Abstract
Objective
To map and explore existing evidence on the use of digital technology to deliver healthcare services with explicit consideration of health inequalities in UK settings.
Methods
We searched six bibliographic databases, and the National Health Service (NHS) websites of each UK nation (England, Scotland, Wales, Northern Ireland). Restrictions were applied on publication date (2013–2021) and publication language (English). Records were independently screened against eligibility criteria by pairs of reviewers from the team. Articles reporting relevant qualitative and/or quantitative research were included. Data were synthesised narratively.
Results
Eleven articles, reporting data from nine interventions, were included. Articles reported findings from quantitative (n = 5), qualitative (n = 5), and mixed-methods (n = 1) studies. Study settings were mainly community based, with only one hospital based. Two interventions targeted service users, and seven interventions targeted healthcare providers. Two studies were explicitly and directly aimed at (and designed for) addressing health inequalities, with the remaining studies addressing them indirectly (e.g. study population can be classed as disadvantaged). Seven articles reported data on implementation outcomes (acceptability, appropriateness, and feasibility) and four articles reported data on effectiveness outcomes, with only one intervention demonstrating cost-effectiveness.
Conclusions
It is not yet clear if digital health interventions/services in the UK work for those most at risk of health inequalities. The current evidence base is significantly underdeveloped, and research/intervention efforts have been largely driven by healthcare provider/system needs, rather than those of service users. Digital health interventions can help address health inequalities, but a range of barriers persist, alongside a potential for exacerbation of health inequalities.
Keywords: Scoping review, digital technology, delivery of health care, health inequities, disadvantaged populations, United Kingdom
Introduction
The need for health systems worldwide to adapt to the restrictions brought about by the response to the COVID-19 pandemic has prompted an unprecedented acceleration of digital healthcare provision. 1 These experiences have highlighted the benefits of embedding digital technologies in healthcare delivery, which have the potential to radically reshape the health services landscape if carried forward and built upon. However, the COVID-19 pandemic has also brought to the fore previously existing digital inequalities and exacerbated their health implications, particularly for those groups in society who were already most adversely affected by health inequalities, such as homeless people or people living with disabilities.2–6
The concept of digital inequalities differs from what is known as the digital divide, which focuses on people's ability to access digital technologies and the differences between those who are connected and those who are not. Conversely, digital inequality refers to how people of different backgrounds incorporate the digital world into their lives; how their digital and social contexts, their skills and their uses differ, and how the life outcomes associated with these differences vary. 7 Therefore, the concept of digital inequality suggests that inequalities are not just a question of access to digital technologies but also stem from different ways of using and engaging with the digital world, and that inequalities would persist beyond issues of access.
Recent calls for digital technologies, or the digital ecosystem, to be recognised as a new determinant of health8,9 highlight the increasingly important interplay between digital inequalities and health outcomes, as well as the growing need to enable a more consistent understanding and measurement of these effects. Following the experiences during COVID-19 restrictions, the issue of whether future models of healthcare delivery should by default rely more heavily on digital technologies has received increasing attention in practice, research and policy debates.10–12 However, alongside acknowledging opportunities for improvement, clinicians and researchers have also warned about several important risks that such shift could bring, 11 including risks to health equity and digital inclusion. In this context, it is therefore crucial to better understand the experiences and impact of digital health interventions for those most adversely affected by health inequalities. This understanding could help ensure that advances in digital health are not at the expense of widening health inequalities.
The aim of this scoping review was to map and explore the evidence available on the use of digital technology to deliver healthcare services with an explicit focus on or consideration of health inequalities in any healthcare setting within the UK.
The concept of ‘health inequalities’ can be comprehensively defined as the systematic, avoidable and unfair differences in health outcomes that can be observed between populations, between social groups within the same population, or as a gradient across a population ranked by social position. 13
For the purpose of this review, we used the term ‘disadvantaged populations’ to refer to those most at risk of being adversely affected by the intersection of digital inequalities and health inequalities. This included population groups with protected characteristics in the UK by the Equality Act 2010 14 (e.g. age, disability and race) as well as those generally recognised as being at increased risk of digital exclusion (e.g. those with a low income, homeless people and rural/remote communities).
Whilst previous reviews with a similar focus have been conducted globally, to our knowledge, this is the first review UK-based evidence on the use of digital technology to deliver healthcare services, with an explicit focus on or consideration of health inequalities at study population level, regardless of intervention type and healthcare setting. Previous reviews in the UK have adopted slightly different emphases, by either focusing on global evidence and excluding certain intervention types such as digital medical devices, 15 or targeting specific healthcare settings such as general practice. 16
Methods
This scoping review was undertaken following the JBI scoping review methodology,17,18 and is reported in keeping with the PRISMA extension for Scoping Reviews (PRISMA-ScR). 19
Search strategy
We searched six biographic databases: MEDLINE, CINAHL Plus, PsycINFO, Web of Science (core collection), SCOPUS and The Cochrane Library (CDSR database). Searches were conducted in May 2021 using combinations of index terms and free text words relating to disadvantaged populations, digital health services and interventions, and health inequalities. A sample search strategy for MEDLINE is provided as supplementary material (Supplemental file 1). The National Health Service (NHS) website of each UK nation (England, Scotland, Wales and Northern Ireland) were hand searched. Reference lists of all included studies and relevant systematic reviews identified were scanned for eligible studies.
Eligibility criteria and study selection
Studies of any research design were eligible for inclusion, including quantitative, qualitative and mixed-methods studies. Restrictions were applied on publication date (2013–2021) and publication language (English). Studies were included if they reported the use of digital technology to deliver health care services with an explicit focus on or consideration of health inequalities, in any context/setting within the UK. Studies were included if they reported the impact of digital health interventions on any disadvantaged populations in any setting within the UK. Studies were included if they focused on population groups with protected characteristics in the UK by the Equality Act 2010 14 (e.g. age, disability and race) or who are generally recognised as being at increased risk of digital exclusion (e.g. those with a low income, homeless people, rural/remote communities).
Studies were excluded if they focused on population groups defined solely by a specific pre-existing medical condition (e.g. heart disease and mental ill health) which was not associated with a protected characteristic (e.g. age, disability and race). Studies were excluded if they were based in non-UK settings. Studies published in languages other than English were excluded. Studies published before 2013 were excluded to ensure that included interventions reflected the most up-to-date technologies. Review articles were excluded but used for reference checking to identify any additional, potentially relevant studies eligible for inclusion.
Titles, abstracts and relevant full texts were independently screened against the eligibility criteria by randomly assigned pairs of reviewers from the authorship group. Any disagreements between reviewers were resolved through discussion and consultation with a third reviewer or by consensus in wider team meetings.
Data extraction
Data extraction was undertaken independently by randomly assigned pairs of reviewers from the authorship group using a piloted data extraction form. Any discrepancies between reviewers were resolved through team discussion and/or in consultation with a third reviewer.
Data synthesis
Data were synthesised narratively, given that any pooled quantitative or qualitative analyses were considered inappropriate due to the broad range of interventions, study types and populations included in this review. Data extracted from included articles were categorised into three sets of categories to address our scoping review aims, based on (1) the types of interventions reported in the included studies; (2) the range of approaches employed to address health inequalities; and (3) the types of evaluations used to examine the impact of, and/or the perceptions about, the included interventions.
Intervention descriptions were coded and mapped against the World Health Organization's classification of digital health interventions, 20 which provides a taxonomy of the different ways in which digital/mobile technologies are used to support health system needs and proposes a shared language to describe the uses of digital technology for healthcare provision.
Any approaches to address health inequalities reported in the included articles were coded and categorised according to whether they explicitly stated to address health inequalities or used any health inequalities conceptual frameworks at study design and/or at intervention development/implementation level.
Finally, study findings reported in the included articles were coded and categorised according to whether they evaluated implementation or effectiveness outcomes, and the findings summarised. Initial coding was undertaken by the lead author and then critically reviewed by the rest of the team. Further revision and refining of the coding and categorisation of included studies was then collectively undertaken by the team at regular meetings held throughout the data synthesis process.
Results
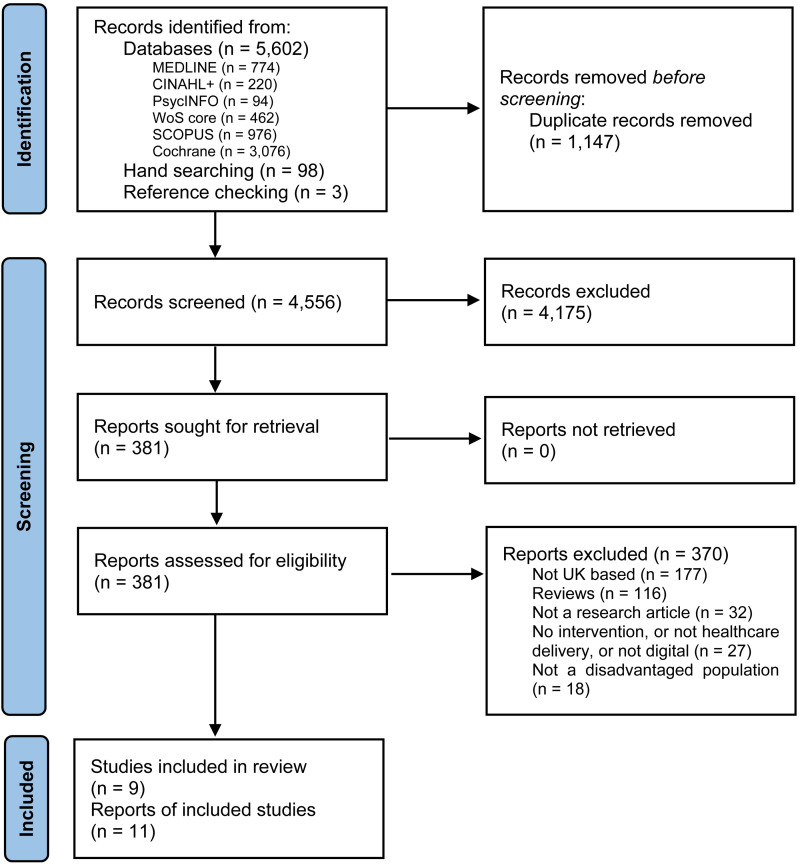
Systematic searches in bibliographic databases yielded 5602 records. A further set of 98 records were identified from hand searches in websites and grey literature sources, and 3 further records were identified through reference screening of relevant reviews identified. After deduplication, a final set of original records were assessed against the eligibility criteria. Title and abstract screening resulted in 381 records considered eligible or inconclusive. Full-text articles were then retrieved and assessed for eligibility, resulting in 11 articles reporting data from 9 interventions being included in the final synthesis (Figure 1).
Figure 1.
PRISMA flow diagram. From: Page et al. 42
Summary of included studies
Five articles21–25 reported findings from quantitative studies (including three randomised controlled trials,21,22,24 one comparative before/after study 25 and one cross-sectional study 23 ); five more articles26–30 reported findings from qualitative studies (all interview studies); and one article 31 reported findings from a mixed-methods study (combining quantitative routine data and qualitative interviews). Study settings were mainly community-based22–24,26–31 with only one intervention based in a hospital setting. 21 A summary of key characteristics of included articles is presented in Table 1.
Table 1.
Key characteristics of included articles.
| Paper | Methodology | Study design | Setting | Population(s) at risk | Sample size | Intervention group sample size | Control group sample size | Intervention | Study aim |
|---|---|---|---|---|---|---|---|---|---|
| Akobeng (2015) | Quantitative | Randomised controlled trial | Hospital | Young people (aged 8–16 years) with inflammatory bowel disease (IBD) living at long distances from regional centres | 86 | 44 | 42 | Remote outpatient consultations | To evaluate effectiveness and cost consequences of the intervention compared to face-to-face consultations |
| Crombie (2018) | Quantitative | Randomised controlled trial | Community | Men from areas classified as being in the most disadvantaged quintile | 825 | 411 | 414 | Text messaging intervention | To evaluate effectiveness and cost-effectiveness of the intervention compared to attentional control text messages on general health topics |
| Hughes (2020) | Mixed-methods | Routine data (quant) and interviews (qual) | Community | Patients categorised as ‘high risk’ and ‘vulnerable’ by NHSE | 781 (quant) 16 (qual) |
- | - | Daily digitally supported conversations | To explore compliance with the intervention aims and assess the experiences of those involved |
| Latif (2019a) | Quantitative | Before/after questionnaire | Community | Marginalised or medically under-served groups |
96 | 62 | 34 | Digital (web-based) education |
To evaluate whether a digital educational intervention could improve staff intention to engage with marginalised groups |
| Latif (2019b) | Qualitative | Interviews | Community | 32 | - | - | To investigate the impact of a novel digital educational intervention (e-learning resource) to improve access in one NHS-funded community pharmacy service known as ‘Medicines Use Reviews’ (MURs) | ||
| Rixon (2017) | Quantitative | Randomised controlled trial | Community | Older primary care patients with chronic obstructive pulmonary disease | 447 | 275 | 172 | Telehealth monitoring devices | To evaluate the effectiveness of the intervention on patients’ quality of life |
| Tuijt (2021) | Qualitative | Interviews | Community | Older people living with dementia and their carers | 46 | - | - | Remote primary care consultations | To understand the remote healthcare experiences of patients living with dementia and their family carers during the COVID-19 pandemic |
| Turnbull (2020) | Qualitative | Interviews | Community | People with type 2 diabetes (T2D) from low-income and ethnic minority populations | 21 | - | - | Digitally supported chronic condition self-care | To explore how adult users talk about their use of digital interventions for self-management of T2D by examining how they spoke about their identity in relation to their technology use and their illness |
| Turnbull (2021) | Qualitative | Interviews | Community | - | - | To explore how and why people with T2D access and use digital health technologies to help them manage their condition and how experiences vary between individuals and social groups | |||
| Vereenooghe (2017) | Qualitative | Interviews | Community | People with an intellectual disability | 6 | - | - | Digital delivery of psychological therapy | To identify the (a) functions and benefits, (b) challenges and barriers, and (c) required design features of computers in therapy for people with intellectual disability |
| Walters (2017) | Quantitative | Feasibility study, questionnaires | Community | Older people | 454 | - | - | Multi-dimensional Risk Appraisal for Older people (MRA-O) system | To test the feasibility and costs of using HRA-O and SWISH tools combined into a MRA-O |
Intervention types and functionalities
Two studies24,28,29 related to interventions targeting service users, and seven studies21–23,26,27,30,31 related to interventions targeting healthcare providers.
Interventions for service users
Targeted service user communication: One study 24 developed and evaluated an intervention using mobile phones to deliver a series of interactive text messages to reducing binge drinking in disadvantaged men from areas of high deprivation. The intervention's primary digital functionality was to transmit targeted alerts and reminders to service users, relying on information systems from primary care (general practice registers) and a Short Message Service system.
Personal health tracking: One study28,29 explored users’ experiences of a set of digital health interventions whose main digital functionality was to enable self-monitoring of health/diagnostic data by service users. The study focused on examining the experiences of those in lower-income neighbourhoods and Black, Asian, and Minority Ethnic groups. The range of interventions used by participants included wearable trackers, mobile apps and web-based tools to enable type 2 diabetes patients to develop self-care expertise, all of them being user-owned and user-managed devices or applications either supplied by health providers or purchased privately.
Interventions for healthcare providers
Healthcare provider decision support: One study 23 adapted and feasibility tested a computer-aided Multi-dimensional Risk Appraisal for Older people (MRA-O) system, comprising: (1) postal questionnaire including health, lifestyle, social and environmental domains; (2) software system generating a personalised feedback report with advice on health and wellbeing; (3) follow-up of people with new concerning or complex needs by general practitioners or practice nurses. The intervention's main digital functionality was to enable healthcare providers to screen service users by risk or other health status, relying on linking the intervention with general practices health records. Key health system challenges addressed by this intervention related primarily to the ‘accountability’ domain, as well as the ‘information’ provision and service ‘utilisation’ domains.
Telemedicine interventions: Four interventions21,26,30,31 focused on delivering consultations between remote service users and healthcare providers: The first study 21 evaluated an intervention targeting young people with inflammatory bowel disease (IBD) living at long distances from a regional paediatric referral centre, using telephone-based outpatient consultations delivered by gastro-enterology doctors; the second study 26 examined the experiences of online provision of psychological therapies for people with intellectual disabilities; a third study 31 evaluated an intervention based on telephone conversations delivered by medical students for populations categorised as ‘high risk’ and ‘vulnerable’ to COVID-19 infection in a rural primary care setting; and the fourth study 30 examined the implications of remote primary care consultations (mainly telephone-based but also including video consultations) for older people living with dementia and/or their carers during the COVID-19 pandemic.
Another telemedicine intervention 22 focused on enabling remote monitoring of service user health/diagnostic data by healthcare providers. The intervention used peripheral devices for older patients with chronic obstructive pulmonary disease (COPD) (pulse oximeter with/without blood pressure monitor, weight scales and additional peripherals depending on clinical need) which were attached to a home monitoring system to allow questions and educational messages to be transmitted to participants.
Healthcare provider training: One study25,27 developed and evaluated the impact of a co-produced digital education intervention (e-learning resource comprising videos, interactivities and self-assessments) for community pharmacy professionals, including: discovering and understanding underserved communities; exploring the medicine experiences and needs of patients who are underserved; and effectively interacting and engaging patients who are underserved. The intervention's main digital functionality was to provide training content to healthcare providers, relying on a self-developed learning and training system.
Strategies used to address health inequalities
Table 2 summarises the strategies to address health inequalities identified in the included articles.
Table 2.
Strategies used to address health inequalities.
| Strategies to address health inequalities reported in included articles | Included studies | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Akobeng (2015) | Crombie (2018) | Hughes (2020) | Latif (2019a, 2019b) | Rixon (2017) | Tuijt (2021) | Turnbull (2020, 2021) | Vereenooghe (2017) | Walters (2017) | ||
| At study design level |
Study aims/objectives or tailored study components (e.g. sampling) explicitly addressing health inequalities | ⬤ | ⬤ | |||||||
| Use of any health inequalities concepts/frameworks to inform data collection/analysis methods | ⬤ | ⬤ | ⬤ | ⬤ | ⬤ | |||||
| Targeted study population that can be classed as ‘disadvantaged’ or at risk of health inequalities | ⬤ | ⬤ | ⬤ | ⬤ | ⬤ | ⬤ | ⬤ | ⬤ | ⬤ | |
| At intervention level |
Intervention aims/objectives or tailored intervention components/features explicitly addressing health inequalities | ⬤ | ||||||||
| Use of any health inequalities concepts/frameworks to inform intervention development/adaptations/delivery | ⬤ | |||||||||
| Intervention specifically designed/tailored to a population that can be classed as ‘disadvantaged’ or at risk of health inequalities | ⬤ | ⬤ | ⬤ | ⬤ | ||||||
Only two studies25,27–29 were identified to be directly aimed at, and designed for, addressing health inequalities; however, only one of them25,27 related to an intervention also explicitly aimed at, and designed for, addressing health inequalities.
Three further studies22,24,30 addressed health inequalities by embedding the use of health inequalities concepts/frameworks to inform their methods (e.g. use of Index of Multiple Deprivation for sampling); however, only one of these 24 related to an intervention specifically designed/tailored to a population that can be classed as ‘disadvantaged’ or at risk of health inequalities.
The remaining four studies21,23,26,31 addressed health inequalities indirectly (i.e. without explicitly claiming to do so) by targeting study populations that could be classed as ‘disadvantaged’ or at risk of health inequalities, with only two studies23,31 relating to interventions with components specifically tailored to those populations. It is however important to note that, the two studies21,26 that did not report any specifically tailored components were both to deliver remote consultations assumed to be patient-centred in terms of content, which was by definition tailored by clinicians at the point of delivery, and therefore any further tailoring may have been considered unnecessary by study/intervention teams.
Overall, the interventions identified were largely generic (five out of nine). Only one intervention25,27 was explicitly aimed at, and designed for, addressing health inequalities. Three further interventions23,24,31 did not explicitly claim to be addressing health inequalities, but were specifically designed/tailored to a population that can be classed as ‘disadvantaged’ or at risk of health inequalities.
Intervention evaluations: implementation outcomes
Digital delivery of psychological therapy was reported as having the potential to improve therapy engagement and experiences for people with an intellectual disability. 26 Digital technologies can help this population overcome in-session communication difficulties and practise skills at home. On-screen pictures, interactive games, symbols, sign language and touch-screens are key design features to help engagement. Implementation barriers include clinician-reported difficulties relating to their own capacity/capability to access and use digital technology and fitting it into their own defined roles.
Digital educational interventions were found to increase pharmacy professionals’ awareness and motivation to engage with marginalised groups, but key structural implementation barriers (e.g. perceived excessive workload) were found to often hinder translation into practice. 27 If supported and promoted effectively by policy makers and employers, digital educational interventions have the potential to enable and facilitate ways for pharmacy professionals to better engage with marginalised groups and bring about improvements in patients’ health and medicines management.
Included studies28,29 suggest that digital interventions to help self-manage long-term conditions can exacerbate health inequalities if experiences of patients from low-income and ethnically diverse communities are not well addressed in intervention development and implementation. Low levels of digital skills and high cost of digital health interventions can also create barriers to access and use of digital interventions to support self-management of long-term conditions. 29 Personal social networks and social status can be leveraged to overcome some of these challenges, therefore, health inequalities can also be exacerbated when those resources are not present in people's lives.
Remote primary care telephone-based consultations may not be well-suited to address the needs and preferences of people living with dementia and their carers, 30 who reported to prefer face-to-face contact. Furthermore, digital and language barriers were reported to prevent older people from accessing virtual services. Remote consultations may not be a good medium for identifying and addressing new problems for people living with dementia and their carers and may limit health providers’ ability to tailor services to individual needs for these populations. However, more targeted interventions delivered as an add-on to routine primary care, such as daily calls to patients categorised as ‘high risk’ and ‘vulnerable’, 31 have the potential to provide additional practical and psychological benefits for these populations, including strengthening their links with community voluntary groups, as well as provide additional opportunities for medical education in primary care settings.
A computer-aided risk appraisal system was found to be feasible to implement for general practices, yielding useful information about health and social problems, and enabling identification of some individual needs. 23 However, participation rates in the feasibility study were particularly low for the oldest old, the poorest and ethnic minority groups, which suggests that this type of intervention may increase inequalities in access. Implementation at scale of this approach would require work to address potential exacerbation of health inequalities.
Overall, seven articles23,26–31 reported data on implementation outcomes, with reports primarily relating to issues of acceptability, appropriateness, and feasibility of digital health interventions. Of the seven articles, five reported on interventions for healthcare providers23,26,27,30,31 and two reported on interventions for service users.28,29
Intervention evaluations: effectiveness outcomes
A randomised controlled trial and economic evaluation 21 found remote consultations to be a cost-effective alternative to face-to-face consultations for the routine outpatient follow-up of children and adolescents with IBD living at long distances from regional centres. No inferiority of telephone-based versus face-to-face consultation was found in relation to improvements in quality-of-life scores (estimated treatment effect in favour of the telephone consultation group was 5.7 points, 95% confidence interval (CI) −2.9 to 14.3; p = 0.19). Telephone consultation reduced consultation time, with an estimated reduction (95% CI) of 4.3 (2.8 to 5.7) minutes in consultation times (p < 0.001); and NHS costs, with a difference of £15.71 (95% CI 11.8–19.6; p < 0.001) per patient consultation.
Another randomised controlled trial 22 showed that telehealth monitoring devices with educational messages for patients with COPD did not reduce quality-of-life nor increase psychological distress. There were small effects (p < 0.05) for improved emotional functioning and mastery over COPD at long-term follow-up (12 months) but not at short-term follow-up (4 months).
An uncontrolled, paired before-and-after survey 25 found an improving trend in pharmacy professionals’ intention to engage with marginalised groups in the short-term after participating in a digital educational intervention, with a significant increase (0.44; 95% CI 0.11 to 0.76, p = 0.009) identified in one out of five behaviours change intention constructs measured (participants’ beliefs about capabilities). However, no significant change was detected in the numbers of patients being offered a medication review.
Finally, a randomised controlled trial 24 showed that text messages to have had a modest, statistically non-significant effect on the proportion of disadvantaged men binge drinking (consuming > 8 units of alcohol) on ≥3 occasions in the previous 28 days, assessed at 12-month follow-up (odds ratio 0.79, 95% confidence interval (CI) 0.57 to 1.08). However, the trial demonstrated that it is possible to recruit and retain large numbers of disadvantaged men in a research study.
Overall, four articles21,22,24,25 reported data on effectiveness, including the following primary outcomes: quality of life,21,22 intention to engage with marginalised groups, 25 and proportion of disadvantaged men binge drinking. 24 Three studies21,22,25 evaluated interventions for healthcare providers, and one study 24 evaluated an intervention for service users.
Discussion
This scoping review sought to map and explore the evidence available on the use of digital technology to deliver healthcare services with an explicit focus on or consideration of health inequalities in UK healthcare settings. Our findings suggest that the current evidence base in this area is significantly underdeveloped, with only eleven articles (reporting on nine interventions/services) identified between 2013 and 2021.
Within this, we found that evidence on effectiveness and health outcomes for those most at risk of health inequalities in the UK is particularly limited. Only four studies21,22,24,25 were identified that contributed data on effectiveness to our synthesis, of which only one study 21 demonstrated cost-effectiveness. Therefore, it is not yet clear if digital health services in the UK work for those most at risk of health inequalities. This is particularly concerning in a potentially radically changing health services landscape, building on service delivery models developed to support COVID-19 restrictions.10–12 In this context, some interventions previously used only as add-ons to routine care (e.g. remote consultations to address geographical inaccessibility of services in rural and remote populations) could now become part of mainstream service delivery. This, in turn, makes the need to better understand the impact of digital health interventions on those most at risk of health inequalities a more fundamental, pressing issue.
The body of evidence identified in this review suggests that research so far has been largely driven by healthcare provider's needs rather than those of service users from populations most at risk of health inequalities. Similarly, the evidence on implementation outcomes identified in this review suggests that digital health interventions remain better aligned with the needs of healthcare providers than those of service users from more disadvantaged populations.
Although the evidence we identified also suggests that digital health interventions can offer promising new avenues to address health inequalities, 15 some significant structural barriers were reported to be at play across most intervention domains as well as the potential for very important unintended impacts such as the exacerbation of health inequalities.2–5
Taken together, these findings highlight the importance for future digital health research and interventions/service development efforts to meaningfully engage with disadvantaged populations, for example, drawing on philosophies such as co-production and co-design, which acknowledge that services users are best placed to advise on how services can be made more accessible to them, while also appreciating the views and needs of those responsible for service delivery.32–34
Recommendations for practice, research and policy
To avoid digital health services inadvertently widening health inequalities, investments in inclusion should be embedded into any investments in digital health.2,15 In this context, the role of implementation research in this area could be of particular importance to advance the understanding of digital health inequalities and enable successful integration of health equity into implementation models. 35 Likewise, research and interventions addressing key issues that could mitigate against the emergence of digital health inequalities can be of particular importance in this context.5,6,15 For example, interventions to facilitate access to connected devices and interventions to increase digital literacy, health literacy or digital health literacy, which for some time have shown potential to improve outcomes for populations most at risk of health inequalities.36–38 Digital-based approaches to support digital health literacy in disadvantaged populations present new opportunities that can complement traditional non-digital strategies, but existing evidence in this area is still sparse. 39 Alongside this, it is important to acknowledge the need to better understand and monitor changing patterns in the use of digital technologies and social media platforms as health support resources,15,40,41 which can in turn change the nature of digital health inequalities. This is in line with calls to consider digital technologies as a new determinant of health.8,9
To enable advances in the understanding of digital health inequalities, more theoretically informed and purposely designed interventions and studies focusing on digital health inequalities are needed. We only identified one intervention25,27 and two studies25,27–29 being directly aimed at, and designed for, addressing digital health inequalities. The remaining interventions and studies only addressed health inequalities indirectly, by either embedding key concepts/frameworks into their methods (e.g. use of Index of Multiple Deprivation for sampling) or by targeting study populations that could be classed as ‘disadvantaged’ or at risk of health inequalities. These are important gaps in the evidence available in UK settings, which is much needed to better understand the implications of digital health interventions for those most at risk of health inequalities.
Alongside this, the broad range of intervention types and functionalities identified in this review should also be considered in future research in this area, particularly in terms of better understanding how digital health inequalities align with existing health-system and information-system challenges, to inform governance and organisational changes required to enable sustainable digital health inclusion efforts at scale.
Strengths and limitations
To our knowledge, this is the first review to bring together and examine primary quantitative and qualitative research relevant to the use of digital technology to deliver healthcare services with an explicit focus on or consideration of health inequalities, in any healthcare setting within the UK. There were some limitations in our search strategy, including limits placed in publication language (only articles in English were included) and publication date (2013–2021). Also, our focus on studies examining the impact of digital interventions on disadvantaged populations carries the limitation that any studies evaluating a health-inequalities-tailored digital health intervention using a general population sample may have been missed. Follow-up review work examining this body of evidence could make an important contribution and inform advances to help achieve equitable health goals in the UK.
Conclusions
It is not yet clear if digital health interventions/services in the UK work for those most at risk of health inequalities. Our findings suggest that the current evidence base in this area is significantly underdeveloped, with only four studies identified that contributed data on effectiveness to our synthesis, of which only one study demonstrated cost-effectiveness.
So far, research and intervention/service development efforts in this area have been largely driven by healthcare provider/system needs, rather than those of service users. A key priority for future UK-based digital health research/interventions should be to meaningfully engage with disadvantaged populations to inform their approaches.
Although the current evidence suggests that digital health interventions can offer promising new avenues to address health inequalities, it also suggests that a range of barriers persist, alongside a potential for exacerbation of health inequalities. To avoid digital health services inadvertently widening health inequalities, investments in inclusion should be integral to any investments in digital health. To successfully enable this, it is paramount to address another important gap identified in this review, the scarcity of theoretically informed digital health research/interventions purposely designed to address health inequalities as an integral part of their goals. These are fundamental developments that should become normalised if we are to achieve equitable digital healthcare provision in the UK.
Supplemental Material
Supplemental material, sj-docx-1-dhj-10.1177_20552076231185442 for Exploring the use of digital technology to deliver healthcare services with explicit consideration of health inequalities in UK settings: A scoping review by Albert Farre, Mei Fang, Beth Hannah, Meiko Makita, Alison McFadden, Deborah Menezes, Andrea Rodriguez, Judith Sixsmith and Nicola M Gray in DIGITAL HEALTH
Acknowledgement
We would like to thank Dr Jordana Salma (Faculty of Nursing, University of Alberta) for her support in this review.
Footnotes
Contributorship: NG, AMcF, AF, JS, MF, AR and BH conceived the study and developed the review protocol. MM undertook the database searches. NG supervised the project's researcher and oversaw study data management. All authors were involved in screening, data extraction and data synthesis. AF wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Institute for Social Sciences Research (ISSR), University of Dundee - Interdisciplinary Incubator Grant (2021).
Guarantor: AF and NG.
ORCID iDs: Albert Farre https://orcid.org/0000-0001-8970-6146
Beth Hannah https://orcid.org/0000-0001-8751-8766
Supplemental material: Supplemental material for this article is available online.
References
- 1.Webster P. Virtual health care in the era of COVID-19. Lancet Lond Engl 2020; 395: 1180–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McAuley A. Digital health interventions: widening access or widening inequalities? Public Health 2014; 128: 1118–1120. [DOI] [PubMed] [Google Scholar]
- 3.Latulippe K, Hamel C, Giroux D. Social health inequalities and eHealth: a literature review with qualitative synthesis of theoretical and empirical studies. J Med Internet Res 2017; 19: e6731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spanakis P, Peckham E, Mathers A, et al. The digital divide: amplifying health inequalities for people with severe mental illness in the time of COVID-19. Br J Psychiatry 2021; 219: 529–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beaunoyer E, Dupéré S, Guitton MJ. COVID-19 and digital inequalities: reciprocal impacts and mitigation strategies. Comput Hum Behav 2020; 111: 106424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Kessel R, Hrzic R, O’Nuallain E, et al. Digital health paradox: international policy perspectives to address increased health inequalities for people living with disabilities. J Med Internet Res 2022; 24: e33819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hargittai E. Introduction to the handbook of digital inequality. In: Hargittai E. (ed.) Handbook of digital inequality. Cheltenham, UK; Northampton, MA: Edward Elgar Publishing, 2021, pp.1–7. [Google Scholar]
- 8.Kickbusch I, Piselli D, Agrawal A, et al. The Lancet and Financial Times Commission on governing health futures 2030: growing up in a digital world. Lancet 2021; 398: 1727–1776. [DOI] [PubMed] [Google Scholar]
- 9. The Lancet Digital Health . Digital technologies: a new determinant of health. Lancet Digit Health 2021; 3: e684. [DOI] [PubMed] [Google Scholar]
- 10.Hancock M. The future of healthcare (speech, 30th July). Lond UK Gov.
- 11.Greenhalgh T, Rosen R. Remote by default general practice: must we, should we, dare we? Br J Gen Pract 2021; 71: 149–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Horton T, Hardie T, Mahadeva S, et al. Securing a positive health care technology legacy from COVID-19. London: Health Foundation, 2021. [Google Scholar]
- 13.McCartney G, Popham F, McMaster R, et al. Defining health and health inequalities. Public Health 2019; 172: 22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Equality Act . https://www.legislation.gov.uk/ukpga/2010/15/contents (2010, accessed 24 August 2018). 2010.
- 15.Honeyman M, Maguire D, Evans H, et al. Digital technology and health inequalities: a scoping review. Cardiff: Public Health Wales, 2020. [Google Scholar]
- 16.Huxley CJ, Atherton H, Watkins JA, et al. Digital communication between clinician and patient and the impact on marginalised groups: a realist review in general practice. Br J Gen Pract 2015; 65: e813–e821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peters MD, Godfrey C, McInerney P, et al. Chapter 11: scoping reviews (2020 version). In: Aromataris E, Munn Z. (eds) JBI manual for evidence synthesis. Adelaide: JBI, 2020, pp. 406–452. https://synthesismanual.jbi.global [Google Scholar]
- 18.Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth 2020; 18: 2119–2126. [DOI] [PubMed] [Google Scholar]
- 19.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018; 169: 467–473. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization. Classification of digital health interventions v1.0. Geneva: World Health Organization, 2018. https://www.who.int/publications-detail-redirect/WHO-RHR-18.06 [Google Scholar]
- 21.Akobeng AK, O’Leary N, Vail A, et al. Telephone consultation as a substitute for routine out-patient face-to-face consultation for children with inflammatory bowel disease: randomised controlled trial and economic evaluation. EBioMedicine 2015; 2: 1251–1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rixon L, Hirani SP, Cartwright M, et al. A RCT of telehealth for COPD patient’s quality of life: the whole system demonstrator evaluation: COPD patient’s quality of life. Clin Respir J 2017; 11: 459–469. [DOI] [PubMed] [Google Scholar]
- 23.Walters K, Kharicha K, Goodman C, et al. Promoting independence, health and well-being for older people: a feasibility study of computer-aided health and social risk appraisal system in primary care. BMC Fam Pract 2017; 18: 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crombie IK, Irvine L, Williams B, et al. Text message intervention to reduce frequency of binge drinking among disadvantaged men: the TRAM RCT. Public Health Res 2018; 6: 1–156. [PubMed] [Google Scholar]
- 25.Latif A, Waring J, Chen L, et al. Supporting the provision of pharmacy medication reviews to marginalised (medically underserved) groups: a before/after questionnaire study investigating the impact of a patient–professional co-produced digital educational intervention. BMJ Open 2019; 9: e031548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vereenooghe L, Gega L, Langdon PE. Intellectual disability and computers in therapy: views of service users and clinical psychologists. Cyberpsychol J Psychosoc Res Cyberspace 2017; 11: Article 11. [Google Scholar]
- 27.Latif A, Waring J, Pollock K, et al. Towards equity: a qualitative exploration of the implementation and impact of a digital educational intervention for pharmacy professionals in England. Int J Equity Health 2019; 18: 151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Turnbull S, Lucas PJ, Hay AD, et al. Digital health interventions for people with type 2 diabetes to develop self-care expertise, adapt to identity changes, and influence other’s perception: qualitative study. J Med Internet Res 2020; 22: e21328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Turnbull S, Lucas PJ, Hay AD, et al. The role of economic, educational and social resources in supporting the use of digital health technologies by people with T2D: a qualitative study. BMC Public Health 2021; 21: 293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tuijt R, Rait G, Frost R, et al. Remote primary care consultations for people living with dementia during the COVID-19 pandemic: experiences of people living with dementia and their carers. Br J Gen Pract 2021; 71: e574–e582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hughes T, Beard E, Bowman A, et al. Medical student support for vulnerable patients during COVID-19 – a convergent mixed-methods study. BMC Med Educ 2020; 20: 377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Voorberg WH, Bekkers VJJM, Tummers LG. A systematic review of co-creation and co-production: embarking on the social innovation journey. Public Manag Rev 2015; 17: 1333–1357. [Google Scholar]
- 33.Fox C, Smith A, Traynor P, et al. Co-creation and coproduction in the United Kingdom: a rapid evidence assessment. Technical Report. Policy Evaluation Research Unit, Manchester Metropolitan University, https://mmuperu.co.uk/wp-content/uploads/2020/09/Co-Creation_and_Co-Production_in_the_United_Kingdom_-_A_Rapid_Evidence_Assessment_-_March_2018.pdf (2018).
- 34.Slattery P, Saeri AK, Bragge P. Research co-design in health: a rapid overview of reviews. Health Res Policy Syst 2020; 18: 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brownson RC, Kumanyika SK, Kreuter MW, et al. Implementation science should give higher priority to health equity. Implement Sci 2021; 16: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tinder Foundation. Health and digital: reducing inequalities, improving society. Sheffield: Tinder Foundation, 2016. [Google Scholar]
- 37.Gann B. Combating digital health inequality in the time of coronavirus. J Consum Health Internet 2020; 24: 278–284. [Google Scholar]
- 38.Walters R, Leslie SJ, Polson R, et al. Establishing the efficacy of interventions to improve health literacy and health behaviours: a systematic review. BMC Public Health 2020; 20: 1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Choukou M-A, Sanchez-Ramirez DC, Pol M, et al. COVID-19 infodemic and digital health literacy in vulnerable populations: a scoping review. Digit Health 2022; 8: 20552076221076930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Song J, Sharp CA, Davies AR. Population health in a digital age: patterns in the use of social media in Wales. UK: Public Health Wales & Bangor University, 2020. [Google Scholar]
- 41.Lupton D. Young people’s use of digital health technologies in the global north: narrative review. J Med Internet Res 2021; 23: e18286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J 2021; 372: n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-dhj-10.1177_20552076231185442 for Exploring the use of digital technology to deliver healthcare services with explicit consideration of health inequalities in UK settings: A scoping review by Albert Farre, Mei Fang, Beth Hannah, Meiko Makita, Alison McFadden, Deborah Menezes, Andrea Rodriguez, Judith Sixsmith and Nicola M Gray in DIGITAL HEALTH