Abstract
Background:
Ankle fractures are among the most common physeal fractures in children. When surgical management is warranted, subsequent hardware removal remains controversial. This study was designed to determine rates of hardware removal in patients with physeal ankle fractures and identify risk factors for removal. Procedure data was utilized to compare rates of subsequent ankle procedures in patients with hardware removed and hardware retained.
Methods:
We conducted a retrospective cohort study utilizing data from the Pediatric Health Information System (PHIS) for the years 2015 through 2021. We longitudinally followed patients treated for distal tibia physeal fractures to determine the rates of hardware removal and subsequent ankle procedures. Patients with open fractures or polytrauma were excluded. We used univariate, multivariate, and descriptive statistics to characterize the rates of hardware removal, identify factors associated with removal, and assess the rates of subsequent procedures.
Results:
This study included 1008 patients who underwent surgical management of a physeal ankle fracture. The mean age at index surgery was 12.6 years with an SD of 2.2 years, and 60% of patients identified as male. Two hundred forty-two patients (24%) had their hardware removed at an average time of 276 days (range, 21-1435 days) following index surgery. Patients with Salter Harris III (SH-III) or Salter Harris IV (SH-IV) fractures had hardware removed more often than patients with Salter-Harris II (SH-II) fractures (28.9% vs 11.7%, P < .01). Four-year rates of subsequent ankle procedures are similar between patients with hardware removed and hardware retained.
Conclusion:
The rate of hardware removal in children with physeal ankle fractures is higher than previously reported. Patients of younger age, higher income, and with fractures involving the epiphysis (SH-III and SH-IV) are more likely to undergo hardware removal.
Level of Evidence:
Level III, retrospective study.
Keywords: physeal ankle fracture, hardware removal, pediatric trauma, ORIF
Introduction
Physeal fractures of the distal tibia represent between 9% and 18% of all physeal injuries in children.9,10,13,14 These injuries may be purely physeal (Salter Harris I) or may involve the distal tibial metaphysis and epiphysis (Salter Harris II-IV).18,23 The management of these injuries includes immobilization or surgical management depending on factors such as fracture displacement, fracture alignment, and patient age. 11 If surgery is indicated for displaced fractures, management may consist of either closed reduction and percutaneous pinning (CRPP) or open reduction internal fixation (ORIF) to achieve anatomic reduction and decrease the risk of growth arrest or future joint degeneration. These fractures are commonly fixed with Kirschner wires (K-wires), screws, or a combination thereof but rarely require plating. The hardware can be removed later for a variety of reasons including pain, mechanical dysfunction, infection, and concern for future arthritis.1,5
Currently, asymptomatic hardware removal remains controversial. A scoping review conducted by Prediger et al 15 demonstrated a lack of convincing evidence regarding the removal of asymptomatic hardware. Removal can be costly for individual patients as well as the health care system. In fact, Boulos et al 2 estimated the typical cost for pediatric orthopaedic hardware removal to be more than $11 000. However, other clinical studies have suggested hardware removal may improve function and reduce pain.4,8,17,21,22 Cadaveric data has suggested that the removal of hardware consisting of epiphyseal screws placed in the setting of pediatric ankle fractures may decrease interarticular forces within the ankle. 3 Altering these forces may decrease the risk for subsequent joint degeneration or growth disturbances, and it is commonly cited as the rationale for elective hardware removal in pediatric ankle fractures.
A recent study found that hardware was removed in 18% of tibia/fibula fractures in the pediatric population. 2 However, there are no studies assessing the rate of hardware removal specifically after physeal ankle fractures. Additionally, previous studies on pediatric ankle fractures have not evaluated outcomes after hardware removal such as the rate of subsequent procedures. Determining the rate of hardware removal after this injury is critical in educating patients and assessing indications and benefits. In this study, we aimed to determine the rate of hardware removal following surgical management of physeal ankle fractures using a large national database. Furthermore, we analyzed differences in age, sex, race, payor type, predicted income, residence, and rates of subsequent ankle procedures between patients who had hardware removed and hardware retained after index surgery.
Materials and Methods
Data Source
A retrospective cohort study was performed using data from the Pediatric Health Information System database (PHIS). The PHIS database is an administrative database containing data from inpatient, emergency department, ambulatory surgery, and observation level encounters from 49 hospitals across the United States. All contributing hospitals are not-for-profit, tertiary pediatric hospitals. Contributing hospitals work in conjunction with the Children’s Hospital Association (Lenexa, KS) to maintain data quality. Data are deidentified and undergo validity and reliability checks before inclusion in the database.
Population and Selection Criteria
Patients receiving care at PHIS centers were identified through International Classification of Diseases, Tenth Revision (ICD-10), codes. All patients <18 years old who had surgery for a distal tibia physeal fracture were included. We identified these patients by ensuring that each had the appropriate diagnosis and procedure codes. Eligible diagnosis codes included the S89.1 codes for distal tibia physeal fractures. Eligible procedure codes included codes for CRPP or ORIF: 0QSG04Z, 0QSG06Z, 0QSG34Z, 0QSH04Z, 0QSH06Z, 0QSH34Z, 0SSF04Z, and 0SSG04Z. Patients with open fractures and polytrauma were excluded. The main cohort consisted of all patients with index surgery between October 1, 2015, and May 31, 2019, within the PHIS database and included 2 years of follow-up data through May 2021. This cohort was used to assess hardware removal rates and demographics. We also analyzed a subgroup of patients with at least 4 years of follow-up, who were treated between October 1, 2015, and May 31, 2017, to calculate the rate of subsequent procedures following hardware removal. Individual patients are deidentified and assigned record numbers in the PHIS database, which allows for longitudinal analysis of specific patients and the analysis of subsequent procedures.
Variables and Statistical Analysis
The primary outcome measure of this study was the rate of hardware removal following operative management of pediatric distal tibia physeal fractures. Patient demographics included age, sex, race, payor type, predicted income, and geography. Income data provided by PHIS was based on patient zip codes and US Census Bureau data. Bivariate analyses were performed to assess differences related to age, sex, race, payor type, predicted income, geography, and fracture type. Analyses were conducted using χ2, Fisher exact, and t tests. After identifying significant variables in the bivariate analysis, multivariate logistic regression was performed to identify predictors of hardware removal. For the multivariate analysis, age was grouped into categorical bins by age groups <8 years, 8-12 years, and ≥12 years. Income was also grouped into income less than $25 000, $25 000 to $50 000, $50 000 to $75 000, and $75 000 and above. P < .05 was considered statistically significant. All analysis was conducted in Excel (Microsoft, Redmond, WA) and Stata (StataCorp, College Station, TX).
Results
Cohort Demographics
Our initial PHIS search resulted in a cohort of 1138 patients. One hundred twenty-five were excluded for polytrauma and 5 were excluded for open fractures, resulting in a final cohort of 1008 patients (Table 1). Eighty-two percent underwent ORIF and 18% underwent CRPP. The average age at index surgery was 12.6 (SD, 2.2 years; range, 3.5-17.8 years). The majority of the cohort was male (60%), and 62% of patients were White/Caucasian whereas 22% were Black/African American. Approximately 47% of patients had commercial insurance whereas 43% had Medicaid insurance. The geographic distribution was approximately 26% Midwest, 14% Northeast, 39% South, and 21% West. The average predicted household income provided by the PHIS database was $47 331.91 (SD, $18 193.32; range, $12 920–$131 088).
Table 1.
Cohort Demographics (N = 1008).
| Characteristic | Mean ± SD or n (%) |
|---|---|
| Age, y, mean ± SD | 12.6 ± 2.2 |
| Sex | |
| Male | 607 (60) |
| Female | 401 (40) |
| Ethnicity | |
| White | 620 (62) |
| Black | 218 (22) |
| Other/unknown | 170 (17) |
| Payor type | |
| Medicaid | 437 (43) |
| Private insurance | 472 (47) |
| Other | 99 (10) |
| Predicted income, $, mean ± SD | 47 331±18 193 |
| Region | |
| Midwest | 260 (26) |
| Northeast | 144 (14) |
| South | 396 (39) |
| West | 208 (21) |
| Surgery type | |
| ORIF | 826 (82) |
| CRPP | 182 (18) |
Abbreviations: CRPP, closed reduction and percutaneous pinning; ORIF, open reduction internal fixation.
Hardware Removal
Of the patients undergoing surgery for all distal tibia physeal fractures, 24.2% had their hardware removed at a mean of 276 days (SD, 186) following index surgery (Figure 1). Patients with fractures involving the epiphysis (Salter Harris III and IV) had a higher rate of hardware removal compared to patients with fractures not involving the epiphysis (Salter Harris I and II) (28.9% vs 11.7%, P < .01). Patients with epiphyseal fractures also underwent hardware removal earlier than patients with nonepiphyseal fractures (258 vs 318 days, P < .01).
Figure 1.
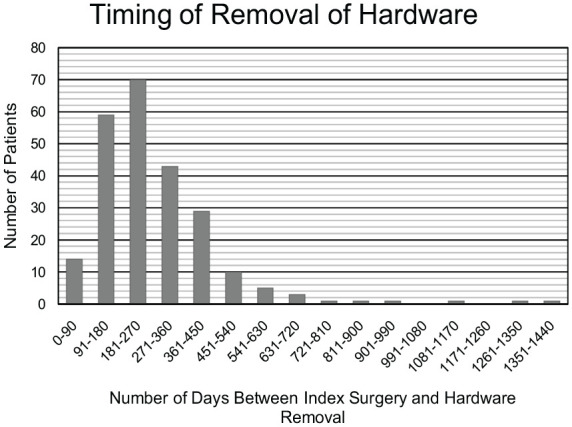
Time from index surgery to hardware removal.
Predictors of Hardware Removal
Univariate analyses demonstrated age and income to be significant predictors of subsequent hardware removal. Specifically, patients with hardware removed had a lower mean age at the time of index procedure compared to patients who did not have their hardware removed (12.0 vs 12.8 years old, P < .01). Patients with hardware removed also had a higher mean predicted income than patients with hardware retained ($49 560 vs $46 621, P = .027). Other demographic variables showed no significant relationship with hardware removal rates (Table 2). In the multivariate analysis, lower age and higher income were both predictors of removal of hardware. Patients under the age of 8 (OR 0.50, 95% CI 0.26-0.96, P = .04) and patients aged 8-12 years (OR 0.29, 95% CI 0.15-0.55, P < .01) were more likely to have hardware removed than patients aged >12 years. Multivariate analysis also showed patients with predicted income greater than $75 000 (OR 3.31, 95% CI 1.41-7.80, P < .01) were more likely to have hardware removed than patients with lower income.
Table 2.
Demographic Information and Univariate Analyses for Predictors of Hardware Removal.
| Hardware Removed, Mean ± SD or n (%) (n=242) |
Hardware Retained, Mean ± SD or n (%) (n=766) |
P Value | |
|---|---|---|---|
| Age, y, mean ± SD | 12.0±2.5 | 12.8±2.1 | <.01 |
| Sex | |||
| Male | 142 (58.7) | 465 (60.7) | NS |
| Female | 100 (41.3) | 301 (39.3) | |
| Ethnicity | |||
| White | 155 (64.0) | 465 (60.7) | |
| Black | 45 (18.5) | 173 (22.6) | NS |
| Other/unknown | 42 (17.4) | 128 (16.7) | |
| Payor type | |||
| Medicaid | 105 (43.4) | 332 (43.3) | |
| Private insurance | 118 (48.8) | 354 (46.2) | NS |
| Other | 19 (7.9) | 80 (10.4) | |
| Predicted income, $, mean ± SD | 49 560±19 114 | 46 621±17 564 | .03 |
| Region | |||
| Midwest | 58 (24.0) | 202 (26.4) | |
| Northeast | 43 (17.8) | 101 (13.2) | NS |
| South | 96 (39.3) | 300 (39.2) | |
| West | 45 (18.6) | 163 (21.3) | |
Abbreviation: NS, nonsignificant.
Subsequent Ankle Procedures
To calculate the rate of subsequent ankle procedures following hardware removal, a subset of patients was identified that underwent index surgery between October 1, 2015, and May 31, 2017, to ensure a minimum of 4 years of follow-up. This resulted in a cohort of 468 patients in which 121 had their hardware removed (25.6%) and 347 had their hardware retained. There was no significant difference in rates of subsequent surgery between patients that did or did not have their hardware removed (3.4% vs 3.7%, P > .05, Figure 2). The most common subsequent procedure in each group was for epiphyseal arrest (Current Procedural Terminology code 27734).
Figure 2.
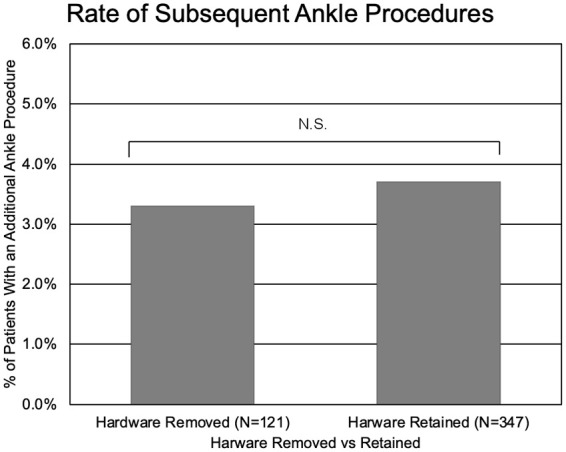
Comparison of rates of additional procedures in patients with hardware removed (3.4%) vs hardware retained (3.7%) (P = .82).
Discussion
Physeal fractures of the distal tibia are among the most common physeal fractures in children.9,10,13,14 Hardware removal has the potential to reduce pain and improve patient satisfaction but remains controversial because of cost and complications associated with additional surgical procedures. Complications associated with hardware removal include refracture, infection, hematoma, wound dehiscence, blood loss, and prolonged operative time. 16 The current study demonstrates a rate of hardware removal of 24.2% in pediatric patients who undergo surgery of physeal ankle fractures. Patients younger than 12 years old or with predicted family annual income greater than $75 000 were more likely to have hardware removed than other groups. Patients with fractures involving the epiphysis were more likely to have their hardware removed than patients with nonepiphyseal fractures.
These results suggest a slightly higher rate of hardware removal for physeal ankle fractures than has been previously shown in the pediatric population. Boulos et al 2 reported that the rate of hardware removal across all injuries treated with surgery in the 10- to 14-year age group was 21% and the rate of hardware removal for tibia/fibula fractures in all pediatric patients was 18%. This observed difference may be related to inherent differences in the databases used for these studies. The current study used the PHIS database and Boulos et al used the Kids’ Inpatient Database (KID). Whereas the KID database includes only inpatient data, the PHIS database includes outpatient data, thereby allowing detection and recording of outpatient hardware removal. Additionally, the currently reported rate of hardware removal is lower than that quoted in the adult literature, which has been reported to be as high as 27%. 12
The rates of subsequent ankle procedures were not significantly different between patients with hardware removed or retained at a minimum of 4 years after index surgery. These findings suggest that leaving hardware in place does not increase the need for further surgeries. Additionally, the current study demonstrates that rates of hardware removal were higher for patients with Salter Harris III and IV type fracture as compared to Salter Harris I and II (28.9% vs 11.7%), which was also consistent with the multivariate analysis. The data are not able to elucidate the cause of this difference; however, one hypothesis is that given Salter Harris III and IV fractures often require more fixation than Salter Harris I and II fractures, this hardware may be more likely to become symptomatic. 3 Further studies looking into specific patient factors are required to further investigate this finding.
The current study also demonstrated that hardware was removed more often in patients with higher predicted income. The multivariate analysis demonstrated that patients with a predicted income greater than $75 000 were >3 times as likely to have hardware removed than patients with lower income. Univariate analysis showed an average of $3000 income gap between patients with hardware removed and hardware retained. This difference represented approximately 6% of the total annual predicted income of these patients. Both groups’ mean predicted income ($46 621–49 560) was roughly the mean personal income in the United States during the study period ($44 510–54 129). 19 Although the current study does not allow for the assessment of causality, it is consistent with prior studies showing association between low income and lower health care specialist utilization. 7 Future work may investigate whether socioeconomics influence the decision to undergo hardware removal as well as access to health care.
The findings from this study have important implications to clinical practice and patient counseling. Specifically, this study allows surgeons to compare their practice to national trends and appropriately counsel patients with this injury. Currently, asymptomatic hardware may occasionally be removed at the family’s request.6,16,20 The current study does not show any significant difference in rates of subsequent procedures involving the surgical extremity irrespective of hardware removal. However, long-term follow-up studies are needed to assess for joint degeneration especially with epiphyseal fixation. Despite the study by Charlton et al 3 showing increased intra-articular pressure with subchondral screws in the distal tibia, additional clinical studies are needed to substantiate these concerns and appropriately counsel patients.
This study has several strengths. This is the first study in the literature assessing the rate of hardware removal following physeal ankle fractures. We included at least 2 years of follow-up, allowing for detection of hardware removal procedures following index surgery. Additionally, the PHIS database includes both inpatient and outpatient data, allowing for detection of outpatient hardware removal procedures, as compared to other studies that focus on inpatient procedures. Lastly, the PHIS database includes data from multiple children’s hospitals across the United States, allowing for generalizability of the current findings.
There are several limitations of the current study. The PHIS database is an administrative database and is therefore susceptible to coding errors, underreporting, and incomplete reporting. This study may underreport the rate of hardware removal and the rate of subsequent procedures because patients may have their hardware removed at a nonparticipating hospital or outside the study period. Additionally, the procedure and diagnosis codes do not allow for the determination of indications for hardware removal (infection, pain, or patient preference). The procedure and diagnosis codes only give broad description of fracture type such as SH-II and SH-III but do not give more specific fracture details. Finally, although we found no difference in rate of additional procedures at 4 years, we are unable to evaluate outcomes at longer time points because of limitations of the PHIS database. Additional longer-term studies using patient-specific clinical, demographic, and radiographic data are needed to better define the risks of leaving hardware in place for pediatric ankle fractures.
In conclusion, this study found that approximately a quarter of all children treated with surgery for ankle fractures undergo hardware removal within 2 years of index surgery. Younger patients, those with higher predicted income, and fractures that involve the epiphysis are more likely to have hardware removed. Rates of subsequent procedures on the operative extremity were not significantly different between patients with hardware removed and hardware retained at a minimum of 4 years after index surgery. Additional multicenter studies using pooled radiographic, demographic, and clinical data are needed to validate the rates of hardware removal, identify indications, and better inform surgical recommendations and patient expectations.
Supplemental Material
Supplemental material, sj-pdf-1-fao-10.1177_24730114231182396 for Rates and Factors Associated With Hardware Removal in Physeal Ankle Fractures: Analysis of the Pediatric Health Information System by Robert J. Pearce, Alejandro Cazzulino and Ishaan Swarup in Foot & Ankle Orthopaedics
Footnotes
Ethical Approval: Ethical approval was not sought for the present study because it involves only deidentified data and does not constitute human subjects research.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Robert J. Pearce, BA,  https://orcid.org/0009-0001-8173-5193
https://orcid.org/0009-0001-8173-5193
References
- 1.Böstman O, Pihlajamäki H.Routine implant removal after fracture surgery: a potentially reducible consumer of hospital resources in trauma units. J Trauma. 1996;41(5):846-849. doi: 10.1097/00005373-199611000-00013 [DOI] [PubMed] [Google Scholar]
- 2.Boulos A, DeFroda SF, Kleiner JE, Thomas N, Gil JA, Cruz AI., Jr.Inpatient orthopaedic hardware removal in children: a cross-sectional study. J Clin Orthop Trauma. 2017;8(3):270-275. doi: 10.1016/j.jcot.2017.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Charlton M, Costello R, Mooney JF, Podeszwa DA.Ankle joint biomechanics following transepiphyseal screw fixation of the distal tibia. J Pediatr Orthop. 2005;25(5):635-640. doi: 10.1097/01.bpo.0000161834.65032.c5 [DOI] [PubMed] [Google Scholar]
- 4.Chu A, Madou MRZ, Sala DA, Chorney GS, Feldman DS.Outcomes analysis after routine removal of implants in healthy pediatric patients. J Pediatr Orthop B. 2009;18(6):381-387. doi: 10.1097/BPB.0b013e32832d5da2 [DOI] [PubMed] [Google Scholar]
- 5.Hanson B, van der Werken C, Stengel D.Surgeons’ beliefs and perceptions about removal of orthopaedic implants. BMC Musculoskelet Disord. 2008;9:73. doi: 10.1186/1471-2474-9-73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loder RT, Feinberg JR. Orthopaedic implants in children: survey results regarding routine removal by the pediatric and nonpediatric specialists. J Pediatr Orthop. 2006;26(4):510-519. doi: 10.1097/01.BPO.0000214924.02939.62 [DOI] [PubMed] [Google Scholar]
- 7.Lueckmann SL, Hoebel J, Roick J, et al. Socioeconomic inequalities in primary-care and specialist physician visits: a systematic review. Int J Equity Health. 2021;20(1):58. doi: 10.1186/S12939-020-01375-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Minkowitz RB, Bhadsavle S, Walsh M, Egol KA.Removal of painful orthopaedic implants after fracture union. J Bone Joint Surg Am. 2007;89(9):1906-1912. doi: 10.2106/JBJS.F.01536 [DOI] [PubMed] [Google Scholar]
- 9.Mizuta T, Benson WM, Foster BK, Paterson DC, Morris LL.Statistical analysis of the incidence of physeal injuries. J Pediatr Orthop. 1987;7(5):518-523. doi: 10.1097/01241398-198709000-00003 [DOI] [PubMed] [Google Scholar]
- 10.Ogden JA.Injury to the growth mechanisms of the immature skeleton. Skeletal Radiol. 1981;6(4):237-253. doi: 10.1007/BF00347197 [DOI] [PubMed] [Google Scholar]
- 11.Olgun ZD, Maestre S.Management of pediatric ankle fractures. Curr Rev Musculoskelet Med. 2018;11(3):475. doi: 10.1007/S12178-018-9510-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Partio N, Huttunen TT, Mäenpää HM, Mattila VM.Reduced incidence and economic cost of hardware removal after ankle fracture surgery: a 20-year nationwide registry study. Acta Orthop. 2020;91(3). doi: 10.1080/17453674.2020.1733749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peterson CA, Peterson HA.Analysis of the incidence of injuries to the epiphyseal growth plate. J Trauma. 1972;12(4):275-281. [DOI] [PubMed] [Google Scholar]
- 14.Peterson HA, Madhok R, Benson JT, Ilstrup DM, Melton LJ.Physeal fractures: part 1. Epidemiology in Olmsted County, Minnesota, 1979-1988. J Pediatr Orthop. 1994;14(4):423-430. doi: 10.1097/01241398-199407000-00002 [DOI] [PubMed] [Google Scholar]
- 15.Prediger B, Mathes T, Probst C, Pieper D.Elective removal vs. retaining of hardware after osteosynthesis in asymptomatic patients-a scoping review. Syst Rev. 2020;9(1):225. doi: 10.1186/s13643-020-01488-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raney EM, Freccero DM, Dolan LA, Lighter DE, Fillman RR, Chambers HG.Evidence-based analysis of removal of orthopaedic implants in the pediatric population. J Pediatr Orthop. 2008;28(7):701-704. doi: 10.1097/BPO.0B013E3181875B60 [DOI] [PubMed] [Google Scholar]
- 17.Reith G, Schmitz-Greven V, Hensel KO, et al. Metal implant removal: benefits and drawbacks – a patient survey. BMC Surg. 2015;15(1):96. doi: 10.1186/S12893-015-0081-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenbaum AJ, DiPreta JA, Uhl RL.Review of distal tibial epiphyseal transitional fractures. Orthopedics. 2012;35(12):1046-1049. doi: 10.3928/01477447-20121120-07 [DOI] [PubMed] [Google Scholar]
- 19.US Census Bureau. Mean personal income in the United States (MAPAINUSA646N) | FRED | St. Louis Fed. Accessed February 21, 2022. https://fred.stlouisfed.org/series/MAPAINUSA646N
- 20.Vos DI, Verhofstad MHJ. Indications for implant removal after fracture healing: a review of the literature. Eur J Trauma Emerg Surg. 2013;39(4):327-337. doi: 10.1007/S00068-013-0283-5 [DOI] [PubMed] [Google Scholar]
- 21.Williams AA, Witten DM, Duester R, Chou LB.The benefits of implant removal from the foot and ankle. J Bone Joint Surg Am. 2012;94(14):1316-1320. doi: 10.2106/JBJS.J.01756 [DOI] [PubMed] [Google Scholar]
- 22.Williams BR, McCreary DL, Parikh HR, Albersheim MS, Cunningham BP.Improvement in functional outcomes after elective symptomatic orthopaedic implant removal. J Am Acad Orthop Surg Glob Res Rev. 2020;4(9):e20.00137. doi: 10.5435/JAAOSGLOBAL-D-20-00137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wuerz TH, Gurd DP.Pediatric physeal ankle fracture. J Am Acad Orthop Surg. 2013;21(4):234-244. doi: 10.5435/JAAOS-21-04-234 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-fao-10.1177_24730114231182396 for Rates and Factors Associated With Hardware Removal in Physeal Ankle Fractures: Analysis of the Pediatric Health Information System by Robert J. Pearce, Alejandro Cazzulino and Ishaan Swarup in Foot & Ankle Orthopaedics


