Introduction
Recent increases in the numbers of children diagnosed with autism spectrum disorder (autism)1 2 have led to growing demand on clinical services, with evidence of long waiting times for diagnostic assessment.3 4 In response, the National Health Service (NHS) Long Term Plan3 expresses the desire ‘to test and implement the most effective ways to reduce waiting times … achieving timely diagnostic assessments… [and] support children with autism or other neurodevelopmental disorders including ADHD’.3 In line with the recent ‘Embracing Complexity in Diagnosis’ report, ‘Multi-Diagnostic Pathways for Neurodevelopmental Conditions’,5 this paper argues that adopting an integrated neurodevelopmental service model, with access to the necessary competencies, and remit, to assess and manage children with any combination of autism, attention deficit hyperactivity disorder (ADHD) and associated conditions may make better use of limited staffing resources, significantly reduce costs of assessment and improve the child and family’s journey through the diagnostic process. This could also give a more accurate overall picture of the child’s needs and diagnostic formulation to inform ongoing support for the child and their family from health services, as well as education and social care.
Autism and ADHD frequently co-occur,6–8 may be genetically linked9 and often present similarly. Yet in the UK, they are often managed in separate pathways under the auspices of Child Development Teams (CDTs) and/or Child and Adolescent Mental Health Services (CAMHS).10 11 This can result in referrals ‘bouncing’ backwards and forwards between CAMHS and CDTs, leading to delays in, and/or duplication of, assessment, and a poor child and family experience. Beyond healthcare, each child will also spend much of their time within educational settings and may also receive support from social and related care services, such as ‘Early Help’. Boundaries around services vary nationally, so for example some CDTs will only see children of preschool age with possible autism, while others see children up to age 19 years.12 13 Similarly, in some centres ADHD is managed in CDTs, while in others this comes under CAMHS. In reality, National Institute for Health and Care Excellence (NICE) guidelines10 11 advise a multidisciplinary approach to diagnosis in both conditions, with access to the skills of both CAMHS and CDT staff, including a core team of a paediatrician or child psychiatrist, a speech and language therapist, a clinical and/or educational psychologist and potentially others including occupational therapists, social workers and nurses. This should enable the assessment to consider, for example, other neurodevelopmental disorders, and mental and behavioural disorders and to ‘construct a profile for each child or young person, for example intellectual ability, language and communication, motor skills, and mental and emotional health’.10
The authors of this paper represent two CDTs. One is based in a large mixed urban–rural county, where there are three provider trusts, four CDTs and four CAMHS teams. While a newly commissioned, joint CAMHS/CDT complex cases clinic pilot is about to start, to assess children with diagnostic complexity, current commissioning and practice requires children with possible autism up to age 11 to be seen within CDTs, while children with possible ADHD and older children with possible autism are the remit of CAMHS. The second centre operates a fully integrated CDT/CAMHS service, colocated in a single building, in a city organised as a unitary authority, facilitating close working between health, education, social care and child and family support services. School-aged children with possible ADHD and autism are seen by an ‘Integrated Neurodevelopmental Team (INT)’ to assess their needs, strengths and diagnostic formulation. The professionals are selected to undertake the assessment based on their competencies and child’s needs rather than professional background.
We present the journeys of a typical primary school-aged child referred with a history suggestive of either autism and/or ADHD and the pathways they would follow in each service. This illustrates how the integrated and non-integrated approaches can affect the professional time involved, the resulting NHS costs and the patient journey. Costings are based on the methodology used for our previous work on costing NHS assessment of a child with possible autism,12 taking costs for the staff involved from the ‘Unit Costs of Health and Social Care 2017’14 and multiplying this by the amount of time each staff member contributed to the child’s assessment.
Scenario
A primary school-aged child was referred to the CDT in the non-integrated service by the general practitioner with concerns about challenging behaviour, difficulties in social interaction and communication, repetitive behaviours and sensory issues, evident across settings including in school. At the initial assessment, the consultant paediatrician felt these concerns warranted a full multidisciplinary diagnostic assessment for possible autism. Additionally, the child was noted to be very hyperactive, while history identified difficulties in concentration, distractibility and impulsivity, confirmed on school and home ADHD Rating scales.15 The child was therefore referred to CAMHS for assessment for possible ADHD, but was passed on to a locally delivered parenting programme. During school observation by a specialist speech therapist, and formalised observation using the Autism Diagnostic Observation Schedule (ADOS)16 by a clinical psychologist, the child exhibited high levels of hyperactivity and poor concentration. Re-referral to CAMHS for assessment of possible ADHD was then accepted.
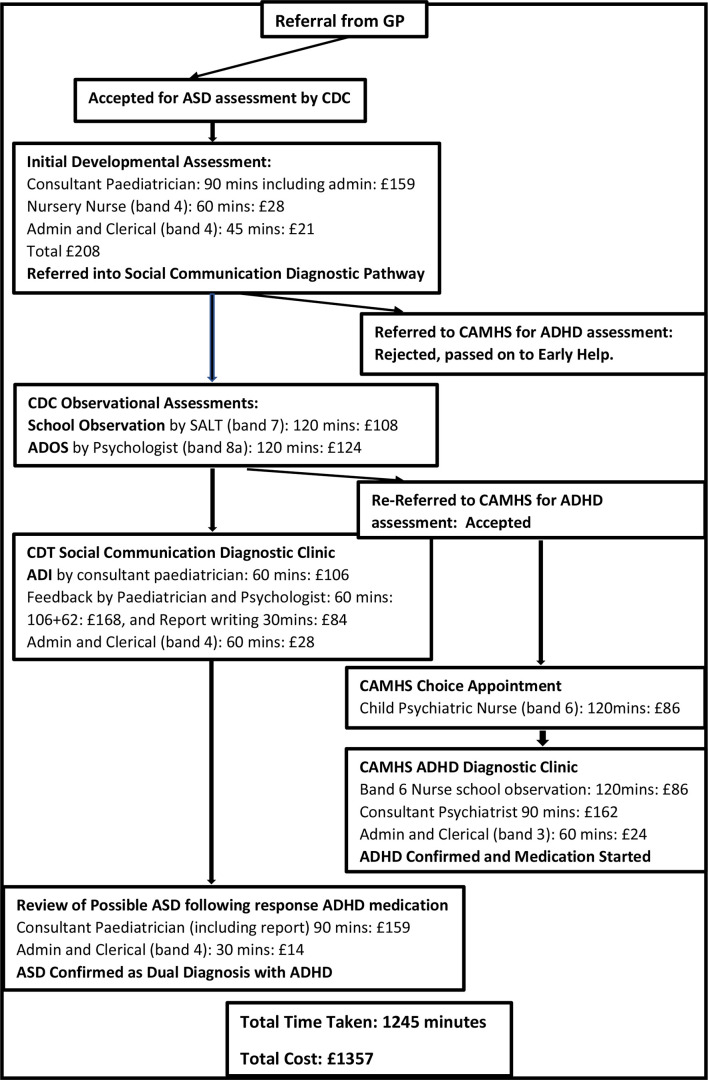
Diagnostic assessment in the CDT, including formal history concluded the child almost certainly had autism, but that ADHD symptoms were at a level where this could also explain his social communication difficulties. It was agreed, therefore, to await the CAMHS assessment and response to treatment, before confirming, or excluding, an autism diagnosis. Following diagnosis of ADHD and initiation of medication, a diagnosis of autism was confirmed by the CDT. The assessment required 20.75 hours of professional time, costing the NHS £1357 (figure 1). The journey time from referral to completed diagnostic formulation could take up to 2 years.
Figure 1.
Diagnostic pathway experienced in the non-integrated approach, including professional time taken at each stage, and resulting NHS costs. ASD, Autism Spectrum Disorder: ADHD, attention deficit hyperactivity disorder; ADI, Autism Diagnostic Interview; ADOS, Autism Diagnostic Observation Schedule; CAMHS, Child and Adolescent Mental Health Services; CDC, Child Development Centre; CDT, Child Development Team; GP, general practitioner; NHS, National Health Service; SALT Speech and Language Therapist.
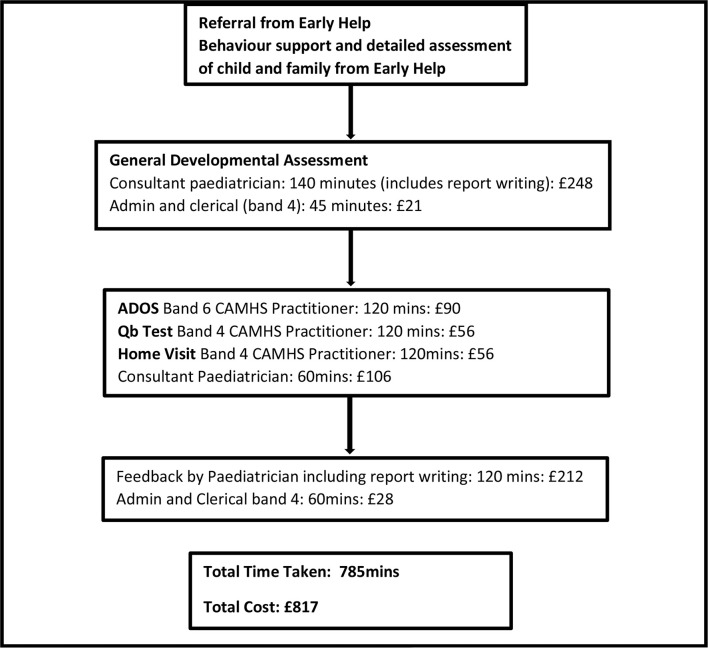
A similar child seen in the integrated service would experience a single joined up assessment pathway (figure 2), following referral through the Early Help assessment process. His parents had already attended a parent training programme and had classroom observations undertaken by a ‘Project for Schools’ mental health nurse commissioned by the Joint Commissioning Unit. The school had implemented needs led support and provided information to support the referral. At the initial General Developmental Assessment, the consultant paediatrician felt these concerns were at a level where a full multidisciplinary diagnostic assessment for possible autism and ADHD was warranted. The child was therefore referred to the INT for this.
Figure 2.
Diagnostic pathway experienced in the integrated approach, including professional time taken at each stage, and resulting NHS costs. ADOS, Autism Diagnostic Observation Schedule; CAMHS, Child and Adolescent Mental Health Services; NHS, National Health Service.
Diagnostic assessment in the INT consisted of ADOS,16 home visit and Qb test (a computerised assessment of hyperactivity, impulsivity and inattention)17 undertaken by CAMHS practitioners. The diagnosis of autism and ADHD was fed back to parents by the paediatrician. The overall assessment required 13 hours of professional time, costing the NHS £817. For the family this journey would last around 26 weeks from the time of the original referral.
Discussion
This scenario demonstrates what often feels like a very inefficient and, for the parents, frustrating journey to a diagnostic conclusion for their child presenting with a mixture of difficulties in social communication, concentration and hyperactivity.5 Commissioning of separate autism and ADHD pathways, one with the CDT and the other with CAMHS, resulted in the child having to go through both pathways despite considerable overlap of assessment. The integrated approach, by running a single assessment process, cutting out this overlap, required less professional time (13 vs 20.75 hours), at a lower cost (£817 vs £1357), and reduced the time taken to reach a completed diagnostic formulation. Furthermore, the additional time and cost taken reduced the capacity of the first service to meet wider demand for assessment.
Given the above, and the negative experiences reported by parents,18 this does beg the question why integrated pathways are still a novelty at secondary care level in neurodevelopmental services. One of the challenges experienced by the authors has been that CAMHS and CDTs often sit in different health trusts, who have been commissioned to deliver specific pathways. With ADHD often perceived as a mental health disorder, and autism, at least in younger children, seen as a neurodevelopmental disorder, commissioning and service delivery frequently fails to recognise how enmeshed these, and related, conditions, such as Developmental Coordination Disorder and Anxiety Disorder, are.5 This has been compounded by the separation of autism and ADHD in previous diagnostic coding systems such as Diagnostic and Statistical Manual of Mental Disorders, 4th Edition,19 in which the two diagnoses were considered mutually exclusive. With the current financial pressures on all NHS trusts, there is an understandable reluctance for trusts to change and take on what is seen as ‘new’, and non-commissioned work. At the same time, injecting new funding which might overcome this reticence is equally challenging for commissioners who are under financial and political pressure to fund services elsewhere in the NHS, for example, in delivering safe and timely accident and emergency or cancer services.
Our experiences suggest that an integrated pathway is possible, and when clinicians from both CDTs and CAMHS get together with parent groups and commissioners, is generally perceived as a sensible way ahead. Experience from running the integrated team as a single service with a shared commitment to working with children who may have autism, ADHD and/or related conditions suggests this is essential. Colocation of administrative and clinical bases is fundamental to develop a true multidisciplinary team that maximises the range of competencies through training and supervision. This also enables assessment of more complex presentations,5 for example in considering differential diagnoses such as attachment disorder, epilepsy and fetal alcohol spectrum disorder (FASD), or underlying conditions such as genetic syndromes. For example, the INT has a specially trained paediatrician experienced in the care of looked after children (LAC) and FASD, and an LAC psychologist with training in attachment disorder. This meets the requirements of the NICE guidelines9 that the team should have the skills to be able to assess and manage differential diagnoses, underlying cause and comorbidity. For example, investigation for underlying genetic disorders or epilepsy tends to be considered the realm of paediatricians, assessment of intellectual ability/disability the realm of a psychologist, whether educational or clinical, while complex psychopharmacology should generally be managed by a child psychiatrist.
Experience from the INT suggests the efficiencies and user experience can be improved further if the pathway is aligned with Early Help Pathways, and prediagnosis and postdiagnosis parent training programmes that are commissioned jointly by NHS and Local Authority commissioning. This can also enhance the quality of information available at the time of referral, including response to any intervention already offered, which in turn can reduce time spent within the diagnostic pathway.
Whether the team should sit within a single organisation, as was agreed for the INT, or whether this is possible when the services are still based in separate organisations remains to be seen. Working within a single organisation accountable for the delivery of the integrated service, one suspects, may reduce the likelihood of each part of the team being put under pressure to deliver other areas their host organisations are currently responsible for, such as anorexia or suicide for CAMHS, or complex neurodisability or child protection in the case of CDTs. This would also enable an approach where the multidisciplinary team required for an individual child’s assessment could be based on the competencies required to address the specific presentation and needs of the child, rather than which service they are referred to.
In conclusion, moves toward running integrated CDT/CAMHS services for children with potential neurodevelopmental and/or mental health conditions have the potential to improve efficiency of service delivery. As such, it is an approach worth exploring elsewhere, to understand the factors that may lead to its success, or indeed failure, in different settings, for example whether this will be achievable in the first centre described above, with its context of being a large county with multiple providers and commissioners. Moves to integrate across other agencies working with children, including social care and education, may further enhance service delivery and family experience.
Acknowledgments
We acknowledge the advice given by Professor Heather Gage, Health Economist at University of Surrey, on the methodology for our previous work on costing autism services, which we also applied to this paper. While this paper was largely written prior to starting our Realist Evaluation of Autism Service Delivery study, and is not a direct output from that study, we also acknowledge our co-applicants in the study team (Professor Jeremy Parr (Newcastle University), Professor Patricia Wilson (University of Kent), Dr Peter Williams (University of Surrey), Amanda Allard (Council for Disabled Children), Dr Lorcan Kenny (Autistica), Dr Grainne Saunders (West Sussex Parent Carer Forum), Dr Victoria Grahame (Northumberland Tyne and Wear NHS Trust), Sue North, MBE (NHS England) and Kat Wilmore (parent), for their contributions to our thinking.
Footnotes
Contributors: All authors have contributed to the writing of this article. IM and VR represent the child development services described, while WF has worked with IM looking into the costs of autism service delivery including paper already published in BMJ Paediatrics Open.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Baio J, Wiggins L, Christensen DL, et al. Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. MMWR Surveill Summ 2018;67:1–23. 10.15585/mmwr.ss6706a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Waugh I. The prevalence of autism (including Asperger syndrome) in school age children in Northern Ireland 2018. information analysis Directorate, DoH, N Ireland 2018.
- 3. NHS England . Learning disability and autism. The NHS long term plan, 2019. Available: https://www.longtermplan.nhs.uk/
- 4. Care quality Commission and Ofsted. local area send Inspections, one year on. Ofsted, Manchester 2017. [Google Scholar]
- 5. Embracing Complexity . Embracing complexity in diagnosis: Multi-Diagnostic pathways for neurodevelopmental conditions. embracing complexity coalition, 2019. Available: http://embracingcomplexity.org.uk/assets/documents/Embracing-Complexity-in-Diagnosis.pdf
- 6. Leitner Y. The co-occurrence of autism and attention deficit hyperactivity disorder in children - what do we know? Front Hum Neurosci 2014;8:268. 10.3389/fnhum.2014.00268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Simonoff E, Pickles A, Charman T, et al. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry 2008;47:921–9. 10.1097/CHI.0b013e318179964f [DOI] [PubMed] [Google Scholar]
- 8. Salazar F, Baird G, Chandler S, et al. Co-Occurring psychiatric disorders in preschool and elementary school-aged children with autism spectrum disorder. J Autism Dev Disord 2015;45:2283–94. 10.1007/s10803-015-2361-5 [DOI] [PubMed] [Google Scholar]
- 9. Ghirardi L, Brikell I, Kuja-Halkola R, et al. The familial co-aggregation of ASD and ADHD: a register-based cohort study. Mol Psychiatry 2018;23:257–62. 10.1038/mp.2017.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. National Institute for Health and Care Excellence . Autism: recognition, referral and diagnosis of children and young people on the autism spectrum (CG128. London, UK: National Institute for Health and Care Excellence, 2011. [Google Scholar]
- 11. National Institute for Health and Care Excellence . Attention deficit hyperactivity disorder: diagnosis and management. (CG72). London, UK: National Institute for Health and Care Excellence, 2008. [Google Scholar]
- 12. Galliver M, Gowling E, Farr W, et al. Cost of assessing a child for possible autism spectrum disorder? an observational study of current practice in child development centres in the UK. BMJ Paediatr Open 2017;1:e000052. 10.1136/bmjpo-2017-000052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. British association of community child health and Royal College of paediatrics and child health. covering all bases. community child health: a paediatric workforce guide. London, UK. RCPCH 2017. [Google Scholar]
- 14. Curtis L, Burns A. Unit costs of health and social care 2017. personal social services research unit, University of Kent, Canterbury 2017.
- 15. DuPaul G, Power T, Anastopoulos A, et al. Adhd rating Scale-IV: checklists, norms, and clinical interpretation. New York: Guilford Press, 1998. [Google Scholar]
- 16. Lord C, Rutter M D, et al. Autism Diagnostic Observation Schedule. 2 edn. Torrance, CA: Western Psychological Services, 2012. [Google Scholar]
- 17. Vogt C, Shameli A. Assessments for attention-deficit hyperactivity disorder: use of objective measurements. Psychiatrist 2011;35:380–3. 10.1192/pb.bp.110.032144 [DOI] [Google Scholar]
- 18. Crane L, Chester JW, Goddard L, et al. Experiences of autism diagnosis: a survey of over 1000 parents in the United Kingdom. Autism 2016;20:153–62. 10.1177/1362361315573636 [DOI] [PubMed] [Google Scholar]
- 19. American Psychiatric Association . Diagnostic and statistical manual of mental disorders. Fourth Edition. Washington DC: American Psychiatric Association, 2000. [Google Scholar]