Abstract
Objective
The Patient Activation Measure (PAM) assesses the knowledge, skills and confidence of patients to manage their health, and has been consistently used as an outcome measure of health interventions. Using the PAM to tailor interventions to a patient’s activation level is less understood. This literature review aimed to examine evidence for interventions using the PAM to tailor care for patients with chronic conditions, including enablers and barriers to implementation, and the impact on quality of care.
Methods and analysis
A scoping review methodology was used to identify literature reporting on PAM-tailored interventions. The Insignia Health website and Medline database were searched. Included papers were published in English from 2004 to 2017, from Organisation for Economic Cooperation and Development countries, included adult patients with chronic conditions, and a PAM-tailored intervention. Eligible full-text papers were assessed against the inclusion criteria. Data were extracted into tables and summarised to assess the key findings, recurring themes and differences across papers.
Results
Twenty-one papers describing the use of PAM-tailored interventions (n=21) were identified. Interventions included motivational interviewing, health coaching, self-management planning and risk profile assessment. The perceived value and function of the PAM held by organisations, clinicians and patients influenced implementation and use. Evidence for the impact of PAM-tailored interventions on quality of care was limited.
Conclusion
The PAM is being used to tailor a range of interventions for patients with chronic conditions. Clinician perceptions and understanding about the PAM’s value and purpose influenced implementation. Further research is needed about how PAM-tailored interventions can be integrated into clinical practice, and guide the patient-clinician interaction, in ways that improve the quality of patient care.
Keywords: chronic disease management
Key messages.
What is already known about this subject?
A substantial body of evidence has established the association between patient activation levels and patient health outcomes and behaviours.
The Patient Activation Measure (PAM) has been widely used as an outcome measure in studies, but its use as a tool to tailor and adapt care is comparatively less established.
What does this study add?
This scoping review examines research on the use of the PAM to tailor care for patients with chronic conditions.
It finds that the PAM has been used to tailor care within a variety of patient interventions.
This scoping review identifies enablers and barriers for consideration by clinicians in the development and implementation of tailored interventions based on levels of patient activation.
How might this impact on clinical practice or future developments?
Further research is required on the use of the PAM to tailor and differentiate interventions based on levels of patient activation, and the impact this has on quality of care and patient outcomes.
Background
Patient activation has been described as a behavioural concept, and relates to the degree to which patients understand their role in their healthcare, and how competent they feel to fulfil that role.1 Patient activation incorporates elements of self-efficacy and readiness to change, and is moderately correlated with health literacy.1 Patient activation can be measured using the Patient Activation Measure (PAM), which aims to assess ‘patient self-reported knowledge, skill and confidence for self-management of one’s health or chronic condition’.2 3 The PAM includes a scale from 0 to 100, which can be divided into four developmental levels:
Patients may be passive and feel overwhelmed about managing their health. They may be unprepared to take an active role in their own health.
Patients may lack the knowledge and confidence to self-manage their health.
Patients are beginning to take action, but may lack the confidence and skill to support and sustain these behaviours.
Patients have adopted many behaviours to support their health, but may be unable to maintain them when faced with adversity or life stressors.1 4
The four PAM activation levels are marker points on a continuum. Patients proceed through these levels as they make improvements in self-management.1 4 Changes in the levels of the PAM are potentially important but understood as partially arbitrary in nature, given the scalar value of PAM scores and changes between levels do not reflect its scalar nature. With appropriate support, we would expect activation to improve and for patients to progress through these levels. However, it should be highlighted that activation can also be changeable in the opposite direction and decline.5
A substantial body of research has established associations between a patient’s activation level and a variety of clinical indicators, health outcomes and health behaviour. Patient activation has also been shown to be a significant predictor of health service utilisation, healthcare costs and patient experience.1 6–9 Early studies on the nature of patient activation indicate the potential to change or improve a patient’s activation level, and for subsequent positive change in self-management behaviours.10 Several studies have assessed interventions or programmes designed to improve patient activation,6 11 12 and the PAM has been used consistently as an outcome measure to evaluate interventions.
While the PAM has previously been used to tailor or design care plans or interventions to be appropriate to a patient’s activation level,2 10 this method of using the PAM is less understood. In this paper, tailoring refers to health programmes or interventions where a patient’s PAM score is used to inform the intervention or support provided to the patient. Ideally, PAM-tailored interventions would be appropriate to a patient’s activation level, and encourage realistic behaviours.5 For example, support for patients at level 1 of activation may aim to develop self-awareness and increase confidence by making small, manageable changes. Patients at level 3 may work on adopting new behaviours and developing knowledge and skills relevant to their condition.13 There is some evidence to suggest there is value in tailoring care to a patient’s activation level. PAM-tailored interventions, which enable patients to build skills and confidence, have been found to positively effect activation, and improve outcomes of disease management.4 7 When patients are more highly activated, their experience of healthcare and their health outcomes can also improve.7 8 In the UK, patients with the highest level of activation experienced 32% fewer attendances to emergency departments (ED) and 38% fewer emergency admissions than patients with the lowest level of activation.14 Health interventions tailored to patient activation levels appear to have the potential to improve activation and positively impact the health outcomes and experiences of patients as their activation levels improve.
The scoping review described in this paper aimed to examine the evidence available for health interventions that have used the PAM to inform and tailor patient care. The review focused on interventions for patients with one or more chronic conditions (excluding serious mental illness), where PAM scores were used to tailor goal setting, care planning or motivational interviewing. We sought to examine how the PAM was integrated into existing models of care, and the results used to enable clinicians to improve the quality of care, rather than simply measuring the impact of an intervention on a patient’s PAM score.
This scoping review aimed to answer three research questions:
How are the results of the PAM used in clinical settings to inform and tailor care for adult patients with chronic conditions?
What are the enablers and barriers to the implementation and use of the PAM to inform and tailor patient care?
What impact does the use of the PAM to inform and tailor patient care, have on the quality of care?
Materials and methods
A scoping review methodology was used to identify literature reporting on PAM-tailored interventions. This method emphasises the ‘mapping’ of the relevant literature and research evidence available within a particular field, including the key underlying concepts, main sources and type of evidence available. Unlike a systematic review, there is less emphasis on assessing the quality of the research, and diverse study designs are often included. The scoping review approach suited the aims of the research which were to capture broadly how the PAM is being used to tailor care within health interventions for patients with chronic disease. A framework for conducting a scoping review has been previously described15 16 and was used to inform the stages for conducting this review (see box 1).
Box 1. Stages for conducting the scoping review.
Stage 1: identifying the research question.
Stage 2: identifying relevant studies.
Stage 3: study selection using an iterative approach based on the research questions, inclusion and exclusion criteria and increasing familiarity with the literature.
Stage 4: extracting the data.
Stage 5: collating, summarising and reporting the results.
Literature searches
The literature searches commenced with a review of key papers and reports identified by the research team.1 6 17 Further citations were identified from the reference lists of these key sources. The Health Foundation (UK) website was searched to identify publications reporting on patient activation.18 A list of research studies available on the Insignia Health website with reported use of the PAM was reviewed to identify relevant studies.19 A Medline search was conducted using search terms relating to ‘patient activation’ and ‘quality of healthcare’. The search terms used are provided in box 2.
Box 2. Medline search terms associated with patient activation and quality of healthcare.
Medline search: conducted between 4 May 2016 and 31 March 2018
‘patient activation measure’.mp.
(patient adj activation adj measure).mp.
‘short form patient activation measure’.mp.
‘PAM-22’.mp.
‘PAM-13’.mp.
1 or 2 or 3 or 4 or 5
‘quality of health care’/ or clinical competence/ or guideline adherence/ or ‘outcome and process assessment (health care)’/ or peer review, health care/ or quality assurance, health care/ or quality improvement/ or quality indicators, health care/
*Professional Practice/og, st (Organization & Administration, Standards)
clinical care.mp.
exp ‘Delivery of Health Care’/mt, og (Methods, Organization & Administration)
‘attitude of health personnel’/ or *attitude to health/
*‘Continuity of Patient Care’/og (Organization & Administration)
patient care planning/ or case management/
*Patient-Centered Care/mt, og, st (Methods, Organization & Administration, Standards)
attitude to health/ or health knowledge, attitudes, practice/
health education/or consumer health information/ or teach-back communication/
change in practice.mp.
health organisations.mp.
(quality and safety data).mp.
exp Motivational Interviewing/
‘motivational interviewing and goal setting’.mp.
coordination of care.mp.
7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22
6 and 23 (Final search terms)
The initial literature searches, data extraction and analysis were undertaken from March to May in 2016. A second series of searches were conducted between March and May 2018 with the purpose of updating the review. These updated searches included a review of the list of reported PAM studies available on the Insignia Health website (list dated 13 March 2018). Papers dated from February 2016 to 13 March 2018 were reviewed. A Medline search was conducted using identical search terms (provided in box 2). Papers dated January 2016 to 31 March 2018 were reviewed.
Development of the inclusion and exclusion criteria was an iterative process based on the research questions and the research team’s increasing familiarity with the literature. An inclusive approach was taken to study design and the literature source. The following inclusion criteria were refined during the review of key papers, and applied to the screening of studies identified in stages 2 and 3:
Published from 2004 to current;
Published in English;
Available electronically;
The research was conducted in an Organisation for Economic Cooperation and Development country;
Adult patients 18 years and over;
Patients with one or more chronic conditions (excluding serious mental illness);
An intervention where the results of the PAM were used to inform patient goal setting, care planning or motivational interviewing.
The timeframe of 2004 onwards was chosen because this coincided with the development and publication of the PAM.2 An underlying purpose of this scoping review was to inform the development of a pilot intervention study, where the PAM would be used to tailor the care of patients with chronic conditions. Criteria four to six aligned with the patient groups that would be participating in the intervention study, and the Australian context. Papers were excluded if they focused on the association of variables with PAM results. Studies using the PAM as a premeasure and postmeasure for an intervention evaluation were excluded unless the results were used to tailor care within the intervention.
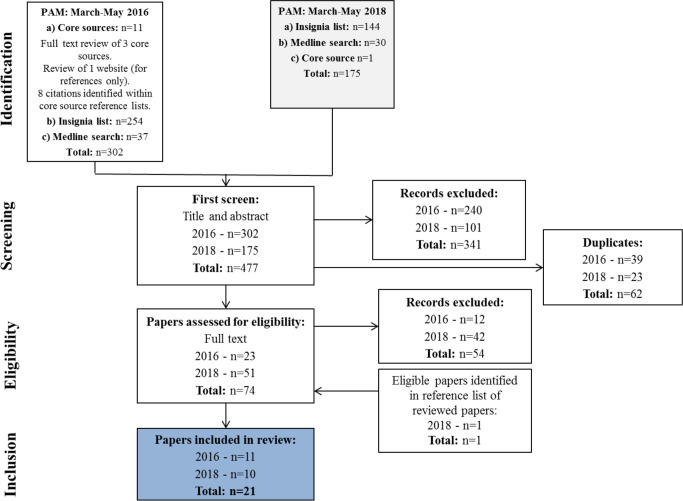
Figure 1 presents a Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow chart describing the review search strategy and screening of studies. Citations from the reference lists of key papers identified by the research team were screened by title and then abstract to determine their relevance to the research questions (RK, JMcD). The titles included in the Insignia Health reference list (published on the Insignia Health website up to 17 March 2016 (list 1) and 13 March 2018 (list 2)) were screened by two reviewers (JMcD, RK). If, after screening the abstract, the paper was determined as eligible, the full paper was obtained for review against the inclusion criteria. Duplicate papers already identified from the review of key papers were excluded. The papers identified by the Medline searches were reviewed using the same process including title and abstract screening, removal of duplicate papers and review of relevant full-text papers against the inclusion criteria (RK). Full-text papers were reviewed by one researcher (RK). Papers were reviewed by another member of the research team (JMcD, BH-R), and discussed during group meetings, if there was uncertainty about whether they met the inclusion criteria.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow chart describing the review search strategy and screening of studies. PAM, Patient Activation Measure.
Data extraction
One researcher performed the data extraction (RK). The data extracted included: author; title; year of publication; country; type of health service; health professionals involved; patient and population groups; study aims, research question; methods; how the PAM was used in clinical settings; how the PAM was administered; enablers and barriers to routine implementation of the PAM results into clinical practice and the impact of implementing the PAM results into clinical practice on clinician and patient behaviour. Information about patient clinical outcomes, health service utilisation and changes to PAM scores were extracted as part of the data on patient behaviours.
Data were summarised focusing on the key information of relevance to the research questions. These summaries were used to assess consistencies and differences across the papers as well as recurring themes. A general summary of all the papers was produced, which provided a ‘snapshot’ of the review and aimed to draw out the key themes and findings of the review.
Results
There were 477 papers identified for screening, including key papers and citations, and targeted searches. The Health Foundation website is identified in the search flow chart as a core source. However, the website was used only to identify other papers and did not contribute data to the review. For this reason, the website is not counted in the number of included papers. After removing 62 duplicates, 341 ineligible papers were excluded following screening of title and abstract. On full-text review, a further 54 ineligible papers were removed. One paper was identified within the reference list of an eligible paper and was included. In total, 21 papers were included in the review. Eleven papers were included from the 2016 series of searches, with a further 10 papers added from the 2018 searches (figure 1).
Characteristics of included papers
Online additional file 1, table 1 presents the characteristics of the included papers. The included papers were published between February 2009 and December 2017 and consisted of project reports and reviews from the grey literature, and intervention studies and evaluations published in peer-reviewed journals. Several papers reported on findings from the same project or study.
ihj-2019-000032supp001.pdf (62.8KB, pdf)
The results describe multiple interventions and approaches for using the PAM to tailor care. Several enablers and barriers for implementation were identified and are described from organisational, clinician and patient perspectives. The impact of PAM-tailored interventions on quality of care focused on changes to clinician and patient behaviours.
Research question 1: how are the results of the PAM used in clinical settings to inform and tailor care for adult patients with chronic conditions?
The included studies demonstrated how the PAM had been used to tailor patient care within a variety of interventions including:
motivational interviewing5 20–22;
health coaching (including coaching for activation)1 4 5 13 22–30;
goal setting11 20 21 27;
development of care and self-management plans11 20 21 31
provision of health information32
hospital to home transition, care coordination, self-management and readmission prevention programmes.1 20 21 24–30
The PAM was used to help clinicians understand how to effectively coach patients, and to tailor support, health information and advice to their activation level.4 11 23 The interventions demonstrated how the PAM could be used to tailor intervention content, health coaching, activity schedules and/or information support.13 24 25 29 30 32 33 The PAM results were also used for risk profile assessment to stratify individuals or population groups based on their clinical indicators and activation level. At-risk individuals or groups could then be targeted for tailored or early intervention programmes.1 5 13 24 25 33
An example of how the PAM was used to adapt patient interventions and encounters included a coaching for activation programme, where coaching interactions were tailored based on the patient’s activation level. For level 1 patients, an appropriate coaching goal could be to enhance their basic knowledge of healthy and non-healthy foods. For level 4 patients, goals were more ambitious and might include implementing healthy eating behaviours.28 In a nurse-led tailored self-management intervention for patients with stroke, PAM results were used to frame discussions with patients to identify goals and develop self-management action plans. Nurses used motivational interviewing and provided self-management advice that was tailored to the patient’s activation level.21 Further detail on how the PAM was used to tailor care is provided in online additional file 2, table 1.
ihj-2019-000032supp002.pdf (196.3KB, pdf)
Research question 2: what are the enablers and barriers to the implementation and use of the PAM to inform and tailor patient care?
Several enablers and barriers affecting the implementation of the PAM to inform and tailor patient care were identified and differentiated into organisation-level, clinician-level and patient-level factors. For some papers, it was difficult to disentangle enablers and barriers that related specifically to implementation of the PAM from the broader intervention. Clinician-level and patient-level enablers and barriers may also have come from various sources. For example, patient-level enablers and barriers were collected from patients or providers. An inclusive approach was taken to reporting considerations for implementation. Further detail about enablers and barriers to the implementation of PAM-tailored interventions is provided in online additional file 2, table 2.
Organisation level
Organisation and leadership support for patient activation, for example, the inclusion of the patient activation concept in the strategic aims of the organisation, influenced the implementation of PAM-tailored interventions.17 23 26 33 Significant planning and support were required at the organisational level to successfully implement a new tool or intervention into existing care arrangements.1 17 23 Cultural changes to patient, professional and provider roles, also influenced implementation and use of the PAM.1
Clinician level
Clinician engagement and ‘buy-in’ about the need for patient-centred care, and the perceived validity of measuring patient activation, were essential to intervention development and implementation.17 33 These factors further emphasise the importance of cultural change at a clinician level.17 Clinicians’ perceptions about the acceptability and value of the PAM, and how easily it could be integrated into care, varied across the studies. In one study, nurses perceived the intervention as an ‘adjunct to ongoing care’ rather than ‘readily integrated’ into routine practice.20 21 The confidence and ability of clinicians to deliver an intervention, and their understanding about the meaning of the PAM results, influenced the implementation process.21 One project evaluation26 found evidence of ‘mediated completion’, where the PAM survey was completed with significant input from others (clinicians or relatives), or clinicians used their pre-existing knowledge of patients to evaluate their responses and intervene if they doubted their validity.26
Patient level
Few papers20 21 26 31 33 discussed patient-level enablers and barriers influencing the implementation of PAM-tailored interventions. There was variation in how the PAM was perceived by patients and professionals,26 and how easy or straightforward it was for patients to complete.20 21 This included challenges associated with language and translation of the survey when administering the PAM with diverse patient groups.33 Some clinicians were concerned that the PAM may not be sufficiently specific to the needs of the patient group they were caring for.20 21 Discrepancies were also observed between patients’ PAM scores, which indicated that most patients were able to actively engage in self-management, and qualitative data which suggested the opposite was true.20 21
Research question 3: what impact does the use of the PAM to inform and tailor patient care have on the quality of care?
We sought to understand the impact of PAM-tailored interventions on quality of care by reviewing the literature for changes in clinician and patient behaviours. We found limited information about behaviour changes, particularly for clinicians, and it was difficult to disentangle the impact of PAM-tailored approaches from the broader interventions. Further detail about the impact of PAM-tailored interventions on quality of care is provided in online additional file 2, tables 3 and 4.
Clinician behaviours
Findings from the included studies indicated that knowing a patient’s activation level could influence the amount of time a coach or clinician spent with that patient,4 17 the type of support they provided and the effectiveness of the clinician-patient interaction.13 28 However, other studies found that using the PAM within self-management interventions had less positive effects on the ability of clinicians to deliver self-management support.20 21 30
Patient behaviours
The effect of PAM-tailored interventions on patient behaviours differed across the studies. The relevant outcomes described included health service utilisation, clinical outcomes and self-management behaviours.
Health service utilisation
Health service utilisation outcomes included ED use, and hospital admissions. Studies assessing ED use reported that PAM-tailored interventions either reduced patient ED use4 23–25 or showed insignificant findings.11 30 Declines in hospital inpatient admissions,4 24 25 patient readmissions25 and hospital days34 were also reported. One study30 found 30-day readmissions were significantly higher in the intervention group. However, the significance of this difference was not maintained over time.
Clinical indicators
Four studies using PAM-tailored interventions reported on patient clinical indicators. These included low-density lipoprotein, hemoglobin A1C and blood pressure B-type natriuretic peptide and urine sodium/creatinine ratio. Significant improvements in clinical indicators were found in some studies, suggesting the possibility of associated changes to health behaviours by patients.4 23 28 However, the findings from this small group of studies also included insignificant results or no improvements to clinical indicators.4 28 30
Self-management behaviours
The reported study outcomes relevant to patient self-management included behaviours such as medication adherence, exercise, diet and self-weigh. Findings about the effect of PAM-tailored interventions on self-management behaviours were variable. While one study reported increased patient adherence to recommended immunisations and drug regimens in the intervention group,4 a second study found that the intervention was not significantly associated with medication adherence.28 The findings from Young et al 30 showed that intervention group patients self-reported improvements in self-management behaviours and greater increases in self-efficacy for heart failure self-management. However, the patients’ clinical outcomes did not reflect these changes. Improvements in PAM scores were consistently identified in studies where the PAM was used to measure the effect of an intervention on patient activation.24 25 27 30
Discussion
This review identified a range of interventions for patients with chronic disease where PAM results were used to tailor the activities or support provided to the patient according to their level of activation. Examples of these interventions included care coordination, health coaching, self-management interventions and in-home/hospital outreach programmes. Most studies describing PAM-tailored interventions were conducted in the USA. The PAM-13 survey has been translated, and validated, into multiple languages.26 However, very few of the included studies described use of these translated versions within PAM-tailored interventions for patients with chronic disease, or discussed the challenges associated with completing the PAM with patients from culturally and linguistically diverse (CALD) backgrounds. Additionally, we did not identify any studies that described interventions specifically aiming to reach minority groups. These findings may imply the presence of challenges or barriers to using the PAM with patients from CALD backgrounds or minority groups, and highlights an area for further research. It is possible that the PAM has been used among these patient groups as an outcome measure for interventions rather than as part of a PAM- tailored intervention.
The identified enablers and barriers to the implementation of PAM-tailored interventions highlight the challenges associated with organisational, clinician and patient perspectives and understanding about the meaning, value and use of the PAM. Multiple interventions and approaches to tailoring care were identified, suggesting that using the PAM for this purpose may be more complex and less understood than as an outcome measure. The PAM tool is not disease-specific and can be used across different patient groups.26 However, its broad and inclusive nature may limit the relevance and usefulness of the results to patients and clinicians if they are not specific enough to patients’ needs.20 21 These findings suggest that questions exist about the role and value of the PAM in improving quality of care.
Normalisation process theory may provide some explanation to some of the identified enablers and barriers to implementing the PAM, through its emphasis on considering the implementation, normalisation and sustainability of complex interventions in practice, during their development.35 A tool or intervention, such as the PAM, may be established as valid and effective, but its value and the likelihood of normalisation into practice can be influenced by contextual factors including the coherence and understanding participants have about the intervention, and their commitment to and engagement in implementation.35 The success of any new tool or intervention depends on its coherence and feasibility to those who are implementing it. The need for clarity and understanding about the purpose and value of the PAM in the clinical context and for the patient group(s) with whom it is being used, was highlighted by Armstrong et al 26 in their description of the ‘tension’ experienced between implementing the PAM as a validated tool, and as a method of tailoring care. The importance of a standardised process for implementation to ensure a valid PAM score was emphasised to clinicians. However, in practice this was often compromised for alternative approaches where patients and clinicians discussed the concept and meaning of patient activation.26 This tension is a relevant consideration when developing and implementing PAM-tailored interventions. While the PAM ‘has a broad range of potential uses and functionality in the context of person-centred care’, it is important to ensure that the use of PAM-generated data is well-defined, and the administration process is appropriate to this purpose.33 Using the PAM to tailor care may demand more flexible administration approaches in clinical settings, than when it is used as an outcome measure for an intervention.33 Further research is needed to enhance our understanding about the PAM’s role and value in tailoring interventions. A qualitative assessment of the PAM, exploring themes such as perceived usefulness by the patient and provider, fit with existing practice and effective methods of administration would be useful to providers and researchers.
PAM-tailored interventions may have the potential to improve patient behaviours, with some intervention studies demonstrating positive changes to self-management behaviours and health service utilisation. Three studies indicated general improvements in clinical outcomes.4 23 28 However, the small number of studies measuring clinical outcomes, and the lack of consistency in the findings across the outcomes measured, limit the extent to which we can make generalisations about the clinical benefits of PAM-tailored interventions. Further studies of PAM-tailored interventions that specifically investigate improvements in clinical indicators and the extent of variation between these will further help to identify the clinical conditions and settings that may benefit from sustained, routine use of PAM. Improvements in patients’ PAM scores were found across the intervention studies that used the PAM as an outcome measure. While not conclusively demonstrated in this group of studies, this finding points towards the potential for PAM-tailored interventions to positively affect patient behaviours and health outcomes. Our findings regarding the impact of PAM-tailored interventions on clinician behaviours and the quality of care provided to patients were varied and limited. There appears to be potential for the PAM to prompt and facilitate changes to how clinicians engage with patients and provide support. However, our findings suggest a better understanding about the concept of patient activation is needed for the PAM to be used effectively in tailoring interventions.
The value of the PAM is about facilitating patient behaviour change and improving health outcomes. Success in achieving these aims also requires a shift in the culture, attitudes and perceptions of clinicians towards person-centred care and concepts such as patient activation and self-management. Greene et al found that clinicians of patients who demonstrated greater improvement in activation reported using strategies to support patient behaviour change, such as emphasising patient ownership over their healthcare, and working in partnership with patients on goal setting and problem solving. Clinicians of patients who showed less improvement were less likely to report using these approaches.36 Improving patient activation and enhancing self-management requires a re-evaluation of how patient’s and clinician’s roles in healthcare are understood. Tailoring care may result in greater improvements in activation across all patients. Tailoring care may also mean that interactions between clinicians and patients are less frustrating because care is harmonised to the patient’s activation level. Clinicians and teams can work alongside patients, rather than against them. Clinical practice is difficult enough without pushing patients in ways they do not feel ready or equipped for. Understanding levels of activation may allow the clinician to work more efficiently and effectively in supporting the patient towards their self-care goals. While further research is needed, the approaches and strategies used by clinicians to support patient behaviour change, and how they shape the clinician-patient interaction, seem to influence patient activation. The PAM is one example of a tool that could be used to encourage and enable clinicians to take a more person-centred approach to patient care. The literature also describes the potential benefits of the PAM in improving clinician and patient satisfaction.37 It would be useful to further explore how the PAM may be used to facilitate cultural and attitudinal changes among clinicians in ways that can improve the quality of patient care.
Limitations
There are number of limitations to this scoping review. First, neither the quality of the studies nor the interventions were assessed and this should be taken into account when considering the strength of the results from the included studies. Similarly, no analysis of bias was undertaken. A limited number of studies were included in the analysis, and all the intervention papers were conducted in the USA or the UK. These factors, combined with a lack of diversity among the linguistic, cultural and demographic background of the patients in the studies, should be acknowledged when considering the applicability of the findings to other contexts. Finally, few papers discussed patient-level enablers and barriers to implementation of the PAM, and those enablers and barriers that were identified were not always taken from patient-level data or the patient perspective and experience.
Conclusion
The PAM is being used to tailor and differentiate care for patients with chronic conditions, within a variety of interventions. The use of PAM as a tailoring tool does not appear to be widespread outside the USA and the UK, or among patients from CALD backgrounds. From the clinician perspective, improved understanding about the purpose and value of using the PAM to tailor interventions, alongside well-defined administration processes that allow for the flexibility required to appropriately inform patient care, are two key factors that could enable the implementation of the PAM-tailored interventions in clinical settings. The effect of PAM-tailored interventions on clinician and patient behaviours was difficult to determine from this review. The role of PAM-tailored interventions in facilitating cultural and attitudinal change among clinicians, and improving the quality of patient care, are potential areas of focus for future research.
Acknowledgments
The authors would like to acknowledge the reviewers of this paper for their contribution to enhancing the paper.
Footnotes
Twitter: @ben_hr
Contributors: RK contributed to the development of the review questions, conducting the literature searches, reviewing the papers, data extraction, analysis of the results, and drafting the manuscript. BH-R supervised the project, contributed to the development of the manuscript, and contributed to the interpretation of findings. JMcD was responsible for the initial project concept and design and contributed to the review of literature and interpretation. HJS assisted with conducting the review, and the development of the manuscript. SD contributed to the study design and provided input on the manuscript development. MH contributed to the study design and review questions and reviewed the paper.
Funding: This project received funding from South Eastern Sydney Local Health District.
Disclaimer: The funders did not have a role in conducting this scoping review. Information about the sources of funding for the included sources of evidence were not extracted from the papers.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Hibbard J, Gilburt H. Supporting people to manage their health: An introduction to patient activation [Internet. London: The Kings Fund, 2014. https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/supporting-people-manage-health-patient-activation-may14.pdf [Google Scholar]
- 2. Hibbard JH, Stockard J, Mahoney ER, et al. Development of the patient activation measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004;39:1005–26. 10.1111/j.1475-6773.2004.00269.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hibbard JH, Mahoney ER, Stockard J, et al. Development and testing of a short form of the patient activation measure. Health Serv Res 2005;40:1918–30. 10.1111/j.1475-6773.2005.00438.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hibbard JH, Greene J, Tusler M. Improving the outcomes of disease management by tailoring care to the patient’s level of activation. Am J Manag Care 2009;15:353–60. [PubMed] [Google Scholar]
- 5. Hibbard JH. Using systematic measurement to target consumer activation strategies. Med Care Res Rev 2009;66:9S–27. 10.1177/1077558708326969 [DOI] [PubMed] [Google Scholar]
- 6. Hibbard JH, Greene J, Shi Y, et al. Taking the long view: how well do patient activation scores predict outcomes four years later? Med Care Res Rev 2015;72:324–37. 10.1177/1077558715573871 [DOI] [PubMed] [Google Scholar]
- 7. Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff 2013;32:207–14. 10.1377/hlthaff.2012.1061 [DOI] [PubMed] [Google Scholar]
- 8. Greene J, Hibbard JH, Sacks R, et al. When seeing the same physician, highly activated patients have better care experiences than less activated patients. Health Aff 2013;32:1299–305. 10.1377/hlthaff.2012.1409 [DOI] [PubMed] [Google Scholar]
- 9. Lindsay A, Hibbard JH, Boothroyd DB, et al. Patient activation changes as a potential signal for changes in health care costs: cohort study of US high-cost patients. J Gen Intern Med 2018;33:2106–12. 10.1007/s11606-018-4657-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hibbard JH, Mahoney ER, Stock R, et al. Do increases in patient activation result in improved self-management behaviors? Health Serv Res 2007;42:1443–63. 10.1111/j.1475-6773.2006.00669.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shively MJ, Gardetto NJ, Kodiath MF, et al. Effect of patient activation on self-management in patients with heart failure. J Cardiovasc Nurs 2013;28:20–34. 10.1097/JCN.0b013e318239f9f9 [DOI] [PubMed] [Google Scholar]
- 12. Deen D, Lu W-H, Rothstein D, et al. Asking questions: the effect of a brief intervention in community health centers on patient activation. Patient Educ Couns 2011;84:257–60. 10.1016/j.pec.2010.07.026 [DOI] [PubMed] [Google Scholar]
- 13. Hibbard J. Motivating the unmotivated client. Care Manag 2016;22:9–12. [Google Scholar]
- 14. Deeny S, Thorlby R, Steventon A. Briefing: Reducing emergency admissions: unlocking the potential of people to better manage their long-term conditions [Internet]. The Health Foundation, 2018. Available: https://www.health.org.uk/sites/default/files/Reducing-Emergency-Admissions-long-term-conditions-briefing.pdf [Accessed 26 Mar 2020].
- 15. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 16. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Armstrong N, Tarrant C, Martin G, et al. Independent evaluation of the feasibility of using the Patient Activation Measure in the NHS in England: Early findings [Internet]. The Health Foundation, 2015. https://www.england.nhs.uk/wp-content/uploads/2015/11/pam-evaluation.pdf [Google Scholar]
- 18. The Health Foundation . The Health Foundation [Internet]. Available: https://www.health.org.uk/
- 19. Insignia Health . Research studies [Internet]. Available: https://www.insigniahealth.com/research/archive/
- 20. Kidd L, Lawrence M, Booth J, et al. Tailored stroke self-management: developing and testing a nurse-led, self-management support intervention (TALISSMAN) [Internet], 2013. Available: https://www.researchgate.net/publication/258448209 [Accessed 9 Mar 2016].
- 21. Kidd L, Lawrence M, Booth J, et al. Development and evaluation of a nurse-led, tailored stroke self-management intervention. BMC Health Serv Res 2015;15:359. 10.1186/s12913-015-1021-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Linden A, Butterworth SW, Prochaska JO. Motivational interviewing-based health coaching as a chronic care intervention. J Eval Clin Pract 2010;16:166–74. 10.1111/j.1365-2753.2009.01300.x [DOI] [PubMed] [Google Scholar]
- 23. Blash L, Dower C, Chapman S. PeaceHealth’s team fillingame uses patient activation measure to customize the medical home [Internet]. San Franscisco: Center for the Health Professions, University of California, 2011. https://healthforce.ucsf.edu/sites/healthforce.ucsf.edu/files/publication-pdf/10.1%202011_05_PeaceHealth%27s_Team%20Fillingame_Uses_Patient_Activation_Measures_to_Customize_the_Medical_Home.pdf [Google Scholar]
- 24. Castillo DJ, Myers JB, Mocko J, et al. Mobile integrated healthcare: preliminary experience and impact analysis with a Medicare advantage population. J Health Econ Outcomes Res 2016;4:172–87. 10.36469/9819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Roeper B, Mocko J, O'Connor LM, et al. Mobile integrated healthcare intervention and impact analysis with a Medicare advantage population. Popul Health Manag 2018;21:349–56. 10.1089/pop.2017.0130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Armstrong N, Tarrant C, Martin G, et al. Independent evaluation of the feasibility of using the patient activation measure in the NHS in England: final report. University of Leicester/The Health Foundation, 2017. [Google Scholar]
- 27. Houlihan BV, Brody M, Everhart-Skeels S, et al. Randomized trial of a Peer-Led, Telephone-Based Empowerment intervention for persons with chronic spinal cord injury improves health self-management. Arch Phys Med Rehabil 2017;98:1067–76. 10.1016/j.apmr.2017.02.005 [DOI] [PubMed] [Google Scholar]
- 28. Reistroffer C, Hearld LR, Szychowski JM. An examination of the relationship between care management with coaching for activation and patient outcomes. Am J Manag Care 2017;23:123–8. [PubMed] [Google Scholar]
- 29. Young L, Barnason S, Do V. Promoting self-management through adherence among heart failure patients discharged from rural hospitals: a study protocol. F1000Res 2015;3:317. 10.12688/f1000research.5998.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Young L, Hertzog M, Barnason S. Effects of a home-based activation intervention on self-management adherence and readmission in rural heart failure patients: the PATCH randomized controlled trial. BMC Cardiovasc Disord 2016;16:176. 10.1186/s12872-016-0339-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kamajian S. Patient activation for population health: shifting from a fee-for-service model toward a proactive, preventive approach with increased engagement. Osteopath Fam Physician 2014;6:28–31. [Google Scholar]
- 32. Hibbard JH. Patient activation and the use of information to support informed health decisions. Patient Educ Couns 2017;100:5–7. 10.1016/j.pec.2016.07.006 [DOI] [PubMed] [Google Scholar]
- 33. Chew S, Brewster L, Tarrant C, et al. Fidelity or flexibility: an ethnographic study of the implementation and use of the patient activation measure. Patient Educ Couns 2018;101:932–7. 10.1016/j.pec.2017.12.012 [DOI] [PubMed] [Google Scholar]
- 34. Langel SJ. Pioneering new ways to engage the disabled. Health Aff 2013;32:215. 10.1377/hlthaff.2013.0027 [DOI] [PubMed] [Google Scholar]
- 35. Murray E, Treweek S, Pope C, et al. Normalisation process theory: a framework for developing, evaluating and implementing complex interventions. BMC Med 2010;8:63. 10.1186/1741-7015-8-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Greene J, Hibbard JH, Alvarez C, et al. Supporting patient behavior change: approaches used by primary care clinicians whose patients have an increase in activation levels. Ann Fam Med 2016;14:148–54. 10.1370/afm.1904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Santana M-J, Feeny D. Framework to assess the effects of using patient-reported outcome measures in chronic care management. Qual Life Res 2014;23:1505–13. 10.1007/s11136-013-0596-1 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ihj-2019-000032supp001.pdf (62.8KB, pdf)
ihj-2019-000032supp002.pdf (196.3KB, pdf)