Abstract
We report a case of ultrasound-guided craniocervical nerve blocks performed with ropivacaine for perioperative local/regional anesthesia in a patient who underwent right partial maxillary resection and neck dissection under general anesthesia. The patient was an 85-year-old woman with multiple medical comorbidities in whom analgesia using nonsteroidal anti-inflammatory drugs and opioids was expected to increase the risk of postoperative complications. Bilateral ultrasound-guided maxillary (V2) nerve blocks and a right superficial cervical plexus block were performed, which provided adequate perioperative anesthesia and avoided postoperative complications. The use of ultrasound-guided craniocervical nerve blocks with ropivacaine can be an effective approach for providing prolonged perioperative local anesthesia and analgesia, minimizing the need for other potentially problematic analgesics.
Keywords: Ultrasound guided, Maxillary nerve block, Superficial cervical plexus block, Postoperative analgesia, General anesthesia, Local regional anesthesia
CASE PRESENTATION
The patient was an 85-year-old woman (height 146 cm; weight 55 kg; body mass index 25 kg/m2) scheduled for right partial maxillary resection and right neck dissection under general anesthesia as treatment for squamous cell carcinoma of the palate. Her medical history included Alzheimer's disease, diabetes mellitus type 2, hypertension, dyslipidemia, C5-C6 cervical spinal stenosis, gastroesophageal reflux disease, and binocular cataracts. In addition, she also had a decreased forced expiratory volume in the first 1 second/forced vital capacity ratio of 67.3%, indicating moderate obstructive lung disease. Ultrasound-guided maxillary (V2) nerve blocks (UGMNBs) for the maxillary resection and a superficial cervical plexus block (SCPB) for neck dissection were planned to minimize the use of nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids. Figures 1 and 2 show the affected surgical areas and effective distribution of the right UGMNB and SCPB planned for this case.
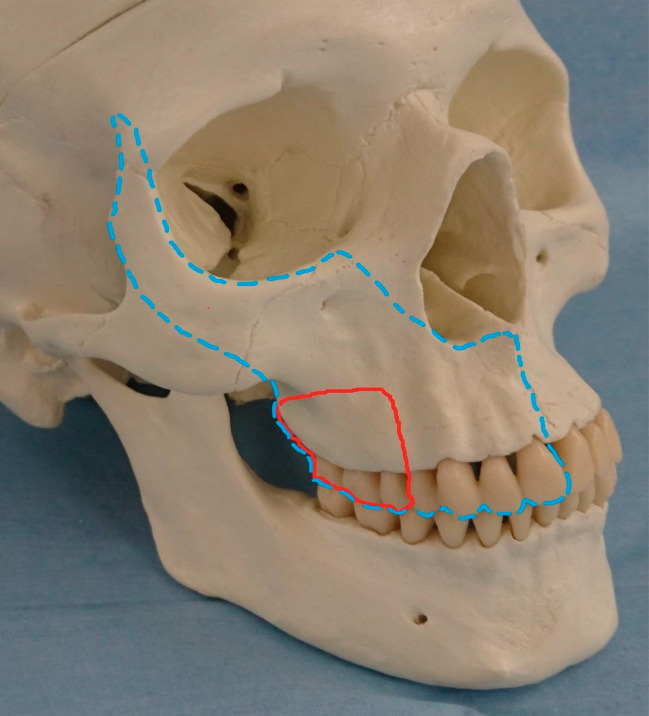
Figure 1.
Right Maxillary Partial Resection and Maxillary (V2) Nerve Block.
The red line indicates the anatomic extent of the right maxillary partial resection. The blue dashed line indicates the effective distribution of the right ultrasound-guided maxillary (V2) nerve block.
Figure 2.
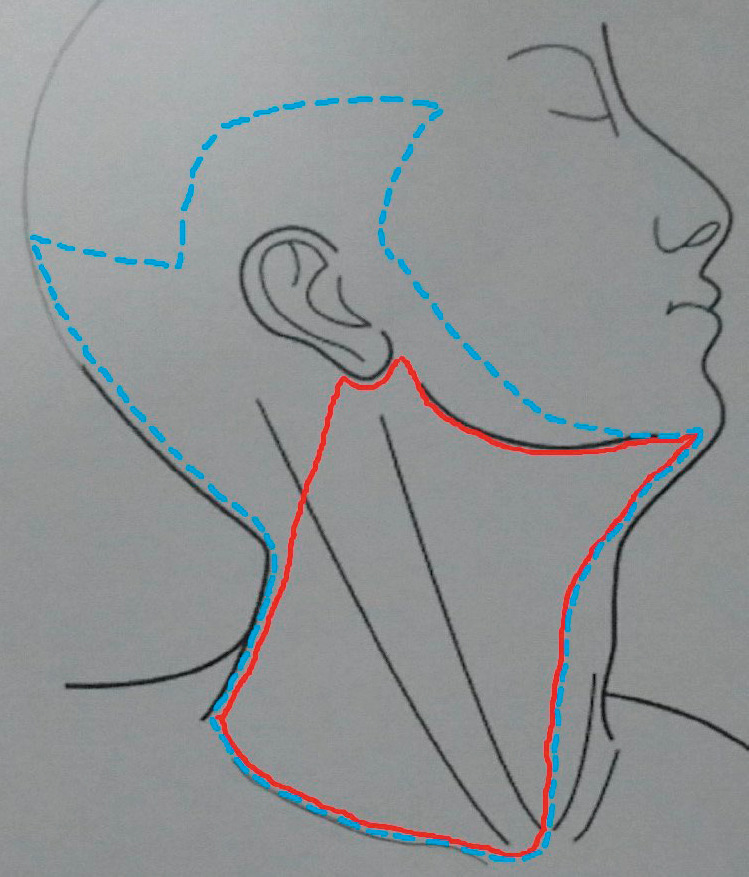
Right Neck Dissection and Superficial Cervical Plexus Block.
The red line indicates the anatomic extent of the planned right neck dissection. The blue dashed line indicates the effective distribution of the right superficial cervical plexus block.
General anesthesia was induced using propofol (30 mg) and rocuronium (40 mg), after which the patient was intubated and the nerve blocks performed. A linear probe for the ultrasound imaging system (SonoSite SII, Fujifilm) was used for guidance during the right UGMNB procedure, which was performed by approaching the pterygopalatine fossa transcutaneously from the zygomatic arch.1 The probe was placed inferior to the zygomatic arch to visualize the maxillary tuberosity and lateral pterygoid plate of the sphenoid bone. The 22-gauge, 80-mm needle (Perican, B. Braun) was inserted at the intersection of the frontal process of the zygomatic bone and zygomatic arch and advanced carefully to avoid damaging the maxillary artery. Normal (0.9%) saline was injected several times during insertion to confirm positioning of the needle tip. When the needle reached the lateral pterygoid plate, 6 mL of 0.375% ropivacaine (22.5 mg) was injected. Because a near-midline incision may be required during tumor resection, a left UGMNB was also performed following the same method.
The right SCPB was performed based on the landmark technique.2 The patient's head was turned to the left, and a 23-gauge, 25-mm needle (NN-2325N, Terumo) was inserted at the posterior border of the sternocleidomastoid muscle at the level of the second cervical vertebra, and 2 mL of 0.375% ropivacaine (7.5 mg) was then injected subcutaneously.
General anesthesia after intubation was maintained with desflurane (4%), oxygen/air (50/50%; 1-2 L/min), and a remifentanil continuous infusion (0.05 μg/kg/min), and fentanyl (100 μg) was administered only at the end of the surgery in case the nerve blocks were unsuccessful. No significant changes in the patient's vital signs were observed intraoperatively.
Upon emerging from general anesthesia, the patient experienced postoperative shivering for a short period, which resolved. Other postoperative complications associated with general anesthesia, such as delirium, nausea, and vomiting, were not observed during recovery. The patient reported no postoperative pain in her right maxilla and neck, and no other analgesics or antiemetics were used postoperatively.
DISCUSSION
Avoiding or reducing the dose of NSAIDs and opioids helps minimize the risk of associated postoperative complications. Potential problems related to NSAIDs may include gastrointestinal and cardiovascular disorders, impaired platelet function, and renal issues, while opioids can cause nausea/vomiting, constipation, drowsiness, delirium/hallucinations, respiratory depression, and hyperalgesia.3 Patient recovery from surgery and their prognosis are more favorable in the absence of such complications.
Ropivacaine has 2 major advantages when used for a nerve block: a prolonged analgesic effect (12-24 hours) and less cardiotoxicity than bupivacaine.4 The ultrasound-guided nerve block techniques used in this case are safe and accurate procedures because they allow real-time visual confirmation of deep anatomical structures and local anesthetic solution delivery as it spreads from the needle tip during injection.5 These benefits help increase the effectiveness of local anesthetics when used for blocks such as an UGMNB and SCPB. Thus, craniocervical nerve blocks performed with ropivacaine under ultrasound guidance can be effective for providing perioperative anesthesia for many invasive oral and maxillofacial surgeries.
This research was originally published in the Journal of the Japanese Dental Society of Anesthesiology, 2022;50:152-154.
REFERENCES
- 1.Sola C, Raux O, Savath L, Macq C, Capdevila X, Dadure C. Ultrasound guidance characteristics and efficiency of suprazygomatic maxillary nerve blocks in infants: a descriptive prospective study. Pediatr Anesth . 2012;22(9):841–846. doi: 10.1111/j.1460-9592.2012.03861.x. [DOI] [PubMed] [Google Scholar]
- 2.Hipskind JE, Ahmed AA. Treasure Island, FL: StatPearls Publishing; 2023. Cervical plexus block. Accessed August 1, 2022. https://www.ncbi.nlm.nih.gov/books/NBK557382/ [PubMed] [Google Scholar]
- 3.Japanese Society for Palliative Medicine. Edited: Pharmacological Treatment Recommendations for Cancer Pain: Clinical Guidelines [in Japanese] Japanese Society for Palliative Medicine. Accessed May 22, 2022. https://www.jspm.ne.jp/files/guideline/pain2020.pdf. [DOI] [PubMed]
- 4.Kojima Y, Furuse K, Murouchi T, Hirabayashi K, Kato M, Oka T. Ultrasound-guided local anesthetic nerve blocks in a forehead flap reconstructive maxillofacial procedure. Anesth Prog . 2020;67(3):164–169. doi: 10.2344/anpr-67-02-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harada S, Takahashi K, Keiko M. Ultrasound-guided nerve blocks (5) practice of nerve blocks in head and neck area: cervical plexus block, stellate ganglion block, greater occipital nerve block [in Japanese] J Jpn Soc Clin Anesth . 2013;33(4):619–628. [Google Scholar]