Abstract
Toxic aggregated amyloid-β accumulation is a key pathogenic event in Alzheimer’s disease. Treatment approaches have focused on the suppression, deferral, or dispersion of amyloid-β fibers and plaques. Gene therapy has evolved as a potential therapeutic option for treating Alzheimer’s disease, owing to its rapid advancement over the recent decade. Small interfering ribonucleic acid has recently garnered considerable attention in gene therapy owing to its ability to down-regulate genes with high sequence specificity and an almost limitless number of therapeutic targets, including those that were once considered undruggable. However, lackluster cellular uptake and the destabilization of small interfering ribonucleic acid in its biological environment restrict its therapeutic application, necessitating the development of a vector that can safeguard the genetic material from early destruction within the bloodstream while effectively delivering therapeutic genes across the blood-brain barrier. Nanotechnology has emerged as a possible solution, and several delivery systems utilizing nanoparticles have been shown to bypass key challenges regarding small interfering ribonucleic acid delivery. By reducing the enzymatic breakdown of genetic components, nanomaterials as gene carriers have considerably enhanced the efficiency of gene therapy. Liposomes, polymeric nanoparticles, magnetic nanoparticles, dendrimers, and micelles are examples of nanocarriers that have been designed, and each has its own set of features. Furthermore, recent advances in the specific delivery of neurotrophic compounds via gene therapy have provided promising results in relation to augmenting cognitive abilities. In this paper, we highlight the use of different nanocarriers in targeted gene delivery and small interfering ribonucleic acid-mediated gene silencing as a potential platform for treating Alzheimer’s disease.
Key Words: Alzheimer’s disease, amyloid-β, BACE1, gene silencing, gene therapy, nanoparticle, neurotrophins, small interfering ribonucleic acid
Introduction
Alzheimer’s disease (AD) is one of the most prevalent neurodegenerative conditions, is characterized by progressive cognitive decline and impaired memory, and accounts for some 60–80% of late-onset dementia cases worldwide. Hallmarks of AD and essential requirements for its diagnosis are the presence of amyloid-beta protein (Aβ) in the brain as extracellular amyloid plaques and hyperphosphorylated Tau as intraneuronal neurofibrillary tangles (Muralidar et al., 2020). A further omnipresent feature is neuroinflammation. In this regard, the blood-brain barrier (BBB) is largely fundamental in the development and persistence of chronic inflammation in AD (McLarnon et al., 2021). The effective brain removal of neurotoxic Aβ is hampered by the defensive role of the BBB (Li et al., 2021). The accumulation of Aβ in the brain combined with BBB malfunction creates a feedback loop that leads to amyloid oligomers and plaque development (Cai et al., 2018), the triggering of tau hyperphosphorylation and other aberrant cascades and, ultimately, cognitive decline and dementia (de Oliveira et al., 2021). Consequently, many Alzheimer’s treatment strategies have focused on the suppression, deferral, or dispersion of Aβ oligomers, fibrils, and plaques (Sanati et al., 2019). This article reviews nanotechnology-based gene therapy approaches for treating AD across potential targets.
Beta-site amyloid precursor protein cleaving enzyme-1 (BACE1) is critical in generating Aβ, whether in physiological or pathological amounts. BACE1 initiates Aβ monomer production by cleaving amyloid precursor protein (APP) at the β-secretase site. Further cleavage by the γ-secretase complex results in Aβ monomers that can potentially clump together to create toxic oligomers and fibrils, and, ultimately, amyloid plaques (Jiang et al., 2022). BACE1 levels have been reported to be elevated in the autopsy of AD brains, implying that heightened BACE1 increases Aβ formation and drives initial disease progression. The amyloid pathway is most likely responsible for the BACE1 increase, which may then lead to a positive-feedback cycle in AD (Zhao et al., 2007). Golgi-localized γ-ear containing ARF binding protein-3 deficiency is also a leading contender for the mechanism driving the BACE1 rise (Kim et al., 2018).
Numerous declines in the levels of key proteins have been reported in the AD brain, such as endogenous neurotrophic factors whose concentrations are essential to maintaining the health and survival of neurons. For example, the first growth factor identified, nerve growth factor (NGF), acts on basal forebrain cholinergic nerve cells, supporting their physiological function in providing the bulk of acetylcholine release across the hippocampal and cortical regions. In AD, these nerve cells dramatically deteriorate, resulting in cognitive decline (Nyakas et al., 2011). NGF deficiency promotes cholinergic abnormalities (Do Carmo et al., 2021). The findings of phase I clinical studies employing the ex vivo gene therapy technique in 8 individuals with moderate AD (Stage V/VI) were published in 2005 (Tuszynski et al., 2005). Cognitive abilities, brain metabolic activity, and the morphological status of cholinergic neurons were reported to improve in this set of people (Stepanichev et al., 2020), highlighting the promise of gene therapy if used adroitly. Following up on this example, within this review article, we evaluate gene therapy strategies to mitigate AD, the targets chosen, and the technologies applied to optimize the treatment strategy.
Search Strategy
We searched PubMed, Google Scholar, Chinese National Knowledge Infrastructure (CNKI), and Excerpta Medica (EMBASE) databases for articles related to nanotechnology-based gene therapy for treating AD from inception to February 2022. The following search terms were used: (gold nanoparticles or treatment or diagnosis) AND (Alzheimer’s disease) in English.
Inclusion criteria
The inclusion criteria are as follows: (1) The article is an experimental study of AD and nanotechnology-based gene therapy; (2) The article also includes AD and nanotechnology-based gene therapy clinical studies, pharmacy studies, and pharmacokinetic studies.
Exclusion criteria
The following are the exclusion criteria: (1) Failure to report the use of nanotechnology-based gene therapy in AD; (2) failure to report the studies related to pharmaceuticals, clinical trials, toxicity, and pharmacokinetics; (3) Studies reported without a control group; (4) letters, case reports, editorials, clinical guidelines, and comments; (5) repeated publications.
Quality assessment
The quality standards are primarily based on a seven-item modified scale developed collaboratively from the collaborative Approach to Meta-Analysis and Review of Animal Data from Experimental Studies: (1) Peer-reviewed publications; (2) blind evaluation of behavioral results; (3) adequate sample size; (4) compliance with animal welfare laws and regulations; (5) declaration of potential conflicts of interest; (6) temperature control; and (7) random assignment to groups.
Search results
The article processing is shown in the flow diagram provided in Figure 1: We screened 190 articles, from which the following were excluded.
Figure 1.
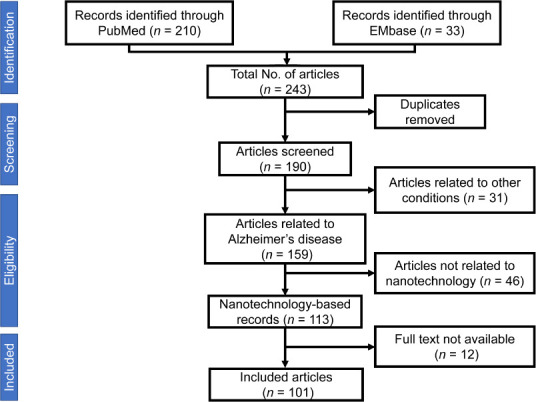
Flow diagram elucidating the methodology of the scientific literature search.
After excluding the articles irrelevant to our study title, we included 101 articles for the review.
Gene Therapy for Alzheimer’s Disease
Gene therapy can increase enzyme activity while balancing the low levels of bioactive substances. It has been increasingly explored in numerous animal AD models with encouraging outcomes. The first clinical trials employing ex vivo gene therapy (relating to NGF) have been completed, with promising reported improvements in AD pathology (Tuszynski et al., 2005). Gene therapy has potential benefits, such as enhanced safety and gene expression selectivity. Furthermore, in specific cases, it may be more effective than small-molecule treatments for the “up-regulation” of an enzyme (Alves et al., 2016).
The various etiologies of AD provide a multitude of potential gene therapy targets (Figure 2), including Aβ-generating proteins (BACE1 and APP), neurotrophins such as brain-derived neurotrophic factor (BDNF) and NGF that support and maintain neuronal health/growth, apolipoprotein E (APOE) and Aβ degradation associated enzymes (endothelin-converting enzyme, cathepsin B and neprilysin) that are targets for small interfering ribonucleic acid (siRNA) mediated gene silencing (Pfundstein et al., 2022). Research has targeted the genes mentioned above and obtained the outcomes detailed in Table 1.
Figure 2.
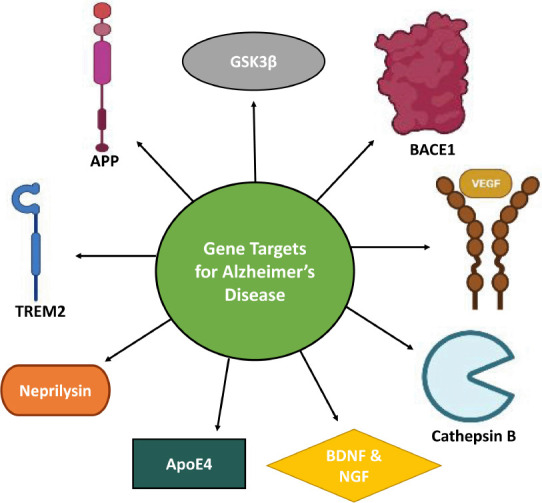
Targets for gene therapy in Alzheimer’s disease.
ApoE4: Apolipoprotein E4; APP: amyloid protein precursor; BACE1: β-site amyloid precursor protein cleaving enzyme 1; BDNF: brain-derived neurotrophic factor; GSK3β: glycogen beta kinase-3-beta; NGF: nerve growth factor; TREM2: triggering receptor expressed on myeloid cells 2; VEGF: vascular endothelial growth factor. Created with BioRender.com.
Table 1.
Potential genes targeted in AD-associated gene therapy
| Target | Role in AD | Type of subjects | Type of gene delivery | Gene therapy outcome | Limitations | References |
|---|---|---|---|---|---|---|
| Transgenic mice | Lentiviral vector delivery of BACE1 siRNA | Reduced Aβ accumulation | Since the active site of BACE1 is hydrophilic and accessible compared to other proteases, its action must be eliminated. However, the focus of this research was on lowering BACE1 activity. | Singer et al., 2005 | ||
| BACE1 | Aβ generation | AppNL-G-F mice | AAV-based vector delivery of Single domain antibodies (VHHs) | Outcomes favorably influence amyloid burden, neuroinflammation, synapse and cognitive function. | – | Rincon et al., 2019 |
| Neurotrophic effect and Aβ initiation | Adult rats | AAV vector system | Mice were shielded against cognitive impairment caused by aging. | – | Klein et al., 2000 | |
| NGF | Eight individuals with mild Alzheimer’s disease | Ex vivo gene delivery | Caused the activation of degenerating neurons and cell hypertrophy | It is difficult to deliver NGF to the brain safely. | Malkki et al., 2015 | |
| Neurotrophic effect | Amyloid-transgenic mice | Entorhinal cortex BDNF delivery | Recovers cognition, partly restores abnormal gene expression, enhances cell signaling, and repairs synaptic loss. | – | Nagahara et al., 2009 | |
| BDNF | APP transgenic mouse line J20 | Lentiviral-mediated BDNF gene delivery | Increased synaptic protein levels, boosted learning and memory, and reduced neurodegeneration. | The alterations in BDNF levels and its mRNA were inconsistent. | Narisawa-Saito et al., 1996 | |
| hAPP mice | Lentiviral-based cathepsin B delivery | Roles in neuroprotection and anti-amyloidogenicity | – | Mueller-Steiner et al., 2006 | ||
| Cathepsin B | Aβ degradation | Human wild-type APP (hAPPwt) mice | Gene knockout | Decreased Aβ40, Aβ42, and CTFβ by a large amount, which is expressed in most AD patients. | This study does not agree with the previous study, which demonstrated that eliminating the cathepsin B gene in hAPP mice did not affect brain Aβ or CTFβ. | Hook et al., 2009 |
| A novel mouse model with overexpression of a mutant form of APP in the hippocampus, using a lentiviral vector (LV-APPSw) | HSV (siRNA) delivery | Down-regulation of APP | The findings did not address whether the model would replicate more extensive pathological alterations similar to those seen in AD if LV-APPSw or the microtubule-associated protein Tau were expressed over a longer period. | Hong et al., 2006 | ||
| APP | Aβ generation | PDAPP transgenic mice | Gene delivery of lentiviral vectors expressing APOE isoforms | Reduced hippocampal Aβ level | In this investigation, neither lenti-apoE3 nor lenti-apoE4 significantly reduced the brain Aβ load. | Dodart et al., 2005 |
| APOE2 | Aβ burden | Chlorocebus aethiops sabaeus nonhuman primates. | AAVrh.10-mediated APOE2 gene delivery | Stimulates localized APOE2 expression | – | Rosenberg et al., 2018 |
| Cultured cells | Herpes simplex virus vector-mediated neprilysin expression. | Reduced Aβ burden by degrading Aβ40 | The study did not address the long-term consequences of overexpression of neprilysin in vivo in transgenic mouse models of AD. | Hong et al., 2006 | ||
| Neuroprotection and improved memory function | A mutant form of human presenilin-1 (DeltaE9) mice, a mutant form of the chimeric mouse/human amyloid precursor protein (APP695) and wild-type (C57BL/6) mice | Lentiviral vector delivery of neprilysin | Decreased the level of total Aβ peptide and abatement of Aβ plaque formation | There has not been any discussion of the impact of increased expression of NEP lentiviral in the brain before Aβ plaque formation. | El-Amouri et al., 2008 | |
| Neprilysin | hAPP transgenic mice | entiviral vector expressing human neprilysin (Lenti-Nep) | Modulates Aβ deposition by splitting fibrils | The oligomer content might rise due to the probable fibril splitting, which would be detrimental. The study did not address this problem. | Marr et al., 2003 |
AAV: Adeno-associated virus; AD: Alzheimer’s disease; APOE: apolipoprotein E; APP: amyloid precursor protein; Aβ: amyloid-β; BACE1: beta-site amyloid precursor protein cleaving enzyme 1; BDNF: brain-derived neurotrophic factor; CTF: carboxyl-terminal fragment; hAPP: human amyloid precursor protein; HSV: herpes simplex virus; NEP: neprilysin; NGF: nerve growth factor; PDAPP: a transgenic Alzheimer’s disease mouse model.
Neurotrophin gene therapy
Recent advances in gene therapy-assisted delivery of neurotrophins have yielded surprising results, including trophic responses of cholinergic neurons and increased cognitive abilities (Nasrolahi et al., 2022). NGF is part of the neurotrophin family, including BDNF, neurotrophin 3 (NT-3), NT-4/5, and NT-6 (Lübke et al., 2021). NGF, albeit the first neurotrophin discovered, has potential actions beyond its neurotrophic effects, and recent research found that depletion of NGF in PC12 (pheochromocytoma) cells triggers the process of Aβ biogenesis; thereby associating NGF with Aβ (Latina et al., 2018). It has been suggested that NGF gene therapy may alleviate AD’s clinical and behavioral manifestations (Peng et al., 2022). Some research has reported an association between the Val66Met mutation in BDNF with Alzheimer’s pathogenicity, while other research did not confirm this (Huang et al., 2007; Gao et al., 2022). Without changing the Aβ burden, BDNF gene delivery has been reported to exert a neuroprotective impact on cells of the entorhinal cortex, which is a key afflicted area in AD (Mueller-Steiner et al., 2006).
Nanotechnology-Based Gene Therapy
Due to recent nano-carrier-based gene therapy developments, scientific organizations have been provided with the technology and impetus to evaluate numerous potential treatment procedures (Wadetwar et al., 2021). In this regard, by reducing the enzymatic breakdown of genetic components, nanomaterials as gene carriers have considerably enhanced the efficiency of gene therapy (Yu et al., 2021). Organically modified silica nanoparticles, the most intriguing of all, were the first to be investigated for in vivo gene delivery to the central nervous system by Bharali et al. (2005).
SiRNA-mediated gene therapy
Genes involved in disease pathology, individual genes, and viral pathogens are promising candidates for RNA interference (RNAi). RNAi can also find new essential genes in pathophysiological processes (Aigner et al., 2019). RNAi modulates gene expression by regulating protein production using a post-transcriptional gene silencing mechanism (Mody et al., 2021). This includes lengthy portions of double-strand RNA (dsRNA) that split into the siRNA fraction and activate RNAi. SiRNA is the most suited agent for the short-term silencing of genes that encode proteins (Mahfuz et al., 2022) and has garnered considerable attention in gene therapy in recent years owing to its ability to down-regulate genes with high sequence specificity and a limitless number of therapeutic targets, including those that are thought to be undruggable (Gupta et al., 2019). However, incorrect delivery carrier choice can diminish the gene-silencing activity of siRNA, change pharmacokinetics, and potentially increase off-target effects (Sioud et al., 2020). It was once assumed that siRNA was biochemically stable and did not necessitate delivery carriers for in vivo siRNA delivery (Artiga et al., 2019). However, several previous studies have revealed the need for the functionalization of siRNA to improve its stability and the use of a unique carrier system that can primarily enhance effective delivery to target tissues (de Fougerolles et al., 2007; Kim et al., 2007; Kuhn et al., 2007; Bumcrot et al., 2016). Nanotechnology has emerged as a possible option, and several delivery systems utilizing nanoparticles have been shown to bypass key delivery challenges regarding siRNA delivery, including the BBB (Zheng et al., 2018; Han et al., 2021). The mechanism of siRNA-nanoparticle-mediated gene silencing is shown in Figure 3. Table 2 shows the various nano complexes used in siRNA-mediated gene therapy in AD.
Figure 3.
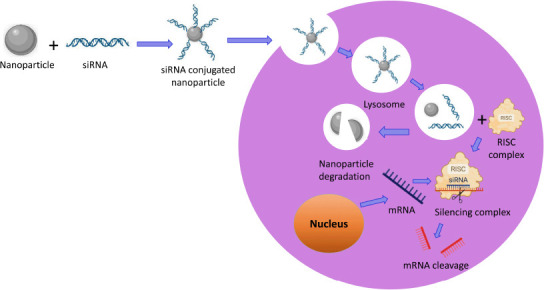
Mechanism of gene silencing by small interfering ribonucleic acid (siRNA).
Inside the cell, siRNA nanoconjugate interacts with lysosomes and disintegrates (Acharya et al., 2017). The nanoparticle degrades, and the siRNA portion combines with RNA-induced silencing complex (RISC) and forms a gene silencing complex, which brings about the downregulation of the gene via mRNA cleavage. Created with BioRender.com.
Table 2.
Nanocomplexes used in siRNA-mediated gene therapy
| No. | Complex | Target gene | Outcome | References |
|---|---|---|---|---|
| 1 | Chitosan-PEG-TAT | Ataxin-1 | Suppression of the Ataxin-1 protein. | Malhotra et al., 2013 |
| 2 | Exosomes -endogenous nano-vesicles | BACE1 | mRNA (60%) and protein (62%) knockdown of BACE1 | Yang et al., 2022 |
| 3 | Gal-NP@siRNA | BACE1 | Restored cognitive functions | Zhou et al., 2020 |
| 4 | NL4-ApoA-I-siRNA-dendrimer | BACE1 | Inhibition of Aβ formation | Zhang et al., 2017; Zhang et al., 2019 |
| 5 | (PEG-PDMAEMA)-CGN-Tet1-siRNA nano-carriers | BACE1 | Directed BACE1 siRNA to brain neurons | Wang et al., 2018 |
| 6 | Chitosan-coated SLNs | BACE1 | Permeates the monolayer to a greater extent and targets BACE1 | Rassu et al., 2017 |
| 7 | siRNA-conjugated magnetite nanoparticles | BACE1 | Down-regulation of the BACE1 gene | Lopez-Barbosa et al., 2020 |
| 8 | siRNA-fluorescent quantum dots | BACE1 | Reduction of Aβ in nerve cells | Li et al., 2012 |
| 9 | NgR-siRNA-BDNF nanocomplex | BDNF | Efficiently overcomes the limitations of conventional AD treatment methods | Wang et al., 2020 |
| 10 | siRNA-PEG-liposomes | BACE1 | Gene silencing of BACE1 | Tagalakis et al., 2014 |
| 11 | PEG-PEI-siRNA-Carboxylated graphene oxide (GO) nanosheets | GSK3β | Reduced expression of amyloid pathway genes | Gupta et al., 2021 |
| 12 | siRNA conjugated with magnetic nanoparticles | TREM2 | Cognitive improvements | Carrillo-Jimenez et al., 2018 |
| 13 | PEI-PEG-based micellar nanoparticle | BACE1 and APP | Knockdown of BACE1 and APP | Shyam et al., 2015 |
AD: Alzheimer’s disease; APP: amyloid precursor protein; Aβ: amyloid-β; BACE1: beta-site amyloid precursor protein cleaving enzyme 1; BDNF: brain-derived neurotrophic factor; GSK3β: glycogen synthase kinase 3β; NgR: Nogo receptor; PEG: polyethylene glycol; siRNA: small interfering ribonucleic acid; TAT: transactivator of transcription.
Nanoparticle-based gene therapy
Liposomes
The adsorption affinity of nanoliposomes coated with an anti-Aβ monoclonal antibody was studied by Canovi et al. (2011). The ability of Aβ-monoclonal antibody -coated liposomes to attach to Aβ plaques in AD brain autopsy samples provided evidence for using such liposomes as potential disease diagnostics and therapeutics. To prevent the cytotoxicity of cationic nanoparticles, anionic siRNA-nanocomplexes were created using polyethylene glycol (PEG)-liposomes (anionic) and targeting peptides (cationic), and, through the use of these nano complexes, BACE1 suppression was accomplished (Tagalakis et al., 2014). For plasmid encoding apolipoprotein E2 delivery, Dos Santos Rodrigues et al. (2019) employed transferrin-penetratin entrapped liposomes and found a remarkable elevation in apolipoprotein E2 levels in mice.
Polymeric nanoparticles
A glycosylated polymeric siRNA nanocomplex (Gal-NP@siRNA) was created and evaluated in a transgenic AD model that selectively suppressed BACE1 and decreased Aβ levels. This mitigated damage to myelin, aided clearance of by-products (owing to its biocompatibility) and helped restore cognitive performance in the mice (Kim et al., 2007). A polymer-based gene carrier having the glycemic phenylalanine-leucine-glycine sequence that is considered sensitive to cleavage by cathepsin B, a lysosomal cysteine protease with a role in intracellular proteolysis, was used to improve plasmid DNA (pDNA) delivery intracellularly (Lee et al., 2017). Cathepsin B levels are considered elevated in AD and neurodegenerative conditions such as following traumatic brain injury, with the protein leaking from the lysosome to the cytosol compartment where, in addition to pathological roles on Aβ generation/clearance, it could more efficiently release pDNA from an appropriately designed nanocarrier-based gene delivery system.
Glycemic monitoring was used as an external stimulus to establish a method for the brain delivery of systemic antisense oligonucleotides by traversing the BBB. Antisense oligonucleotides can be encapsulated in glucose-installed polymeric nanoparticles that may be coupled to glucose transporter-1 (Min et al., 2020). These antisense oligonucleotides target messenger RNA (mRNA) for APP or its processing enzymes to reduce toxic Aβ levels (Grabowska-Pyrzewicz et al., 2021). Malhotra et al. (2013) developed nanoparticles for siRNA delivery using a new cell-targeting peptide called transactivator of transcription, PEG, and chitosan polymer. The Chitosan-PEG-transactivator of transcription complex was produced and utilized to create nanoparticles with a diameter of approximately 5 nm coupled with siRNA for delivery to nerve cells to suppress the ataxin-1 gene, which is responsible for BACE1 expression and is involved in Aβ pathology (Suh et al., 2019). In another investigation, a poly-siRNA/thiolated glycol chitosan nanoparticle was utilized to silence vascular endothelial growth factor, which is found to be elevated in AD brain and has been associated with loss of pericytes, elevated BBB permeability, more severe AD and particularly Tau pathology, and greater clinical signs of AD (Lee et al., 2012). Various polymer-siRNA nanoconjugates used in gene therapy are schematically depicted in Figure 4.
Figure 4.
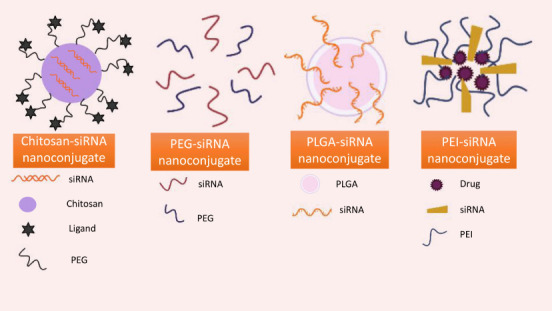
Types of polymer-siRNA nanoconjugates.
PEG: Polyethylene glycol; PEI: polyethyleneimine; PLGA: poly(lactic-co-glycolic acid); siRNA: small interfering ribonucleic acid. Created with BioRender.com.
Dendrimers
Zhang et al. (2017, 2019) coated dendrimer nanoparticles with NL4 peptide and apolipoprotein A–I. They then employed these dendrimer nanoparticles in a unique dual-targeting drug delivery system to selectively transport siRNA into neuronal tissue to suppress BACE1 and, thereby, reduce Aβ generation. A multifunctional nanocarrier was created in a separate study using PEGylated dendrigraft poly-L-lysines to deliver desired genes and peptides to the brain via systemic injection. The delivery of non-coding ribonucleic acid (RNA) plasmids was used to down-regulate the main enzymes involved in Aβ production (Ouyang et al., 2022).
Lipid nanoparticles
CD45 (cluster of differentiation 45) expression has been reported to be elevated in microglial cells in AD patients (Singh et al., 2021). In line with this finding, Basha et al. (2011) utilized lipid nanoparticles for CD45-directed siRNA delivery to immune cells. A further study employed chitosan-coated and uncoated solid lipid nanoparticles for nose-to-brain siRNA delivery by exploiting the olfactory and trigeminal nerve pathways. It was discovered, using a Caco-2 epithelial cell model, that siRNA released from chitosan-coated solid lipid nanoparticles penetrated the monolayer more effectively to support the targeting of BACE1 (Rassu et al., 2017).
Magnetic nanoparticles
A straightforward strategy for knocking down the expression of several genes, including triggering receptors expressed on myeloid cells 2 (TREM2; a gene involved in regulating microglial inflammatory responses and revealed by genome-wide association studies to have variants associated with AD pathology and impairment), was demonstrated by utilizing siRNA linked with magnetic nanoparticles (Carrillo-Jimenez et al., 2018). In another study, PEGylated magnetic nanoparticles were employed to deliver siRNA to nerve cells via endocytosis to suppress the BACE1 gene (Lopez-Barbosa et al., 2020) to lower Aβ generation.
Micelles
Shyam et al. (2015) used a micellar nanoparticle technique based on a copolymer comprising polyethyleneimine (PEI) and PEG to target BACE1 and APP via siRNA delivery. This study demonstrated that the design of siRNA-conjugated nanoparticles is a crucial predictor of their distribution and gene-silencing efficacy in the central nervous system (Shyam et al., 2015). By reducing neurodegeneration and improving Aβ clearance, intranasal delivery of neprilysin-coated extracellular vesicles mitigated behavioral impairments in a rat AD model (Izadpanah et al., 2020). Delivering neprilysin mRNA packaged in polyplex nanomicelles has also been reported to improve Aβ clearance (Meng et al., 2021).
Silicon nanoparticles
To create effective scaffolds for the transport of the siRNA strand, mesoporous silica nanoparticles were prepared and treated with PEI and aluminum (Badihi et al., 2021). Studies found that NGF-loaded porous silicon nanostructures elicited typical trophic responses (Mitra et al., 2021) and had a significant cytoprotective impact against damage caused by Aβ (Zilony-Hanin et al., 2019; Xu et al., 2021).
Miscellaneous nano complexes
Wang et al. synthesized siRNA nanocarriers that were modified with cingulin and ten-eleven translocation methylcytosine dioxygenase 1 peptides (CT/siRNA). The CT/siRNA nanocomplexes proved to be efficient in selectively targeting and decreasing the expression of BACE1 (Rassu et al., 2017). Nogo receptor-siRNA (NgR-siRNA) and BDNF were combined to create a new nanoparticle. Cell culture and rodent experiments revealed that the described nanoparticles could effectively overcome select shortcomings of traditional AD treatment approaches, supporting the brain cholinergic system and augmenting cognitive function in APP/PS1 AD mice (Wang et al., 2020). For siRNA-mediated gene silencing of glycogen synthase kinase three betas, carboxylated graphene oxide nanosheets were prepared and complexed with PEG and PEI, which downregulated amyloid cascade genes (APP and BACE1) (Gupta et al., 2021). CRISPR-Cas9 nanocomplexes were employed in two mouse AD models to target BACE1 and decrease Aβ-associated abnormalities and cognitive impairments (Park et al., 2019; Baker C, 2022). To improve the BACE1 targeting efficiency of siRNA and reduce Aβ in neurons, fluorescent quantum dots (Li et al., 2012) and exosomes-endogenous nano-vesicles (Yang et al., 2022) were utilized. In another study, Lv et al. (2020) conjugated epigallocatechin-3-gallate and BACE1 antisense shRNA-encoded plasmid with a multifunctional nanocarrier for downregulation of BACE1.
Thus, the nanoparticles mentioned above/nano complexes appear as promising gene delivery candidates in preclinical studies for consideration for translation to patients with AD. Whereas nanoparticle-based gene delivery strives to transfer the product with tolerability and selectivity to the target region, it should be noted that it becomes susceptible to degradation by intracellular enzymes after penetrating the cytoplasm. This can impact the final efficiency of the delivery system. The delivery of various neurotrophic factors using nanocarriers is tabulated in Table 3.
Table 3.
Therapeutic nanoparticle-based neurotrophin targeting for AD
| No. | Nanocarrier | Neurotrophic factor | Model | References |
|---|---|---|---|---|
| 1 | Cubosome NPs | Gly 14-humanin | Rat | Wu et al., 2012 |
| 2 | Cationic liposomes | Plasmid encoding NGF or GDNF | In vitro | Lu et al., 2002 |
| 3 | PEGylated cationic lipid NPs | BDNF coding plasmid | In vitro | Angelov et al., 2011, 2012 |
| 4 | Fusion protein vectors | NGF-IgG; BDNF-IgG (OX26); GDNF-Tat | Rat | Bickel et al., 2001; Boado et al., 2007, 2011; Kabanov et al., 2007; Pardgridge et al., 2008, 2010 |
| 5 | Cubosome NPs with omega-3 fatty acid | BDNF | In vitro | Géral et al., 2012 |
| 6 | NTS (neurotensin)-polyplex nanocarrier | Neurotrophic genes (GDNF, NRTN, BDNF) | Rat, in vitro | Xie et al., 2005; Kuo et al., 2014; Rodrigues et al., 2020 |
| 8 | Polysorbate-coated poly (butyl cyanoacrylate) (PBCA) NPs | NGF | Mouse | Kurakhmaeva et al., 2009 |
| 9 | Nanoporous poly-L-glutamic acid (PGA) particles | BDNF | In vitro | Tan et al., 2012 |
AD: Alzheimer’s disease; BDNF: brain-derived neurotrophic factor; GDNF: glial cell-derived neurotrophic factor; NGF: nerve growth factor; NPs: nanoparticles; PEG: polyethylene glycol; Tat: transactivator of transcription.
Challenges Regarding Nanotechnology-Based Gene Therapy
Even though nanotechnology-based gene therapy has the potential to become a breakthrough strategy to improve the treatment and management of a host of debilitating diseases in the coming years, there remain key challenges associated with it - that require to be addressed. Nanotechnology has raised considerable concerns about nanoparticle-mediated cytotoxicity and undesirable effects from gene delivery. Regarding toxicity, various components of nano constructs may modify or disrupt the hemostatic mediator transportation within the central nervous system. Furthermore, internalized nanoparticles can potentially cause necrosis or apoptosis of neuronal cells via various mechanisms. Polymers appear to influence gene expression, which might cause significant issues with nucleic acid delivery to brain cells. The timing and duration between doses should be carefully considered in relation to minimizing nanoparticle-mediated undesirable effects. The design of gene therapy carriers for delivery across the brain is among the primary problems in optimizing therapeutic applications of gene therapy. To carry the gene to the designated targets, appropriate delivery techniques are required, along with the management of any off-target consequences. Because AD is a multifaceted disease, effectively treating it with a single gene transfer might not be possible as there appear to be multiple triggered cascades within the AD brain that lead to a host of neuronal impairments, pathology, and cognitive decline.
Consequently, it remains a significant challenge to determine how to assemble the many RNAi elements and transport them to a targeted site of interest. Which element(s) and targeted site(s) should best be selected, and at what stage during the disease process? As previously indicated, antibodies have also been frequently employed for targeting. However, a significant drawback of this particular strategy is the large size of antibody molecules, making it harder to attach them to nano vehicles.
Future Prospects
RNAi has evolved as a powerful research tool that has provided the AD field with a better understanding of AD pathophysiology and is now being evaluated as a practical strategy for therapeutic use. Consequent to its benefits over other existing therapies, RNAi technology is anticipated to help tackle unanswered concerns about AD through in vitro and in vivo techniques. Optimizing this technology for clinical application remains a highly important focus of the required work in the immediate future.
Certainly, nanoparticles have considerable promise in bioengineering, especially for delivering bioactive drugs to patients with neurological illnesses. Nevertheless, it should be acknowledged that nanomaterials’ formulation and development are not confined to a single system but embody a platform wherein the nanomaterials can be modified to potentially treat any disease by substituting the target-specific molecule on the nanoparticles’ surface. This can be considered an advantage, as it offers considerable potential (i.e., numerous options) to optimize the therapy to overcome the specific challenges associated with AD versus a different neurological disorder or, indeed, a systemic disease. A possible disadvantage is that the technology platform offers many potential evaluation choices. So many that this may complicate the optimization process in relation to gaining both an enhanced understanding and in-depth knowledge of the methods employed to synthesize and utilize nanoparticles as gene carrier systems that are valuable and, necessarily, practical. Last but not least, future research should additionally focus on tolerability and undesired gene silencing difficulties caused by chemical modifications to the delivery vehicle.
Conclusion
Presently, no truly disease-modifying therapy for AD is available. There are numerous treatment approaches, and the amyloid cascade hypothesis, for good (Selkoe et al., 2021) or bad (Thambisetty et al., 2021), has emphasized amyloid-associated pathways and resulted in the invention of Aβ-generating enzyme (BACE1 and γ-secretase) inhibitors and Aβ clearance and anti-aggregation monoclonal antibody therapeutics. Gene therapy can selectively access these same targets and bring about their inhibition or augmentation in a different but parallel manner, as well as potentially target other key proteins supported by other AD hypotheses, even those considered potentially undruggable. Thus, gene therapy is among the most innovative and promising new ways to treat AD. Combining gene therapy with nanotechnology has emerged as a valuable discipline for gene delivery across the BBB and other biological barriers. The development of multifunctional nanocomplexes for siRNA delivery has accelerated in recent years. These highly adaptable complexes provide various unique options as custom delivery carriers to improve the effectiveness and selectivity of gene therapy. This article reviewed many such proof-of-concept studies. However, there remain several issues in nanotechnology that need to be addressed before they can be practically utilized as gene delivery methods, such as low transfection efficacy and potential toxicity/tolerability issues. To address these constraints, it will be necessary to understand better diverse cell structure components, cell metabolism pathways, and microenvironments and support the creation of innovative nanostructures with specialized characteristics for neurological disorders.
Additional file: Open peer review report 1 (85.9KB, pdf) .
Acknowledgments:
All authors are grateful for the support from their associated scientific institutions.
Footnotes
Author contributions: Conception, literature search and evaluation, initial draft: AU; conception, literature evaluation, editing/revision: MAK; conception, editing/revision, literature evaluation: NHG. All authors approved the final version of the manuscript.
Conflicts of interest: There are no conflicts of interest.
Data availability statement: The data are available from the corresponding author on reasonable request.
Open peer reviewer: Shaul Schreiber, Tel Aviv Sourasky Medical Center, Israel.
P-Reviewer: Schreiber S; C-Editors: Zhao M, Liu WJ, Qiu Y; T-Editor: Jia Y
References
- 1.Acharya R, Saha S, Ray S, Hazra S, Mitra MK, Chakraborty J. siRNA-nanoparticle conjugate in gene silencing: a future cure to deadly diseases? Mater Sci Eng C Mater Biol Appl. 2017;76:1378–1400. doi: 10.1016/j.msec.2017.03.009. [DOI] [PubMed] [Google Scholar]
- 2.Aigner A. Perspectives, issues and solutions in RNAi therapy: the expected and the less expected. Nanomedicine (Lond) 2019;14:2777–2782. doi: 10.2217/nnm-2019-0321. [DOI] [PubMed] [Google Scholar]
- 3.Alves S, Fol R, Cartier N. Gene therapy strategies for Alzheimer's disease: an overview. Hum Gene Ther. 2016;27:100–107. doi: 10.1089/hum.2016.017. [DOI] [PubMed] [Google Scholar]
- 4.Angelov B, Angelova A, Filippov S, Karlsson G, Terrill N, Lesieur S, Štěpánek P. Topology and internal structure of PEGylated lipid nanocarriers for neuronal transfection: synchrotron radiation SAXS and cryo-TEM studies. Soft Matter. 2011;7:9714–9720. [Google Scholar]
- 5.Angelov B, Angelova A, Filippov S, Karlsson G, Terrill N, Lesieur S, Štěpánek P. SAXS study of sterically stabilized lipid nanocarriers functionalized by DNA. J Phys Conf Series. 2012;351:012004. [Google Scholar]
- 6.Artiga Á, Serrano-Sevilla I, De Matteis L, Mitchell SG, de la Fuente JM. Current status and future perspectives of gold nanoparticle vectors for siRNA delivery. J Mater Chem B. 2019;7:876–896. doi: 10.1039/c8tb02484g. [DOI] [PubMed] [Google Scholar]
- 7.Badihi R, Mahmoudi A, Sazegar MR, Nazari K. Synthesis of nanocomposites based on mesoporous aluminosilicate and polyethyleneimine (PEI) for sirna delivery: potential usefulness of the synergistic effect of Al3+ion and PEI on the sirna delivery efficiency for diseases treatment. J Nanotech Res. 2021;4:029–044. [Google Scholar]
- 8.Bake C. Scientists Use CRISPR-Cas9 as 'DNA Scissors'to cut out Alzheimer's gene in mice. 2022. [Accessed February 9, 2022]. Available at: https://alzheimersnewstoday.com/2020/02/14/scientists-use-crispr-cas9-technology-dna-scissors-cut-out-alzheimers-gene-mice/
- 9.Basha G, Novobrantseva TI, Rosin N, Tam YY, Hafez IM, Wong MK, Sugo T, Ruda VM, Qin J, Klebanov B, Ciufolini M, Akinc A, Tam YK, Hope MJ, Cullis PR. Influence of cationic lipid composition on gene silencing properties of lipid nanoparticle formulations of siRNA in antigen-presenting cells. Mol Ther. 2011;19:2186–2200. doi: 10.1038/mt.2011.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bharali DJ, Klejbor I, Stachowiak EK, Dutta P, Roy I, Kaur N, Bergey EJ, Prasad PN, Stachowiak MK. Organically modified silica nanoparticles: a nonviral vector for in vivo gene delivery and expression in the brain. Proc Natl Acad Sci U S A. 2005;102:11539–11544. doi: 10.1073/pnas.0504926102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bickel U, Yoshikawa T, Pardridge WM. Delivery of peptides and proteins through the blood-brain barrier. Adv Drug Deliv Rev. 2001;46:247–279. doi: 10.1016/s0169-409x(00)00139-3. [DOI] [PubMed] [Google Scholar]
- 12.Boado RJ, Zhang Y, Zhang Y, Pardridge WM. Genetic engineering, expression, and activity of a fusion protein of a human neurotrophin and a molecular Trojan horse for delivery across the human blood-brain barrier. Biotechnol Bioeng. 2007;97:1376–1386. doi: 10.1002/bit.21369. [DOI] [PubMed] [Google Scholar]
- 13.Boado RJ, Pardridge WM. The Trojan horse liposome technology for nonviral gene transfer across the blood-brain barrier. J Drug Deliv. 2011;2011:296151. doi: 10.1155/2011/296151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bumcrot D, Manoharan M, Koteliansky V, Sah DW. RNAi therapeutics: a potential new class of pharmaceutical drugs. Nat Chem Biol. 2006;2:711–719. doi: 10.1038/nchembio839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cai Z, Qiao PF, Wan CQ, Cai M, Zhou NK, Li Q. Role of blood-brain barrier in Alzheimer's disease. J Alzheimers Dis. 2018;63:1223–1234. doi: 10.3233/JAD-180098. [DOI] [PubMed] [Google Scholar]
- 16.Canovi M, Markoutsa E, Lazar AN, Pampalakis G, Clemente C, Re F, Sesana S, Masserini M, Salmona M, Duyckaerts C, Flores O, Gobbi M, Antimisiaris SG. The binding affinity of anti-Aβ1-42 MAb-decorated nanoliposomes to Aβ1-42 peptides in vitro and to amyloid deposits in post-mortem tissue. Biomaterials. 2011;32:5489–5497. doi: 10.1016/j.biomaterials.2011.04.020. [DOI] [PubMed] [Google Scholar]
- 17.Carrillo-Jimenez A, Puigdellívol M, Vilalta A, Venero JL, Brown GC, StGeorge-Hyslop P, Burguillos MA. Effective knockdown of gene expression in primary microglia with siRNA and magnetic nanoparticles without cell death or inflammation. Front Cell Neurosci. 2018;12:313. doi: 10.3389/fncel.2018.00313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Fougerolles A, Vornlocher HP, Maraganore J, Lieberman J. Interfering with disease: a progress report on siRNA-based therapeutics. Nat Rev Drug Discov. 2007;6:443–453. doi: 10.1038/nrd2310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Oliveira J, Kucharska E, Garcez ML, Rodrigues MS, Quevedo J, Moreno-Gonzalez I, Budni J. Inflammatory cascade in Alzheimer's disease pathogenesis: a review of experimental findings. Cells. 2021;10:2581. doi: 10.3390/cells10102581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Do Carmo S, Kannel B, Cuello AC. The nerve growth factor metabolic pathway dysregulation as cause of Alzheimer's cholinergic atrophy. Cells. 2021;11:16. doi: 10.3390/cells11010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dodart JC, Marr RA, Koistinaho M, Gregersen BM, Malkani S, Verma IM, Paul SM. Gene delivery of human apolipoprotein E alters brain Abeta burden in a mouse model of Alzheimer's disease. Proc Natl Acad Sci U S A. 2005;102:1211–1216. doi: 10.1073/pnas.0409072102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dos Santos Rodrigues B, Kanekiyo T, Singh J. ApoE-2 brain-targeted gene therapy through transferrin and penetratin tagged liposomal nanoparticles. Pharm Res. 2019;36:161. doi: 10.1007/s11095-019-2691-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.El-Amouri SS, Zhu H, Yu J, Marr R, Verma IM, Kindy MS. Neprilysin: an enzyme candidate to slow the progression of Alzheimer's disease. Am J Pathol. 2008;172:1342–1354. doi: 10.2353/ajpath.2008.070620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gao L, Zhang Y, Sterling K, Song W. Brain-derived neurotrophic factor in Alzheimer's disease and its pharmaceutical potential. Transl Neurodegener. 2022;11:4. doi: 10.1186/s40035-022-00279-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Géral C, Angelova A, Angelov B, Nicolas V, Lesieur S. Multicompartment lipid nanocarriers for targeting of cells expressing brain receptors. In: Garti N, Mezzenga R, Somasundaran P, editors. Self-assembled supramolecular architectures:lyotropic liquid crystals. Hoboken: John Wiley &Sons, Inc; 2012. pp. 319–355. [Google Scholar]
- 26.Grabowska-Pyrzewicz W, Want A, Leszek J, Wojda U. Antisense oligonucleotides for Alzheimer's disease therapy: from the mRNA to miRNA paradigm. EBioMedicine. 2021;74:103691. doi: 10.1016/j.ebiom.2021.103691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gupta N, Rai DB, Jangid AK, Pooja D, Kulhari H. Nanomaterials-based siRNA delivery: routes of administration, hurdles and role of nanocarriers. In: Singh S, Maurya P, editors. Nanotechnology in modern animal biotechnology. Singapore: Springer; 2019. pp. 67–114. [Google Scholar]
- 28.Gupta S, Singh V, Ganesh S, Singhal NK, Sandhir R. siRNA mediated GSK3βknockdown targets insulin signaling pathway and rescues Alzheimer's disease pathology: evidence from in vitro and in vivo studies. ACS Appl Mater Interfaces. 2022;14:69–93. doi: 10.1021/acsami.1c15305. [DOI] [PubMed] [Google Scholar]
- 29.Han L, Jiang C. Evolution of blood-brain barrier in brain diseases and related systemic nanoscale brain-targeting drug delivery strategies. Acta Pharm Sin B. 2021;11:2306–2325. doi: 10.1016/j.apsb.2020.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hong CS, Goins WF, Goss JR, Burton EA, Glorioso JC. Herpes simplex virus RNAi and neprilysin gene transfer vectors reduce accumulation of Alzheimer's disease-related amyloid-beta peptide in vivo. Gene Ther. 2006;13:1068–1079. doi: 10.1038/sj.gt.3302719. [DOI] [PubMed] [Google Scholar]
- 31.Hook VY, Kindy M, Reinheckel T, Peters C, Hook G. Genetic cathepsin B deficiency reduces beta-amyloid in transgenic mice expressing human wild-type amyloid precursor protein. Biochem Biophys Res Commun. 2009;386:284–288. doi: 10.1016/j.bbrc.2009.05.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang R, Huang J, Cathcart H, Smith S, Poduslo SE. Genetic variants in brain-derived neurotrophic factor associated with Alzheimer's disease. J Med Genet. 2007;44:e66. doi: 10.1136/jmg.2006.044883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Izadpanah M, Dargahi L, Ai J, Asgari Taei A, Ebrahimi Barough S, Mowla SJ, TavoosiDana G, Farahmandfar M. Extracellular vesicles as a neprilysin delivery system memory improvement in Alzheimer's disease. Iran J Pharm Res. 2020;19:45–60. doi: 10.22037/ijpr.2020.112062.13508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jiang Y, Zeng Z, Yao J, Guan Y, Jia P, Zhao X, Xu L. Treatment of Alzheimer's disease with small-molecule photosensitizers. Chin Chem Lett. 2022 doi.org/10.1016/j.cclet.2022.107966. [Google Scholar]
- 35.Kabanov AV, Gendelman HE. Nanomedicine in the diagnosis and therapy of neurodegenerative disorders. Prog Polym Sci. 2007;32:1054–1082. doi: 10.1016/j.progpolymsci.2007.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim DH, Rossi JJ. Strategies for silencing human disease using RNA interference. Nat Rev Genet. 2007;8:173–184. doi: 10.1038/nrg2006. [DOI] [PubMed] [Google Scholar]
- 37.Kim W, Ma L, Lomoio S, Willen R, Lombardo S, Dong J, Haydon PG, Tesco G. BACE1 elevation engendered by GGA3 deletion increases β-amyloid pathology in association with APP elevation and decreased CHL1 processing in 5XFAD mice. Mol Neurodegener. 2018;13:6. doi: 10.1186/s13024-018-0239-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Klein RL, Hirko AC, Meyers CA, Grimes JR, Muzyczka N, Meyer EM. NGF gene transfer to intrinsic basal forebrain neurons increases cholinergic cell size and protects from age-related, spatial memory deficits in middle-aged rats. Brain Res. 2000;875:144–151. doi: 10.1016/s0006-8993(00)02634-2. [DOI] [PubMed] [Google Scholar]
- 39.Kühn R, Streif S, Wurst W. RNA interference in mice. Handb Exp Pharmacol. 2007;2007:149–176. doi: 10.1007/978-3-540-35109-2_7. [DOI] [PubMed] [Google Scholar]
- 40.Kuo YC, Wang CT. Protection of SK-N-MC cells against β-amyloid peptide-induced degeneration using neuron growth factor-loaded liposomes with surface lactoferrin. Biomaterials. 2014;35:5954–5964. doi: 10.1016/j.biomaterials.2014.03.082. [DOI] [PubMed] [Google Scholar]
- 41.Kurakhmaeva KB, Djindjikhashvili IA, Petrov VE, Balabanyan VU, Voronina TA, Trofimov SS, Kreuter J, Gelperina S, Begley D, Alyautdin RN. Brain targeting of nerve growth factor using poly(butyl cyanoacrylate) nanoparticles. J Drug Target. 2009;17:564–574. doi: 10.1080/10611860903112842. [DOI] [PubMed] [Google Scholar]
- 42.Latina V, Caioli S, Zona C, Ciotti MT, Borreca A, Calissano P, Amadoro G. NGF-dependent changes in ubiquitin homeostasis trigger early cholinergic degeneration in cellular and animal AD-model. Front Cell Neurosci. 2018;12:487. doi: 10.3389/fncel.2018.00487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee JY, Lee SH, Oh MH, Kim JS, Park TG, Nam YS. Prolonged gene silencing by siRNA/chitosan-g-deoxycholic acid polyplexes loaded within biodegradable polymer nanoparticles. J Control Release. 2012;162:407–413. doi: 10.1016/j.jconrel.2012.07.006. [DOI] [PubMed] [Google Scholar]
- 44.Lee S, Son SJ, Song SJ, Ha TH, Choi JS. Polyamidoamine (PAMAM) dendrimers modified with cathepsin-B cleavable oligopeptides for enhanced gene delivery. Polymers (Basel) 2017;9:224. doi: 10.3390/polym9060224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li J, Zheng M, Shimoni O, Banks WA, Bush AI, Gamble JR, Shi B. Development of novel therapeutics targeting the blood-brain barrier: from barrier to carrier. Adv Sci (Weinh) 2021;8:e2101090. doi: 10.1002/advs.202101090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li S, Liu Z, Ji F, Xiao Z, Wang M, Peng Y, Zhang Y, Liu L, Liang Z, Li F. Delivery of quantum dot-siRNA nanoplexes in SK-N-SH cells for BACE1 gene silencing and intracellular imaging. Mol Ther Nucleic Acids. 2012;1:e20. doi: 10.1038/mtna.2012.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lopez-Barbosa N, Garcia JG, Cifuentes J, Castro LM, Vargas F, Ostos C, Cardona-Gomez GP, Hernandez AM, Cruz JC. Multifunctional magnetite nanoparticles to enable delivery of siRNA for the potential treatment of Alzheimer's. Drug Deliv. 2020;27:864–875. doi: 10.1080/10717544.2020.1775724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lu KW, Chen ZY, Jin DD, Hou TS, Cao L, Fu Q. Cationic liposome-mediated GDNF gene transfer after spinal cord injury. J Neurotrauma. 2002;19:1081–1090. doi: 10.1089/089771502760341983. [DOI] [PubMed] [Google Scholar]
- 49.Lübke JH, Idoon F, Mohasel-Roodi M, Alipour F, Hami J, Ehteshampour A, Mostafaee H, Sadeghi A. Neurotrophic factors in Alzheimer's disease: pathogenesis and therapy. Acta Neurobiol Exp (Wars) ; 2021;81:314–327. [PubMed] [Google Scholar]
- 50.Lv L, Yang F, Li H, Yuan J. Brain-targeted co-delivery of β-amyloid converting enzyme 1 shRNA and epigallocatechin-3-gallate by multifunctional nanocarriers for Alzheimer's disease treatment. IUBMB Life. 2020;72:1819–1829. doi: 10.1002/iub.2330. [DOI] [PubMed] [Google Scholar]
- 51.Mahfuz A, Khan MA, Sajib EH, Deb A, Mahmud S, Hasan M, Saha O, Islam A, Rahaman MM. Designing potential siRNA molecules for silencing the gene of the nucleocapsid protein of Nipah virus: A computational investigation. Infect Genet E. 2022;102:105310. doi: 10.1016/j.meegid.2022.105310. [DOI] [PubMed] [Google Scholar]
- 52.Malhotra M, Tomaro-Duchesneau C, Prakash S. Synthesis of TAT peptide-tagged PEGylated chitosan nanoparticles for siRNA delivery targeting neurodegenerative diseases. Biomaterials. 2013;34:1270–1280. doi: 10.1016/j.biomaterials.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 53.Malkki H. Alzheimer disease: NGF gene therapy activates neurons in the AD patient brain. Nat Rev Neurol. 2015;11:548. doi: 10.1038/nrneurol.2015.170. [DOI] [PubMed] [Google Scholar]
- 54.Marr RA, Rockenstein E, Mukherjee A, Kindy MS, Hersh LB, Gage FH, Verma IM, Masliah E. Neprilysin gene transfer reduces human amyloid pathology in transgenic mice. J Neurosci. 2003;23:1992–1996. doi: 10.1523/JNEUROSCI.23-06-01992.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McLarnon JG. A leaky blood-brain barrier to fibrinogen contributes to oxidative damage in Alzheimer's disease. Antioxidants (Basel) 2021;11:102. doi: 10.3390/antiox11010102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Meng C, Chen Z, Li G, Welte T, Shen H. Nanoplatforms for mRNA therapeutics. Adv Ther. 2021;4:2000099. [Google Scholar]
- 57.Min HS, Kim HJ, Naito M, Ogura S, Toh K, Hayashi K, Kim BS, Fukushima S, Anraku Y, Miyata K, Kataoka K. Systemic brain delivery of antisense oligonucleotides across the blood-brain barrier with a glucose-coated polymeric nanocarrier. Angew Chem Int Ed Engl. 2020;59:8173–8180. doi: 10.1002/anie.201914751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mitra S, Gera R, Linderoth B, Lind G, Wahlberg L, Almqvist P, Behbahani H, Eriksdotter M. A review of techniques for biodelivery of nerve growth factor (NGF) to the brain in relation to Alzheimer's disease. Adv Exp Med Biol. 2021;1331:167–191. doi: 10.1007/978-3-030-74046-7_11. [DOI] [PubMed] [Google Scholar]
- 59.Mody D, Verma V, Rani V. Modulating host gene expression via gut microbiome-microRNA interplay to treat human diseases. Crit Rev Microbiol. 2021;47:596–611. doi: 10.1080/1040841X.2021.1907739. [DOI] [PubMed] [Google Scholar]
- 60.Mueller-Steiner S, Zhou Y, Arai H, Roberson ED, Sun B, Chen J, Wang X, Yu G, Esposito L, Mucke L, Gan L. Antiamyloidogenic and neuroprotective functions of cathepsin B: implications for Alzheimer's disease. Neuron. 2006;51:703–714. doi: 10.1016/j.neuron.2006.07.027. [DOI] [PubMed] [Google Scholar]
- 61.Muralidar S, Ambi SV, Sekaran S, Thirumalai D, Palaniappan B. Role of tau protein in Alzheimer's disease: the prime pathological player. Int J Biol Macromol. 2020;163:1599–1617. doi: 10.1016/j.ijbiomac.2020.07.327. [DOI] [PubMed] [Google Scholar]
- 62.Nagahara AH, Merrill DA, Coppola G, Tsukada S, Schroeder BE, Shaked GM, Wang L, Blesch A, Kim A, Conner JM, Rockenstein E, Chao MV, Koo EH, Geschwind D, Masliah E, Chiba AA, Tuszynski MH. Neuroprotective effects of brain-derived neurotrophic factor in rodent and primate models of Alzheimer's disease. Nat Med. 2009;15:331–337. doi: 10.1038/nm.1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Narisawa-Saito M, Wakabayashi K, Tsuji S, Takahashi H, Nawa H. Regional specificity of alterations in NGF, BDNF and NT-3 levels in Alzheimer's disease. Neuroreport. 1996;7:2925–2928. doi: 10.1097/00001756-199611250-00024. [DOI] [PubMed] [Google Scholar]
- 64.Nasrolahi A, Javaherforooshzadeh F, Jafarzadeh-Gharehziaaddin M, Mahmoudi J, Asl KD, Shabani Z. Therapeutic potential of neurotrophic factors in Alzheimer's disease. Mol Biol Rep. 2022;49:2345–2357. doi: 10.1007/s11033-021-06968-9. [DOI] [PubMed] [Google Scholar]
- 65.Nyakas C, Granic I, Halmy LG, Banerjee P, Luiten PG. The basal forebrain cholinergic system in aging and dementia. Rescuing cholinergic neurons from neurotoxic amyloid-β42 with memantine. Behav Brain Res. 2011;221:594–603. doi: 10.1016/j.bbr.2010.05.033. [DOI] [PubMed] [Google Scholar]
- 66.Ouyang Q, Meng Y, Zhou W, Tong J, Cheng Z, Zhu Q. New advances in brain-targeting nano-drug delivery systems for Alzheimer's disease. J Drug Target. 2022;30:61–81. doi: 10.1080/1061186X.2021.1927055. [DOI] [PubMed] [Google Scholar]
- 67.Pardridge WM. Re-engineering biopharmaceuticals for delivery to brain with molecular Trojan horses. Bioconjug Chem. 2008;19:1327–1338. doi: 10.1021/bc800148t. [DOI] [PubMed] [Google Scholar]
- 68.Pardridge WM. Biopharmaceutical drug targeting to the brain. J Drug Target. 2010;18:157–167. doi: 10.3109/10611860903548354. [DOI] [PubMed] [Google Scholar]
- 69.Park H, Oh J, Shim G, Cho B, Chang Y, Kim S, Baek S, Kim H, Shin J, Choi H, Yoo J, Kim J, Jun W, Lee M, Lengner CJ, Oh YK, Kim J. In vivo neuronal gene editing via CRISPR-Cas9 amphiphilic nanocomplexes alleviates deficits in mouse models of Alzheimer's disease. Nat Neurosci. 2019;22:524–528. doi: 10.1038/s41593-019-0352-0. [DOI] [PubMed] [Google Scholar]
- 70.Peng L, Bestard-Lorigados I, Song W. The synapse as a treatment avenue for Alzheimer's disease. Mol Psychiatry. 2022;27:2940–2949. doi: 10.1038/s41380-022-01565-z. [DOI] [PubMed] [Google Scholar]
- 71.Pfundstein G, Nikonenko AG, Sytnyk V. Amyloid precursor protein (APP) and amyloid β(Aβ) interact with cell adhesion molecules: Implications in Alzheimer's disease and normal physiology. Front Cell Dev Biol. 2022;10:969547. doi: 10.3389/fcell.2022.969547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rassu G, Soddu E, Posadino AM, Pintus G, Sarmento B, Giunchedi P, Gavini E. Nose-to-brain delivery of BACE1 siRNA loaded in solid lipid nanoparticles for Alzheimer's therapy. Colloids Surf B Biointerfaces. 2017;152:296–301. doi: 10.1016/j.colsurfb.2017.01.031. [DOI] [PubMed] [Google Scholar]
- 73.Rincon MY, Zhou L, Marneffe C, Voytyuk I, Wouters Y, Dewilde M, Duqué SI, Vincke C, Levites Y, Golde TE, Muyldermans S. AAV-mediated delivery of a novel anti-BACE1 VHH reduces Abeta in an Alzheimer's disease mouse model. Hum Gene Ther. 2019;30:A95–A95. [Google Scholar]
- 74.Rodrigues BDS, Kanekiyo T, Singh J. Nerve growth factor gene delivery across the blood-brain barrier to reduce beta amyloid accumulation in AD mice. Mol Pharm. 2020;17:2054–2063. doi: 10.1021/acs.molpharmaceut.0c00218. [DOI] [PubMed] [Google Scholar]
- 75.Rosenberg JB, Kaplitt MG, De BP, Chen A, Flagiello T, Salami C, Pey E, Zhao L, Ricart Arbona RJ, Monette S, Dyke JP, Ballon DJ, Kaminsky SM, Sondhi D, Petsko GA, Paul SM, Crystal RG. AAVrh.10-mediated APOE2 central nervous system gene therapy for APOE4-associated Alzheimer's disease. Hum Gene Ther Clin Dev. 2018;29:24–47. doi: 10.1089/humc.2017.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sanati M, Khodagholi F, Aminyavari S, Ghasemi F, Gholami M, Kebriaeezadeh A, Sabzevari O, Hajipour MJ, Imani M, Mahmoudi M, Sharifzadeh M. Impact of gold nanoparticles on amyloid β-induced Alzheimer's disease in a rat animal model: involvement of STIM proteins. ACS Chem Neurosci. 2019;10:2299–2309. doi: 10.1021/acschemneuro.8b00622. [DOI] [PubMed] [Google Scholar]
- 77.Selkoe DJ. Treatments for Alzheimer's disease emerge. Science. 2021;373:624–626. doi: 10.1126/science.abi6401. [DOI] [PubMed] [Google Scholar]
- 78.Shyam R, Ren Y, Lee J, Braunstein KE, Mao HQ, Wong PC. Intraventricular delivery of siRNA nanoparticles to the central nervous system. Mol Ther Nucleic Acids. 2015;4:e242. doi: 10.1038/mtna.2015.15. [DOI] [PubMed] [Google Scholar]
- 79.Singer O, Marr RA, Rockenstein E, Crews L, Coufal NG, Gage FH, Verma IM, Masliah E. Targeting BACE1 with siRNAs ameliorates Alzheimer disease neuropathology in a transgenic model. Nat Neurosci. 2005;8:1343–1349. doi: 10.1038/nn1531. [DOI] [PubMed] [Google Scholar]
- 80.Singh YP, Rai H, Singh G, Singh GK, Mishra S, Kumar S, Srikrishna S, Modi G. A review on ferulic acid and analogs based scaffolds for the management of Alzheimer's disease. Eur J Med Chem. 2021;215:113278. doi: 10.1016/j.ejmech.2021.113278. [DOI] [PubMed] [Google Scholar]
- 81.Sioud M. RNA and CRISPR interferences: past, present, and future perspectives. Methods Mol Biol. 2020;2115:1–22. doi: 10.1007/978-1-0716-0290-4_1. [DOI] [PubMed] [Google Scholar]
- 82.Stepanichev M. Gene editing and Alzheimer's disease: is there light at the end of the tunnel? Front Genome Ed. 2020;2:4. doi: 10.3389/fgeed.2020.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Suh J, Romano DM, Nitschke L, Herrick SP, DiMarzio BA, Dzhala V, Bae JS, Oram MK, Zheng Y, Hooli B, Mullin K, Gennarino VA, Wasco W, Schmahmann JD, Albers MW, Zoghbi HY, Tanzi RE. Loss of ataxin-1 potentiates Alzheimer's pathogenesis by elevating cerebral BACE1 transcription. Cell. 2019;178:1159–1175. doi: 10.1016/j.cell.2019.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tagalakis AD, Lee DH, Bienemann AS, Zhou H, Munye MM, Saraiva L, McCarthy D, Du Z, Vink CA, Maeshima R, White EA, Gustafsson K, Hart SL. Multifunctional, self-assembling anionic peptide-lipid nanocomplexes for targeted siRNA delivery. Biomaterials. 2014;35:8406–8415. doi: 10.1016/j.biomaterials.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 85.Tan J, Wang Y, Yip X, Glynn F, Shepherd RK, Caruso F. Nanoporous peptide particles for encapsulating and releasing neurotrophic factors in an animal model of neurodegeneration. Adv Mater. 2012;24:3362–3366. doi: 10.1002/adma.201200634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Thambisetty M, Howard R, Glymour MM, Schneider LS. Alzheimer's drugs: does reducing amyloid work? Science. 2021;374:544–545. doi: 10.1126/science.abl8366. [DOI] [PubMed] [Google Scholar]
- 87.Tuszynski MH, Thal L, Pay M, Salmon DP, U HS, Bakay R, Patel P, Blesch A, Vahlsing HL, Ho G, Tong G, Potkin SG, Fallon J, Hansen L, Mufson EJ, Kordower JH, Gall C, Conner J. A phase 1 clinical trial of nerve growth factor gene therapy for Alzheimer disease. Nat Med. 2005;11:551–555. doi: 10.1038/nm1239. [DOI] [PubMed] [Google Scholar]
- 88.Wadetwar RN, Godbole AP. Nanocarriers: a tool for effective gene delivery. Nanopharm Adv Deliv Sys. 2021;2021:161–185. [Google Scholar]
- 89.Wang P, Zheng X, Guo Q, Yang P, Pang X, Qian K, Lu W, Zhang Q, Jiang X. Systemic delivery of BACE1 siRNA through neuron-targeted nanocomplexes for treatment of Alzheimer's disease. J Control Release. 2018;279:220–233. doi: 10.1016/j.jconrel.2018.04.034. [DOI] [PubMed] [Google Scholar]
- 90.Wang Z, Cheng Y, Zhao D, Pliss A, Liu J, Luan P. Synergic treatment of Alzheimer's disease with brain targeted nanoparticles incorporating NgR-siRNA and brain derived neurotrophic factor. Smart Mater Med. 2020;1:125–130. [Google Scholar]
- 91.Wu H, Li J, Zhang Q, Yan X, Guo L, Gao X, Qiu M, Jiang X, Lai R, Chen H. A novel small Odorranalectin-bearing cubosomes: preparation, brain delivery and pharmacodynamic study on amyloid-β25-35-treated rats following intranasal administration. Eur J Pharm Biopharm. 2012;80:368–378. doi: 10.1016/j.ejpb.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 92.Xie Y, Ye L, Zhang X, Cui W, Lou J, Nagai T, Hou X. Transport of nerve growth factor encapsulated into liposomes across the blood-brain barrier: in vitro and in vivo studies. J Control Release. 2005;105:106–119. doi: 10.1016/j.jconrel.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 93.Xu H, Zhou Q, Liu B, Cheng KW, Chen F, Wang M. Neuroprotective potential of Mung Bean (Vigna radiata L.). Polyphenols in Alzheimer's disease: a review. J Agric Food Chem. 2021;69:11554–11571. doi: 10.1021/acs.jafc.1c04049. [DOI] [PubMed] [Google Scholar]
- 94.Yang Z, Li Y, Wang Z. Recent advances in the application of mesenchymal stem cell-derived exosomes for cardiovascular and neurodegenerative disease therapies. Pharmaceutics. 2022;14:618. doi: 10.3390/pharmaceutics14030618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yu C, Li L, Hu P, Yang Y, Wei W, Deng X, Wang L, Tay FR, Ma J. Recent advances in stimulus-responsive nanocarriers for gene therapy. Adv Sci (Weinh) 2021;8:2100540. doi: 10.1002/advs.202100540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zhang C, Gu Z, Shen L, Liu X, Lin H. A dual targeting drug delivery system for penetrating blood-brain barrier and selectively delivering siRNA to neurons for Alzheimer's disease treatment. Curr Pharm Biotechnol. 2017;18:1124–1131. doi: 10.2174/1389201019666180226152542. [DOI] [PubMed] [Google Scholar]
- 97.Zhang C, Gu Z, Shen L, Liu X, Lin H. In vivo evaluation and Alzheimer's disease treatment outcome of siRNA loaded dual targeting drug delivery system. Curr Pharm Biotechnol. 2019;20:56–62. doi: 10.2174/1389201020666190204141046. [DOI] [PubMed] [Google Scholar]
- 98.Zhao J, Fu Y, Yasvoina M, Shao P, Hitt B, O'Connor T, Logan S, Maus E, Citron M, Berry R, Binder L, Vassar R. Beta-site amyloid precursor protein cleaving enzyme 1 levels become elevated in neurons around amyloid plaques: implications for Alzheimer's disease pathogenesis. J Neurosci. 2007;27:3639–3649. doi: 10.1523/JNEUROSCI.4396-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zheng M, Tao W, Zou Y, Farokhzad OC, Shi B. Nanotechnology-based strategies for siRNA brain delivery for disease therapy. Trends Biotechnol. 2018;36:562–575. doi: 10.1016/j.tibtech.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 100.Zhou Y, Zhu F, Liu Y, Zheng M, Wang Y, Zhang D, Anraku Y, Zou Y, Li J, Wu H, Pang X, Tao W, Shimoni O, Bush AI, Xue X, Shi B. Blood-brain barrier-penetrating siRNA nanomedicine for Alzheimer's disease therapy. Sci Adv. 2020;6:eabc7031. doi: 10.1126/sciadv.abc7031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zilony-Hanin N, Rosenberg M, Richman M, Yehuda R, Schori H, Motiei M, Rahimipour S, Groisman A, Segal E, Shefi O. Neuroprotective effect of nerve growth factor loaded in porous silicon nanostructures in an Alzheimer's disease model and potential delivery to the brain. Small. 2019;15:e1904203. doi: 10.1002/smll.201904203. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


