Extract
Increased age is a strong risk factor for mortality in patients with coronavirus disease 2019 (COVID-19) [1, 2]. Risk of death increases 1.5 times for every 10 years [1]. Among the 3.4 million people who died worldwide up to May 2023 from COVID-19, 2.4 million (71%) were people older than 65 years [3].
Tweetable abstract
Increased age is a strong risk factor for mortality in patients with COVID-19. Understanding the dynamic changes in plasma biomarkers associated with age is crucial for unravelling the intricate interplay between ageing, immune response and outcomes. https://bit.ly/3BWgSjP
Increased age is a strong risk factor for mortality in patients with coronavirus disease 2019 (COVID-19) [1, 2]. Risk of death increases 1.5 times for every 10 years [1]. Among the 3.4 million people who died worldwide up to May 2023 from COVID-19, 2.4 million (71%) were people older than 65 years [3].
In this issue of the European Respiratory Journal, Michels et al. [4] assessed the association between age, host response and 30-day mortality in patients with COVID-19. This study offers valuable insights that can significantly contribute to the development of targeted interventions for COVID-19 patients. The study included 464 patients stratified into age groups (<50, 50–60, 60–70 and ≥70 years). Among them, 89 patients (19.2%) were younger than 50 years, 111 (23.9%) were between 50 and 60 years, 135 (29.1%) were between 60 and 70 years, and 129 (27.8%) were 70 years or older. The researchers examined 43 biomarkers associated with alterations in four domains related to the pathophysiological mechanisms of COVID-19: endothelial cell and coagulation activation; inflammation and organ damage; cytokine release; and chemokine release.
Understanding the dynamic changes in plasma biomarkers associated with age is crucial for unravelling the intricate interplay between ageing, immune response and outcomes. The study findings demonstrate distinct patterns of biomarkers across four different age groups. Ageing was associated with elevation of biomarkers reflecting greater activation of the endothelium, coagulation system, inflammation and organ damage. Alterations in cytokines and chemokines were mixed. Some cytokines increased with age, while others remained at a similar level. In addition, some chemokine levels increased with age, while others decreased. Mediation analysis showed that several biomarkers explained part of the age-related increased in 30-day mortality. The strongest mediators were soluble thrombomodulin, soluble tumour necrosis factor receptor 1 (sTNF-R1) and soluble triggering receptor expressed on myeloid cells 1 (sTREM-1). Each explained approximately 13% of the age effect on mortality.
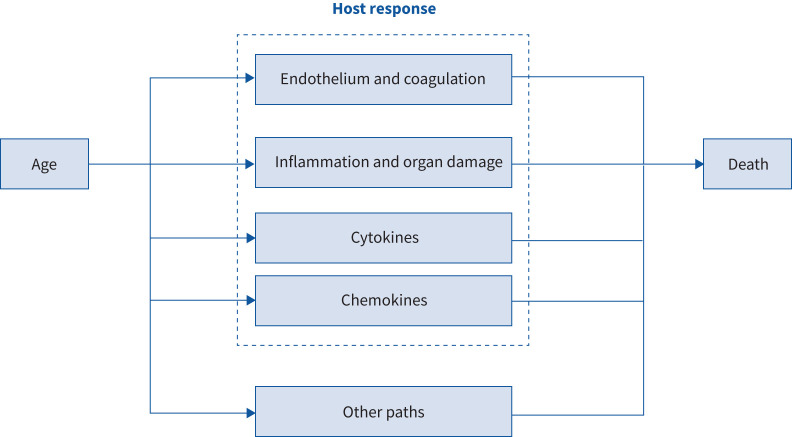
The study reported by Michels et al. [4] has several distinctive strengths. First, the authors sought to provide insights into the causal pathways linking age, host response and mortality in COVID-19. The analysis was based on pre-specified causal models, considering that in patients with COVID-19, there might be age-related effects on the host response, which in turn would affect mortality (figure 1). The mediation models were then adjusted accordingly. Second, a substantial number of biomarkers reflecting four pathophysiological domains were assessed: endothelial cell and coagulation activation; inflammation and organ damage; cytokines; and chemokines. Third, missingness was minimal. Fourth, the methods were sophisticated and complex, denoting thoughtful planning and were described in rich detail. Fifth, statistical analysis was rigorous with methods deployed to mitigate type I error inflation due to multiple hypothesis testing. Additionally, associations were validated in two independent cohorts (157 critically ill patients and 196 non-intubated patients) to ensure that associations were consistent and likely to be generalisable.
FIGURE 1.
Physio-pathological mechanisms of age, host response and mortality in COVID-19.
Another nice feature of the study is the practice of routinely storing plasma obtained from leftover blood from clinical care in two participant institutions. This practice might facilitate conduction of research involving biological samples without the need for study-specific blood sampling.
The study has substantial implications for future research because it presents a number of potential COVID-19 age-specific mechanisms. First, older COVID-19 patients present with more profound endotheliopathy, which may contribute to coagulation activation. For example, the markers of endotheliopathy soluble thrombomodulin and soluble vascular cellular adhesion molecule-1 were significant mediators of age-related mortality. Would these biomarkers be useful in predicting a beneficial effect of anticoagulation in elderly patients with COVID-19? Second, sTNF-R1 and sTREM-1 were mediators that explained part of the ageing-driven increase in mortality. Would inhibition of these pathways be beneficial for older patients? Fourth, interleukin (IL)-6 was not found to mediate age-related mortality in COVID-19, suggesting that IL-6 blockade may not be effective for older patients. The limitations of the study are well discussed by the authors. Most relevant is that findings do not imply definitive causal relationships because of the observational nature of the study. Additionally, the mediation analyses consider one mediator of age-related COVID-19 at a time; therefore, the results do not reflect the effect of each mediator adjusting for the effect of others.
Overall, this study offers valuable contributions to the development of targeted interventions and improved personalised patient management strategies for COVID-19.
Shareable PDF
Footnotes
Conflict of interest: The authors have no potential conflicts of interest to disclose.
References
- 1.Kartsonaki C, Baillie JK, Barrio NG, et al. . Characteristics and outcomes of an international cohort of 600 000 hospitalized patients with COVID-19. Int J Epidemiol 2023; 52: 355–376. doi: 10.1093/ije/dyad012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Romero Starke K, Reissig D, Petereit-Haack G, et al. . The isolated effect of age on the risk of COVID-19 severe outcomes: a systematic review with meta-analysis. BMJ Glob Health 2021; 6: e006434. doi: 10.1136/bmjgh-2021-006434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Date last assessed: 11 May 2023. https://covid19.who.int/
- 4.Michels EHA, Appelman B, de Brabander J, et al. . Age-related changes in plasma biomarkers and their association with mortality in COVID-19. Eur Respir J 2023; 62: 2300011. doi: 10.1183/13993003.00011-2023 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This one-page PDF can be shared freely online.
Shareable PDF ERJ-00796-2023.Shareable (224.3KB, pdf)