Abstract
Patients with hypermobile Ehlers Danlos Syndrome often experience psychological distress resulting from the perceived hostility and disinterest of their clinicians. We conducted 26 in-depth interviews with patients to understand the origins of this trauma and how it could be addressed in practice. We found that the cumulative effects of numerous negative encounters lead patients to lose trust in their healthcare providers and the healthcare system, and to develop acute anxiety about returning to clinic to seek further care. We describe this as clinician-associated traumatization. Ultimately, our interviewees described the result of this traumatization as worse – but preventable – health outcomes.
Keywords: Clinician-associated traumatization, Medical trauma, Post-traumatic stress symptoms, Ehlers-Danlos Syndromes, Bioethics, Medical anthropology, In-depth interviews, United States of America, Iatrogenic, Trauma symptoms
1. Introduction
Individuals with chronic conditions may find themselves labeled “difficult patients” by clinicians due to their numerous hospital visits and the amount of time they spend describing their conditions at intake. People affected by hypermobile Ehlers-Danlos Syndrome (hEDS) often suffer from negative treatment due to this and similar labels (Halverson et al., 2021; Bennett et al., 2019; Berglund et al., 2000; Bovet et al., 2016). Hypermobile Ehlers-Danlos Syndrome is a complex, multisystemic condition affecting the connective tissues, and it is characterized by complaints of chronic pain and fatigue, along with many neurological, cardiovascular, and gastrointestinal issues. These features add to the bias that many clinicians harbor against individuals with hEDS as so-called “difficult patients.”
In a previous study on the barriers to diagnosis facing patients with hEDS, many of our interviewees described acute psychological distress resulting from hostility and disinterest that they perceived on the part of their clinicians (Halverson et al., 2021; see also Berglund et al., 2010). The suggestions of trauma resulting from clinical visits was concerning to us from an ethical perspective, but it was also medically worrying, as sequelae of trauma symptoms include nonadherence (Kronish et al., 2012), psychiatric comorbidities (Kessler, 1995), and poorer health status (Ouimette et al., 2004).
Therefore, we set out to conduct further interviews with these patients to understand the origins of their trauma and how that trauma might be addressed. In the present paper, we describe the issue of a specific form of medical trauma we have found in patients with hypermobile Ehlers-Danlos Syndrome, which we refer to as clinician-associated traumatization. This construct describes the physical and psychological effects of negative healthcare encounters on patients that lead them to have aversive responses to people, events, objects, and places that they associate with the index events. We demonstrate that the cumulative effects of traumatic experiences in clinic constitute more than only an epistemic injustice, in which an individual is “wronged specifically in her capacity as a knower” (Fricker, 2017, p. 18), although this also occurs. We establish the pathways by which difficult clinical encounters directly contribute to worse patient–provider relationships, to the patient’s decreased trust in the healthcare system and in themselves, and ultimately, to negative health outcomes. Based on this empirically grounded analysis, we discuss the usefulness as well as the limits of the concept of medical trauma in analyzing the experiences and responses that our interviewees described to us.
1.1. Background
In previous work, we have established how the chronicity of hEDS and the presentation of patients with hEDS predispose them to experience difficult clinical encounters (Halverson et al., 2021). A summary of some of the issues is appropriate to provide the reader with a basic understanding of the issues and the stakes discussed in this paper.
Due to the subjective nature of their symptoms, our interviewees felt that many of their clinicians were overly skeptical of their health complaints, especially those related to pain and fatigue. This led clinicians to be unempathetic and dismissive, they explained, which caused our interviewees to develop self-doubt as well as a fear of seeking medical attention. Two mothers described clinicians who had threatened to call the Department of Child Protective Services (DCPS) or a related state agency and accused them of harming their children by seeking care for their hEDS-related symptoms. As a result of their health needs, patients and their families were exposed to these and other potentially traumatizing situations. One woman even told us that she had been diagnosed by her psychologist with complex post-traumatic stress disorder (PTSD) because of her negative treatment in clinic. In fact, in a recent large survey (N = 503), we found that 33% of respondents with hEDS reported a diagnosis of PTSD, making it the fourteenth most common comorbidity out of the 64 diagnoses about which we queried (Halverson, under review). Moreover, the majority (81%) of the respondents who had received a PTSD diagnosis believed that this was an appropriate construct to explain their symptoms.
It is important to note that many of our participants described situations in which clinicians were not necessarily aware of the harm they were causing. They instead attributed the harm to what they perceived as a lack of education on the rare disease, frustration with its incurability, and inattentiveness as alternative or additional causes of their behavior. A lack of intent, however, did not prevent the clinicians’ attitudes from being traumatizing, alongside the more explicit forms of mistreatment participants described.
1.2. The concept of medical trauma
Since the publication of the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (American Psychiatric Association, 1994), life-threatening medical illness has been listed as a potential trigger for post-traumatic stress disorder, in this instance called medical trauma. This definition was clarified in the DSM-5 (American Psychiatric Association, 2013), in which the trigger of the trauma was specifically limited to a sudden, unexpected, and potentially lethal medical event. Like classic PTSD, the experience of medical trauma has been linked to hyperarousal, avoidance of and numbing to triggers, and the experience of flashbacks (Pothemont et al., 2021).
The DSM-5’s definition of medical trauma is insufficient to describe the triggers that many of our interviewees identified in our initial study. They reported a challenging “diagnostic odyssey,” characterized by repeated negative confrontations with clinicians, persistent and troubling uncertainty about their health status, and a pervasive sense of anxiety and depression, rather than (solely) an unexpected and discrete brush with mortality. Nonetheless, the symptomatology ascribed to medical trauma aligns in suggestive ways with their reports. Our interviewees felt intense psychological and physical distress resulting directly from their medical care. Therefore, we developed an in-depth interview study to examine the specific experiences and their lasting effects on the hEDS population’s engagement with the American healthcare system.
2. Methods
This study evolved out of earlier work on hEDS conducted by our team, in which we identified significant negative affect among patient participants related to their relationship with their clinicians (Halverson et al., 2021). The current study draws on in-depth, qualitative interviews with patients suffering from hEDS which were conducted between December 2020 and April 2021. This study was approved by the Institutional Review Board (IRB) of Indiana University School of Medicine.
We developed an interview guide based on a literature review, as well as on the results of our prior research with this population (Halverson et al., 2021, 2022). In particular, we consulted the literature on PTSD and medical trauma, including instruments designed to measure perceptions of clinician empathy (Hojat & DeSantis, 2017), the therapeutic alliance (Elvins & Green, 2008), and trauma exposure (Carlson et al., 2011; Hooper et al., 2011). The interview guide was divided into three sections. The first assessed participants’ memory and emotional response to one or a small number of difficult clinical encounters. The second investigated long-term or downstream effects of those difficult encounters. In the third section, we asked about general impressions of the clinical care that they had personally received. We additionally collected demographic information, including gender, age, and race and ethnicity. (The interview guide is available upon request from the corresponding author.)
We recruited patients from the Indiana University Ehlers-Danlos Clinic, a major site for research, education, and care for individuals living with EDS. All candidates were at least 18 years of age at the time of the interview, had a clinical diagnosis of hEDS, and were comfortable speaking English. Recruitment continued until thematic saturation was achieved (Strauss & Corbin, 1998). All participants provided written and verbal consent prior to participation in the interviews.
The first author (CMEH) conducted the interviews over the phone and took field notes during the conversations. The interviews were audio-recorded and transcribed verbatim. They were then assigned a random, three-digit identification number, which we provide in parentheses after each quotation. The research team systematically conducted a thematic analysis of the interviews using Dedoose, a mixed-methods analysis tool (Holstein & Gubrium, 1997).
3. Results
Twenty-six individuals completed an interview. The majority were White (N = 24) and female (N = 22), a demographic skew that closely reflects that of the population with a known hEDS diagnosis (Demmler et al., 2019; Voermans et al., 2009). Participants ranged in age from 19 to 60 years old, with a mean of 39 years. Further demographic information about our cohort can be found in Table 1. The in-depth interviews lasted an average of 51 min, with a range of 26 min to one and a half hours.
Table 1.
Demographics (N = 26).
| Gender | |
| Male | 1 (4%) |
| Female | 22 (85%) |
| Nonbinary | 3 (12%) |
| Age | |
| 18–29 | 7 (27%) |
| 30–39 | 7 (27%) |
| 40–49 | 6 (23%) |
| 50–59 | 5 (19%) |
| 60+ | 1 (4%) |
| Average | 39 years |
| Range | 19–60 years |
| Race/Ethnicity | |
| White | 24 (92%) |
| Mixed race | 2 (8%) |
Analysis of the results of our interviews focuses on four main themes: 1) the ubiquity of difficult clinical encounters, 2) the effect of these encounters on the patient–provider relationship, 3) their effect on participants’ trust in the healthcare system as well as in themselves, and 4) resulting negative health outcomes.
3.1. Difficult clinical encounters
The vast majority (85%) of our interviewees were immediately able to identify and describe one or a small, discrete number of encounters with clinicians that they recalled as particularly stressful. For instance, one participant described a negative encounter with an audiologist. Her mother joined us for the interview and described the experience from her perspective. After several hearing tests, she recalls:
“The doctor strolls in, pompous, with five med students. He sits down in his chair and says, ‘She’s faking it.’ I’m like, ‘Excuse me?’ He’s like, ‘She’s completely faking it.’ Now [my daughter’s] crying in this chair with these five med students all looking at her, proclaiming based on her age and her sex – because she was female and at the time, she was like 13 or 14 – that it was typical for them to fake it. I looked at him, and I’m like, ‘We’ve been dealing with this for over a year. She wears hearing aids; she’s had multiple tests. You don’t get it. We’ve had hearing tests at three difference places, and they all come in all the same.’ He was just adamant. […] ‘She’s faking it, and she just needs to stop.’ […] I never went back to him. He then also called the organization associated with the school for the deaf that advocates for kids with hearing loss. […] He went and told them that she was faking it. I don’t even know what would possess someone to be that vindictive and evil!”
(256)
Ultimately, this call prevented her daughter from being admitted to the school, where her disability could have been best accommodated. Another participant described a difficult encounter with a dentist:
“I was probably seven or eight at this point, and the dentist wanted to pull teeth because my mouth was overcrowded and he was doing the numbing, and I kept saying it was hurting and that I could feel it. But he didn’t believe me. And then he got angrier and angrier. He called me a liar. He dragged me into the waiting room where my mom was. And then he finally gave me laughing gas, and that worked fine. […] But yeah, it traumatized me.”
(158)
Even the residual 15% of participants who did not immediately recall a particular, discrete encounter, reported negative experiences with clinicians in general. They merely could not identify a single event that stood out among a crowd of difficult encounters. As one of these individuals expressed, “It is not so much a single instance but several writ large.” She went on to describe one event that she called “a turning point” in her anxiety, but ultimately, she attributed her anxiety to “so many other experiences […] even though they weren’t as dramatic” as the case she described (207).
3.2. Patient–provider relationships
Our participants had come to expect clinicians’ negative attitudes and disbelief. Eighty-nine percent said that they felt clinicians had been disrespectful or unprofessional toward them. Another ninety-two percent said they had felt invalidated by their clinicians. One individual said, “They don’t take you seriously, or they think you’re overbearing or just paranoid” (253). One woman suggested that some of the difficulty in her experience could have been due to misogyny or a generally lower level of trust in women’s abilities to understand their bodies and express their subjective symptoms: “You’re just a tired mommy and you need to rest,” she said, imitating how she felt clinicians spoke to her when she complained of chronic pain (258). Another participant explained, “You’re crying out and asking- begging for help, and then not being believed. And it’s not one doctor; it was many doctors, and then that’s traumatizing in itself” (155).
A smaller, but still disturbingly large, percentage of participants (46%) believed that their clinician had acted punitively toward them. Some described situations such as the case with the audiologist presented above, in which clinicians proactively undertook actions to prevent their patients from pursuing the care or treatments they believed they needed. These individuals felt that clinicians acted overzealously in their role as gatekeepers: “My way or the highway” (201). Most, however, intended something quite different when they described their clinicians as punitive, namely, that when a clinician expressed an inability to care further for the patient, this constituted a sort of punishment in itself. Such dismissal felt like abandonment to these patients, like their clinician was saying “I’m done with you,” as so many had done before (156).
Participants also noted that their clinicians’ perceived lack of empathy negatively affected the patient–provider relationship. Fourteen percent believed that clinicians understood their emotions most of the time or always. A quarter said that when they provided feedback on their clinic visits, it was heeded most of the time or always. In general, our participants narrated experiences that suggested many of their clinicians had not expressed careful attention to their psychological wellbeing and came across as brusque and unaccommodating.
Most participants (71%) acknowledged that their negative feelings toward clinicians were evident in how they behaved toward those clinicians. They recognized that this might contribute in a looping manner to the challenging interpersonal situations they encounter in clinic. Many described consciously trying to moderate their emotions for that reason: “If we were being ourselves or being more authentic, we would be crying […] and yelling,” one participant stated (207). In order to curb the difficulty of her clinic visits, however, this woman explained that she refrained from openly expressing to her clinicians the extent of her discomfort and anxiety.
When clinicians terminated their relationship with our participants either through a referral or more abruptly and finally, many participants experienced this as a form of abandonment (73%). One participant described a clinician who stopped responding to her requests to review particular test results with her: “I called them multiple times. […] No one would call me, and so after a month of that, I just gave up. I’m like, I just need to get over this. It was a terrible experience, because it was actually really traumatic. I see pain and rehab psychology, and I talked about it a lot with [my therapist]. It was just to the point where it was really traumatic to keep thinking about [the test] and worrying about it and being overwhelmed about it” (125).
As was noted above, this abandonment at times could feel punitive to some individuals. Without the consistent support from a clinician over time, they were left to navigate the complex medical bureaucracy on their own. Alone, they were forced to investigate disability benefits and payment options, find transportation and housing when visiting distant healthcare centers, get special needs accommodations, garner appropriate referrals, and appraise the risks and benefits of complementary and alternative medical techniques. One woman summarized this feeling of desertion: When she was told by a clinician whom she had seen for a while and had come to trust, “I really don’t know what to do with you. I’m at a loss,” she wanted to cry out: “I understand that you don’t know what to do, but we can’t just leave me here like this!” (116).
Several participants underscored their belief that the clinicians’ negative attitudes were fundamentally the consequence of their limited understanding of EDS and the limited resources at their disposal to manage the patients’ complaints of pain. However, the boldness with which their clinicians nonetheless acted dismissively and disbelievingly struck the patients as arrogance. “A lot of it is just ignorance, [but that’s] not an excuse for poor behavior” (253). “I’ve been to a lot of doctors who […] this may not be their area of expertise or may not know something, but they may speak on it as if they do” (457). When prompted with a Likert scale (see Fig. 1), 15% said that clinicians in their experience recognized their weaknesses most of the time or always, and 11% said that clinicians were receptive to new information. Overall, participants had the impression that an important source of strife in their clinic visits was clinicians’ lack of humility in encountering a relatively rare disorder about which they often knew little.
Fig. 1.
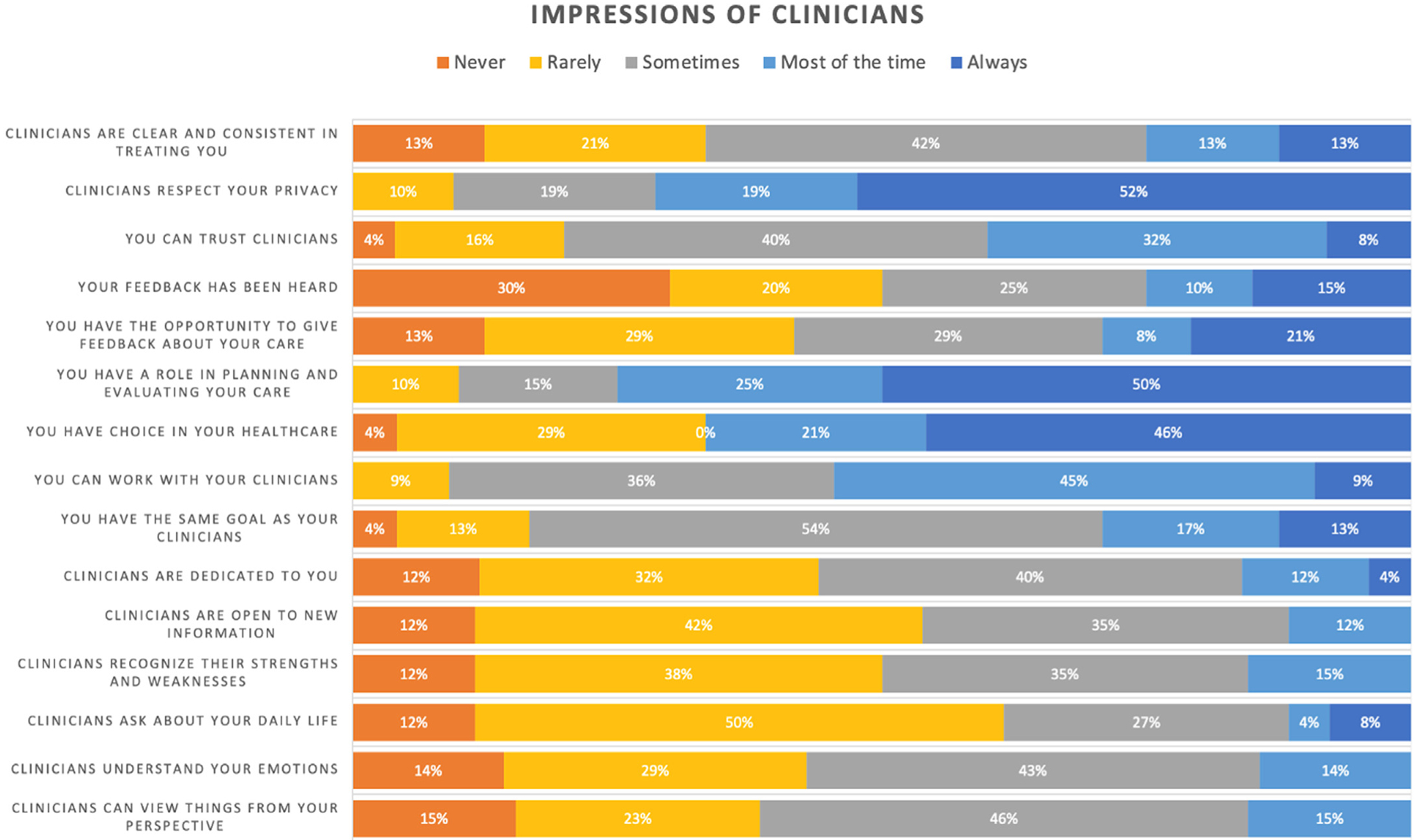
Impressions of clinicians.
The healthcare system itself also appeared as an antagonistic force in our participants’ narratives (96%). They underscored in particular how interacting with the medical bureaucracy had interfered with their ability to live a life apart from healthcare, with raising children and maintaining gainful employment (87%). “I do several treatments a week, so it’s a fulltime job,” one participant explained (253). While we did not prompt participants with specific features of the institution, they listed insurance, disability benefits, referral and record transfer, scheduling, and transportation as significant additional burdens and frustrations. “I’ve been on the phone with insurance for about half my life,” one woman told us (210).
3.3. Trust in healthcare and in the self
Resulting from these negative experiences, many of our interviewees expressed a strong distrust of the medical institution. One interviewee said, “You can’t really trust [clinicians], because you know there’s something going on. You can feel it” (157). Her lack of trust in her clinicians caused clinic visits to seem like “a waste of time.” Although distrust was pervasive, several participants qualified it, saying that they had amassed a team of clinicians in whom they felt they could safely place their confidence. However, each of these individuals still noted a sense of concern or even dismay at the thought of having to see a new clinician who was not part of this already-vetted circle. As one participant explained: “My cardiologist, I would say I trust her right now, but she sat with me and took the time to speak with me. But the other doctors, no,” she contrasted, “You can’t trust them because they’re not listening to you” (156).
Many participants additionally expressed a growing self-doubt, coming to question their own experiences and sensations. One woman described an encounter with a clinician whom she recalled telling her, “I think this is all in your head.” “How would that not make someone doubt themselves, when a medical doctor tells me that he thinks it’s all in my head? […] And I’m like, ‘What if it is? What if I’m just making all this up and I’m just crazy?’” (355).
3.4. Adverse health outcomes
The majority of participants (81%) said that they had experienced negative health outcomes resulting from the inappropriate care they received in clinic. Often, they attributed these adverse events to clinicians’ lack of understanding of EDS and unwillingness to take the participants’ concerns about treatments seriously. For instance, one woman described an encounter in which a clinician prescribed an antibiotic for a sinus infection that made her connective tissue laxer, causing her to wake in the middle of the night, gasping for breath (258). Another participant described the adhesive pads used to conduct a sleep study resulting in lasting scars (457), a common but also easily avoidable consequence of hEDS. And another said she suffered two spinal bleeds from spinal taps that had failed to clot properly (201), a further example of an outcome that someone more knowledgeable about hEDS could have foreseen and prevented.
Many participants stated that they had been treated by numerous physical therapists (PTs) who were too aggressive and inattentive to their physical limitations, causing them to leave sessions in greater pain than they had previously experienced: “Before I found a good PT, pretty much every time I went in there, I felt like I came out worse than I went in” (158). As with the other events described by participants, all of these issues could have been avoided had the clinicians either been more familiar with the medical issues related to EDS or had been willing to heed the concerns expressed by their patients.
Finally, a more opaque but nevertheless negative outcome of these compounding difficult encounters is the emergence of avoidance behaviors in many of our participants. The majority (85%) said that they have avoided specific clinicians with whom they had negative experiences. “I’m kind of at the point where I don’t want to see doctors anymore,” said one woman (150). “I don’t want to keep going there and being made to feel like I’m crazy, or nothing’s wrong with me, or I’m a hypochondriac” one woman explained (157). Another 85% stated that they have additionally avoided clinical care in general. “We took time off; we stopped searching,” one participant said of the sense of resignation she experienced in the midst of her diagnostic odyssey (156). Most acute for our interviewees was the fear of seeing new clinicians, whose attitudes toward EDS were as yet unknown to them. However, even the anticipation of seeing known, “nice doctors” could send at least one young woman into a panic and prevent her from sleeping (207), so significant was the cumulative weight of the other, difficult encounters. Strikingly, eight participants expressed – unprompted – that they had previously been suicidal as the result of unmanaged pain for which they felt no hope of treatment and for which they felt too despondent and anxious to seek further care.
Of the two participants who provided the block quotes at the beginning of this section, the first refuses to return to see any audiologist and experiences panic-like symptoms even simply walking past hearing aids at a retail store, and thus her legal deafness remains clinically unmanaged. The second has developed a fear of dentists so severe that she has not had her teeth cleaned in decades. Others made similar comments about avoiding medical care altogether.
Moreover, many participants (68%) said that when they manage to convince themselves to see a clinician, they nonetheless have avoided talking about their diagnosis of EDS for fear of the stigma and bias they feel that it can engender. “I think there’s a stereotypical EDS patient that some doctors have in their head,” one woman explained, “and [it’s] not a very gracious interpretation. I see it as a hysterical woman who is a hypochondriac” (201). Even when our participants chose to disclose their diagnosis, they noted that they downplayed their symptoms for fear of being treated like “just a crazy person […] I’ll be in a lot of pain, but I’ll pretend I’m not” (207).
4. Discussion
In this article, we have investigated the experiences of hEDS patients with difficult clinical encounters and their responses to them. This study builds on previous findings that show trauma symptoms in patients experiencing chronic illness and frequent healthcare visits, as well as medical trauma in individuals who have undergone longer term in-patient treatment (Hatch et al., 2011; Unseld et al., 2019; Valsø et al., 2020; Wade et al., 2012). These studies have found that prolonged hospital stays themselves frequently result in long-lasting psychiatric morbidity, including increased anxiety, depression, and somatic complaints triggered by the stay, rather than by health events preceding admission. However, our work illustrates the qualitative, lived experiences that lead to trauma symptoms. In particular, we show that it is not merely the hospital setting, the medical interventions, or the disease process that leads to this trauma. Instead, we have found that compounding negative interactional dynamics with healthcare providers result in what we call clinician-associated traumatization, which parallels the symptoms of more traditional conceptualizations of PTSD and medical trauma.
Specifically, we found that patients regularly experience intrusive thoughts and emotions related to their negative clinical encounters. They persistently avoid specific clinicians, general healthcare settings, and sometimes more distal triggers such as the hearing-aid aisle at retail stores. They experience fear, shame, anhedonia, and exaggerated negative beliefs about themselves and those around them. And they are irritable and hypervigilant, even without a specific or present threat. In many ways, as we have said, these symptoms closely parallel the diagnostic criteria for PTSD, and while we are certainly not contradicting our participants who have received this diagnostic label, we believe we are describing something different or additional as well.
We have found trauma symptoms in our participants’ narratives in which sudden, unexpected, and life-threatening medical events are not necessarily present. Rather, our participants’ traumatization results from chronic mistreatment and compounding negative encounters. Some events our participants described struck them immediately as traumatic, while others expressed their trauma as the cumulative outcome of a long series of troubling clinic visits and hospital stays. In fact, some scholars have argued that even the conceptualization of more traditional constructs like PTSD through “the worst single incident” may limit a clinician’s ability to interpret and treat a patient’s symptoms successfully (Priebe et al., 2018).
Our participants expressed a strong distrust of clinicians. The lack of trust they felt is particularly worrisome, as trust in clinicians is positively associated with adherence to recommended protocols (Torresan et al., 2015), accurate and timely diagnosis (Calnan & Rowe, 2006), improved continuity of care (Hall et al., 2002), and greater patient satisfaction (Platonova et al., 2008). As patients in the situations described in our study are already especially vulnerable to adverse health outcomes, harm from something completely manageable and even preventable, such as the interpersonal dynamics of the patient–provider relationship, should strike the reader as both an ethical and a medical concern.
Positive trust has been shown to arise from patients’ perceptions of honesty as well as empathy (Lee et al., 2019), underscoring the importance of clinicians’ compassionate attention to their patients’ emotional lives. Empathy has likewise been shown to improve the therapeutic alliance and improve clinical outcomes on the side of the patient (Canale et al., 2012; Hojat, 2016; Hojat et al., 2011), as well as reduce professional stress and burnout on the side of the clinician (Thirioux et al., 2016). Being empathetic to one’s patient can also prevent the inadvertent retraumatization or triggering of the patient on their path to trauma recovery.
However, a trusting relationship between a patient and a single clinician is not sufficient to repair the effects of institutional betrayal (Smith, 2017). Institutional betrayal is the violation of a patient’s trust that the system will act in the patient’s best interest (Smith & Freyd, 2013). Such betrayal is particularly damaging in cases such as ours, when patients are dependent on and forced to continue to function within the same institution that has betrayed their trust. As one of our participants explained, the compounding effects of other negative encounters made her anxious even to see “nice doctors” (207). In a survey study, only 26.9% of participants with hEDS expressed trust in their healthcare providers (Langhinrichsen-Rohling et al., 2021).
Distrust functions in tandem with self-doubt, what some scholars call “epistemic insecurity” (Medina, 2013). If unaddressed, the inchoate doubt that patients feel in their interpretations of their own experiences can grow into a more fixed and more harmful outlook on themselves and their bodies (El Kassar, 2021). Several participants believed they were “going crazy,” and one even characterized this feeling as a response to “medical gaslighting,” drawing on a phrase popularized by a 2018 Atlantic article (Fetters, 2018) but building on a much longer history of medical invalidation (Dusenbery, 2018). Such self-doubt can lead patients into isolation, further increasing their vulnerability (Halverson, under review; Clark & Knight, 2017; Kidd & Carel, 2017). It has led many of our interviewees to avoid discussing what they perceive to be a stigmatizing diagnosis, and – as we show elsewhere – to an unwillingness or inability to give complete and accurate reports of their symptoms (Halverson et al., 2022; see also Bennett et al., 2019).
Distrust in one’s own understanding of his or her experiences has been described as a form of epistemic injustice (Blease et al., 2017; Byskov, 2021; Fricker, 2017). In particular, many of our interviewees felt unfairly disenfranchised from contributing their insight and knowledge to healthcare decisions that were directly relevant to them. As EDS is a rare syndrome about which many patients have spent significant time and resources educating themselves, an EDS-naïve clinician’s refusal to listen to his or her patient’s understanding of the disease can do more than simply invalidate that patient: It can lead to medical harm based on uninformed decision making.
As mentioned in the Introduction, two participants in our initial study described encounters with DCPS or a related state agency after being accused of harming their children by pursuing medical care for hEDS. While these accusations were certainly traumatizing events for both families, DCPS has actually removed children from their parents in some similar cases. One of the authors (CAF) served as an expert witness on a legal case of “suspected Munchausen by proxy syndrome” (Weber, 2008), now called factitious disorder imposed on another (FDIA). In this case, four children were removed from their family home and placed in foster families because a clinician worried that the mother was pursuing inappropriate medical care for her daughter. After a lengthy trial, the judge concluded that the accusation against the mother was “worthless,” saying her accuser either was “careless, or she has an agenda.” Despite this otherwise positive outcome, the family had been publicly disparaged by the legal case, and the hospital sent their insurer a letter saying the family was disruptive and would therefore no longer be seen for treatment there. All four of the children and the parents have separately expressed a feeling of being acutely traumatized by these events.
While such stories “ripped from the headlines” may be obvious sources of trauma, we have additionally seen how the incremental accumulation of less overtly negative encounters can have lasting adverse psychosocial effects on patients. It is critical that clinicians attune themselves to these potentially “inadvertent […] slights” (Lilienfeld, 2017) and invalidations (Kool et al., 2010), as well. We have found that the construct of medical trauma does not entirely capture the experiences and attitudes of our participants. Most distinctively, our participants – even the majority who recalled with distress one or a small, discrete number of difficult clinical encounters – suffered from cumulative insult and frustration. However, the sequelae of clinician-associated traumatization parallel those of the more traditional construct of PTSD.
For patients with syndromes characterized by chronic pain, including hEDS, findings such as ours are particularly important, as research has demonstrated that trauma symptoms both exacerbate and are exacerbated by chronic pain (Beck & Clapp, 2011). And for our predominantly female patient population, it is noteworthy that women may be more likely than men to develop persistent trauma symptoms, even when exposed to the same event (Christiansen & Hansen, 2015). Our data demonstrate the contributory role that invalidating and dismissive comments – which are a significant issue faced by many patients with fibromyalgia and rheumatic diseases (Kool et al., 2010) – play in both negative psychosocial and physical outcomes.
4.1. Limitations
This study demonstrates the impact of negative clinical encounters on patients’ current attitudes toward their health and healthcare. However, their narratives are based on their subjective recall ability, which is simultaneously a limitation and highly informative as to how they have made sense of their experiences and how those experiences affect their current decision-making practices. An additional limitation of our study is that our sample was largely White and female. This reflects the demographics of the population of individuals with an official clinical diagnosis of hEDS, and is thus potentially more generalizable, but it also means that we have not necessarily captured the breadth of experiences of patients with other demographic characteristics, some of whom we might expect to have experienced even more traumatic clinical encounters (Satcher & Dawes, 2021). Finally, though our participants lived in cities and towns spread across the United States and their stories related experiences from numerous institutions, they were recruited from a single academic medical center. In this way as well, they may not be representative of the whole population.
5. Conclusion and future directions
Medical trauma is conceptualized as a form of PTSD triggered by a sudden, unexpected, and potentially lethal medical event (American Psychiatric Association, 2013). In this study, we analyzed the usefulness and limits of the construct of medical trauma to explain the experiences and responses of patients living with hEDS. We have demonstrated that it is not merely that patients suffer epistemic injustice resulting from what they experience as difficult clinical encounters, but that they also directly suffer demonstrably adverse clinical outcomes. Because of the frequency with which many of our interviewees interact with clinicians, even small difficulties can quickly compound, resulting in lasting trauma that leads to worse patient–provider relations, decreased trust in the healthcare system and the self, and adverse health outcomes.
We have found that negative encounters lead to a breakdown in the patient–provider relationship, even when experiences are primarily of inadvertent slights or microinteractional insults and invalidations, due to their cumulative weight. Repeatedly being dismissed as “exaggerating” and “inventing symptoms” causes patients to lose faith in the healthcare system and in their ability to assess and advocate for their own best interests. This results in anxiety about returning to specific clinicians and avoidance of healthcare settings altogether. Ultimately, this means that patients suffering from clinician-associated traumatization experience worse – but preventable – health outcomes.
It is clear that some of the traumatizing behavior reported by our interviewees, though effected by clinicians, was driven by forces operating at the scale of the institution or the healthcare system conceptualized even more broadly. Clinicians labor, of course, within an institutional context that both enables and constrains their repertoires of behaviors. All action in medical settings – as elsewhere – is the result of “distributed decision making” (Clinch & Benson, 2013; Rapley, 2008) and informed by “collectively reinforced, internalised, tacit guidelines” (Gabbay & May 2004). Moreover, separate negative interactions with other avatars of the healthcare institution can compound a patient’s traumatization and color their interpretation of interactions with clinicians. However, we believe that many if not all of the encounters described in this article could have been managed by the clinicians involved in ways that at the least would have decreased their contribution to the patient’s traumatization. While it is important to recognize these actors’ embeddedness within larger infrastructures that limit their freedom to care for their patients, we suggest several ways that they might act to lessen the potential for traumatizing experiences in healthcare encounters:
Educating clinicians about hEDS and similar conditions has the potential to be instrumental in reducing the negative outcomes described in this article. The Ehlers-Danlos Society Extension for Community Health Care Outcomes (EDS ECHO) is just such a program, aimed at increasing the knowledge of EDS for clinicians across specialties. The program has been shown additionally to reduce clinicians’ feelings of being overwhelmed or frustrated by the prospect of caring for this population, which could improve clinician empathy and sensitivity to the issues facing their patients (Hakim et al., 2021; Schubart et al., 2021). An explicit goal of the EDS ECHO program is to create clinician champions willing and able, not only to care for, but also to advocate for their patients. Such advocacy is particularly important for patients who feel invalidated and traumatized and may not be able to speak up for themselves. (That said, EDS ECHO also offers programing for lay members of the EDS community to develop advocacy skills.) Education that builds clinician humility – in particular, an openness to other ideas and experiences and an emphasis on listening attentively to one’s patients’ complaints – may also significantly improve patient satisfaction and trust (Huynh, 2020).
Regardless of what psychological construct best captures the experiences and attitudes of our interviewees, it is clear that there are numerous, cascading iatrogenic effects from their difficult interactions with clinicians. One participant, however, reframed her own history: “We could define an EDS patient who has not been properly diagnosed over the years as a trauma survivor,” she said (421). While she has never sought an official diagnosis of PTSD or any other related construct, she has pursued trauma therapy as a way of dealing with the fear of clinicians that she had developed over a lifetime of regular hospital visits: Now, “the past is definitely in the past, and I can talk to you about it without tearing up or getting emotional. I can laugh about it. There was a time when I couldn’t even get the words out, it was so painful. I wonder for other folks that have been mistreated, I wonder if they would respond to trauma therapy, too. […] I went through trauma recovery, and I don’t have white coat syndrome anymore. I don’t fear them.”
In closing with this quotation, we would like to suggest that the experiences described by our interviewees certainly represent actual traumas. Treating them as such may underscore both the severe sequelae of indelicate behavior on the part of clinicians and the healing potential of therapies that have been developed for more traditionally recognized forms of trauma. Future research is needed to explore the role that trauma therapy could play in repairing the patient–provider relationship in this population. Future research should also seek to determine whether the findings in our population also arise in other populations with conditions characterized by chronic pain and frequent and challenging clinic visits.
Acknowledgements:
The authors gratefully acknowledge all the individuals who participated in our interviews. This publication was made possible with support from Grant Number, UL1TR002529 (Sharon M. Moe and Sarah E. Wiehe, co-PIs) from the National Institutes of Health, National Center for Advancing Translational Sciences, Clinical and Translational Sciences, Clinical and Translational Sciences Award. It was further supported by the Indiana Clinical and Translational Sciences Institute (IU Grand Challenges Program), the Precision Health Initiative at Indiana University, the Ehlers-Danlos Society, and the IU Health Foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Declaration of competing interest
The authors have no conflicts of interest to disclose.
References
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, D.C: Author. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Beck JG, & Clapp JD (2011). A different kind of comorbidity: Understanding posttraumatic stress disorder and chronic pain. Psychological Trauma: Theory, Research, Practice, and Policy, 3, 101–108. 10.1037/a0021263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett SE, Walsh N, Moss T, & Palmer S (2019). The lived experience of joint hypermobility and ehlers-danlos syndromes: A systematic review and thematic synthesis. Physical Therapy Reviews, 24, 12–28. 10.1080/10833196.2019.1590674 [DOI] [Google Scholar]
- Berglund B, Anne-Cathrine M, & Randers I (2010). Dignity not fully upheld when seeking health care: Experiences expressed by individuals suffering from Ehlers–Danlos syndrome. Disability & Rehabilitation, 32, 1–7. 10.3109/09638280903178407 [DOI] [PubMed] [Google Scholar]
- Berglund B, Nordstrom G, & Lützen K (2000). Living a restricted life with ehlers-danlos syndrome (EDS). International Journal of Nursing Studies, 37, 111–118. [DOI] [PubMed] [Google Scholar]
- Blease C, Carel H, & Geraghty K (2017). Epistemic injustice in healthcare encounters: Evidence from chronic fatigue syndrome. Journal of Medical Ethics, 43, 549–557. 10.1136/medethics-2016-103691 [DOI] [PubMed] [Google Scholar]
- Bovet C, Carlson M, & Taylor M (2016). Quality of life, unmet needs, and iatrogenic injuries in rehabilitation of patients with Ehlers-Danlos Syndrome hypermobility type/Joint Hypermobility Syndrome. American Journal of Medical Genetics, Part A, 170A, 2044–2051. [DOI] [PubMed] [Google Scholar]
- Byskov MF (2021). What makes epistemic injustice an “injustice”. Journal of Social Philosophy, 52, 114–131. 10.1111/josp.12348 [DOI] [Google Scholar]
- Calnan M, & Rowe R (2006). Researching trust relations in health care: Conceptual and methodological challenges – an introduction. Journal of Health, Organisation and Management, 20, 349–358. 10.1108/14777260610701759 [DOI] [PubMed] [Google Scholar]
- Canale SD, Louis DZ, Maio V, Wang X, Rossi G, Hojat M, & Gonnella JS (2012). The relationship between physician empathy and disease complications: An empirical study of primary care physicians and their diabetic patients in parma, Italy. Academic Medicine, 87, 1243–1249. 10.1097/ACM.0b013e3182628fbf [DOI] [PubMed] [Google Scholar]
- Carlson EB, Smith SR, Palmieri PA, Dalenberg C, Ruzek JI, Kimerling R, Burling TA, & Spain DA (2011). Development and validation of a brief self-report measure of trauma exposure: The Trauma History Screen. Psychological Assessment, 23, 463–477. 10.1037/a0022294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christiansen DM, & Hansen M (2015). Accounting for sex differences in PTSD: A multi-variable mediation model. European Journal of Psychotraumatology, 6, Article 26068. 10.3402/ejpt.v6.26068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark CJ, & Knight I (2017). A humanisation approach for the management of joint hypermobility syndrome/ehlers-danlos syndrome-hypermobility type (JHS/EDS-HT). International Journal of Qualitative Studies on Health and Well-Being, 12, Article 1371993. 10.1080/17482631.2017.1371993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clinch M, & Benson J (2013). Making information ‘relevant’: General Practitioner judgments and the production of patient involvement. Social Science & Medicine, 96, 104–111. 10.1016/j.socscimed.2013.07.034 [DOI] [PubMed] [Google Scholar]
- Demmler JC, Atkinson MD, Reinhold EJ, Choy E, Lyons RA, & Brophy ST (2019). Diagnosed prevalence of ehlers-danlos syndrome and hypermobility spectrum disorder in wales, UK: A national electronic cohort study and case–control comparison. BMJ Open, 9, Article e031365. 10.1136/bmjopen-2019-031365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dusenbery M (2018). Doing harm: The truth about how bad medicine and lazy science leave women dismissed, misdiagnosed, and sick. New York: HarperOne. [Google Scholar]
- El Kassar N (2021). The powers of individual and collective intellectual self-trust in dealing with epistemic injustice. Social Epistemology, 35, 197–209. 10.1080/02691728.2020.1839592 [DOI] [Google Scholar]
- Elvins R, & Green J (2008). The conceptualization and measurement of therapeutic alliance: An empirical review. Clinical Psychology Review, 28, 1167–1187. 10.1016/j.cpr.2008.04.002 [DOI] [PubMed] [Google Scholar]
- Fetters A (2018). The doctor doesn’t listen to her. The Atlantic: But the Media Is Starting To. [Google Scholar]
- Fricker M (2017). Evolving concepts of epistemic injustice. In Kidd IJ, Medina J, & Pohlhaus G (Eds.), The routledge handbook of epistemic injustice. Routledge (1 [edition, pp. 53–60). New York: Routledge. 10.4324/9781315212043-5,2017. [DOI] [Google Scholar]
- Gabbay J, & May A. le (2004). Evidence based guidelines or collectively constructed “mindlines?” Ethnographic study of knowledge management in primary care. BMJ, 329, 1013. 10.1136/bmj.329.7473.1013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakim A, Schubart J, Francomano C, Bascom R, & Bloom L (2021). EDS ECHO: Virtual case based learning in the assessment and management of ehlers-danlos syndrome and hypermobility spectrum disorders. Rheumatology, 60, keab247. 10.1093/rheumatology/keab247.082,082. [DOI] [Google Scholar]
- Hall MA, Zheng B, Dugan E, Camacho F, Kidd KE, Mishra A, & Balkrishnan R (2002). Measuring patients’ trust in their primary care providers. Medical Care Research and Review, 59, 293–318. 10.1177/1077558702059003004 [DOI] [PubMed] [Google Scholar]
- Halverson CME Loneliness and social isolation: Physical symptoms leading to the erosion of a support network. In Francomano CA, Hakim AJ, & Henderson FC (Eds.), Symptomatic: The Symptom-Based Handbook for EDS and Hypermobility. Elsevier. [Google Scholar]
- Halverson CME, Clayton EW, Garcia Sierra A, & Francomano C (2021). Patients with Ehlers-Danlos syndrome on the diagnostic odyssey: Rethinking complexity and difficulty as a hero’s journey. American Journal of Medical Genetics, 187, 416–424. 10.1002/ajmg.c.31935 [DOI] [PubMed] [Google Scholar]
- Halverson CME, Kroenke K, Penwell HL, & Francomano CA (2022). Evolving attitudes toward numeric pain assessment among patients with hypermobile Ehlers-Danlos Syndrome: A qualitative interview study. Pain Medicine, 167. https://doi.org.proxy.ulib.uits.iu.edu/10.1093/pm/pnac167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halverson CME, Penwell HL, Perkins SM, & Francomano CA. (under review). Comorbidity, misdiagnoses, and the diagnostic odyssey in patients with hypermobile Ehlers-Danlos Syndrome. Genetics in Medicine. [Google Scholar]
- Hatch R, McKechnie S, & Griffiths J (2011). Psychological intervention to prevent ICU-related PTSD: Who, when and for how long? Critical Care, 15, 141. 10.1186/cc10054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hojat M (2016). Empathy in health professions education and patient care. Cham: Springer International Publishing. 10.1007/978-3-319-27625-0 [DOI] [Google Scholar]
- Hojat M, & DeSantis J (2017). Patient perceptions of clinician’s empathy. Journal of Patient Experience, 4, 78–83. 10.1177/2374373517699273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, & Gonnella JS (2011). Physiciansʼ empathy and clinical outcomes for diabetic patients. Academic Medicine, 86, 359–364. 10.1097/ACM.0b013e3182086fe1 [DOI] [PubMed] [Google Scholar]
- Holstein JA, & Gubrium JF (1997). Active interviewing. In Qualitative research: Theory, method and practice (pp. 113–129). London: Sage Publications. [Google Scholar]
- Hooper LM, Stockton P, Krupnick JL, & Green BL (2011). Development, use, and psychometric properties of the trauma history questionnaire. Journal of Loss & Trauma, 16, 258–283. 10.1080/15325024.2011.572035 [DOI] [Google Scholar]
- Huynh HP (2020). Humble doctors, healthy patients? Exploring the relationships between clinician humility and patient satisfaction, trust, and health status. Patient Education and Counseling, 7. [DOI] [PubMed] [Google Scholar]
- Kessler RC (1995). Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry, 52, 1048. 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- Kidd IJ, & Carel H (2017). Epistemic injustice and illness. Journal of Applied Philosophy, 34, 172–190. 10.1111/japp.12172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kool MB, van Middendorp H, Lumley MA, Schenk Y, Jacobs JWG, Bijlsma JWJ, & Geenen R (2010). Lack of understanding in fibromyalgia and rheumatoid arthritis: The illness invalidation inventory (3*I). Annals of the Rheumatic Diseases, 69, 1990–1995. 10.1136/ard.2009.123224 [DOI] [PubMed] [Google Scholar]
- Kronish IM, Edmondson D, Li Y, & Cohen BE (2012). Post-traumatic stress disorder and medication adherence: Results from the mind your heart study. Journal of Psychiatric Research, 46, 1595–1599. 10.1016/j.jpsychires.2012.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langhinrichsen-Rohling J, Lewis CL, McCabe S, Lathan EC, Agnew GA, Selwyn CN, & Gigler ME (2021). They’ve been BITTEN: Reports of institutional and provider betrayal and links with ehlers-danlos syndrome patients’ current symptoms, unmet needs and healthcare expectations. Therapeutic Advances in Respiratory Disease, 2, Article 263300402110220. 10.1177/26330040211022033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee TH, McGlynn EA, & Safran DG (2019). A framework for increasing trust between patients and the organizations that care for them. JAMA, 321, 539. 10.1001/jama.2018.19186 [DOI] [PubMed] [Google Scholar]
- Lilienfeld SO (2017). Microaggressions: Strong claims, inadequate evidence. Perspectives on Psychological Science, 12, 138–169. 10.1177/1745691616659391 [DOI] [PubMed] [Google Scholar]
- Medina J (2013). The epistemology of resistance: Gender and racial oppression, epistemic injustice, and the social imagination. Oxford University Press. 10.1093/acprof:oso/9780199929023.001.0001 [DOI] [Google Scholar]
- Ouimette P, Cronkite R, Henson BR, Prins A, Gima K, & Moos RH (2004). Posttraumatic stress disorder and health status among female and male medical patients. Journal of Traumatic Stress, 17, 1–9. 10.1023/B:JOTS.0000014670.68240.38 [DOI] [PubMed] [Google Scholar]
- Platonova EA, Kennedy KN, & Shewchuk RM (2008). Understanding patient satisfaction, trust, and loyalty to primary care physicians. Medical Care Research and Review, 65, 696–712. 10.1177/1077558708322863 [DOI] [PubMed] [Google Scholar]
- Pothemont K, Quinton S, Jayoushe M, Jedel S, Bedell A, Hanauer SB, Mutlu EA, & Taft TH (2021). Patient perspectives on medical trauma related to inflammatory bowel disease. Journal of Clinical Psychology in Medical Settings. 10.1007/s10880-021-09805-0 [DOI] [PubMed] [Google Scholar]
- Priebe K, Kleindienst N, Schropp A, Dyer A, Krüger-Gottschalk A, Schmahl C, Steil R, & Bohus M (2018). Defining the index trauma in post-traumatic stress disorder patients with multiple trauma exposure: Impact on severity scores and treatment effects of using worst single incident versus multiple traumatic events. European Journal of Psychotraumatology, 9, Article 1486124. 10.1080/20008198.2018.1486124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapley T (2008). Distributed decision making: The anatomy of decisions-in-action: Doctor-patient relationships and distributed decision making. Sociology of Health & Illness, 30, 429–444. 10.1111/j.1467-9566.2007.01064.x [DOI] [PubMed] [Google Scholar]
- Satcher D, & Dawes DE (2021). Race and the patient-physician relationship in 2021. JAMA, 326, 595–596. 10.1001/jama.2021.12454 [DOI] [PubMed] [Google Scholar]
- Schubart JR, Bascom R, Francomano CA, Bloom L, & Hakim AJ (2021). Initial description and evaluation of EDS ECHO: An international effort to improve care for people with the Ehlers-Danlos syndromes and hypermobility spectrum disorders. American Journal of Medical Genetics, 187, 609–615. 10.1002/ajmg.c.31960 [DOI] [PubMed] [Google Scholar]
- Smith C (2017). First, do no harm: Institutional betrayal and trust in health care organizations. JMDH, 10, 133–144. 10.2147/JMDH.S125885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith CP, & Freyd JJ (2013). Dangerous safe havens: Institutional betrayal exacerbates sexual trauma: Institutional betrayal exacerbates sexual trauma. Journal of Traumatic Stress, 26, 119–124. 10.1002/jts.21778 [DOI] [PubMed] [Google Scholar]
- Strauss A, & Corbin J (1998). Basics of qualitative research: Techniques and procedures for developing grounded theory (2nd ed.). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Thirioux B, Birault F, & Jaafari N (2016). Empathy is a protective factor of burnout in physicians: New neuro-phenomenological hypotheses regarding empathy and sympathy in care relationship. Frontiers in Psychology, 7. 10.3389/fpsyg.2016.00763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torresan MM, Garrino L, Borraccino A, Macchi G, De Luca A, & Dimonte V (2015). Adherence to treatment in patient with severe cancer pain: A qualitative enquiry through illness narratives. European Journal of Oncology Nursing, 19, 397–404. 10.1016/j.ejon.2015.01.001 [DOI] [PubMed] [Google Scholar]
- Unseld M, Krammer K, Lubowitzki S, Jachs M, Baumann L, Vyssoki B, Riedel J, Puhr H, Zehentgruber S, Prager G, Masel EK, Preusser M, Jaeger U, & Gaiger A (2019). Screening for post-traumatic stress disorders in 1017 cancer patients and correlation with anxiety, depression, and distress. Psycho-Oncology, 28, 2382–2388. 10.1002/pon.5239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valsø Å, Rustøen T, Skogstad L, Schou-Bredal I, Ekeberg Ø, Småstuen MC, Myhren H, Sunde K, & Tøien K (2020). Post-traumatic stress symptoms and sense of coherence in proximity to intensive care unit discharge. Nursing in Critical Care, 25, 117–125. 10.1111/nicc.12466 [DOI] [PubMed] [Google Scholar]
- Voermans NC, van Alfen N, Pillen S, Lammens M, Schalkwijk J, Zwarts MJ, van Rooij IA, Hamel BCJ, & van Engelen BG (2009). Neuromuscular involvement in various types of Ehlers-Danlos syndrome. Annals of Neurology, 65, 687–697. 10.1002/ana.21643 [DOI] [PubMed] [Google Scholar]
- Wade DM, Howell DC, Weinman JA, Hardy RJ, Mythen MG, Brewin CR, Borja-Boluda S, Matejowsky CF, & Raine RA (2012). Investigating risk factors for psychological morbidity three months after intensive care: A prospective cohort study. Critical Care, 16, R192. 10.1186/cc11677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber T (2008). Maternal care – or harm? Los angeles times.


