499573 [DOI] [Google Scholar]
- 6.Kaplan SJ, Pelcovitz D, Salzinger S, et al. Adolescent physical abuse: risk for adolescent psychiatric disorders. Am J Psychiatry 1998;155:954-9. 10.1176/ajp.155.7.954 [DOI] [PubMed] [Google Scholar]
- 7.Vostanis P, Graves A, Meltzer H, et al. Relationship between parental psychopathology, parenting strategies and child mental health. Soc Psychiatry Psychiatr Epidemiol 2006;41:509–514. 10.1007/s00127-006-0061-3 [DOI] [PubMed] [Google Scholar]
- 8.Vicente B, Saldivia S, de la Barra F, et al. Prevalence of child and adolescent mental disorders in Chile: a community epidemiological study. J Child Psychol Psychiatry 2012;53:1026-35. 10.1111/j.1469-7610.2012.02566.x [DOI] [PubMed] [Google Scholar]
- 9.Kaltiala-Heino R, Rimpelä M, Rantanen P, et al. Bullying at school—an indicator of adolescents at risk for mental disorders. J Adolesc 2000;23:661-74. 10.1006/jado.2000.0351 [DOI] [PubMed] [Google Scholar]
- 10.Li J, Li J, Jia R, et al. Mental health problems and associated school interpersonal relationships among adolescents in China: a cross-sectional study. Child Adolesc Psychiatry Ment Health 2020;14:12. 10.1186/s13034-020-00318-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen R, Peng K, Liu J, et al. Interpersonal Trauma and Risk of Depression Among Adolescents: The Mediating and Moderating Effect of Interpersonal Relationship and Physical Exercise. Front Psychiatry 2020;11:194. 10.3389/fpsyt.2020.00194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guillon MS, Crocq MA, Bailey PE. The relationship between self-esteem and psychiatric disorders in adolescents. Eur Psychiatry 2003;18:59-62. 10.1016/S0924-9338(03)00002-6 [DOI] [PubMed] [Google Scholar]
- 13.Nguyen DT, Wright EP, Dedding C, et al. Low Self-Esteem and Its Association With Anxiety, Depression, and Suicidal Ideation in Vietnamese Secondary School Students: A Cross-Sectional Study. Front Psychiatry 2019;10:698. 10.3389/fpsyt.2019.00698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Orth U, Robins RW. Understanding the link between low self-esteem and depression. Curr Dir Psychol Sci 2013;22:455-60. 10.1177/0963721413492763 [DOI] [Google Scholar]
- 15.Mantilla EF, Birgegård A. The enemy within: the association between self-image and eating disorder symptoms in healthy, non help-seeking and clinical young women. J Eat Disord 2015;3:30. 10.1186/s40337-015-0067-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tran AWY, Lumley MN. Internalized stigma and student well-being: the role of adaptive and maladaptive coping. Soc Work Ment Health 2019;17:408-25 10.1080/15332985.2018.1563023 [DOI] [Google Scholar]
- 17.Choi KW, Sikkema KJ, Velloza J, et al. Maladaptive coping mediates the influence of childhood trauma on depression and PTSD among pregnant women in South Africa. Arch Womens Ment Health 2015;18:731-8. 10.1007/s00737-015-0501-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Z, Zhang J. Coping skills, mental disorders, and suicide among rural youths in China. J Nerv Ment Dis 2012;200:885-90. 10.1097/NMD.0b013e31826b6ecc [DOI] [PubMed] [Google Scholar]
- 19.Yook K, Kim KH, Suh SY, et al. Intolerance of uncertainty, worry, and rumination in major depressive disorder and generalized anxiety disorder. J Anxiety Disord 2010;24:623-8. 10.1016/j.janxdis.2010.04.003 [DOI] [PubMed] [Google Scholar]
- 20.Lau JY, Waters AM. Annual Research Review: An expanded account of information-processing mechanisms in risk for child and adolescent anxiety and depression. J Child Psychol Psychiatry 2017;58:387-407. 10.1111/jcpp.12653 [DOI] [PubMed] [Google Scholar]
- 21.Berking M, Wupperman P. Emotion regulation and mental health: recent findings, current challenges, and future directions. Curr Opin Psychiatry 2012;25:128-34. 10.1097/YCO.0b013e3283503669 [DOI] [PubMed] [Google Scholar]
- 22.Scholten H, Malmberg M, Lobel A, et al. A Randomized Controlled Trial to Test the Effectiveness of an Immersive 3D Video Game for Anxiety Prevention among Adolescents. PLoS One 2016;11:e0147763. 10.1371/journal.pone.0147763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schuppert HM, Timmerman ME, Bloo J, et al. Emotion regulation training for adolescents with borderline personality disorder traits: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2012;51:1314-1323.e2. 10.1016/j.jaac.2012.09.002 [DOI] [PubMed] [Google Scholar]
- 24.Singh N, Reece J. Psychotherapy, pharmacotherapy, and their combination for adolescents with major depressive disorder: A meta-analysis. Educ Dev Psychol 2014;31:47-65. 10.1017/edp.2013.20 [DOI] [Google Scholar]
- 25.Pampallona S, Bollini P, Tibaldi G, et al. Combined pharmacotherapy and psychological treatment for depression: a systematic review. Arch Gen Psychiatry 2004;61:714-9. 10.1001/archpsyc.61.7.714 [DOI] [PubMed] [Google Scholar]
- 26.Patel V, Flisher AJ, Hetrick S, et al. Mental health of young people: a global public-health challenge. Lancet 2007;369:1302-13. 10.1016/S0140-6736(07)60368-7 [DOI] [PubMed] [Google Scholar]
- 27.Nebhinani N, Jain S. Adolescent mental health: Issues, challenges, and solutions. Ann Indian Psychiatry 2019;3:4-7. 10.4103/aip.aip_24_19 [DOI] [Google Scholar]
- 28.Gamm L, Stone S, Pittman S. Mental health and mental disorders—A rural challenge: A literature review. Rural Healthy People 2010: A companion document to Healthy People 2010. College Station, TX: The Texas A&M University System Healthy Science Center, School of Rural Public Health, Southwest Rural Health Research Center; 2010;2:97-114. [Google Scholar]
- 29.Fonagy P, Kächele H. Psychoanalysis and other long-term dynamic psychotherapies. In: Gelder M, Andreasen N, Lopez-Ibor J, et al. editors. New Oxford Textbook of Psychiatry, 2nd edition. Oxford: Oxford University Press; 2012;1338-50. [Google Scholar]
- 30.Taylor D. Psychoanalytic and psychodynamic therapies for depression: The evidence base. Advance Psychiatr Treat 2008;14:401-13. 10.1192/apt.bp.107.004382 [DOI] [Google Scholar]
- 31.Hoffman L. Foundations of family therapy. New York: Basic Books; 1981. [Google Scholar]
- 32.Nichols MP, Schwartz RC. Family therapy: Concepts and methods. 4th ed. Needham Heights, MA: Allyn & Bacon; 1998. [Google Scholar]
- 33.Ozechowski TJ, Liddle HA. Family-based therapy for adolescent drug abuse: knowns and unknowns. Clin Child Fam Psychol Rev 2000;3:269-98. 10.1023/A:1026429205294 [DOI] [PubMed] [Google Scholar]
- 34.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Capron DW, Schmidt NB. Development and randomized trial evaluation of a novel computer-delivered anxiety sensitivity intervention. Behav Res Ther 2016;81:47-55. 10.1016/j.brat.2016.04.001 [DOI] [PubMed] [Google Scholar]
- 36.de Hullu E, Sportel BE, Nauta MH, et al. Cognitive bias modification and CBT as early interventions for adolescent social and test anxiety: Two-year follow-up of a randomized controlled trial. J Behav Ther Exp Psychiatry 2017;55:81-9. 10.1016/j.jbtep.2016.11.011 [DOI] [PubMed] [Google Scholar]
- 37.Knapp AA, Feldner M, Allan NP, et al. Test of an Anxiety Sensitivity Amelioration Program for at-risk youth (ASAP-Y). Behav Res Ther 2020;126:103544. 10.1016/j.brat.2019.103544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bechor M, Pettit JW, Silverman WK, et al. Attention Bias Modification Treatment for children with anxiety disorders who do not respond to cognitive behavioral therapy: a case series. J Anxiety Disord 2014;28:154-9. 10.1016/j.janxdis.2013.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pössel P, Martin NC, Garber J, et al. A randomized controlled trial of a cognitive-behavioral program for the prevention of depression in adolescents compared with nonspecific and no-intervention control conditions. J Couns Psychol 2013;60:432-8. 10.1037/a0032308 [DOI] [PubMed] [Google Scholar]
- 40.Kindt KC, Kleinjan M, Janssens JM, et al. Evaluation of a school-based depression prevention program among adolescents from low-income areas: a randomized controlled effectiveness trial. Int J Environ Res Public Health 2014;11:5273-93. 10.3390/ijerph110505273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gest S, Holtmann M, Bogen S, et al. Chronotherapeutic treatments for depression in youth. Eur Child Adolesc Psychiatry 2016;25:151-61. 10.1007/s00787-015-0720-6 [DOI] [PubMed] [Google Scholar]
- 42.Trainor C, Gorrell S, Hughes EK, et al. Family-based treatment for adolescent anorexia nervosa: What happens to rates of comorbid diagnoses? Eur Eat Disord Rev 2020;28:351-7. 10.1002/erv.2725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lock J, Agras WS, Bryson SW, et al. Does family-based treatment reduce the need for hospitalization in adolescent anorexia nervosa? Int J Eat Disord 2016;49:891-4. 10.1002/eat.22536 [DOI] [PubMed] [Google Scholar]
- 44.Lock J, Le Grange D, Agras WS, et al. Can adaptive treatment improve outcomes in family-based therapy for adolescents with anorexia nervosa? Feasibility and treatment effects of a multi-site treatment study. Behav Res Ther 2015;73:90-5. 10.1016/j.brat.2015.07.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Herscovici CR, Kovalskys I, Orellana L. An Exploratory Evaluation of the Family Meal Intervention for Adolescent Anorexia Nervosa. Fam Process 2017;56:364-75. 10.1111/famp.12199 [DOI] [PubMed] [Google Scholar]
- 46.Accurso EC, Ciao AC, Fitzsimmons-Craft EE, et al. Is weight gain really a catalyst for broader recovery?: The impact of weight gain on psychological symptoms in the treatment of adolescent anorexia nervosa. Behav Res Ther 2014;56:1-6. 10.1016/j.brat.2014.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Le Grange D, Lock J, Agras WS, et al. Moderators and mediators of remission in family-based treatment and adolescent focused therapy for anorexia nervosa. Behav Res Ther 2012;50:85-92. 10.1016/j.brat.2011.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rienecke RD, Accurso EC, Lock J, et al. Expressed Emotion, Family Functioning, and Treatment Outcome for Adolescents with Anorexia Nervosa. Eur Eat Disord Rev 2016;24:43-51. 10.1002/erv.2389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ciao AC, Accurso EC, Fitzsimmons-Craft EE, et al. Family functioning in two treatments for adolescent anorexia nervosa. Int J Eat Disord 2015;48:81-90. 10.1002/eat.22314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Eisler I, Simic M, Hodsoll J, et al. A pragmatic randomised multi-centre trial of multifamily and single family therapy for adolescent anorexia nervosa. BMC Psychiatry 2016;16:422. 10.1186/s12888-016-1129-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Philipp J, Franta C, Zeiler M, et al. Does a Skills Intervention for Parents Have a Positive Impact on Adolescents' Anorexia Nervosa Outcome? Answers from a Quasi-Randomised Feasibility Trial of SUCCEAT. Int J Environ Res Public Health 2021;18:4656. 10.3390/ijerph18094656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Biney H, Giles E, Hutt M, et al. Self-esteem as a catalyst for change in adolescent inpatients with anorexia nervosa: a pilot randomised controlled trial. Eat Weight Disord 2022;27:189-98. 10.1007/s40519-021-01161-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Herbrich L, van Noort B, Pfeiffer E, et al. Follow-up Assessment of Cognitive Remediation Therapy in Adolescent Anorexia Nervosa: A Pilot Study. Eur Eat Disord Rev 2017;25:104-13. 10.1002/erv.2501 [DOI] [PubMed] [Google Scholar]
- 54.Glashouwer KA, Neimeijer RAM, de Koning ML, et al. Evaluative conditioning as a body image intervention for adolescents with eating disorders. J Consult Clin Psychol 2018;86:1046-55. 10.1037/ccp0000311 [DOI] [PubMed] [Google Scholar]
- 55.Giel KE, Zipfel S, Schweizer R, et al. Eating disorder pathology in adolescents participating in a lifestyle intervention for obesity: associations with weight change, general psychopathology and health-related quality of life. Obes Facts 2013;6:307-16. 10.1159/000354534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Boyer B, MacKay KJ, McLeod BD, et al. Comparing Alliance in Two Cognitive-Behavioural Therapies for Adolescents With ADHD Using a Randomized Controlled Trial. Behav Ther 2018;49:781-95. 10.1016/j.beth.2018.01.003 [DOI] [PubMed] [Google Scholar]
- 57.Langberg JM, Dvorsky MR, Molitor SJ, et al. Overcoming the research-to-practice gap: A randomized trial with two brief homework and organization interventions for students with ADHD as implemented by school mental health providers. J Consult Clin Psychol 2018;86:39-55. 10.1037/ccp0000265 [DOI] [PubMed] [Google Scholar]
- 58.Sibley MH, Rodriguez L, Coxe S, et al. Parent-Teen Group versus Dyadic Treatment for Adolescent ADHD: What Works for Whom? J Clin Child Adolesc Psychol 2020;49:476-92. 10.1080/15374416.2019.1585257 [DOI] [PubMed] [Google Scholar]
- 59.Weiss B, Han S, Harris V, et al. An independent randomized clinical trial of multisystemic therapy with non-court-referred adolescents with serious conduct problems. J Consult Clin Psychol 2013;81:1027-39. 10.1037/a0033928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Caldwell MF, McCormick D, Wolfe J, et al. Treatment-related changes in psychopathy features and behavior in adolescent offenders. Crim Justice Behav 2012;39:144-55. 10.1177/0093854811429542 [DOI] [Google Scholar]
- 61.Van Ryzin MJ, Dishion TJ. The impact of a family-centered intervention on the ecology of adolescent antisocial behavior: modeling developmental sequelae and trajectories during adolescence. Dev Psychopathol 2012;24:1139-55. 10.1017/S0954579412000582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Idris S, van Pelt BJ, Jagersma G, et al. A randomized controlled trial to examine the effectiveness of the Dutch version of the Program for the Education and Enrichment of Relational Skills (PEERS®). BMC Psychiatry 2022;22:293. 10.1186/s12888-022-03913-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hendriks V, van der Schee E, Blanken P. Matching adolescents with a cannabis use disorder to multidimensional family therapy or cognitive behavioral therapy: treatment effect moderators in a randomized controlled trial. Drug Alcohol Depend 2012;125:119-26. 10.1016/j.drugalcdep.2012.03.023 [DOI] [PubMed] [Google Scholar]
- 64.Lammers J, Goossens F, Conrod P, et al. Effectiveness of a selective intervention program targeting personality risk factors for alcohol misuse among young adolescents: results of a cluster randomized controlled trial. Addiction 2015;110:1101-9. 10.1111/add.12952 [DOI] [PubMed] [Google Scholar]
- 65.Lammers J, Goossens F, Conrod P, et al. Effectiveness of a selective alcohol prevention program targeting personality risk factors: Results of interaction analyses. Addict Behav 2017;71:82-8. 10.1016/j.addbeh.2017.02.030 [DOI] [PubMed] [Google Scholar]
- 66.Lindenberg K, Kindt S, Szász-Janocha C. Effectiveness of Cognitive Behavioral Therapy-Based Intervention in Preventing Gaming Disorder and Unspecified Internet Use Disorder in Adolescents: A Cluster Randomized Clinical Trial. JAMA Netw Open 2022;5:e2148995. 10.1001/jamanetworkopen.2021.48995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chaplin TM, Mauro KL, Curby TW, et al. Effects of A Parenting-Focused Mindfulness Intervention on Adolescent Substance Use and Psychopathology: A Randomized Controlled Trial. Res Child Adolesc Psychopathol 2021;49:861-75. 10.1007/s10802-021-00782-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.de Bruin EJ, Bögels SM, Oort FJ, et al. Improvements of adolescent psychopathology after insomnia treatment: results from a randomized controlled trial over 1 year. J Child Psychol Psychiatry 2018;59:509-22. 10.1111/jcpp.12834 [DOI] [PubMed] [Google Scholar]
- 69.Dong L, Dolsen MR, Martinez AJ, et al. A transdiagnostic sleep and circadian intervention for adolescents: six-month follow-up of a randomized controlled trial. J Child Psychol Psychiatry 2020;61:653-61. 10.1111/jcpp.13154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Jørgensen MS, Storebø OJ, Bo S, et al. Mentalization-based treatment in groups for adolescents with Borderline Personality Disorder: 3- and 12-month follow-up of a randomized controlled trial. Eur Child Adolesc Psychiatry 2021;30:699-710. 10.1007/s00787-020-01551-2 [DOI] [PubMed] [Google Scholar]
- 71.She P, Zeng H, Yang B. Effect of self-consistency group intervention for adolescents with schizophrenia: An inpatient randomized controlled trial. J Psychiatr Res 2016;73:63-70. 10.1016/j.jpsychires.2015.11.006 [DOI] [PubMed] [Google Scholar]
- 72.Poulton R, Van Ryzin MJ, Harold GT, et al. Effects of multidimensional treatment foster care on psychotic symptoms in girls. J Am Acad Child Adolesc Psychiatry 2014;53:1279-87. 10.1016/j.jaac.2014.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schleider JL, Weisz JR. Reducing risk for anxiety and depression in adolescents: Effects of a single-session intervention teaching that personality can change. Behav Res Ther 2016;87:170-81. 10.1016/j.brat.2016.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schleider J, Weisz J. A single-session growth mindset intervention for adolescent anxiety and depression: 9-month outcomes of a randomized trial. J Child Psychol Psychiatry 2018;59:160-70. 10.1111/jcpp.12811 [DOI] [PubMed] [Google Scholar]
- 75.Osborn TL, Wasil AR, Venturo-Conerly KE, et al. Group Intervention for Adolescent Anxiety and Depression: Outcomes of a Randomized Trial with Adolescents in Kenya. Behav Ther 2020;51:601-15. 10.1016/j.beth.2019.09.005 [DOI] [PubMed] [Google Scholar]
- 76.Johnson C, Burke C, Brinkman S, et al. Effectiveness of a school-based mindfulness program for transdiagnostic prevention in young adolescents. Behav Res Ther 2016;81:1-11. 10.1016/j.brat.2016.03.002 [DOI] [PubMed] [Google Scholar]
- 77.Bluth K, Roberson PN, Gaylord SA. A Pilot Study of a Mindfulness Intervention for Adolescents and the Potential Role of Self-Compassion in Reducing Stress. Explore (NY) 2015;11:292-5. 10.1016/j.explore.2015.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bluth K, Eisenlohr-Moul TA. Response to a mindful self-compassion intervention in teens: A within-person association of mindfulness, self-compassion, and emotional well-being outcomes. J Adolesc 2017;57:108-18. 10.1016/j.adolescence.2017.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bei B, Byrne ML, Ivens C, et al. Pilot study of a mindfulness-based, multi-component, in-school group sleep intervention in adolescent girls. Early Interv Psychiatry 2013;7:213-20. 10.1111/j.1751-7893.2012.00382.x [DOI] [PubMed] [Google Scholar]
- 80.Bierman KL, Heinrichs BS, Welsh JA, et al. Reducing Adolescent Psychopathology in Socioeconomically Disadvantaged Children With a Preschool Intervention: A Randomized Controlled Trial. Am J Psychiatry 2021;178:305-12. 10.1176/appi.ajp.2020.20030343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shoshani A, Steinmetz S. Positive psychology at school: A school-based intervention to promote adolescents’ mental health and well-being. J Happiness Stud 2014;15:1289-311. 10.1007/s10902-013-9476-1 [DOI] [Google Scholar]
- 82.Manicavasagar V, Horswood D, Burckhardt R, et al. Feasibility and effectiveness of a web-based positive psychology program for youth mental health: randomized controlled trial. J Med Internet Res 2014;16:e140. 10.2196/jmir.3176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kaslow NJ, Broth MR, Smith CO, et al. Family-based interventions for child and adolescent disorders. J Marital Fam Ther 2012;38:82-100. 10.1111/j.1752-0606.2011.00257.x [DOI] [PubMed] [Google Scholar]
- 84.Evans SW, Langberg JM, Schultz BK, et al. Evaluation of a school-based treatment program for young adolescents with ADHD. J Consult Clin Psychol 2016;84:15-30. 10.1037/ccp0000057 [DOI] [PubMed] [Google Scholar]
- 85.Becker SP, Breaux R, Cusick CN, et al. Remote Learning During COVID-19: Examining School Practices, Service Continuation, and Difficulties for Adolescents With and Without Attention-Deficit/Hyperactivity Disorder. J Adolesc Health 2020;67:769-77. 10.1016/j.jadohealth.2020.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hawton K, Saunders KE, O'Connor RC. Self-harm and suicide in adolescents. Lancet 2012;379:2373-82. 10.1016/S0140-6736(12)60322-5 [DOI] [PubMed] [Google Scholar]
- 87.Leichsenring F, Leibing E, Kruse J, et al. Borderline personality disorder. Lancet 2011;377:74-84. 10.1016/S0140-6736(10)61422-5 [DOI] [PubMed] [Google Scholar]
- 88.Weitkamp K, Daniels JK, Hofmann H, et al. Psychoanalytic psychotherapy for children and adolescents with severe depressive psychopathology: preliminary results of an effectiveness trial. Psychotherapy (Chic) 2014;51:138-47. 10.1037/a0034178 [DOI] [PubMed] [Google Scholar]
- 89.Weitkamp K, Daniels JK, Romer G, et al. Psychoanalytic Psychotherapy for Children and Adolescents with Severe Externalising Psychopathology: An Effectiveness Trial. Z Psychosom Med Psychother 2017;63:251-66. 10.13109/zptm.2017.63.3.251 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as


