Abstract
Background
The ulnar collateral ligament (UCL) is a commonly injured elbow stabilizer during throwing. Shear wave elastography (SWE) is a technique that may reveal structural changes in the UCL that are indicative of ligament health and injury risk. The purpose of this study was to assess preseason and inseason shear wave velocity (SWV) in the UCL of collegiate pitchers and to asses repeatability of this measurement technique in healthy volunteers.
Methods
Seventeen collegiate baseball pitchers and 11 sex-matched volunteers were recruited. Two-dimensional SWE of the UCL was performed by a single radiologist. In pitchers, SWV was measured at the proximal, midsubstance, and distal UCL for dominant and nondominant elbows preseason, midseason, and postseason, and Kerlan-Jobe Orthopaedic Clinic (KJOC) Shoulder and Elbow questionnaire scores were recorded. In volunteers, SWV was measured at UCL midsubstance in dominant elbows at 3 separate occasions over 1 week. An independent samples t-test was used to compare preseason midsubstance measures between pitchers and the healthy volunteers. A mixed-model analysis of covariance (covaried on preseason measures) was used to compare SWV measures at the preseason, midseason, and postseason time points. A similar generalized linear model for nonparametric data was used to compare KJOC scores. Type-I error was set at P < .05.
Results
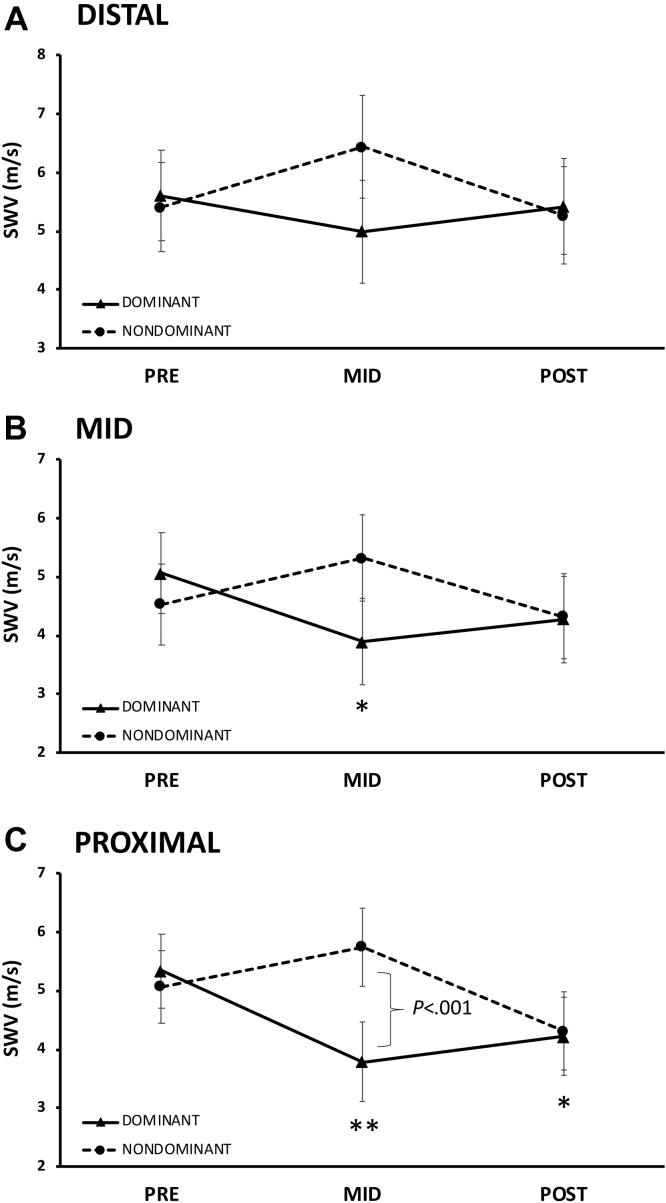
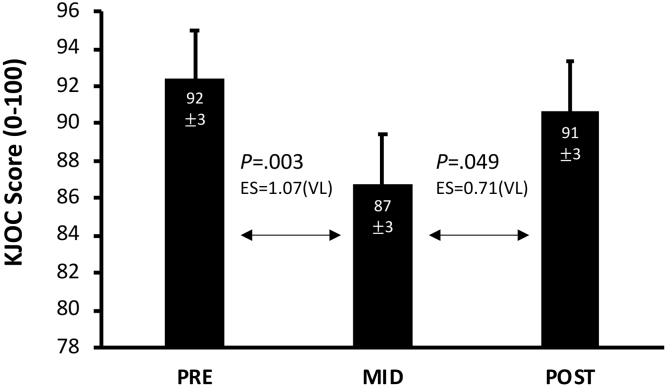
Mean preseason midsubstance dominant arm UCL SWV did not significantly differ between the pitchers (5.40 ± 1.65 m/s) compared to the healthy volunteers (4.35 ± 1.45 m/s). For inseason measures among the pitchers, a decrease in midsubstance (−1.17 ± 0.99 m/s, P = .021) and proximal (−1.55 ± 0.91 m/s, P = .001) SWV was observed at midseason compared to preseason. The proximal measure was also observed to be significantly lower than the nondominant arm (−1.97 ± 0.95 m/s, P < .001). Proximal SWV remained reduced relative to the preseason and the postseason mark (−1.13 ± 0.91 m/s, P = .015). KJOC scores decreased at midseason compared to preseason (P = .003) but then increased to a similar preseason value at the postseason measurement (preseason = 92 ± 3, midseason = 87 ± 3, postseason = 91 ± 3). The repeatability coefficient of SWE in the volunteer cohort was 1.98 m/s.
Conclusion
Decreased SWV in the proximal and midsubstance of the dominant arm UCL at midseason suggests structural changes indicative of increasing laxity or ‘softening’ of the UCL. Associated decline in KJOC scores suggests that these changes are associated with functional decline. Future studies with more frequent sampling would be invaluable to further explore this observation and its significance for predicting and managing UCL injury risk.
Keywords: Ulnar collateral ligament (UCL), Shear wave elastography (SWE), Shear wave velocity (SWV), Baseball, Throwing, Pitching, Elbow
The anterior bundle of the ulnar collateral ligament (UCL) is a frequently injured structure in the elbow of baseball pitchers, accounting for more than 460,000 days lost and more than $7 billion in expenses since the year 2000 in Major League Baseball.9,10,32 Collegiate baseball players suffer similar loss of productivity and professional opportunities plummet after UCL injury.10,12 Pitchers are prone to UCL injury because each throwing motion subjects the elbow to more than 120N of valgus force, half of which is resisted by the UCL alone.5,14,32 Over time, repetitive stretching of the UCL leads to changes in the ligament’s structure which can ultimately lead to partial or complete rupture.20,28,33 UCL injuries can occur anywhere along the ligament, but seem to more frequently involve the proximal humeral attachment and midsubstance.11,19
A recent systematic review found the reported sensitivity of magnetic resonance imaging for diagnosing partial and full thickness tears of the UCL ranges from 57%-100%, improving to 81%-100% with intra-articular contrast.6,23 While magnetic resonance imaging can identify signal changes in the injured ligament, it is poorly predictive for impending UCL rupture, time consuming and may not be readily available at the point-of-care.2,16,18,21 Stress ultrasonography has been used to infer changes in UCL structure by measuring elbow joint laxity, but this has similarly shown mixed results for predicting UCL injuries.4,8,30
Given the lack of a reliable modality to assess the health of the UCL prior to rupture, our group previously investigated the utility of 2-dimensional (2D) shear wave elastography (SWE) in assessing the UCL.17 SWE relies upon generation of shear waves in the imaged tissue, often through the use of a focused sonographic ‘push pulse’ (acoustic radiation force impulse).24 The shear waves are then tracked sonographically using various speckle tracking techniques, and the shear wave velocity (SWV) is determined. Once the SWV is known, the tissue’s shear modulus can be calculated in kilopascals. SWV is often reported as a surrogate for the shear modulus, as the latter is a derived value, while the SWV is directly obtained. Prior studies using SWE in Achilles’ and patellar tendons found higher SWV was associated with stiff, healthy tissue and lower SWV was associated with soft, tendonotic, degenerative tissue.13,26,31
Extrapolating the results from tendons, it was felt that this technology may be a useful way to assess ligament health. In our previous study, we examined the UCL in both dominant and nondominant elbows of healthy volunteers and established normative values while assessing the repeatability of the technique.17 Only one prior report exists to our knowledge where SWE was used to assess the UCL in elite throwing athletes.22 That report included 1 collegiate baseball pitcher with a ruptured UCL and found the SWV was 79% lower in the injured UCL compared to the contralateral UCL. The present study further investigates the utility of SWE in assessing the UCL of elite overhead throwing athletes.
The primary objective of this study was to estimate preseason UCL SWV in elbows of collegiate pitchers and to follow the trend of SWV in pitchers’ UCL over a collegiate season. A secondary objective was to evaluate normative UCL SWV values in the dominant arms of healthy volunteers using a lower frequency transducer than in our previous study (to improve reliability) and to assess the repeatability coefficient with this transducer.17 Our hypotheses were the following: SWV in pitchers’ dominant arms would change throughout the course of a season and would differ between pitchers’ dominant and nondominant arms. As secondary aims, we also sought to determine if SWV would be different in pitchers’ elbows at baseline (preseason) compared to healthy volunteers and to determine if using a lower frequency transducer would result in better interobserver repeatability than our prior study.16 We present the following article in accordance with the Consolidated Standards of Reporting Trials reporting checklist.
Materials and methods
Population
Seventeen male National Collegiate Athletic Association Division I collegiate baseball pitchers and 11 gender-matched healthy volunteers were recruited for the study from October to November 2018. All pitching athletes were dedicated pitchers who did not alternate between other defensive positions. Exclusion criteria were active elbow injury at baseline. All participants provided a written informed consent for participation and the study was approved by our institutional review board. An a priori power analysis indicated a sample size of 10 subjects in each group would detect a change in SWV of 1.59 m/s over 2 time points at a power of 80% and an alpha of 0.05. This effect size was selected based on the results of a pilot study performed by our group,17 which demonstrated a repeatability coefficient of 1.95 m/s (95% confidence interval [CI] 1.61-2.37 m/s), that is, the study was powered to demonstrate a change in SWV at least as small as the lower bounds of the repeatability coefficient of the diagnostic modality. Inseason pitching regimens involved either in-game performances or a scheduled bullpen (30-50 pitches) at least twice per week.
Shear wave elastography protocol
Pitchers underwent SWE of the dominant elbow UCL at 3 separate time intervals between January and May 2019: “preseason” (1/15/2019), “midseason” (3/27/2019), and “postseason” (5/8/2019). Pitchers completed the Kerlan-Jobe Orthopaedic Clinic (KJOC) Shoulder and Elbow questionnaire at each time point as well, which is a validated subjective assessment of upper extremity dysfunction.1,15 Healthy volunteers underwent SWE of the dominant elbow UCL at 3 separate time intervals over the span of 1 week in October 2018. The primary measurement was SWV, as measured with an Acuson S3000 ultrasound machine (Virtual Touch Imaging and Quantification, Siemens Medical Solutions; Issaquah, WA, USA) using a 9 MHz linear transducer (9L4; Siemens Medical Solutions; Issaquah, WA, USA), which was the most suitable probe available for musculoskeletal applications with SWE capability on this system.
All examinations were performed by an unblinded, fellowship-trained radiologist with 3 years’ experience in sonoelastography. The subject was seated upright with the arm in approximately 15-30° of flexion and fixed in a Telos SD900 stress machine with 5N of valgus stress applied across the elbow. Fig. 1 demonstrates subject position with the elbow in valgus stress.
Figure 1.
Telos positioning. Subject seated upright with arm in 15-30° of flexion in a Telos SD900 stress machine with a fixed 5N of valgus stress applied across the elbow.
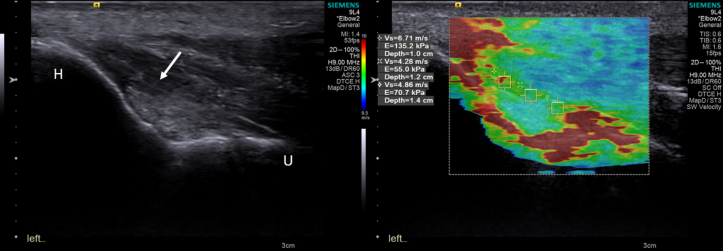
The anterior bundle of the UCL was identified as an oblique isoehoic to hypoechoic band deep to the common flexor tendon extending from the medial epicondyle of the humerus to the sublime tubercle of the ulna (Fig. 2). Care was taken to minimize transducer pressure while maintaining adequate skin contact with an appropriate amount of ultrasound coupling gel. 2D color elastograms were obtained and 1 mm square regions of interest (ROIs) were deposited as follows. For the pitcher cohort, ROIs were drawn at proximal, midsubstance, and distal locations of the UCL on the dominant and nondominant elbow. Fig. 2 illustrates an example of ROI position for the pitcher cohort. This was repeated for 3 separate elastograms obtained in the same session, for a total of 3 measurements at each location, 9 measurements total. Median value at each location and time point was recorded and used for subsequent analysis. For volunteers, elastograms were obtained from the dominant elbow during each session at the midsubstance of the UCL on each elastogram. Median value was recorded and used for subsequent analysis. Compared to the pitching athletes, 2 additional measurements (total of 5) were performed at the midsubstance to further assess repeatability of the measure. This protocol was repeated for each group at the matched scheduled time intervals.
Figure 2.
Assessment of shear wave velocity. Gray-scale sonogram (Left) demonstrating the UCL (arrow), an oblique isoechoic to hypoechoic band deep to the common flexor tendon extending from the medial epicondyle of the humerus (H) to the sublime tubercle of the ulna (U). Elastogram (Right) overlaid on the ulnar collateral ligament of a collegiate pitcher. Square ROIs were placed on the proximal, midsubstance and distal ulnar collateral ligament. ROI, regions of interest.
Statistical analysis
All data analyses were performed in SPSS Statistics software (v23; IBM Corp., Armonk, NY, USA). An independent samples t-test was used to compare preseason midsubstance measures between pitchers and the healthy volunteer group. A 2-arm by 3–time point mixed model analysis of covariance (covaried on preseason measures) was used to compare SWV measures at the preseason, midseason, and postseason time points. Similarly, a generalized linear mixed model for nonparametric data was used to compare KJOC scores at the same time points. For significant interactions observed for SWV and KJOC measures, a Bonerroni post hoc test was performed to detect significant pairwise comparisons. Finally, correlation analysis was used to determine the relationship between SWV and KJOC measures among the pitchers across all measurement time points. Correlation strength was interpreted as follows: r = 0-0.3 (weak); r = 0.3-0.7 (moderate); r = > 0.7 (strong). Type-I Error for all analyses was set at α = 0.05 for all analyses. For significant pairwise comparisons, effect size (ES) is reported as a Cohen’s d statistic and interpreted as follows: 0-0.1, Negligible (N); 0.1-0.3, Small (S); 0.3-0.5, Moderate (M); 0.5-0.7, Large (L); > 0.7, Very large (VL).7,29 The reliability and repeatability of SWV measurements were assessed in similar manner as this group’s prior study, using the healthy volunteer cohort.17 For the healthy volunteer cohort, the median and interquartile range (IQR) were calculated for each set of 10 SWV measurements. A set of measurements was deemed reliable if the IQR/median ratio was < 0.3.3 Secondary analysis was conducted to estimate the repeatability coefficient (RC), which is defined as (where is the within-subject variance) and which represents the maximum difference that is likely to occur between 2 repeated test results with a probability of 95% (29). Unreliable data (IQR/median > 0.3) were excluded from RC calculation.
Results
Subject characteristics
Of the 11 volunteers, 1 could not complete all 3 scans due to illness and was excluded from analysis. The remaining 10 volunteers were included in the final analysis. Of the 17 pitchers initially recruited for the study, 14 completed preseason scans and were included in baseline analysis and comparison to healthy controls, 13 completed midseason evaluation, and 12 completed final postseason evaluation. One pitcher was unavailable for all 3 time points. Reasons for subject drop-out included nonelbow related injury, release from the team, and academic ineligibility. Mean age was 19.7 ± 1.4 years for pitchers and 31.2 ± 4.7 years for volunteers. All subjects were male; 77.8% of pitchers and 100% of volunteers were right-handed. Table I summarizes participant demographics.
Table I.
Participant demographics.
| Pitchers | Healthy volunteers | |
|---|---|---|
| N | 16 | 10 |
| Age (yrs) | 20.0 1.4 | 31.2 4.7 |
| Right Handedness | 14/16 | 10/10 |
| Years Played (yrs) | 13.3 4.6 | N/A |
Data are presented as counts and as means standard deviation.
UCL SWV in pitchers
UCL SWV measures among the pitching athletes are shown in Fig. 3. A decrease in midsubstance [-1.17 ± 0.99 m/s, P = .021, ES = 0.82 (VL), Fig. 3B] and proximal [-1.55 ± 0.91 m/s, P = .001, ES = 1.19 (VL), Fig. 3C] SWV measures were observed at the midseason mark compared to preseason and the proximal measure was also observed to be significantly lower than the nondominant arm [-1.97 ± 0.95 m/s, P < .001, ES = 1.46 (VL) Fig. 3C]. Proximal SWV measures remained reduced relative to baseline at the postseason mark [-1.13 ± 0.91 m/s, P = .015, ES = 0.87 (VL) Fig. 3C].
Figure 3.
SWV in collegiate pitchers across a sport season. Data are shown as means ± 95% CI for UCL SWV expressed in meters per second (m/s) at preseason, midseason, and postseason assessment time points measured at the distal (A), midsubstance (B), and proximal (C) UCL in the dominant and nondominant arms. ∗,∗∗ = Significantly different from preseason measurement at P < .05 and P < .01 respectfully. SWV, shear wave velocity; CI, confidence interval; UCL, ulnar collateral ligament.
KJOC scores
KJOC scores assessed in the pitching athletes at the preseason, midseason, and postseason time points are shown in Fig. 4 where scores were observed to decrease at midseason compared to preseason but then increased to a similar preseason value at the postseason measurement (P < .05). When analyzed across all measurement time points, SWV measures were observed to be moderately correlated with KJOC scores (midsubstance: r = 0.401, P = .002 | proximal: r = 0.345, P = .009 | distal: r = 0.360, P = .028).
Figure 4.
KJOC scores. Data are shown as means ± 95% CI for KJOC scores recorded at preseason, midseason, and postseason assessment time points. Significance set at P < .05. For significant pairwise comparisons, effect size (ES) is reported as a Cohen’s d statistic and interpreted as follows: 0-0.1, Negligible (N); 0.1-0.3, Small (S); 0.3-0.5, Moderate (M); 0.5-0.7, Large (L); > 0.7, Very large (VL). KJOC, Kerlan-Jobe Orthopaedic Clinic; CI, confidence interval.
Mean UCL SWV in volunteers
Mean SWV at the midsubstance UCL of the dominant elbow in healthy volunteers across 3 time points was 4.35 ± 1.45 m/s. Reliable results (as defined by IQR/median ratio < 0.3) were obtained in 24 of 30 measurements (80%). Repeatability coefficient was 1.98 m/s (95% CI 1.35 to 2.89 m/s). Mean preseason SWV at the midsubstance UCL of the dominant elbow in pitchers compared to volunteers was 5.40 ± 1.65 m/s vs. 4.19 ± 0.85 m/s, respectively. There was a strong trend toward higher SWV in pitchers as compared to volunteers, although the difference did not reach statistical significance (P = .056).
Discussion
UCL injury is a significant concern for baseball pitchers, and a point-of-care modality to monitor the health of the UCL would have the potential to reduce injury and improve pitcher longevity. Ultrasound is a widely available point-of-care modality, and we previously reported on the repeatability of 2D-SWE of the UCL in a cohort of healthy volunteers.17 To our knowledge, this study is the first to longitudinally measure the SWV of the UCL in baseball pitchers over the duration of a season, and we demonstrated a statistically significant decline in the proximal and midsubstance of the dominant arm UCL SWV at midseason compared to preseason baseline values (P < .05), suggesting increasing laxity or ‘softening’ of the UCL by midseason. We also demonstrated lower KJOC scores at midseason (P = .003), potentially indicative of a relationship between declining subjective functional assessment of the upper extremity and declining SWV. We also demonstrated a strong trend toward higher dominant arm SWV in preseason pitchers as compared to healthy volunteers, although not reaching statistical significance (P = .056). Further study in a larger sample would be needed to confirm these findings. Finally, we also demonstrated the feasibility of SWV of the UCL with a lower frequency transducer than that which we previously demonstrated and obtained similar repeatability.
The decline in SWV by midseason that we observed would suggest ‘softening’ and structural changes within the UCL. This decline was seen at our first (and only) point during the season (midseason) and while there seemed to be some recovery in SWV by postseason, SWV in the proximal segment remained significantly below baseline preseason values. We postulate this apparent recovery may be attributed to a few reasons: (1) time off for rest and recovery after the end of the season prior to scanning (this is supported by the concomitantly observed recovery of KJOC scores by the postseason examination) and/or (2) exclusion of subjects who sustained arm injury or who were otherwise not playing due to arm trouble. Therefore, future studies may benefit from more frequent sampling, particularly earlier in the season, to establish the full-time course of these changes while frequent postseason sampling may help to establish a time course for their reversal. SWV was higher (on average) in the distal segment than the proximal or midsubstance, and these results may provide a structural basis for the observation of Joyner et al that UCL ruptures occur most frequently at the proximal humeral attachment and of Conway et al that found more frequent tears in the midsubstance.11,19 While the minimum clinically important difference in SWV for the UCL is not currently known, we did demonstrate a statistically significant decline in KJOC score at midseason which accompanied a significant decline in SWV in proximal and midsubstance of the UCL. If confirmed in a larger study, this would further support the hypothesis that declining SWV is indicative of structural weakening of the UCL and would provide a clinical correlate for such.
Previously, we had reported a repeatability coefficient of 1.95 m/s for UCL SWV measurements in healthy volunteers using a different SWE system (Toshiba Aplio i800 ultrasound system; Toshiba, Tokyo, Japan) and with a higher frequency transducer (18 MHz i18LX5),17 very similar to the 1.98 m/s which was observed in the present study with a lower frequency transducer from a different vendor. With the higher frequency transducer, however, we noted a relatively high incidence (∼35%) of unreliable datasets, largely secondary to poor quality elastograms. In the present study using a lower frequency transducer, 80% of datasets were reliable. Although this hypothesis was not rigorously tested and other variables may certainly be involved, these data suggest that lower frequency transducers such as that used in this study may be better suited to SWE of the UCL. Indeed, it has been recognized that propagating shear waves at high frequencies is technically more demanding than at lower frequencies.27 This is due largely to the decreasing shear wave amplitude at higher frequencies. While high frequency probes are preferred for B-mode musculoskeletal imaging, our data suggest that lower frequency probes are beneficial for shear wave applications. Reliability aside, the mean SWV in the dominant arm UCL of healthy volunteers in this study of 4.35 ± 1.45 m/s does fall within the 95% CI of that in our prior study of 5.14 +/− 0.53 m/s as well.
The present study is not without limitations. Most notably, the small sample size of pitchers and subject dropout. We initially enrolled 17 pitchers, although all 17 were not available at all time points for reasons stated earlier, and 1 pitcher was unavailable at all time points, reducing the final sample to 16. However, despite this, we were able to demonstrate a statistically significant decline in SWV during the season. Another limitation of this study was that all pitchers were from the same athletic program. This would magnify the positive or negative effect of seasonal changes in throwing workout intensity, which may contribute to the overall health of the athlete’s elbow and manifest as variations in UCL SWV. Additionally, all scans were conducted by a single diagnostic radiologist. While this does ensure all SWE examinations were conducted with a consistent technique, reproducibility of these results by multiple examiners should be evaluated in future studies. Notably, interoperator reproducibility of musculoskeletal SWE has been demonstrated in other studies, for example, in the Achilles’ tendon.25 Finally, no pitchers in our cohort sustained a UCL injury. The goal of this particular study was to assess for occult changes in SWV in the UCL over the course of a season, but for this technique to ultimately have clinical utility, it will need to be studied in symptomatic pitchers who ultimately sustain UCL injury as well. Finally, the healthy volunteer participants, while still relatively young adults, were older in comparison to the collegiate pitching athletes. While it might be reasonable to hypothesize the potential for basal UCL stiffness to decrease with age (depending on individual physical activity), there is little information on how age may effect assessments using this relatively new technique. Future investigations will be required to determine the impact of age on SWV measures across large sample sizes of healthy adults to better establish comparative general population norms.
In summary, we have demonstrated a decline in SWV in the proximal and midsubstance of the UCL in collegiate pitchers’ dominant arm during the course of a season. While the degree of change in SWV tolerable by the UCL prior to rupture is not known, future studies should aim to address this question. To this end, future studies of SWE in the UCL should include a larger number of pitchers from multiple athletic organizations and should include athletes who ultimately sustain UCL injuries or otherwise require UCL reconstruction. Additionally, more frequent sampling in the early part of the season as well as during the immediate postseason timeframe may help to more fully elucidate the time-course of SWV decline and subsequent recovery. Theoretically, such data might one day establish a “safe zone” of UCL SWV variation over a competitive season and could help inform recommendations for pitch counts and return to play recommendations following surgical and/or nonsurgical treatment of UCL injury.
Conclusion
There is a significant decline in SWV in the proximal and midsubstance of the UCL in pitchers’ throwing arms during the course of the season, with associated subjective functional decline as well. Future studies with a larger sample size and more frequent sampling would be invaluable to further explore this observation and its clinical significance with respect to predicting and managing UCL injury risk.
Acknowledgments
The authors would like to acknowledge Rice University Athletics for significant contributions to athlete recruitment and participation.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interest: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Houston Methodist Research Institute approved this study, Approval: 2/7/2019, Pro00016330.
References
- 1.Alberta F.G., ElAttrache N.S., Bissell S., Mohr K., Browdy J., Yocum L., et al. The development and validation of a functional assessment tool for the upper extremity in the overhead athlete. Am J Sport Med. 2010;38:903–911. doi: 10.1177/0363546509355642. [DOI] [PubMed] [Google Scholar]
- 2.Andrews J.R., Wilk K.E., Satterwhite Y.E., Tedder J.L. Physical examination of the thrower's elbow. J Orthop Sport Phys Ther. 1993;17:296–304. doi: 10.2519/jospt.1993.17.6.296. [DOI] [PubMed] [Google Scholar]
- 3.Barr R.G., Ferraioli G., Palmeri M.L., Goodman Z.D., Garcia-Tsao G., Rubin J., et al. Elastography assessment of liver fibrosis: society of radiologists in ultrasound consensus conference statement. Radiology. 2015;276:845–861. doi: 10.1097/RUQ.0000000000000209. [DOI] [PubMed] [Google Scholar]
- 4.Bica D., Armen J., Kulas A.S., Youngs K., Womack Z. Reliability and precision of stress sonography of the ulnar collateral ligament. J Ultrasound Med. 2015;34:371–376. doi: 10.7863/ultra.34.3.371. [DOI] [PubMed] [Google Scholar]
- 5.Callaway G.H., Field L.D., Deng X.H., Torzilli P.A., O’Brien S.J., Altchek D.W., et al. Biomechanical evaluation of the medial collateral ligament of the elbow. J Bone Joint Surg. 1997;79:1223–1231. doi: 10.2106/00004623-199708000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Campbell R.E., McGhee A.N., Freedman K.B., Tjoumakaris F.P. Diagnostic imaging of ulnar collateral ligament injury: a systematic review. Am J Sports Med. 2020;48:2819–2827. doi: 10.1177/0363546520937302. [DOI] [PubMed] [Google Scholar]
- 7.Chapleau J., Sullivan T., Lambert B., Clyburn T.A., Incavo S.J. Postoperative alignment in revision total knee arthroplasty, a comparison between intra and extra-medullary tibial alignment. The Knee. 2021;28:319–325. doi: 10.1016/j.knee.2020.12.013. [DOI] [PubMed] [Google Scholar]
- 8.Ciccotti M.G., Atanda A., Nazarian L.N., Dodson C.C., Holmes L., Cohen S.B. Stress sonography of the ulnar collateral ligament of the elbow in professional baseball pitchers: a 10-year study. Am J Sports Med. 2014;42:544–551. doi: 10.1177/0363546513516592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conte S., Camp C.L., Dines J.S. Injury trends in major league baseball over 18 seasons: 1998-2015. Am J Orthop. 2016;45:116–123. no doi. [PubMed] [Google Scholar]
- 10.Conte S.A., Fleisig G.S., Dines J.S., Wilk K.E., Aune K.T., Patterson-Flynn N., et al. Prevalence of ulnar collateral ligament surgery in professional baseball players. Am J Sports Med. 2015;43:1764–1769. doi: 10.1177/0363546515580792. [DOI] [PubMed] [Google Scholar]
- 11.Conway J., Jobe F., Glousman R., Pink M. Medial instability of the elbow in throwing athletes. Treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg. 1992;74:67–83. [PubMed] [Google Scholar]
- 12.DeFroda S.F., Goodman A.D., Gil J.A., Owens B.D. Epidemiology of elbow ulnar collateral ligament injuries among baseball players: National Collegiate Athletic Association Injury Surveillance Program, 2009-2010 through 2013-2014. Am J Sports Med. 2018;46:2142–2147. doi: 10.1177/0363546518773314. [DOI] [PubMed] [Google Scholar]
- 13.Drakonaki E., Allen G., Wilson D. Ultrasound elastography for musculoskeletal applications. Br J Radiol. 2012;85:1435–1445. doi: 10.1259/bjr/93042867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fleisig G.S., Andrews J.R., Dillman C.J., Escamilla R.F. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23:233–239. doi: 10.1177/036354659502300218. [DOI] [PubMed] [Google Scholar]
- 15.Franz J.O., McCulloch P.C., Kneip C.J., Noble P.C., Lintner D.M. The utility of the KJOC score in professional baseball in the United States. Am J Sports Med. 2013;41:2167–2173. doi: 10.1177/0363546513495177. [DOI] [PubMed] [Google Scholar]
- 16.Garcia G.H., Gowd A.K., Cabarcas B.C., Liu J.N., Meyer J.R., White G.M., et al. Magnetic resonance imaging findings of the asymptomatic elbow predict injuries and surgery in major league baseball pitchers. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967118818413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gupta N., Labis J.S., Harris J., Trakhtenbroit M.A., Peterson L.E., Jack R.A., et al. Shear-wave elastography of the ulnar collateral ligament of the elbow in healthy volunteers: a pilot study. Skeletal Radiol. 2019;48:1241–1249. doi: 10.1007/s00256-019-3162-2. [DOI] [PubMed] [Google Scholar]
- 18.Gutierrez N.M., Granville C., Kaplan L., Baraga M., Jose J. Elbow MRI findings do not correlate with future placement on the disabled list in asymptomatic professional baseball pitchers. Sports Health. 2017;9:222–229. doi: 10.1177/1941738117701769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Joyner P.W., Bruce J., Hess R., Mates A., Mills F.B., Andrews J.R. Magnetic resonance imaging–based classification for ulnar collateral ligament injuries of the elbow. J Shoulder Elbow Surg. 2016;25:1710–1716. doi: 10.1016/j.jse.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 20.Labott J.R., Aibinder W.R., Dines J.S., Camp C.L. Understanding the medial ulnar collateral ligament of the elbow: review of native ligament anatomy and function. World J Orthop. 2018;9:78. doi: 10.5312/wjo.v9.i6.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.LiMarzi G.M., O’Dell M.C., Scherer K., Pettis C., Wasyliw C.W., Bancroft L.W. Magnetic resonance arthrography of the wrist and elbow. Magn Reson Imaging Clin. 2015;23:441–455. doi: 10.1016/j.mric.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 22.Lin C.-Y., Sadeghi S., Bader D.A., Cortes D.H. Ultrasound shear wave elastography of the elbow ulnar collateral ligament: reliability test and a preliminary case study in a baseball pitcher. J Eng Sci Med Diag Ther. 2018;1 doi: 10.1115/1.4038259. [DOI] [Google Scholar]
- 23.Magee T. Accuracy of 3-T MR arthrography versus conventional 3-T MRI of elbow tendons and ligaments compared with surgery. Am J Roentgenol. 2015;204:W70–W75. doi: 10.2214/AJR.14.12553. [DOI] [PubMed] [Google Scholar]
- 24.Nightingale K., Soo M.S., Nightingale R., Trahey G. Acoustic radiation force impulse imaging: in vivo demonstration of clinical feasibility. Ultrasound Med Biol. 2002;28:227–235. doi: 10.1016/s0301-5629(01)00499-9. [DOI] [PubMed] [Google Scholar]
- 25.Payne C., Watt P., Cercignani M., Webborn N. Reproducibility of shear wave elastography measuresof the Achilles tendon. Skeletal Radiol. 2018;47:779–784. doi: 10.1007/s00256-017-2846-8. [DOI] [PubMed] [Google Scholar]
- 26.Prado-Costa R., Rebelo J., Monteiro-Barroso J., Preto A.S. Ultrasound elastography: compression elastography and shear-wave elastography in the assessment of tendon injury. Insights Into Imaging. 2018;9:791–814. doi: 10.1007/s13244-018-0642-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sadeghi S.R.S., Akbarian D., Daniel H. Effect of frequency and focal depth of push pulses on acoustic intensity, mechanical index, and shear wave amplitude for elastography imaging. M J Biomed Eng. 2017;3:779–784. [Google Scholar]
- 28.Safran M., Ahmad C.S., Elattrache N.S. Ulnar collateral ligament of the elbow. Arthroscopy. 2005;21:1381–1395. doi: 10.1016/j.arthro.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 29.Sawilowsky S.S. New effect size rules of thumb. J Mod Appl Stat Method. 2009;8:26. doi: 10.22237/jmasm/1257035100. [DOI] [Google Scholar]
- 30.Shanley E., Smith M., Mayer B.K., Bailey L.B., Thigpen C.A., Tokish J.M., et al. Using stress ultrasonography to understand the risk of UCL injury among professional baseball pitchers based on ligament morphology and dynamic abnormalities. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118788847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taljanovic M.S., Gimber L.H., Becker G.W., Latt L.D., Klauser A.S., Melville D.M., et al. Shear-wave elastography: basic physics and musculoskeletal applications. Radiographics. 2017;37:855–870. doi: 10.1148/rg.2017160116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Werner S.L., Fleisig G.S., Dillman C.J., Andrews J.R. Biomechanics of the elbow during baseball pitching. J Orthop Sports Phys Ther. 1993;17:274–278. doi: 10.2519/jospt.1993.17.6.274. [DOI] [PubMed] [Google Scholar]
- 33.Werner S.L., Murray T.A., Hawkins R.J., Gill T.J. Relationship between throwing mechanics and elbow valgus in professional baseball pitchers. J Shoulder Elbow Surg. 2002;11:151–155. doi: 10.1067/mse.2002.121481. [DOI] [PubMed] [Google Scholar]