Abstract
Heart valve leaflet’s aneurysm is a rare finding, and literature about this topic is sparse. Early recognition is important because their rupture can lead to catastrophic valve regurgitation. An 84-year-old male with chronic ischemic cardiomyopathy was admitted to the coronary intensive care unit for non-ST elevation myocardial infarction. Baseline transthoracic echocardiography showed normal biventricular function with inhomogeneous thickening of aortic leaflets with moderate aortic regurgitation. Because the acoustic window was limited, a transesophageal echocardiography was performed, detecting a small mass in the right aortic coronary cusp with moderate regurgitation (orifice regurgitation area: 0.54 cm2; med/max gradient: 16/32 mmHg). Endocarditis was ruled out. Because of the rapid worsening of the patient’s conditions, requiring mechanical ventilation and hemofiltration, and the potential hazard of an urgent coronary angiography, a cardiac computed tomographic angiography was performed. Detailed spatial reconstructions highlighted a bilobed cavitation in the aortic leaflets. Diagnosis of aortic leaflets’ aneurysm was made. A ”wait and see” strategy was chosen, and the patient’s general conditions gradually improved and now he is stable and uneventful. To date, no aortic leaflet’s aneurysm was described in literature.
Keywords: Aortic valve, cardiac computed tomographic angiography, valvular leaflet aneurysm
INTRODUCTION
Valvular aneurysm (VA) is rare entities, and literature about this topic is sparse, principally focusing on the mitral valve. VA formation and rupture are unusual without infectious involvement, in fact, infective endocarditis (IE) is the most common reported cause.[1-3] Connective tissue disorders, myxomatous valve’s degeneration and trauma related to past surgery are other rare causes of valvular aneurysms. Early recognition is important because it may cause catastrophic valve regurgitation.[1,2] Mitral valve aneurysms have a reported incidence of only 0.2%–0.29%, while to our knowledge, no cases of aortic leaflet’s aneurysms have been reported.[2]
We report the first case of an aortic VA detected by cardiac computed tomographic angiography (CCTA).
CASE REPORT
An 84-year-old male with chronic ischemic cardiomyopathy 43 and multiple comorbidities (type 2 diabetes, hypertension, peripheral vasculopathy, multiple cerebral transient ischemic attacks, chronic atrial fibrillation, trifascicular block treated with previous pacemaker implantation) was admitted to coronary intensive care unit for non-ST-elevation myocardial infarction. The patient’s general conditions worsened with progressive renal and respiratory failure, which needed endotracheal intubation and continuous venovenous hemofiltration. Baseline transthoracic echocardiography (TTE) showed normal biventricular sizes and function (left ventricular ejection fraction 62% and end-diastolic volume 60 ml/m2) with an inhomogeneous mass-like thickening of aortic leaflets and moderate aortic regurgitation (AR). A transesophageal echocardiography (TEE) was then performed, detecting two vacuolated masses on the ventricular aspect of the aortic leaflets with rolled-up margins; moderate AR was also confirmed [Figure 1].
Figure 1.
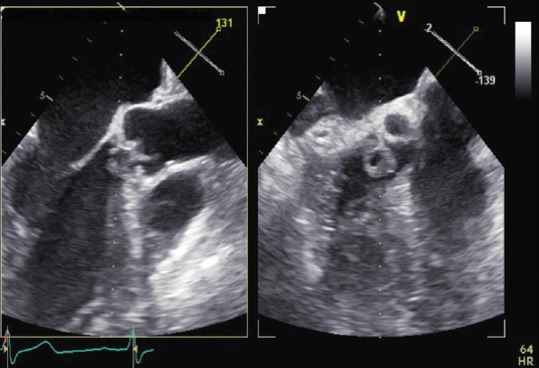
TEE mid-esophageal long and short axis view showing a vacuolated mass on the ventricular aspect of the aortic leaflets with rolled-up margins. TEE: Transesophageal echocardiography
Primary differential diagnosis included valvular neoplasia or IE, but neither fever nor bacterial growth in serial blood cultures was detected; moreover, no immunological or embolic phenomena related to IE were observed. Inflammatory markers (C-reactive protein and procalcitonin) persisted unremarkable, and IE was ruled out.
Given the potential hazard of an urgent coronary angiography, physicians oriented toward a more detailed noninvasive imaging and CCTA was performed by a third generation, 320 mm × 0.5 mm detector row unit (Aquilion ONE ViSION Edition; Toshiba Medical Systems, Otawara, Japan). Data were transferred to an external workstation (Vitrea, Canon Medical Informatics, Inc.), providing multiplane and volume-rendering reconstructions. It was then detected a “bilobed” saccular outpouching of the aortic leaflets, one in the commissure between right-left aortic coronary cusps measuring 8 mm × 9 mm × 12 mm and the other in the left coronary cusp measuring 8 mm × 10 mm × 15 mm [Videos 1 and 2].
Given the original finding, the case was urgently discussed by the local multidisciplinary team. The patient’s conditions were prohibitive for surgery and a “wait and see” strategy was chosen. Patient’s condition gradually improved, and he was successfully extubated with unmodified TTE findings.
DISCUSSION
CCTA is an even more emerging imaging technique for the analysis of cardiac anatomy. Its high spatial resolution and its feasibility in providing detailed anatomical reconstructions make it an excellent tool to get the most accurate cardiologic differentials.[4]
VAs are principally related to IE as the leading cause, but given the rarity of these phenomena, only a few case series have been reported. Galzerano et al. confirmed the main role of IE in the genesis of VA but also reported two patients with VA where no IE was diagnosed, inferring their possible pathogenesis on a remote surgical procedure (left atrial dissection) in one patient, and on degenerative phenomena of the MV bioprosthesis in the other.[5] TEE, integrated by three-dimensional TEE, is the primary imaging tool orienting the differentials toward VA diagnosis, but being the imaging findings uncommon, it is important not to misinterpret the VA features with large vegetations, cystic lesions, or abscess. In our case, these misinterpretations were prevented by the unremarkable physical and laboratory findings; on the other hand, no history of surgical procedure was present. The unusual echocardiographic features need to be detected as early as possible to let the patient have the most suitable intervention.[5]
All the cases described by Galzerano et al. were associated with valve perforation and severe regurgitation together with a high incidence of embolism. All of them required surgery except one that died in medical therapy.[5] Our case, differently from what foreseeable, remained stable with medical therapy. A close TTE monitoring is programmed as there is evidence from the previous report that ysmalaneurysms may rupture, causing severe acute AR.
At the moment, the role of CCTA in the detection of VA remains unknown because of the rareness of these entities. In our situation, CCTA was fundamental to clarify the final diagnosis providing detailed and diagnostic kinetic MPRs, overcoming all the difficulties related to sparse acoustic windows. Anyway, CCTA has a well-established role in the diagnosis of IE and its local complications, with a sensitivity and specificity of 100% when integrated into TEE,[6] and IE was our primary diagnosis. What we can infer from this report is that multimodality CCTA-integrated imaging will be more and more essential in reaching the final diagnosis in those cardiopathies where diagnosis persists unclear at “first-level” tests.
Since the patient had no history of traumas or recent cardiac procedures, our hypothesis is that he may have suffered from previous IE having these two aneurysms as residues.
Ethics statement
This paper was written in accordance with the Declaration of Helsinki.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos avaliable on: https://journals.lww.com/JCEG
REFERENCES
- 1.Tomsic A, Li WW, van Paridon M, Bindraban NR, de Mol BA. Infective endocarditis of the aortic valve with anterior mitral valve leaflet aneurysm. Tex Heart Inst J. 2016;43:345–9. doi: 10.14503/THIJ-15-5322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raval AN, Menkis AH, Boughner DR. Mitral valve aneurysm associated with aortic valve endocarditis and regurgitation. Heart Surg Forum. 2002;5:298–9. [PubMed] [Google Scholar]
- 3.Güler A, Hatipoğlu S, Karabay CY, Kırma C. A rare cause of severe mitral regurgitation: Mitral valve aneurysm. Turk Kardiyol Dern Ars. 2011;39:690–2. doi: 10.5543/tkda.2011.01671. [DOI] [PubMed] [Google Scholar]
- 4.Pergola V, Cabrelle G, De Conti G, Barbiero G, Mele D, Motta R. Challenging cases of aortic prosthesis dysfunction, the importance of multimodality imaging, a case series. Diagnostics (Basel) 2021;11:2305. doi: 10.3390/diagnostics11122305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Galzerano D, Vriz O, Khalil F, Ur Rehman S, Al Amro B, Jazzar Y, et al. Clinical and echocardiographic features of valvular aneurysms. Eur Heart J Cardiovasc Imaging. 2022;23(Suppl 1) doi: https://doi.org/10.1093/ehjci/jeab289.208. [Google Scholar]
- 6.Hryniewiecki T, Zatorska K, Abramczuk E, Zakrzewski D, Szymański P, Kuśmierczyk M, et al. The usefulness of cardiac CT in the diagnosis of perivalvular complications in patients with infective endocarditis. Eur Radiol. 2019;29:4368–76. doi: 10.1007/s00330-018-5965-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


