Fractures of the proximal radial metadiaphysis are relatively uncommon.5 Only a few cases of isolated fractures around bicipital tuberosity have been reported.5,7 Available treatment methods for radial head/neck and diaphyseal fractures may be difficult to apply to fractures of the metadiaphyseal proximal radius. The morphology of the bone, its articulation with the ulna, nearby neurovascular structures, and the origins and insertions of various muscles limit safe surgical exposure as well as the application of an implant. Precontoured radial head plates and plates intended for the radial diaphysis can be difficult to apply to the anatomy of the metadiaphyseal proximal radius in a manner that satisfactorily restores the native anatomy, preserves prono-supination, and provides sufficient fixation proximal and distal to the fracture.5 In this report, we describe a rare case of proximal radial fracture in which good postoperative results were achieved.
Case presentation
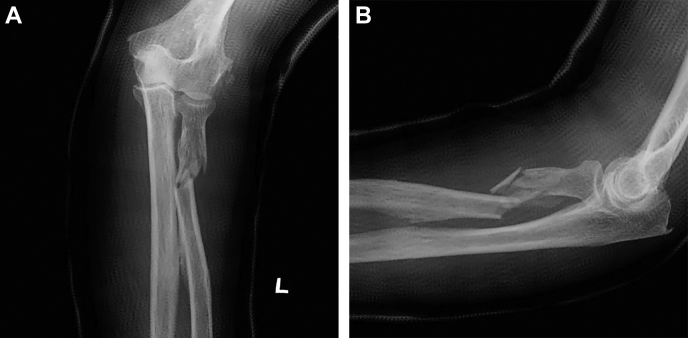
A 77-year-old right-handed woman fell down and hit her left hand against the bathroom wall. Two days after the injury, she visited a local orthopedic clinic complaining left proximal forearm pain where she was subsequently diagnosed with a fracture of the proximal radius metadiaphysis. After 1 week of immobilization, she was referred to our department for surgery given that substantial fracture displacement had been observed. Her medical and surgical history included bilateral total knee arthroplasty for osteoarthritis of the knee, hypertension, dyslipidemia, and fatty liver. On physical examination, subcutaneous hemorrhage around the left elbow and mild swelling of the forearm were observed, with no open wound. The sensory and motor functions of her left fingers and wrist were intact, with no evidence of neural damage. Radiography revealed a fracture on the proximal radial metadiaphysis with a few displaced fragments around the bicipital tuberosity (Figs. 1 and 2). Joint dislocation was not found on the elbow or wrist. Old fracture fragments were found on the lateral epicondyle of the humerus.
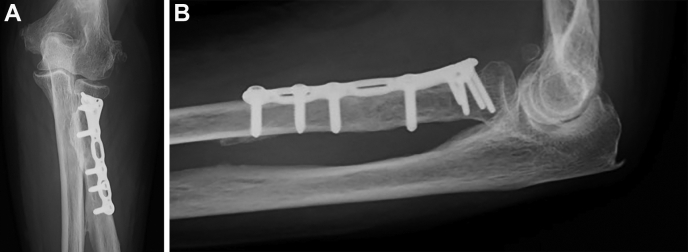
Figure 1.
Plain radiographs demonstrating a fracture of proximal radius metadiaphysis around bicipital tuberosity with fracture displacement. (A) Frontal view. (B) Lateral view.
Figure 2.
Three-dimensional computed tomography image demonstrating a fracture of proximal radius metadiaphysis around bicipital tuberosity with fracture displacement. (A) Frontal view. (B) Lateral view.
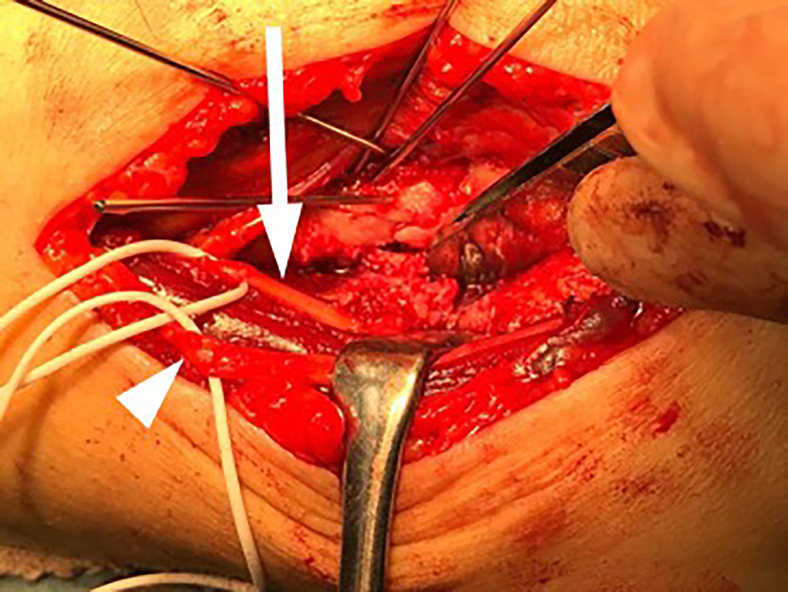
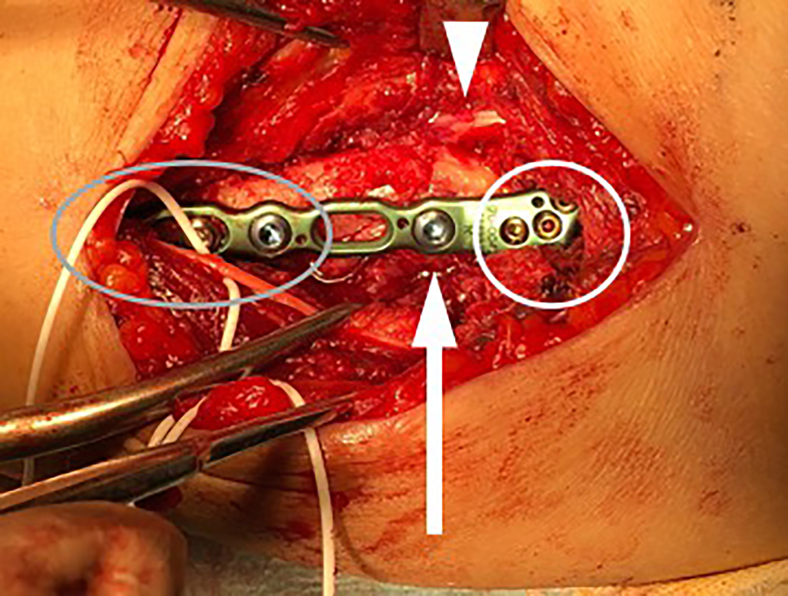
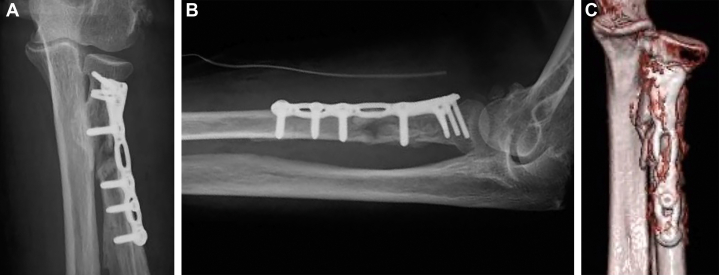
Surgical treatment was selected to reposition the fracture dislocation and shorten the immobilization period in order to achieve acceptable elbow function with a quick return to daily life. Under general anesthesia, open reduction and internal fixation were performed 17 days after the injury through volar Henry approach, during which the superficial branch of the radial nerve and the lateral antebrachial cutaneous nerve were identified and carefully protected (Fig. 3). We found that the biceps tendon was intact, but its small bony fragment attachment was displaced by the fracture (Fig. 4) Displaced bony fragments were repositioned and fixed with Acu-Loc Volar Distal Ulna Long Right (Acumed, Hillsboro, OR, USA). Four 2.3-mm locking screws were inserted into the proximal fragment, one 3.5-mm cortical screw and two 3.5-mm locking screws were inserted into the distal fragment, and one 3.5-mm locking screw was inserted into the third fragment (Figs. 4 and 5). Following 2 weeks of immobilization, a rehabilitation program was prescribed. Further, bone union was achieved after 4 months of surgery with no angular deformity or shortening (Fig. 6). After 10 months, the patient showed no difficulties in activities of daily living, with her elbow joint regaining nearly normal range of motion (right/left; flexion = 135°/135°, extension = 0/−5°, pronation = 90°/60°, and supination = 90°/80°). Her disabilities of the arm, shoulder, and hand score was 27.5; notably, this score was influenced by a recent left distal radial fracture.
Figure 3.
Intraoperative images of the proximal radius explored via the volar Henry approach. The superficial branch of the radial nerve (white arrow) and the lateral antebrachial cutaneous nerve (arrow head) were identified and protected throughout the surgery. The fracture was temporarily fixed using Kirchner wires.
Figure 4.
The biceps tendon was intact. Moreover, the biceps tendon’s small bony fragment attachment was displaced by the fracture (arrow head). The fracture dislocation was repositioned and fixed using Acu-Loc Volar Distal Ulna Long Right (Acumed, Hillsboro, OR, USA) while inserting four 2.3-mm locking screws into proximal fragment (white circle), one 3.5-mm cortical screw and two 3.5-mm locking screws into distal fragment (gray circle), and one 3.5-mm locking screw into third fragment (white arrow).
Figure 5.
Postoperative radiographs and three-dimensional computed tomography image demonstrating that the fracture dislocation was well repositioned and that the plate was in a satisfactory position (A, B, C). The width of the plate was the same as that of the proximal radius (C).
Figure 6.
At 4 months postoperatively, radiographs revealed bone union with no angular deformity or bone shortening. (A) Frontal view. (B) Lateral view.
Discussion
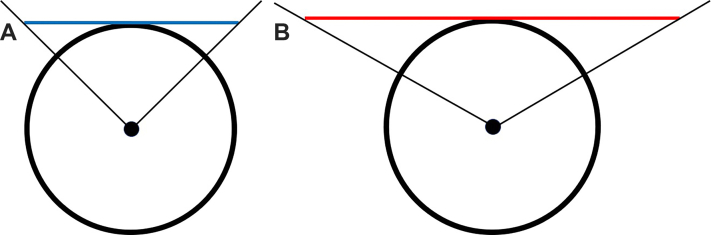
A number of case reports have utilized plates or intramedullary nails to treat fractures of the proximal radius metadiaphysis.2,5,7 Moreover, plates for the distal radius and mini-plates have been used.2,5 During the selection of an implant, the plate width and the fixation force must be considered because these are often incompatible. We used a plate for the distal ulna for two reasons. First, the width of the plate corresponded to the proximal radius. Demetri et al utilized the arc of the nonarticulating proximal radius (ie, the safe zone used for proximal radius plates in fractures extending to the bicipital tuberosity).5 The safe zone expands approximately 65° anterior and 45° posterior to the bisecting reference line created with the forearm in the neutral position.12 The considerable number of cases in which the distal radius plate had been turned over, Demetri et al found that the distal radius plate can cause impingement with terminal supination, which should be removed after the fracture has healed.5 Kuhn et al noted that the min–max width value of the proximal radial neck was 13.9-16.3 mm.8 Studies have shown that distal width of the distal radius plates was 24-26 mm,9 whereas that of the distal ulna plate used herein was 14 mm,1 which was almost equal to or smaller than the width of the radial neck. Using the volar distal ulna plate for patients whose width of proximal radial neck is 13.9 mm would create an approximately 90° geometric angle between both edges of the plate and the bone axis of the proximal radial neck. In contrast, using a distal radius plate for patients whose proximal radial neck has a width of 13.9 mm would create an approximately 120° geometric angle (Fig. 7). Therefore, distal ulna plates may lower the risk of impingement compared to using distal radius plates. Actually, despite the fact that the plate had to be placed ulnar to the safety zone in order to insert the screw into the dorsal fragment, 10 months after her surgery, our patient had a better range of motion in terms of both pronation and supination compared to previously reported cases using plates.5 Therefore, removing the hardware in our case was unnecessary. Second reason is that locking screws are available. In fact, four locking screws can be inserted into the distal part of the plate (ie, the proximal radial fragment), allowing for its firm fixation. Moreover, hand plates or foot plates have been used in some cases.2,5 However, in the case of an elderly woman with poor bone quality, such as in the current case, strong fixation is desirable, making this plate more advantageous. Given that the ulna and radius are both forearm bones of similar size and load-bearing capacity, it is reasonable to use a distal ulna plate for fractures of the proximal radial diaphysis. However, this plate is only available for fractures up to 66 mm long and is not applicable for fractures requiring longer plates. An intramedullary nail is not recommended for this type of fracture given that it does not provide sufficient proximal fixation, as suggested by Imao et al.7
Figure 7.
Simplified schema of the angle between both ends of the plate and the bone axis. The circles indicate axial planes of a proximal radial neck, the dots indicate the bone axis of the proximal radial neck, the blue line indicates axial plane of the distal portion of the volar distal ulna plate (A), and the red line indicates that of distal radius plate (B), respectively. Using the volar distal ulna plate for patients whose proximal radial neck has a width of 13.9 mm would create an approximately 90° geometric angle between both ends of the plate and the bone axis (A). In contrast, using a distal radius plate would create an approximately 120° geometric angle (B).
In addition, this case report provides important information on the choice of surgical approach. However, the surgical approaches for treating proximal radial metadiaphyseal fractures are still controversial. The most commonly used approaches for proximal radius fractures are the volar Henry and dorsal Thompson approaches.3, 4, 5, 6,10,11,13 According to previous reports, the dorsal approach has been recommended given that it allows for more proximal plate placement and direct visualization and protection of the posterior interosseous nerve (PIN). Furthermore, it is difficult to place a plate proximal to the biceps tuberosity, and PIN may be at risk of being injured during screw insertion when using the volar approach.3, 4, 5, 6,10,11,13 However, a recent multicenter study showed that the volar approach has similar safety and placement ability as the dorsal approach for biceps tuberosity osteosynthesis cases. Moreover, the same study concluded that the decision should be based on the surgeon's experience.4 In fact, we were able to place the plate in the intended position using the volar Henry approach without complications.
The limitation of this study is the insufficient numbers of cases. It is desirable that similar case reports be accumulated and verified.
When fixing plates to fractures in uncommon sites, the anatomy and biomechanics of the fracture site, as well as the shape and fixing capacity of the plate, should be thoroughly considered. Postoperative evaluation results of similar cases should be compared based on whether bone union was achieved, the duration of bone healing, the range of motion, and the disabilities of the arm, shoulder, and hand score.
Conclusion
We herein report our experience with a case that developed very rare fracture around the bicipital tuberosity of the radius. A distal ulna plate, which had not been previously reported, was useful for avoiding impingements and achieving a robust fixation, subsequently achieving good postoperative results. The volar Henry approach allowed for the safe exposure of the fracture and sufficient plate placement at the intended position.
Acknowledgment
The authors would like to thank Enago (www.enago.jp) for the English language review.
Footnotes
Institutional review board approval was not required for this case report.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
References
- 1.Acumed Acu-Loc2 wrist plating system surgical technique. https://www.acumed.net/wp-content/uploads/2018/06/Acumed-Surgical-Technique-EN-Acu-Loc-2-HNW00-06-AB.pdf Available from: Accessed 18 May, 2022.
- 2.Badia A., Sambandam S.N., Khanchandani P. Proximal radial fracture after revision of distal biceps tendon repair: a case report. J Shoulder Elbow Surg. 2007;16:e4–e6. doi: 10.1016/j.jse.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 3.Cross J.D., White J.A., Johnson A.E., Blair J.A., Hsu J.R. Comparison of dorsal and volar approaches to the proximal radius. Orthopedics. 2011;34:93. doi: 10.3928/01477447-20101221-14. [DOI] [PubMed] [Google Scholar]
- 4.Dashe J., Murray B., Tornetta P., Grott K.M., Mullis B., Bellevue K.D., et al. Henry versus thompson approach for fixation of proximal third radial shaft fractures: a multicenter study. J Orthop Trauma. 2020;34:108–112. doi: 10.1097/BOT.0000000000001651. [DOI] [PubMed] [Google Scholar]
- 5.Demetri L., Young C., Patterson J.T., Kandemir U., Morshed S., Immerman I., et al. Management of metadiaphyseal proximal radius fractures. Tech Hand Up Extrem Surg. 2020;25:156–164. doi: 10.1097/BTH.0000000000000325. [DOI] [PubMed] [Google Scholar]
- 6.Henry A.K. Complete exposure of the radius. Br J Surg. 2005;13:506–508. doi: 10.1002/bjs.1800135109. [DOI] [Google Scholar]
- 7.Imao K., Miwa H., Watanabe K., Imai N., Endo N. A case report of an isolated fracture through the radial bicipital tuberosity. Int J Surg Case Rep. 2017;41:230–233. doi: 10.1016/j.ijscr.2017.10.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuhn S., Burkhart K.J., Schneider J., Muelbert B.K., Hartmann F., Mueller L.P., et al. The anatomy of the proximal radius: implications on fracture implant design. J Shoulder Elbow Surg. 2012;21:1247–1254. doi: 10.1016/j.jse.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 9.Limthongthang R., Bachoura A., Jacoby S.M., Osterman A.L. Distal radius volar locking plate design and associated vulnerability of the flexor pollicis longus. J Hand Surg Am. 2014;39:852–860. doi: 10.1016/j.jhsa.2014.01.038. [DOI] [PubMed] [Google Scholar]
- 10.Mekhail A.O., Ebraheim N.A., Jackson W.T., Yeasting R.A. Vulnerability of the posterior interosseous nerve during proximal radius exposures. Clin Orthop Relat Res. 1995;315:199–208. [PubMed] [Google Scholar]
- 11.Nasab S.A.M., Sarrafan N., Fakoor M., Mohammadzadeh M. Comparison of volar and dorsal approaches for surgical treatment in fracture of proximal half of the radius. Pak J Med Sci. 2013;29:532–535. doi: 10.12669/pjms.292.3226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith G.R., Hotchkiss R.N., York N. Radial head and neck fractures: anatomic guidelines for proper placement of internal fixation. J Shoulder Elbow Surg. 1996;5:113–117. doi: 10.1016/s1058-2746(96)80005-x. [DOI] [PubMed] [Google Scholar]
- 13.Thompson J.E. Anatomical methods of approach in operations on the long bones of the extremities. Ann Surg. 1918;68:309–329. doi: 10.1097/00000658-191809000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]