Abstract
More than 16 million Americans provide unpaid care for someone with Alzheimer’s disease and related dementias (ADRD). During the COVID-19 pandemic, unpaid caregivers experienced increased chronic severe stress from widespread closures and social distancing. We conducted eight surveys from March 2020 to March 2021 among a cohort of over 10,000 individuals. Cross-sectional analysis was conducted to investigate frequency and ratios of groups reporting increased stress across surveys. A longitudinal analysis was also performed with the 1,030 participants who took more than one survey. We found a growing crisis among dementia caregivers: By Survey 8, current caregivers reported 2.9 times higher stress levels than the comparator group. By that time, 64% of current caregivers reported having multiple stress symptoms typically found in people experiencing severe stress. Both analyses reported increased levels of stressors over time that were more associated with certain caregiver groups. Our findings underscore the urgent need for public policy initiatives and supportive community infrastructure to support ADRD caregivers.
Keywords: Alzheimer’s, ADRD, dementia caregiver, severe stress, COVID-19
Introduction
Each year, more than 16 million Americans provide more than 17 billion hours of unpaid care for family members and friends with Alzheimer’s disease and related dementias (ADRD) (Centers for Disease Control and Prevention, 2022a). A majority of these caregivers reported high levels of stress prior to the pandemic.
A 2022 report found that 59% of family caregivers of people with ADRD rated the emotional stress of caregiving as high or very high (Alzheimer’s Association, 2023, p. 46). Another recent study of the needs of caregivers of color found that 54% reported feeling stressed as a top challenge (respondents were Black/African American, Latino, and Asian) (T. L. Frangiosa et al., 2021).
The stress associated with caregiving may exacerbate declines in caregiver health that occur with age. A 2020 report notes that the stress associated with caregiving may exacerbate declines in health that occur with age, with only 42% of caregivers of people ages 50 and older considering their health to be excellent or very good, down significantly from 2015 (48%) (National Alliance for Caregiving & AARP, 2021, p. 37).
Stress experienced by unpaid caregivers also affects the care of people with ADRD. For example, one study shows that distress on the part of family caregivers is associated with increased institutionalization, exacerbated behavioral and psychological challenges, and an increased likelihood of abuse of people with dementia (Stall et al., 2019).
The COVID-19 pandemic that struck in early 2020 triggered a crisis for unpaid caregivers in the Unites States, about 30% of whom are age 65 or older (Alzheimer’s Association, 2023, p. 42). Challenges included (1) no or reduced in-home help from family, friends, and paid caregivers; (2) shuttered respite and day programs for people living with ADRD; (3) confusion experienced by some with dementia managing COVID-related requirements such as masking and social distancing; (4) inability to visit or communicate consistently with loved ones living in long-term care; (5) worry about consistency of care for the person with ADRD; and (6) fear of contracting COVID-19 or infecting a loved one with dementia. Several published papers report on the impact of COVID on dementia caregivers, including Beach et al. (2021), Cohen et al. (2021), Aledeh and Habib Adam (2020). This growing body of literature includes a paper on the first four surveys from this multiyear study (T. Frangiosa et al., 2020).
To learn how people living with ADRD and unpaid family caregivers were affected by pandemic restrictions, we launched what became a multiyear series of eight surveys. This article reports on the survey series and our findings.
Methods
This research was conducted through the A-LIST What Matters Most Insight Series Study. The A-LIST is a convenience sample of over 10,000 people who are affected by ADRD/Mild Cognitive Impairment (MCI) or interested in brain health. Individuals have been recruited over a period of time since 2016, with recruitment ongoing. These individuals have opted to participate in previous surveys on a variety of topics. There are no exclusion criteria for this unique cohort, with inclusion/exclusion criteria being defined at the point of each survey conducted, when necessary. However, participants self-identify as (1) current (unpaid) care partners; (2) former (unpaid) care partners (of now deceased individuals); (3) individuals diagnosed with MCI, Alzheimer’s disease, or another dementia; (4) individuals at risk for MCI, Alzheimer’s disease, or another dementia; and (5) individuals with general interest in brain health (if not falling into the other categories). For this project, a total of eight surveys were conducted with the subset of this cohort who opted in between March 2020 and March 2021 (on a nearly monthly basis). Fielded by email, the series centered on the impact of COVID-19 restrictions. This corresponded with the start of statewide restrictions across the U.S. through the rise of the COVID-19 Delta variant. No inducement was offered to respondents.
The A-LIST What Matters Most Insights Study is overseen by an Institutional Review Board and conducted in accordance with International Conference on Good Clinical Practice and applicable United States Code of Federal Regulations. Surveys are programed within Survey Monkey to consenting individuals, and data are stored in a secure database.
The eight surveys on impacts of COVID-19 restrictions asked participants to self-identify with one of the five groups as specified above. The group with a general interest in brain health is the comparator group. Note that the terms “care partners” and “caregivers” are used interchangeably. Each survey took under 30 min to complete.
The surveys asked about a wide range of aspects of the pandemic, including the effects on cognition for people with ADRD, attitudes toward COVID-19 testing and vaccines, holiday disruptions, coping strategies, burden experienced by caregivers, and the impact on care for people with ADRD.
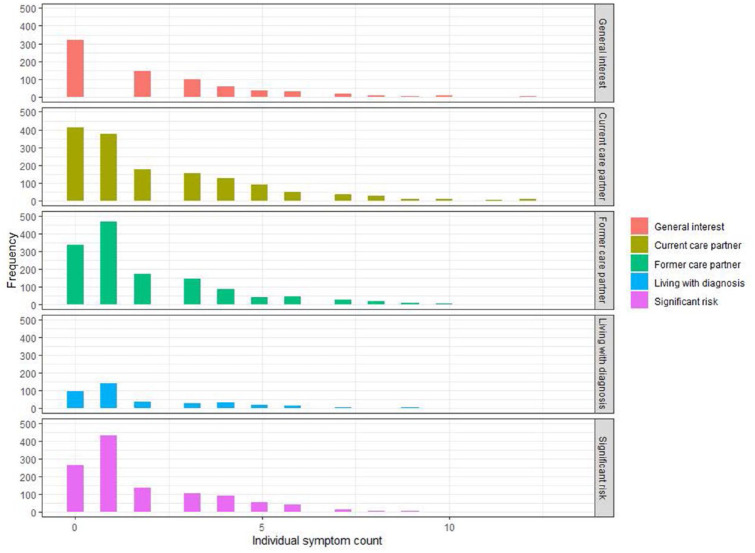
In each survey, participants were asked to rate their current stress level compared to what it was prior to the start of COVID-19 restrictions. Because of the increasing stress levels seen in the second survey, beginning with Survey 3 participants were asked to indicate which of 13 possible trauma-related symptoms they had experienced or none (see Figure 1). Note that the majority of symptoms queried referenced several of the DSM-5 criteria for Posttraumatic Stress Disorder 309.81 (F43.10). Nonetheless, no standardized symptom measures or scales were used. The selected symptoms are neither exhaustive nor intended to confer a PTSD diagnosis.
Figure 1.
Stress symptoms in Surveys 3 to 8.
Statistical Methods
Two analytical approaches were used: cross-sectional and longitudinal. Cross-sectional analyses summarized each group’s responses at the point in time for each survey. Longitudinal analyses assessed how individual respondents’ answers changed over time.
We used both cross-sectional and longitudinal data in this study to provide a more comprehensive understanding of the research question being investigated. The cross-sectional analysis allowed us to gain insights into the prevalence of certain feelings and behaviors at a specific point in time. This can be helpful in, for example, identifying potential risk factors or associations between variables at the start of the study.
The longitudinal data analysis allowed us to track changes over time and better understand the development and change in these feelings and behaviors.
By analyzing both types of data together, we sought to gain a more complete picture of how these factors interact and influence outcomes over time. Additionally, combining cross-sectional and longitudinal data may also help to address issues related to confounding variables and selection bias.
Cross-Sectional Methods
Exploratory analyses were conducted to investigate the frequency and ratios of the various groups reporting increasing levels of stress across the eight surveys. Summary counts at each survey for each pairwise comparison (2 × 2 contingency table) were compared statistically using chi-squared. Association between the groups and reported stress levels were interpreted by calculating the standardized residuals from the chi-squared test.
Longitudinal Methods
Data were modeled using a longitudinal multilevel model (linear mixed effects model) with repeated measures on participants in different groups represented by each survey. We performed two separate analyses with the following dependent variables:
i. the individual stress symptoms
ii. the sum of the reported stressors during the course of the survey
In this model, the reported symptoms for each participant were summed to a single score and this score evaluated to determine whether the accumulation of different stress symptoms changed over time.
In both the cross-sectional and longitudinal methods, the explanatory variables were compared to a reference group. The explanatory variables used were participant group (general interest in brain health was used as the reference), gender (female was used as the reference), education (high school education was used as the reference), and income (<$25,000 annually was used as the reference). Only individuals who completed more than one survey were included in these longitudinal analyses.
Participation
Between 500 and 1,000 individuals responded to each of the eight surveys. Table 1 highlights numbers and groups that participants identified with for each survey. Groups generally had more than 100 respondents in each survey except the “Living with diagnosis” group, in which participation ranged from 40 to 60 respondents.
Table 1.
Respondent Overview for Cross-Sectional Analysis.
| Survey # | Date | Total, n* | Interest in brain health, n | Current care partner, n | Former care partner, n | Living with diagnosis, n | Significant risk, n |
|---|---|---|---|---|---|---|---|
| 1 | 03/2020 | 597 | 135 | 170 | 143 | 39 | 110 |
| 2 | 04/2020 | 779 | 172 | 217 | 187 | 54 | 149 |
| 3 | 05/2020 | 671 | 141 | 183 | 156 | 58 | 133 |
| 4 | 06/2020 | 581 | 161 | 202 | 168 | 50 | 134 |
| 5 | 07/2020 | 729 | 197 | 181 | 160 | 42 | 149 |
| 6 | 09/2020 | 963 | 223 | 218 | 252 | 58 | 212 |
| 7 | 10/2020 | 547 | 110 | 150 | 127 | 39 | 121 |
| 8 | 03/2021 | 667 | 134 | 167 | 169 | 44 | 153 |
Individuals who did not select a participant group were not included in the analyses and are not represented here.
Across all eight surveys, regardless of analysis type, responses from 2,201 unique participants were received. Many participants responded to multiple surveys, with 98 responding to all eight surveys. For each survey, a contingency table was created to evaluate how responses differed across each of the identified groups.
For the longitudinal analyses, while 1,030 participants took more than one survey, 855 participants remained after those with missing data were dropped for complete case analysis.
As shown in Table 2, participant numbers were again well-distributed across the groups except the “Living with diagnosis” group. The sample was predominantly female, Caucasian, and over 65 years of age (see Supplemental Table for age groups). These demographics are reflective of the cohort.
Table 2.
Population Demographics for Participants Who Completed Multiple Surveys and Qualified for Longitudinal Complete Case Analysis (n = 855).
| Characteristic and frequency (%) | Interest in brain health (n = 176) | Current care partner (n = 214) | Former care partner (n = 210) | Living with diagnosis (n = 80) | Significant risk (n = 175) |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 119 (67.6%) | 143 (66.8%) | 164 (78.1%) | 50 (62.5%) | 125 (71.4%) |
| Male | 57 (32.4%) | 71 (33.2%) | 46 (21.9%) | 30 (37.5%) | 49 (28.0%) |
| Prefer not to say | 0 | 0 | 0 | 0 | 1 (0.6%) |
| Ethnicity | |||||
| White/Caucasian | 168 (95.5%) | 180 (84.1%) | 197 (93.8%) | 72 (90.0%) | 166 (94.9%) |
| Other | 7 (4.0%) | 30 (14.0%) | 13 (6.2%) | 7 (8.8%) | 8 (4.6%) |
| Prefer not to say | 1 (0.5%) | 4 (1.9%) | 0 | 1 (1.2%) | 1 (0.5%) |
| Age | |||||
| 65 and younger | 65 (36.9%) | 97 (45.3%) | 95 (45.2%) | 36 (45.0%) | 62 (35.4%) |
| Over 65 | 111 (63.1%) | 117 (54.7%) | 115 (54.8%) | 44 (55.0%) | 113 (64.6%) |
| Income | |||||
| Less than $25k | 24 (13.6%) | 9 (4.2%) | 19 (9.0%) | 13 (16.3%) | 19 (10.9%) |
| $25-$49k | 28 (16.0%) | 28 (13.1%) | 44 (21.0%) | 12 (15.0%) | 33 (18.9%) |
| $50-$99k | 68 (38.6%) | 105 (49.1%) | 81 (38.6%) | 30 (37.5%) | 61 (34.9%) |
| $100k+ | 51 (29.0%) | 66 (30.8%) | 60 (28.6%) | 24 (30.0%) | 60 (34.2%) |
| Prefer not to say | 5 (2.8%) | 6 (2.8%) | 6 (2.8%) | 1 (1.2%) | 2 (1.1%) |
| Education | |||||
| High school | 37 (21.0%) | 33 (15.4%) | 53 (25.2%) | 8 (10.0%) | 32 (18.3%) |
| Undergraduate degree | 73 (41.5%) | 90 (42.1%) | 90 (42.9%) | 34 (42.5%) | 69 (39.4%) |
| Postgraduate degree | 66 (37.5%) | 89 (41.6%) | 67 (31.9%) | 37 (46.3%) | 72 (41.1%) |
| Prefer not to say | 0 | 2 (0.9%) | 0 | 1 (1.2%) | 2 (1.2%) |
Results
Key Findings of Cross-Sectional Analysis of Increased Stress
In each survey, respondents were asked, “How has YOUR stress level changed as a result of coronavirus restrictions?” with potential answers of “Significantly lower,” “Somewhat lower,” “About the Same,” “Somewhat higher,” or “Significantly higher.”
In the first survey, 25% (41/165) of current caregivers reported significantly higher stress since COVID-19 restrictions were implemented. This was nearly 1.5 times higher than the comparator group (respondents who identified as interested in brain health) (14%; 21/128) (chi-squared p = .107). By Survey 8, this proportion of people reporting high levels of stress was maintained in the current caregiver group (22%), but much reduced in the comparator group (7%), resulting in a 2.9 times higher reported level of stress in the current caregivers (p = .0013). Further, when combining data for those reporting either higher or significantly higher stress at Survey 8 this was higher still, with 78% of current caregivers reporting this versus 57% in the comparator group (p < .001).
Other groups also reported significantly higher levels of stress, which trended upward over the 13-month span of the surveys. For example, while former caregivers and those diagnosed with MCI/ADRD did not report significantly higher levels of stress at Survey 1, this rose to more than two times that of the comparator group by Survey 8 (p = .038 and .012, respectively). Significantly more (p = .014) former caregivers reported experiencing either higher or significantly higher stress: 71% compared with the comparator group. Participants identifying as “at risk for dementia” reported similar levels of stress to those in the comparator group.
When taking all responses into consideration, at Survey 1 there was no significant difference between groups for reported stress levels (chi-squared p = .325). However, a significant overall effect was observed in Survey 8 (chi-squared p = .0045). The association between the groups and reported stress levels are represented in Figure 2 as the standardized residual scores. These scores help interpret the results of the chi-squared analysis by providing information about which values contribute to the significant results. Here, positive values specify a positive association between group and reported stress (shown in blue), whereas negative values specify a negative association (red). This analysis shows that current care partners and, to a lesser extent, those living with a diagnosis, report levels of significantly higher stress at Survey 8 (large blue circle) versus those with a general interest in brain health (and those at significant risk), who show a negative association with significantly higher stress.
Figure 2.
Assessment of contributing factors to the total chi-square score using Pearson residuals. Blue circles denote positive association; red circles denote negative association. Circle size represents magnitude of effect.
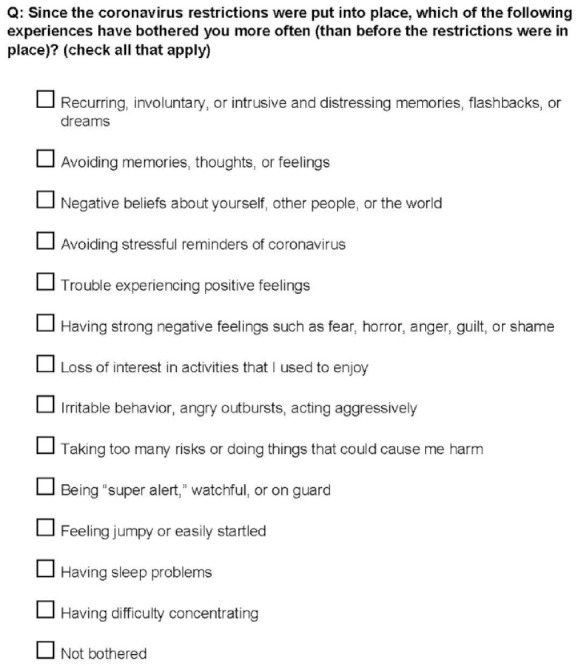
An evaluation of the symptoms reported for all participants across Surveys 3 to 8 showed 64% of current caregivers having multiple stress symptoms typically found in people experiencing severe stress, indicating 1 year of a consistently felt high number of stressors. This is compared to 54% in the former caregiver group, 48% of those living with a diagnosis, and 43% of the comparator group (those interested in brain health). Figure 3 shows total symptom counts for the participants completing surveys that included these questions. The differences in symptom reporting appeared to be consistent with differences between groups in reported stress levels as described above (i.e., current and former caregivers tend to report higher number of total symptoms as compared to other groups).
Figure 3.
Counts of total symptoms for participants completing all surveys.
Key Findings of Longitudinal Analysis of Symptoms of Severe Stress
A longitudinal analysis of the number and type of stress symptoms was conducted to assess whether individuals were impacted by pandemic-associated stress over time. The current caregiver group reported a statistically significant increase in eight of the 13 stress-related symptoms (fixed effects model p < .05) over the 13-month period. These eight are shown in Figure 4.
Figure 4.
Model of stress-related symptoms over time.
For the score representing the sum of reported symptoms, using a linear mixed effects model we observed that the main effect of current caregiver group generally reporting a higher number of different stressors over time was significant when accounting for several other covariates in the model including gender, education, and income (β = .65, SE = 0.12, p = <.001) (see Figure 5).
Figure 5.
Model estimating testing for the association between total stressors over time and covariates of interest.
The analysis showed that males reported less of an increase in symptoms when compared to females (β = −.32, SE = 0.13, p = .015), while those in the over-65 age category reported fewer stress symptoms compared to the younger group (β = −.45, SE = 0.11, p = <.001). Although not statistically significant, as income bracket increased there was a trend toward reporting fewer symptoms over time, and those in the non-Caucasian ethnicity groups showed a trend toward reporting more symptoms. Variance inflation factor (Fox & Monette, 1992) was approximately 1 for all variables, suggesting that collinearity was not observed (see Table 3).
Table 3.
Summary of Estimates From Linear Mixed Effects Model.
| Estimate | Standard error | p-Value | |
|---|---|---|---|
| (Intercept) | 2.60 | 0.238 | <.001 |
| Survey number | 0.054 | 0.018 | .003 |
| Category (reference: General interest in brain health) | |||
| Current care partner | 0.571 | 0.144 | <.001 |
| Former care partner | 0.131 | 0.133 | .325 |
| Living with diagnosis | 0.521 | 0.195 | .008 |
| At significant risk | 0.091 | 0.128 | .476 |
| Gender (reference: Female) | |||
| Male | −0.324 | 0.133 | .015 |
| Prefer not to say | 0.49 | 0.827 | .553 |
| Education (reference: High School) | |||
| Undergraduate degree | 0.003 | 0.146 | .98 |
| Postgraduate degree | 0.005 | 0.159 | .977 |
| Prefer not to say | −0.115 | 0.498 | .817 |
| Income (reference: <$25k) | |||
| $25-49k | −0.19 | 0.189 | .313 |
| $50-99k | −0.287 | 0.186 | .123 |
| $100k+ | −0.355 | 0.197 | .071 |
| Prefer not to say | −0.071 | 0.317 | .823 |
| Ethnicity (reference: White/Caucasian) | |||
| Other | 0.262 | 0.173 | .131 |
| Prefer not to say | 0.446 | 0.438 | .308 |
| Age (reference: 65 and younger) | |||
| Over 65 | −0.453 | 0.114 | <.001 |
This model incorporating several predictor variables accounted for 63% of the variance in reported symptoms (R2 = 0.63), yielding an Akaike Information Criterion (AIC) of 2,260.8 and a Bayesian Information Criterion (BIC) of 2,350.2. We compared this to a model that included only timepoint as a predictor, which resulted in an AIC of 2,755.7 and a BIC of 2,783.257. Therefore, the model which incorporated several additional covariates showed a substantial improvement in model fit, suggesting that the inclusion of the additional covariates provided a more comprehensive explanation of the observed data.
The comparison between the two models highlights the importance of considering relevant covariates in addition to timepoint when modeling symptom severity. The lower AIC and BIC values for our reported model indicate a better balance between model fit and complexity.
Discussion
Our findings indicate that caregivers reported the highest stress and the greatest number of stress-related symptoms over time, but all study groups were impacted by COVID restrictions. Even at Survey 1, current caregivers experienced 1.5 times more stress than the comparator group (respondents who identified as interested in brain health). At Survey 8 (final survey), 78% of current caregivers described experiencing higher or significantly higher stress symptoms since the pandemic’s onset although, of note, nearly as many former caregivers reported these levels compared to the general interest group. This was 2.9 times higher than the comparator group. These findings were consistent for both overall stress levels and the number of individual symptoms.
These data are broadly consistent with findings in the traumatic stress literature describing the numerous negative psychosocial impacts of COVID-19 and its associated restrictions as well as the considerable mental health burden that the pandemic placed on many people (Carbone et al., 2021; Blasco-Belled et al., 2022; Ledford, 2022; Panchal et al., 2021). In addition to the general public, those working in health services and the helping professions appear to have been especially affected (Blasco-Belled et al., 2022), highlighting the need for further attention to cumulative stress in such times.
We describe the most frequently reported symptoms, which potentially reflect aspects of stress as well as reactions related to depression. Research in stress and traumatic stress has long noted the concordance of these symptoms in any number of populations, along with high rates of comorbidity between actual PTSD and major depressive disorders (Franklin & Zimmerman, 2001; Gros et al., 2012; Post et al., 2011). Paths for more clearly differentiating these symptoms and suggestions for their remediation are needed.
Current caregivers in our sample generally reported differences among total symptoms over time compared to other study groups. Further, longitudinal analysis showed that younger caregivers and also ethnic minority participants may have been more heavily affected, although the latter was not statistically significant in our model.
The current study has some limitations. We relied exclusively on online self-reporting in a convenience sample. Moreover, we cannot speak to the reliability or validity of reporting, in particular for the ADRD participants where we lack any measure of cognitive ability. This method precluded characterizing a caregiver’s relationship to a patient, which does not allow us to thoroughly understand, for example, why younger caregivers have higher stress levels. Although we presume stress inherent with caregiving, we did not include any quantifiable measure of that burden or the possibility of exposure to other stressful life events. We also did not assess any impact on overall quality of life beyond the symptoms noted. These issues would be important to address in future research. Finally and critically, we cannot speak to the presence or absence of actual traumatic stress, as that exceeds the scope of our inquiry. There is no psychometric evidence in support of the stress items we selected for evaluation, even though they were broadly based on DSM-5 criteria. The symptoms reported are based on DSM-5 criteria for PTSD. They are neither exhaustive nor exclusive to PTSD but do appear within that diagnostic category. It is a limitation of this paper that we were not able at the outset to include a standardized measure of PTSD, as that was not the specific focus of the original survey. Relatedly, it is not possible to assume that the symptoms or experiences reported are not also tied to depression or a related state. This is further confounded by the fact that there is a strong diagnostic overlap between PTSD and various depressive disorders. It is possible that what we describe reflects the widespread, adverse impact of the pandemic and its general restrictions for any number of individuals.
We believe this is the first longitudinal study of the impact of COVID-19 restrictions in these groups (in a large ADRD caregiver sample) to examine some of the many emotional and psychological effects of caregiving during the COVID-19 pandemic. We acknowledge that in a longitudinal study, repeated measurements of participants over time may introduce bias if the timing or frequency of data collection coincides with certain events or experiences that could affect outcomes. We anticipated that the COVID pandemic would introduce increased stress in caregivers generally, but we made efforts to control for potential confounding variables that could skew results. For example, we collected data at multiple points throughout the year and adjusted analyses for factors such as age, sex, socioeconomic status, and caregiver group to increase the reliability of our findings.
We acknowledge that missing data is a common issue in linear mixed effects models (LMMs), the approach used here to analyze the longitudinal data. There are several approaches that can be used to handle missing data in LMMs, including deletion methods, imputation methods, and maximum likelihood estimation. Here we used pairwise (not listwise) deletion, which involves using only the available data for each specific analysis. Maximum likelihood estimation (MLE) can handle missing data in LMMs by estimating parameters based on all available information, including incomplete cases.
Finally, it is important to emphasize that the results from this investigation describing the associations between predictor variables and the outcome variable do not imply causality. To establish causality, more rigorous research designs such as randomized controlled trials or quasi-experimental studies are needed, which can control for potential confounders and provide stronger evidence for causal relationships. Our current results should be interpreted as evidence of statistical associations, and further research using robust designs and methods is required to draw causal inferences between the predictor variables and the outcome variable.
Conclusion
The COVID-19 pandemic led to more than 1 million deaths in the United States and millions of affected family members (Centers for Disease Control and Prevention, 2022b) with a disproportionate burden on communities of color (Hill & Artiga, 2022). It also affected the mental health and wellness of millions of other people. This research uncovered the amplified impact on current ADRD caregivers (and former to a lesser extent) and the urgent need for public policy initiatives and public health infrastructure to ensure better support for these 16 million caregivers during the next crisis. For example, implementation of the Administration for Community Living’s National Strategy to Support Family Caregivers should be considered to help ensure access to services and supports to reduce caregiver stress. And best practices for virtual services, such as telehealth and community-based caregiver support, should also be identified and amplified. These steps would benefit all unpaid caregivers and other vulnerable communities and individuals.
Supplemental Material
Supplemental material, sj-docx-1-ggm-10.1177_23337214231185664 for Caring for Dementia Caregivers: Understanding Caregiver Stress During the COVID-19 Pandemic by Lee Lancashire, Virginia Biggar, Meryl Comer, Terry Frangiosa, Allyson Gage, Russ Paulsen, Amber Roniger and Jessica Wolfe in Gerontology and Geriatric Medicine
Acknowledgments
UsAgainstAlzheimer’s and the A-LIST research team are deeply grateful to the members of the A-LIST who made this research possible. We appreciate their support during an unprecedented national crisis impacting so many families. We also want to express appreciation to our research partners, Home Instead Senior Care, CaringKind, and Alzheimer’s Los Angeles. In addition, we thank Kelly Murphy for data analysis and Elizabeth Hurwit for editorial guidance.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: UsAgainstAlzheimer’s is grateful for the financial support of our philanthropic and industry partners who made this survey series possible, including the Eisai USA Foundation, Inc., naviHealth, and Biogen. In addition, Cohen Veterans Bioscience and UsAgainstAlzheimer’s have funded the data analysis and interpretation described in this article, as well as the open access status.
Ethical Approval: Ethical Board/IRB Approval: #Pro00029894. Advarra, Inc. 6100 Merriweather Dr., Suite 600, Columbia, MD 21044, Phone: 410.884.2900.
ORCID iD: Virginia Biggar  https://orcid.org/0000-0001-6995-3035
https://orcid.org/0000-0001-6995-3035
Supplemental Material: Supplemental material for this article is available online.
References
- Aledeh M., Habib Adam P. (2020). Caring for dementia caregivers in times of the COVID-19 crisis: A systematic review. American Journal of Nursing Research, 8(5), 552–561. 10.12691/ajnr-8-5-8 [DOI] [Google Scholar]
- Alzheimer’s Association. (2023). Alzheimer’s disease facts and figures. Created with data from the Alzheimer’s Association. https://www.alz.org/media/documents/alzheimers-facts-and-figures.pdf
- Beach S. R., Schulz R., Donovan H., Rosland A. M. (2021). Family caregiving during the COVID-19 pandemic. The Gerontologist, 61(5), 650–660. 10.1093/geront/gnab049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blasco-Belled A., Tejada-Gallardo C., Fatsini-Prats M., Alsinet C. (2022). Mental health among the general population and healthcare workers during the COVID-19 pandemic: A meta-analysis of well-being and psychological distress prevalence. Current Psychology. Advance online publication. 10.1007/s12144-022-02913-6 [DOI] [PMC free article] [PubMed]
- Carbone E. A., de Filippis R., Roberti R., Rania M., Destefano L., Russo E., De Sarro G., Segura-Garcia C., De Fazio P. (2021). The mental health of caregivers and their patients with dementia during the COVID-19 pandemic: A systematic review. Frontiers in Psychology, 12, 782833. 10.3389/fpsyg.2021.782833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2022. a). Caregiving for a person with Alzheimer’s disease or a related dementia. Based on CDC Division of Population Health Alzheimer's Disease and Healthy Aging Dataset updated May 2022. https://www.cdc.gov/aging/caregiving/alzheimer.htm
- Centers for Disease Control and Prevention. (2022. b). COVID-19 mortality overview. Based on data from CDC National Center for Health Statistics. https://www.cdc.gov/nchs/covid19/mortality-overview.htm
- Cohen S. A., Kunicki Z. J., Drohan M. M., Greaney M. L. (2021). Exploring changes in caregiver burden and caregiving intensity due to COVID-19. Gerontology and Geriatric Medicine, 7, 2333721421999279. 10.1177/2333721421999279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox J., Monette G. (1992). Generalized collinearity diagnostics. Journal of the American Statistical Association, 87, 178–183. 10.1080/01621459.1992.10475190 [DOI] [Google Scholar]
- Frangiosa T., Biggar V., Comer M., Roniger A. (2020). Research survey series shows effects of COVID-19 shutdowns on Alzheimer’s community, with especially high stress on caregivers. Advances in Geriatric Medicine and Research, 4(3), e200020. 10.20900/agmr20200020 [DOI] [Google Scholar]
- Frangiosa T. L., Biggar V., Resendez J., Monroe S., Schmidt H., Loud S. (2021). The changing face of Alzheimer's: a survey on burden for caregivers from communities of color [Poster presentation]. Alzheimer’s Association Virtual Conference. https://www.usagainstalzheimers.org/sites/default/files/2021-06/Changing_Face_of_Alzheimers_caregiver_burden_poster.pdf [Google Scholar]
- Franklin C. L., Zimmerman M. (2001). Posttraumatic stress disorder and major depressive disorder: Investigating the role of overlapping symptoms in diagnostic comorbidity. The Journal of Nervous and Mental Disease, 189(8), 548–551. [DOI] [PubMed] [Google Scholar]
- Gros D. F., Price M., Magruder K. M., Frueh B. C. (2012). Symptom overlap in posttraumatic stress disorder and major depression. Psychiatry Research, 196(2–3), 267–270. 10.1016/j.psychres.2011.10.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill L., Artiga S. (2022). COVID-19 cases and deaths by race/ethnicity: current data and changes over time. https://www.kff.org/coronavirus-covid-19/issue-brief/covid-19-cases-and-deaths-by-race-ethnicity-current-data-and-changes-over-time/
- Ledford H. (2022). How common is long covid? why studies give different answers. Our Nature, 606, 852–853. https://www.nature.com/articles/d41586-022-01702-2 [DOI] [PubMed] [Google Scholar]
- National Alliance for Caregiving & AARP. (2021). Caregiving in the U.S. 2020: a focused look at family caregivers of adults age 50+. https://www.caregiving.org/wp-content/uploads/2021/05/AARP1340_RR_Caregiving50Plus_508.pdf
- Panchal N., Kamal R., Cox C., Garfield R. (2021). The implications of COVID-19 for mental health and substance use. https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/
- Post L. M., Zoellner L. A., Youngstrom E., Feeny N. C. (2011). Understanding the relationship between co-occurring PTSD and MDD: Symptom severity and affect. Journal of Anxiety Disorders, 25(8), 1123–1130. 10.1016/j.janxdis.2011.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall N. M., Kim S. J., Hardacre K. A., Shah P. S., Straus S. E., Bronskill S. E., Lix L. M., Bell C. M., Rochon P. A. (2019). Association of informal caregiver distress with health outcomes of community-dwelling dementia care recipients: A systematic review. Journal of the American Geriatrics Society, 67(3), 609–617. 10.1111/jgs.15690 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-ggm-10.1177_23337214231185664 for Caring for Dementia Caregivers: Understanding Caregiver Stress During the COVID-19 Pandemic by Lee Lancashire, Virginia Biggar, Meryl Comer, Terry Frangiosa, Allyson Gage, Russ Paulsen, Amber Roniger and Jessica Wolfe in Gerontology and Geriatric Medicine