Abstract
The unrelenting rise in healthcare costs over the past 50 years has caused policymakers to respond. Their reactions have led to a gradual economic transformation of medicine. As a result, detailed billing, quality controls, financial incentives, savings targets and digitalisation are now putting increasing pressures on the nursing and medical staff. In addition, the humanity of care of the patient–doctor and/or patient–nurse interactions has been cast aside to a great extent. Therefore, the immaterial side of care has been neglected or even removed from these relationships. These changes are now perceived as intolerable by most health workers and patients. Yet healthcare costs are still rising. This paper presents a hypothesis that should enable healthcare systems to respond more effectively. It proposes the introduction of the Meikirch model, a new comprehensive definition of health. The Meikirch model takes human nature fully into account, including health and disease. The inclusion of the individual potentials, the social surroundings and the natural environment leads to the concept of health as a complex adaptive system (CAS). Care for such a definition of health requires medical organisations to change from top–down management to bottom–up leadership. Such innovations are now mature and ready for implementation. They require a long-term investment, a comprehensive approach to patient care and new qualifications for leadership. The Meikirch model reads: ‘To be healthy a human individual must be able to satisfy the demands of life. For this purpose, each person disposes of a biologically given and a personally acquired potential, both of which are closely related to the social surroundings and the natural environment. The resulting CAS enables the individual to unfold a personal identity and to develop it further until death. Healthcare has the purpose to empower each individual to fully realize optimal health’. This hypothesis postulates that the new definition of health will further develop healthcare systems in such a way that better health results at lower costs.
Keywords: healthcare quality improvement, leadership, management, organisational culture, teamwork
Key messages.
What is already known about this subject?
The best-known definition of health is available in the preamble of the constitution of the WHO. It is, however, generally rejected, because of its unrealistic content. Later efforts to define health have clarified only parts.
What does this study add?
The Meikirch-model, described in this review, is a new, complete, and functionally discerning definition of health. Its approach to healthcare offers interesting new features for prevention, diagnosis, and treatment of diseases.
How might this impact on clinical practice or future developments?
Application of this model in health care may lead to more whole person approaches and better health than current practices. Presumably, it will also reduce healthcare costs.
Introduction
A famous quote from Albert Einstein reads: ‘We cannot solve our problems with the same thinking we used when we created them’. Unfortunately, this is exactly what is still being tried again and again in today’s healthcare systems. Not surprisingly, the crises only get worse. Costs, expressed as a fraction of the gross domestic product, are constantly increasing and becoming more and more difficult to finance. Billing demands a great deal of bureaucracy, and doctors and nurses must spend an ever-increasing part of their working hours with the computer instead of with patients. As a result, time available for consultation with patients is reduced accordingly. Digitalisation is also on the increase and, somehow, the administrative requirements no longer match the conditions for a fulfilling and high-quality professional practice. In Switzerland, one in seven young doctors or nurses are leaving their professions. Whenever managers believe they recognise opportunities for cost savings, they respond with more detailed orders that, in the end, do not work. Einstein's quote simply is not seriously considered. In contrast, I would like to introduce a new paradigm, the Meikirch model.1–3 This new definition of health offers an opportunity to rethink and redesign healthcare systems. Implementation, obviously, will require a substantial investment.
For centuries, everyone has been able to say whether or not she or he is healthy or diseased. Yet, there has been no established criteria. Everyone just knew by themselves when they are ill. This type of knowledge, however, is not suitable for shaping a social organisation such as a healthcare system. Yet, so far, there has been no better method available. Doctors determine how diseased people should be cared for, and health systems work with simple methods. It has been only the uncontrolled rise in healthcare costs that has attracted the attention of politicians. These have commissioned economists to solve the problems. Professors Michael E Porter and Olmsted Teisberg are outstanding representatives.4 5 In two remarkable publications, they describe how the work in a hospital is to be billed and how competitive thinking may be introduced into healthcare. Since then, more and more economic principles have been introduced. The present difficulties have become possible, because the question of what health and disease truly are has no clear answer and, consequently, the healthcare system has no clear objectives. It is therefore not appropriate to accuse anyone for today's problems.
The purpose of this review was to create an overall hypothesis of what theoretically may be achieved if the hypothesis of a new definition of health is applied to all aspects of healthcare systems.
Previous attempts to define health
The best-known definition of health originates from the preamble of the WHO, founded in 1948.6 It postulates ‘a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity’. Yet today, this is considered to be excessive, and this definition is therefore generally rejected. In 1987, the Swedish health philosopher Lennart Nordenfelt dared to try again: ‘A is completely healthy, if and only if A is in a bodily and mental state which is such that A is able to realise all his or her vital goals, given accepted circumstances’.7 8 Bircher summarised health in 2005 as a precursor of the present Meikirch model: ‘Health is a dynamic state of wellbeing characterised by a physical, mental and social potential, which satisfies the demands of a life commensurate with age, culture, and personal responsibility’.9 After an interdisciplinary meeting in the Netherlands, Machteld Huber et al summed up in 2011: ‘Health is the ability to adapt and to lead oneself in the presence of social, physical and emotional challenges’.10 In 2014, Bircher and Kuruvilla published the final Meikirch model which postulates that ‘health is a state of wellbeing emergent from conducive interactions between individuals’ potentials, life’s demands, and social and environmental determinants’.2 In 2019, Piet van Spijk expressed health as follows: ‘The absence of illness means small health. The feeling of living a meaningful life plays an important role in determining a great human health’.11 These various authors listed essential aspects of a definition of health. To date, the Meikirch model more or less includes them all.
Meikirch model
The distinction between health and disease is inherently blurred. Every healthy person, however, must be able to meet the demands that life—as a natural and personal process—places on him or her. These include the preservation of the physical body, the work on the development of the personality, social integration, as well as the relationship to the environment. If a person can meet these requirements, he or she is healthy. If these requirements cannot be fully met, there is illness. A small carcinoma somewhere in the body is ‘pathological’ and endangers a person's long-term future. However, the actual finding itself does not make him or her diseased. Most people with head or back pain say they are healthy. This means that absence of pathology or of complaints is no precondition for health.1 3
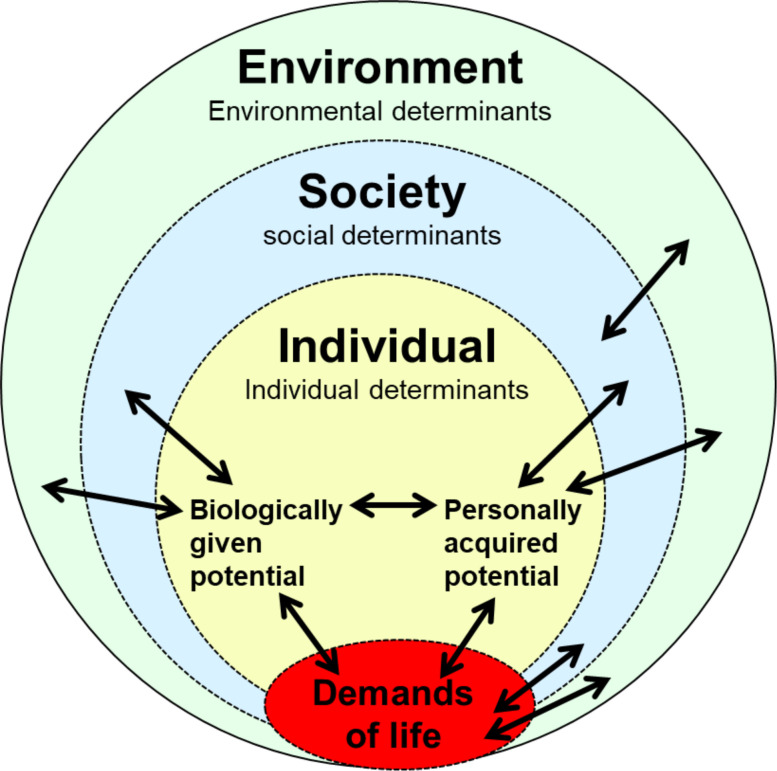
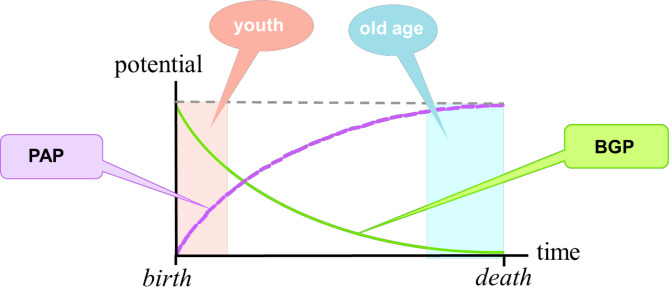
Where does a person find the resources to meet the demands of life? To this end, each human being has a biologically given potential (BGP) and a personally acquired potential (PAP) (figure 1). These two resources must be available not only in the present, but also in the short-term and long-term future. That is why they are termed potentials. The BGP results from the genetic equipment and the quality of the pregnancy. It is the gift every person receives at birth (figure 2). It is greatest at the time of birth but decreases over time and reaches zero at the time of death. It is supported, for example, by a healthy lifestyle and by physical training, or reduced by undernutrition, overweight, alcohol and drug use. Any physical illness reduces the BGP temporarily or even permanently.
At birth the PAP is small but already present as an expression of the personality of the newborn. At first, it expands rapidly, with time, however, more slowly. Whenever a person continuously strives to improve it, the PAP can evolve favourably throughout the whole life. Everything that has been learnt, the way life was led, and how negative experiences were taken care of may increase maturity. The PAP may also compensate in part for losses of the BGP. An outstanding example is paraplegia. Such patients may learn to deal with their new and difficult life situations and may even become professionally active again. As soon as they meet the demands of their life, the Meikirch model considers them again as healthy.
Every person lives in contact with his or her social environment, that is, with the social determinants of health. An infant is nursed and cared for by the mother. Often, a father and siblings are also there. Later, nursery, schools and vocational training are added. For adolescents, the social environment develops continuously into adulthood, into working life and into their own family life. Even in the later phase of life, the person has to deal with himself and the social environment. But individuals also shape their environment. Culture of social relations, peace and war, and wealth and poverty leave their marks.
Figure 1.
Schematic representation of the Meikirch model. The five components of the model are labelled. Among them, there are 10 complex interactions represented as double-ended arrows.
Figure 2.
Timeline of the potentials. While the BGB decreases spontaneously with ageing, the PAP rises from its beginning. Over time, it will take more and more personal commitment by the concerned person to work for its increase. In real life, both potentials are always needed at the same time. The sum of the two potentials, the dashed line, happens to be horizontal in this graph. This occurred just by chance. BGP, biologically given potential; PAP, personally acquired potential.
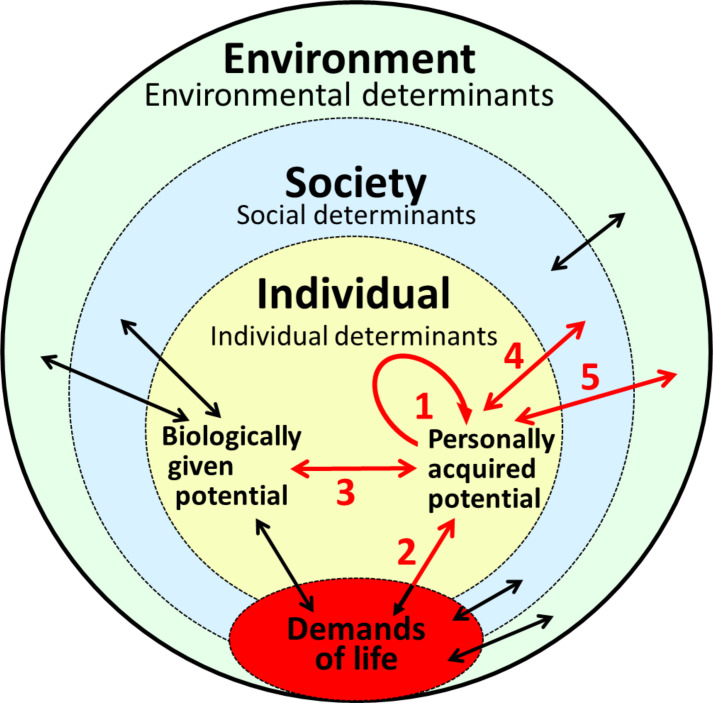
An individual must assume responsibility for his or her health in five different relationships which function mutually (figure 3):
Figure 3.
Personal responsibility for health must - as discussed in the text - be analysed in the five different directions shown in red.
First of all, the person bears responsibility for his or her own PAP because its further development depends on the commitment of the individual to evolve in self-responsibility.
The PAP, together with the BGP, must be adequate and appropriate for the demands of life. Both underdemand and overdemand may be damaging. These demands are not entirely within the control of an individual, but when analysed from a distance, there are always degrees of freedom.
The relationship between the PAP and the BGP can be compared to the relationship between a rider and his horse. The horse needs adequate nutrition and fluid supply, a sheltered place for the night, horseshoes and a place where it can move around. The better the rider takes care of his horse, the better his horse can provide him with the desired services.
Each person is continuously in contact with various members of the society, whether they are family, friends, or professional or official contacts. These interactions can be cordial, friendly, formal, cold or even hostile. However, we cannot shirk our responsibilities to other people. Human relationships are vital for our personal development.
The outermost layer of the Meikirch model shows that every human being is surrounded by the natural environment. It contains our livelihoods, but also our risks. Today, people are increasingly damaging the environment for personal advantages. There are many vicious circles, but, unfortunately, they are not sufficiently recognised. Looking at international politics, we find that humanity is not truly willing to assume its responsibility.
With the aforementioned explanations, the five components of the Meikirch model are described. It is crucial to note that there are 10 complex exchange processes, always working in both directions between all components as illustrated by double arrows in figure 1.
Health as a complex adaptive system (CAS)
The present combination of 5 components and 10 complex interactions can be understood as a CAS.12 13 Such systems are not easy to describe. In our context, however, they have several characteristic properties that are relevant for personal developments of individuals, patient–physician interactions, for the organisation of healthcare and for public health.14 I would like to point out just a few of them that are particularly important within our context.
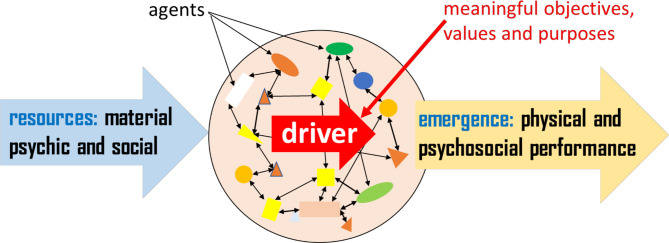
A CAS is an autonomous unit that is clearly separated from its surroundings and contains in its interior many different parts (figure 4). These are called agents. Each of them performs its own specific functions and exchanges materials rules and ideas with each other on an ongoing basis. The inner force that organises the CAS is the so-called driver. It results in part from the attitude toward the biology, that is, from hunger, thirst, and other necessities of life. In everyone, however, it also includes human relationships, the need for sexual fulfilment (hedonism) or for the meaning of life (eudaimonia) and many other motives. Interestingly, the driver is not fully but more or less in control of the agents. In each person, the input, that is, the source of energy, consists of material, psychic and social resources that involve material and immaterial—psychosocial—features. The total productive performance of a CAS is called emergence and includes, for example, the ordered physical and psychosocial actions of a person. Thanks to this arrangement, a CAS always functions as a self-determined whole.
Figure 4.
Schematic representation of a complex adaptive system.
The organisation of a CAS varies between stability and lability. For this reason, a CAS is able to maintain an identity while slowly, and autonomously, adapting to minor changes in its environment. This is how childhood, further evolution and ageing of persons occur. However, if these changes exceed certain limits, the CAS will be plunged into a crisis. This is the case when it is exposed to strong influences from the outside or inside. In humans, crises arise, for example, during puberty, after a psychological shock, as a result of an accident or in response to an aggressive infectious agent. While in the crisis, the CAS first tries to compensate or repair the foreign influences, but as soon as possible, it returns to its prestate. As an alternative, a CAS may also evolve to real adaptation reactions that lead to a further development of the CAS. In any case, the driver, representing the identity of the system, resists external influences as much and as long as it is able to. For example, a CAS may avoid a crisis by resisting authoritarian rules. This explains why external instructions from above or from the side are usually ineffective. Intrinsic motivation is essential.
The sum of the listed properties of a CAS explains why all persons can and must develop themselves from birth to death. In addition, difficulties and crises are normal occurrences, and unfortunately, many of them are not overcome successfully. Then they can be the causes of symptoms and diseases and may need to be approached with understanding and compassion by nurses, psychologists and physicians. Psychotherapy may be needed.
Meikirch model
The Meikirch model may be summarised as follows: ‘To be healthy a human individual must be able to satisfy the demands of life. For this purpose, each person disposes of a biologically given and a personally acquired potential, both of which are closely related to the social surroundings and the natural environment. The resulting complex adaptive system enables the individual to unfold a personal identity and to develop it further until death. Healthcare has the purpose to empower each individual to fully realize optimal health’.
Hypotheses for the healthcare system derived from the Meikirch model
The Meikirch model provides a concept of health that is scientifically based and can be rationally analysed. It generates hypotheses that can be compared with the current practice of medicine and public health. In comparison, the current organisation for improving and maintaining people's health suffers from important limitations. If today’s medicine and public health recognised both potentials and a lifelong evolution of the CAS as essential parts of health, many of today's difficulties might become much more manageable. Improved health and reduced healthcare costs become quite probable. These hypotheses could be tested and the consequences implemented.
Biologically given potential
So far, somatic medicine was focused on treating disorders of the BGP with medications, surgery, radiation, genetic tools and rehabilitation measures. For this purpose, whenever possible, scientific methods were applied. In so doing, medicine has in some fields achieved great improvements in health, because many diseases that hitherto could not be treated are now amenable to therapy. Medical research is also working to develop further innovative treatments. While many new drugs are becoming excessively expensive, various therapeutic options have improved significantly in recent years. Despite all the accumulated evidence, the real benefit of treatments may still not be optimal. Many patients are neither given the best instructions nor are they motivated to make the best out of their treatment options. Consequently, the question should be investigated as to whether care for the BGP should not be combined with compulsory attention to every patient’s PAP and CAS. This approach may lead to better short-term and long-term results, thereby reducing healthcare costs. Two recent developments are interesting. Digital self-monitoring (self-tracking) is now used for many conditions to improve personal feedback.15 16 These are good possibilities to improve self-management in chronic diseases but need further investigation.
Personally acquired potential
Unfortunately, in today’s ‘scientific’ medicine, the PAP predominantly remains a ‘blind spot’ and is often benevolently neglected. The personality of a patient is viewed as being his private matter. A person growing up and living in good circumstances tends to experience a normal maturation of his or her PAP that corresponds approximately to the individual’s age. Ideally, the patient should not have been exposed to circumstances that led to significant blockages of the evolution of the CAS. Yet, the cultures of today’s societies are concerned with income and consumerism and do not care for personal maturation or for the overcoming of blockages that have arisen due to stressing experiences in the past. The overall tendency is to avoid speaking about this subject. This attitude does not support health.
At present, the responsibility of the individual and of the society for a healthy evolution of a CAS or a PAP is a matter of culture. Interestingly, positive psychology offers different techniques for reduction of symptoms, for improvement of personal resilience and for facilitating development of the personality.17–19 Therefore, these methods deal with the CAS and the PAP. They can be applied by professionals or learnt by individuals and become included within their daily routine. Such treatments include different forms of meditation and the emotional freedom technique. Since the PAP may now be open to self-treatment and treatments by therapists, the hypothesis may be tested as to whether all treatments for the BGP should, in the interest of the patients, be combined with an assessment and treatment of the PAP. In addition, such an approach may also fulfil the interest in reducing costs.
Attention to the PAP might be particularly important for chronic conditions such as diabetes mellitus, hypertension, asthma and many others that require a continuous careful treatment.20–22 This entails adequate knowledge and a personality that is ready to assume such a long-term responsibility. Presumably, repeated highly trusted interactions with a nurse, a psychologist or a physician may be required. These postulates result from the Meikirch model but should be verified scientifically.
When services for the PAP need to be paid, difficulties arise because the personal and social responsibilities for a healthy evolution are unclear. It would therefore be important to better understand how the two could be evaluated and what the implications for the coverage of any associated costs might be. Individual development generally is considered to be a personal responsibility. Yet, the society may have been damaging it. Therefore, it is not clear, how to find a rational basis for a health insurance to cover such costs. There is an urgent need to better understand the PAP and the CAS in every person in order to draw the proper conclusions for financing treatments.
Healthcare system as a CAS
The healthcare system is by itself also a CAS. What does this assertion contribute to a better understanding of the rising healthcare costs? How could it help to reduce costs? Political measures of cost reduction have so far remained futile and have damaged the best interests of patients, healthcare personnel and citizens. Therefore, Sturmberg and I have explored the possibilities of interpreting healthcare systems as socially constructed CAS. We found that by their very nature, such systems cannot be expected to respond properly to top–down organisations. They rather follow their driver, the primary purpose, and this is health as defined by the Meikirch model.12 14 Yet, unfortunately, today’s healthcare systems are organised top–down and their economic models are based on profit maximisation. Such constructs are fundamentally unsuitable for adequately responding to the complexities of health and of healthcare. They have rather shifted their focus away from health towards pressing economic considerations. Although these are important, they must serve the main purpose of healthcare and not dominate its delivery. Consequently, excessive needs for money and unhappy personnel are logical consequences of an inadequate structure.
An organisation having the purpose to respond to the complexity of each patient’s health-needs has, by necessity, to be organised from the bottom–up.23 Since health is the goal to be pursued for each individual patient, the Meikirch model needs to be taught to all collaborators. Interdisciplinary teams of, for example, physicians, nurses, physiotherapists, psychologists, social workers and administrators are optimal organisations to address the complex problems of each individual patient. For the functioning of the institution as a whole, leadership is needed but not management. Such a setting allows physicians to follow their professional norms as codified in the universally accepted Declaration of Geneva 2017.24 This also postulates that the health and well-being of patients must come first. An interesting example of a bottom–up organisation in healthcare has arisen in the Netherlands. ‘Buurtzorg’ is a nurse-led, nurse-run organisation of self-managed teams that provide home care to patients in their neighbourhoods.25 Their vision is championing humanity over bureaucracy, autonomous teams that work with primary care providers, community support and family resources to bring patients to optimal functioning as quickly as possible. The award-winning organisation grew out of a common-sense approach based on principles of trust, autonomy, creativity, simplicity and collaboration. These organisational principles and values translate into highly effective and efficient care, very satisfied patients and enthusiastic nurses. In addition, Ernst and Young have calculated a 40% reduction in costs.25 The model is being replicated worldwide, with teams starting in Minnesota, Sweden, Japan and other countries, including Switzerland.
Therefore, it may be hypothesised that a bottom–up reorganisation of healthcare systems with the goal of improving human health—in accordance with the Meikirch model—will improve the quality of care, increase patient satisfaction, improve the motivation of the workers and finally reduce costs. There are many good reasons for this hypothesis, but obviously it needs to be tested.
Healthcare of patients is a high and noble challenge
As a result of the many regulations, financial incentives and quality controls, a highly qualified standard of care for patients has become difficult to achieve. These summarised influences deal only with the material side of medicine and neglect the PAP of the patients. The staff members are also exposed only to material features. Many regulations neglect the PAP, have nothing to do with health as CAS and dehumanise the health system. In contrast, interaction with a person in a health crisis is a great, multidimensional challenge for all types of caregivers. Therefore, when one of them suddenly becomes able to commit himself or herself to the goal of achieving the best health for every diseased person, a burst of inner strength and dynamism results. The trust of patients and coworkers that arises from this attitude is rewarding and makes being a doctor or a nurse one of the most inspiring professions that exist. It offers fulfilment and meaning. Doctors and nurses who experience this acknowledge a deep satisfaction in their profession. If the working conditions are good and include a reasonable salary, they can hardly become motivated to change their ways and attitude by bonuses and a seductive income.
Since the industrialisation of medicine, however, materialism has penetrated deeply into the healthcare system. Time and financial pressures do not leave enough strength and creativity for the cultivation of the patient–doctor relationship and thereby damage the endowment with meaning of this special type of human interaction. Similar considerations also apply to nursing care. Only a full reorientation towards healthcare as expressed by the Meikirch model can preserve high-quality medical care. For this purpose, all financial incentives must strictly be eliminated. Already now many employees spontaneously see it this way. Some other people involved in the healthcare system will, however, have to do some rethinking and acquire new inspirations. An interesting example is the Mayo Clinic. For years, it has received the highest ranking of US health institutions. At this clinic, all doctors have been employed with a negotiated fixed salary that eliminates financial incentives. Only in recent years, a minor value-based compensation percentage has been introduced.26 Therefore, despite the enormous size of the organisation, it brings about a nationally recognised top quality. The guiding principle reads: ‘The needs of patients come first’.
Hypotheses for public health resulting from the Meikirch model
Public health is already providing a great service concerning people's health. In Switzerland, the iodination of salt, the fluoridation of toothpastes and the vaccination against poliomyelitis were extremely successful against hypothyroidism, dental caries and poliomyelitis. Vaccinations have also greatly reduced many other infectious diseases. Clean water and hygienic handling of food are normal. However, obesity, hypertension, alcoholism, smoking and other chronic illnesses are not eliminated and still lead to the corresponding follow-up diseases, such as diabetes mellitus, hypertension, myocardial infarctions, lung cancer and chronic obstructive pulmonary disease. Interestingly, even now, measles vaccination is meeting with resistance from the population.27 AIDS and other venereal diseases are still spreading, just a little slower and at a more discreet level than before.28 These examples reveal that public health can be highly successful in protecting the BGP. It has its limits, however, when the PAP or the driver of the CAS is involved. This could be related to the fact that external information about disease risks and requests to change life habits reach people mainly from the outside—that is, ‘top–down’—and accordingly are repelled. In addition, many people live with the idea that, in the case of an accident or a disease, we have a good healthcare system that will take care of the problem.
For a greater success of health promotion, it might be advisable to focus more on the development of the PAP and combine this with an approach via the driver of the CAS. For this purpose, it might be interesting to investigate whether health promotion with the Meikirch model might be more successful when it has already been introduced in primary schools. This is a time when the driver of the CAS is in an early stage of development. In the early years, the prerequisites for attracting the children to a realistic idea of health might be more favourable than during puberty. Approaches to this idea are already available, for example, in the form of school dental care, which in Switzerland has been highly successful in the 20th century. Presumably, teaching might continue during puberty until the end of formal education and training. This approach should also involve the CAS with its driver. The aim must be to create a new culture of health throughout the whole population. In adults, teaching about health should be based on the complete Meikirch model. Some details may be very informing: the BGP is a personal gift that must be maintained and protected from harm throughout the whole life. The PAP is a sphere of self-responsibility that evolves continuously. It allows an individual to grow towards becoming a mature person. When difficulties occur, there is a possibility for help. Within this context, self-guided exercises could also be quite useful. Already children should learn what the CAS and its driver are, how to prevent bad feelings and how to deal positively with them. Such teaching in children may stimulate the interest of the parents and friends and eventually fulfil its purpose, the establishment of a living culture of health. The effect of these measures on uncontrolled diseases in adults, such as obesity, diabetes, hypertension, alcoholism, smoking and venereal diseases, needs to be demonstrated.
Footnotes
Contributors: JB is the sole author.
Funding: All costs of the project have only been payed by the author. He has not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Bircher J. Meikirch-Modell. Available: www.meikirch-model.ch
- 2. Bircher J, Kuruvilla S. Defining health by addressing individual, social, and environmental determinants: new opportunities for health care and public health. J Public Health Policy 2014;35:363–86. 10.1057/jphp.2014.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bircher J, Hahn EG. Will the Meikirch model, a new framework for health, induce a paradigm shift in healthcare? Cureus 2017;9:e1081. 10.7759/cureus.1081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Porter ME, Teisberg EO. Redefining competition in health care. Harv Bus Rev 2004;82:64–76. 136. [PubMed] [Google Scholar]
- 5. Porter ME, Teisberg EO. Redefining health care. Harvard Business School Press, 2006. [Google Scholar]
- 6. World Health Organization . WHO definition of health, 1948. Available: http://www.who.int/about/definition/en/print.htmlNo
- 7. Nordenfelt L. On the nature of health. Kluwer Academic Publishers. [Google Scholar]
- 8. Nordenfelt L, Liss P-E. Dimensions of health and health promotion. Amsterdam-New York, NY: Editions Rodopi, 2003. [Google Scholar]
- 9. Bircher J. Towards a dynamic definition of health and disease. Med Health Care Philos 2005;8:335–41. 10.1007/s11019-005-0538-y [DOI] [PubMed] [Google Scholar]
- 10. Huber M, Knottnerus JA, Green L, et al. How should we define health? BMJ 2011;343:d4163. 10.1136/bmj.d4163 [DOI] [PubMed] [Google Scholar]
- 11. van Spijk P. On human health. Med Health Care Philos 2015;18:245–51. 10.1007/s11019-014-9602-9 [DOI] [PubMed] [Google Scholar]
- 12. Sturmberg JP, Bircher J. Better and fulfilling healthcare at lower costs: the need to manage health systems as complex adaptive systems. F1000Res 2019;8:789. 10.12688/f1000research.19414.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sturmberg JP, Martin CM. Handbook of systems and complexity. New York: Springer Science+Business Media, 2013. [Google Scholar]
- 14. Sturmberg JP. Health system redesign. Cham: Springer International Publishing, 2018. [Google Scholar]
- 15. Morton K, Dennison L, May C, et al. Using digital interventions for self-management of chronic physical health conditions. Patient Educ Couns 2017;100:616–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bartels SL, van Knippenberg RJM, Dassen FCM, et al. A narrative synthesis systematic review of digital self-monitoring interventions for middle-aged and older adults. Internet Interv 2019;18:100283. 10.1016/j.invent.2019.100283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Garland EL, Farb NA, Goldin P, et al. Mindfulness broadens awareness and builds Eudaimonic meaning: a process model of mindful positive emotion regulation. Psychol Inq 2015;26:293–314. 10.1080/1047840X.2015.1064294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Stahl JE, Dossett ML, LaJoie AS, et al. Relaxation response and resiliency training and its effect on healthcare resource utilization. PLoS One 2015;10:e0140212. 10.1371/journal.pone.0140212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lin Y, Fisher ME, Roberts SMM, et al. Deconstructing the emotion regulatory properties of mindfulness: an electrophysiological investigation. Front Hum Neurosci 2016;10:1–13. 10.3389/fnhum.2016.00451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Coventry PA, Small N, Panagioti M, et al. Living with complexity; marshalling resources: a systematic review and qualitative meta-synthesis of lived experience of mental and physical multimorbidity. BMC Fam Pract 2015;16:171. 10.1186/s12875-015-0345-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Orom H, Underwood W, Cheng Z, et al. Relationships as medicine: quality of the physician-patient relationship determines physician influence on treatment recommendation adherence. Health Serv Res 2018;53:580–96. 10.1111/1475-6773.12629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kissling B, Ryser P. Die Ärztliche Konsultation. Vandenhoek & Ruprecht Verlage, 2019. [Google Scholar]
- 23. Laloux F. Reinventing organizations, a guide to creating organizations inspired by the next stage of human consciousness. Maharashtra, India: Knowledge Partners, 2018. [Google Scholar]
- 24. World Medical Association . Declaration of Geneva, 2017. Available: https://www.wma.net/policies-post/wma-declaration-of-geneva/ [DOI] [PMC free article] [PubMed]
- 25. Monsen KA, de Blok J. Buurtzorg: nurse-led community care. Creat Nurs 2018;24:112–7. 10.1891/1078-4535.19.3.122 [DOI] [PubMed] [Google Scholar]
- 26. Bunkers B, Koch M, Lubinsky J, et al. Value-Based physician compensation: a link to performance improvement. Healthc Financ Manage 2016;70:52–8. [PubMed] [Google Scholar]
- 27. Richard J-L, Mäusezahl M, Basler S, et al. Approaching measles elimination in Switzerland: changing epidemiology 2007-2018. Swiss Med Wkly 2019;149:w20102. 10.4414/smw.2019.20102 [DOI] [PubMed] [Google Scholar]
- 28. HIV, syphilis, Gonorrhoe und Chlamydiose in der Schweiz im Jahr 2018: eine epidemiologische Übersicht 2018.