Abstract
Background
The aim of this study was to compare the clinical outcomes and retear rate of arthroscopic superior capsular reconstruction (SCR) with dermal allograft following structural failure of a previous rotator cuff repair, with a cohort of primary SCRs.
Methods
This was a retrospective comparative study with a study group comprising 22 patients who were followed up at a minimum of 24 (mean, 41; range, 27-65) months after SCR with dermal allograft performed for structural failure of a previous rotator cuff repair. The control group included 13 patients who previously underwent a primary SCR using dermal allograft and were followed up for 24 months. Clinical outcome measures comprised range of motion, the American Shoulder and Elbow Surgeons score, and the Western Ontario Rotator Cuff (WORC) Index. Radiological outcomes included the acromiohumeral interval and graft integrity on magnetic resonance imaging at one year. Logistic regression was used to determine whether SCR being undertaken as either a primary or revision procedure influenced functional outcomes or retear rate.
Results
The mean age at the time of surgery was 58 (range, 39-74) years for the study group and 60 (range, 48-70) years for the control group. Forward flexion improved from a mean of 117° (range, 7°-180°) preoperatively to 140° (range, 45°-170°) postoperatively (P = .11), and external rotation increased from a mean of 31° (range, 0°-70°) preoperatively to 36° (range, 0°-60°) postoperatively (P = .23). The American Shoulder and Elbow Surgeons score improved (P = 0) from a mean of 38 (range, 12-68) to 73 (range, 17-95), and the WORC Index improved (P = 0) from a mean of 29 (range, 7-58) to 59 (range, 30-97). Following SCR, there was no significant change in the acromiohumeral interval. The graft was intact in 42% of cases on magnetic resonance imaging and none of the retears underwent further surgery. Compared to revision SCR, primary SCR resulted in a significant improvement in forward flexion (P = .001), external rotation (P = 0), and WORC Index (P = .019). Logistic regression demonstrated that SCR performed as a revision procedure was associated with a higher retear rate (P = .006) and worse forward flexion (P = .009) and external rotation (P = .008).
Conclusion
SCR using human dermal allograft following structural failure of a previous rotator cuff repair can lead to an improvement in clinical outcomes but the results are inferior to primary procedures.
Keywords: Allograft, Revision surgery, Rotator cuff repair, Rotator cuff retear, Rotator cuff tear, Superior capsular reconstruction
Massive rotator cuff tears are defined as those that involve at least two tendons or measure ≥5 cm in the anteroposterior dimension.7,13 Treatment options for young, active patients are limited, particularly in massive, irreparable tears and include subacromial decompression with or without tear débridement, partial repair, the use of grafts, muscle or tendon transfer, and a subacromial balloon spacer.2,5,8,26,35 In this population, reverse total shoulder arthroplasty (RTSA) is not the preferred option due to concerns over complications such as loosening and the need for revision.9
Direct tendon-bone repair in massive tears can be achieved but is associated with a failure rate of 40%-94%.4,12,25,46 Although some retears may be asymptomatic, there is a risk of tear progression and deterioration in muscle quality resulting in the onset of debilitating symptoms and cuff tear arthropathy.21,34 Results of surgery can be favorable and characterized by an improvement in range of motion and functional outcome; however, the complication and reoperation rates are 12% and 5%, respectively.3
Hanada et al16 and Mihata et al33 conceptualized a unique surgical strategy for the treatment of massive, irreparable cuff tears focusing on restoring superior stability to the humeral head. In doing so, there would be a reduction in subacromial contact pressure, centering of the humeral head, and restoration of the glenohumeral fulcrum of motion. Superior capsular reconstruction (SCR) was borne from this and initially popularized using a fascia lata autograft.31 After a minimum follow-up of two years, there was a significant improvement in active elevation, external rotation, and functional outcome as measured by the American Shoulder and Elbow Surgeons (ASES) score. Intact tendons were present in 83.3% of the cohort and there was no progression to arthritis. Out of the 24 cases studied, though, only four were performed as a revision operation. Subsequent reports of SCR have similarly focused on the outcomes in primary cases, with very few studies examining its effectiveness in the revision setting.1,10,11,15,36
Structural failure of a rotator cuff repair poses several technical challenges due to a combination of tissue loss, poor tendon quality, and limited tendon mobility. SCR in this setting is an appealing option because it preserves the joint and provides a superior restraint to the humeral head.31 The purpose of this study was to compare the clinical outcomes and retear rate of arthroscopic SCR with dermal allograft following structural failure of a previous rotator cuff repair, with a historical control of primary SCRs.36 We hypothesized that clinical and radiological outcomes following primary SCR would be superior to those in the revision group.
Materials and methods
A retrospective review of consecutive patients who underwent arthroscopic SCR for the revision of massive rotator cuff retears using 3 mm-thick human dermal allograft (ArthroFLEX; Arthrex, Naples, FL, USA) was performed. SCR was chosen for revision in favor of other procedures because it has been shown to improve clinical outcomes in this setting.39 Institutional review board approval was obtained before the commencement of the study. Inclusion criteria were patients who had failed nonoperative treatment (physiotherapy and analgesia) and had persistent pain and limited function following a previous rotator cuff repair and subsequent failure of healing or a retear (as determined by ultrasonography or magnetic resonance imaging [MRI]).
All patients had massive irreparable posterosuperior rotator cuff tears (Type V on the criteria outlined by Sugaya et al44), poor residual tendon quality (preventing the use of an interpositional bridging graft), and no or minimal (grade 1 Samilson and Prieto characterized by an inferior humeral head or glenoid osteophyte measuring less than 3 mm in height) glenohumeral arthritis.41 While all patients in the study had massive irreparable posterosuperior rotator cuff tears, some patients additionally had subscapularis tears since these were not excluded from either group. Massive cuff tears were defined as those measuring ≥5 cm in the anteroposterior dimension and/or involving at least two tendons.7,13 Follow-up was for a minimum of two years. Exclusion criteria comprised the presence of arthritis on plain radiographs greater than grade 1 on the Samilson and Prieto classification and workers’ compensation patients, since this subset of the population are unable to participate in research. Medical records and operative reports were analyzed by an orthopedic surgeon who was not involved in the surgical procedures. We compared this study cohort to a group of patients (n = 13) who previously participated in a randomized controlled trial evaluating the outcome of SCR as a primary procedure for an irreparable rotator cuff tear.36 Postoperative rehabilitation protocols were identical between groups.
Participants
From September 2014 to July 2019, 22 patients were eligible for the study group. The cohort consisted of 18 males and four females with a mean age of 58 (range, 39-74) years at the time of surgery. There were two smokers and no diabetics. Surgery was performed on the dominant arm in 14 cases. All patients had one previous rotator cuff repair that went onto structural failure before undergoing SCR. The interval between primary rotator cuff repair and revision surgery was 80 (range, 12-216) months. The mean duration of symptoms prior to revision surgery was 21 (range, 6-84) months.
The historical primary SCR group consisted of 11 males and two females with a mean age of 60 (range, 48-70) years at the time of surgery. Surgery was performed on the dominant arm in eight cases. The mean duration of symptoms prior to surgery was 28 (6-45) months.
Outcome measures
Clinical evaluation involved the subjective assessment of range of motion (forward flexion and external rotation) with the patient standing in the anatomic position with the arm at the side and the palm forward. Patient-reported outcome measures included the ASES score and the Western Ontario Rotator Cuff (WORC) Index.23,28 The WORC Index relies on patient self-reporting and consists of 21 questions grouped into five categories: physical symptoms, sports/recreation, work, lifestyle, and emotions. Each question uses a visual analog scale to provide a final rating from 0% (lowest functional status) to 100% (the highest functional status). All outcome scores were collected and managed using REDCap (Research Electronic Data Capture) electronic data capture tools hosted at the University of Calgary.17,18 This is a secure, web-based software platform designed to support data collection for research studies without the involvement of the treatment surgeon. Radiological evaluation was carried out by a fellowship-trained orthopedic surgeon and entailed determining the preoperative Hamada grading, the acromiohumeral distance on plain radiographs at least one year postoperatively, and graft integrity on MRI at 12 months.14
Surgical technique
All operations were performed by the senior author (I.K.L.). Preoperative assessment specifically focused on determining the details of previous surgeries with a particular emphasis on tear size, tear retraction, tendon quality, tendon mobility, tendons involved, associated pathology, concomitant procedures (eg, biceps tenotomy/tenodesis and distal clavicle excision), and whether a single or double row construct was utilized. Under general anesthesia, the patient was positioned in the lateral decubitus position. The arm was held in place with the SPIDER Arm positioner (TENET Medical Products; Smith & Nephew, Andover, MA, USA) to optimize graft tension with the arm in 30° glenohumeral abduction.32
A diagnostic arthroscopy was performed with a pump maintaining pressure at 30 mm Hg. In cases where the long head of the biceps tendon was grossly tendinopathic or unstable, a tenotomy or a tenodesis was done dependent upon patient age and activity level. For the latter, a tenodesis screw (7 mm Bio-tenodesis screw; Arthrex, Naples, FL, USA) was inserted at the bottom of the biceps groove to dock the tendon within the bone. Upper and full-thickness subscapularis tears were repaired in all cases. Acromioplasty was not routinely performed and nor was resection of the coracoacromial ligament, so as to prevent anterosuperior escape of the humeral head.19 Sutures and suture anchors from the previous procedure were removed. After débriding the posterosuperior rotator cuff tissue, all tears were extensively mobilized and a partial repair was carried out if possible. SCR was performed in cases where the tendon could not be mobilized to the footprint and was of such poor quality that it would not accept sutures for a bridging graft. In cases where a partial repair was performed, SCR was carried out to fill the remaining defect.
Tissue was cleared from the superior glenoid and two or three 3 mm BioComposite SutureTak anchors (Arthrex, Naples, FL, USA) were inserted taking care not to penetrate the cartilage (Fig. 1). For the humerus, two 4.75 mm double-loaded suture anchors (Healicoil Regenesorb; Smith and Nephew, Andover, MA, USA) were placed anteriorly and posteriorly along the medial margin of the humeral footprint adjacent to the articular margin (Fig. 2). Multiple simple sutures using #2 FiberWire (Arthrex, Naples, FL, USA) were then placed into the anterior and posterior portions of the rotator cuff in order to facilitate side-to-side closure of the graft to the anterior and posterior margins of the rotator cuff, respectively. A dedicated measuring device (SCR guide; Arthrex, Naples, FL, USA) was used to measure the distance between anchors, and an appropriately sized graft was cut with a 1-cm overlap laterally to facilitate a double-row repair on the humerus. The graft was folded to double its thickness before it was prepared.
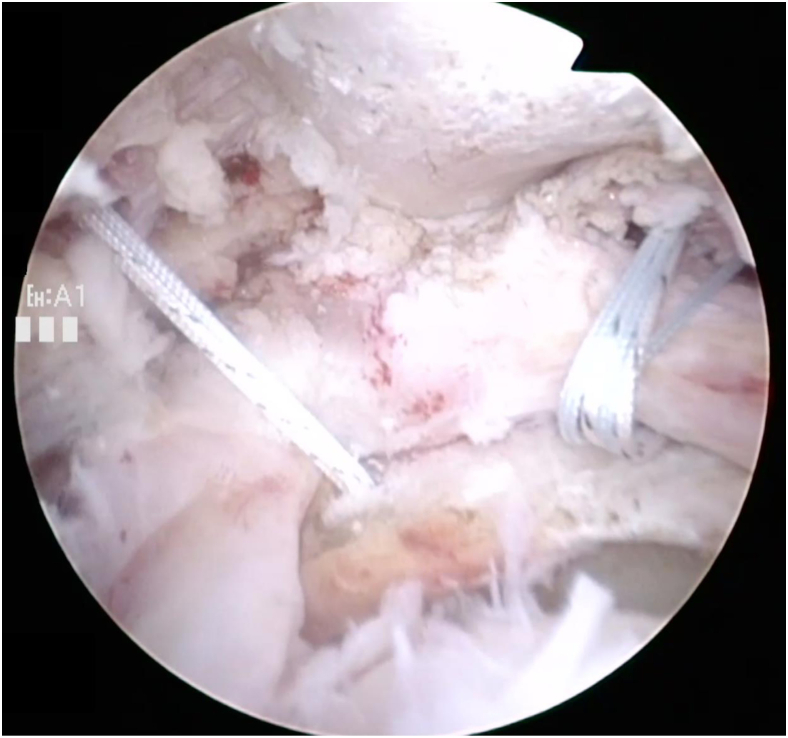
Figure 1.
Right shoulder arthroscopy viewing from the mid-lateral portal. Two suture anchors positioned anteriorly and posteriorly in the superior glenoid.
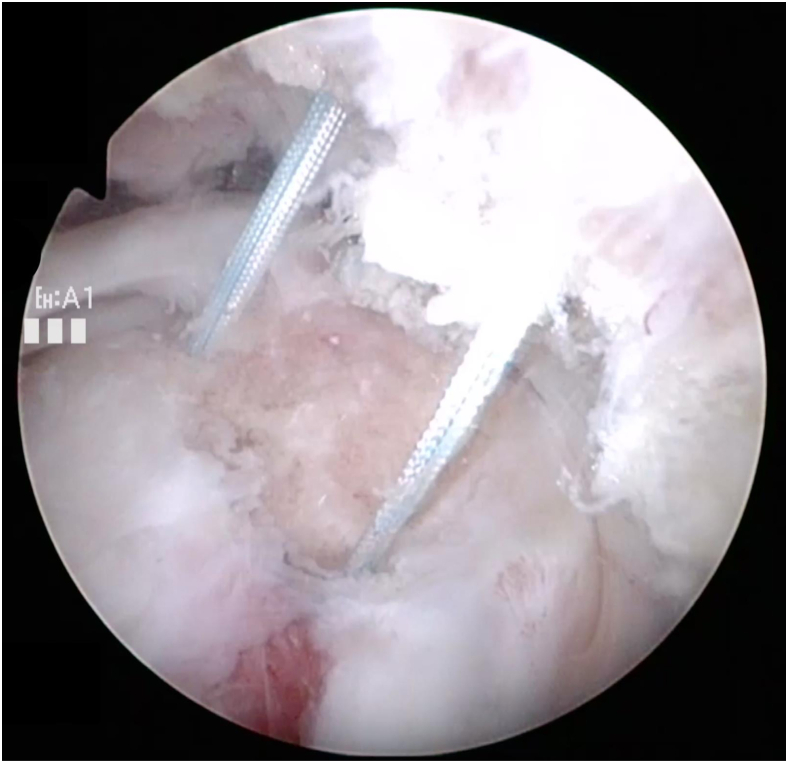
Figure 2.
Right shoulder arthroscopy viewing from the posterior portal. Two suture anchors positioned anteriorly and posteriorly on the medial aspect of the footprint.
A 10 ml syringe was inserted through a mid-lateral portal and sutures from the medial and lateral anchors were passed through the graft extracorporeally. A 70° degree arthroscope helped ensure that none of the suture limbs crossed over before arranging them around the syringe using a previously described technique (Fig. 3).40 The graft was then shuttled through the syringe to cover the residual rotator cuff defect and positioned deep into the remaining medial cuff tissue. The medial sutures were tied first, followed by the lateral ones. The side-to-side sutures were subsequently passed through the anterior and posterior portions of the graft and tied. The procedure was completed by securing the lateral aspect of the graft with two 4.75 mm lateral row anchors (Biocomposite SwiveLock; Arthrex, Naples, FL, USA) to create a double row construct with good tendon-bone compression (Fig. 4).
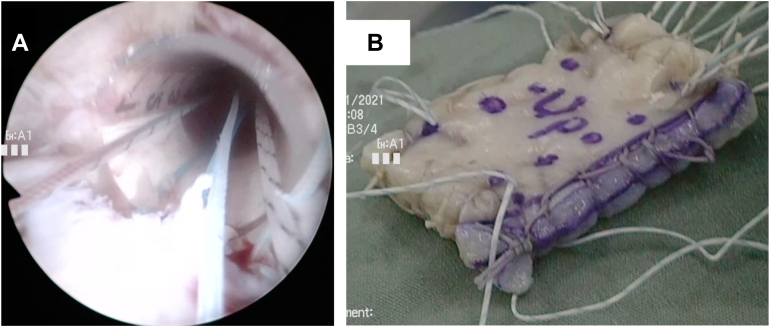
Figure 3.
Right shoulder arthroscopy viewing from the posterior portal using a 70° arthroscope to ensure that none of the suture limbs crossed as they entered the 10 ml syringe (A), before they were passed through the graft (B).
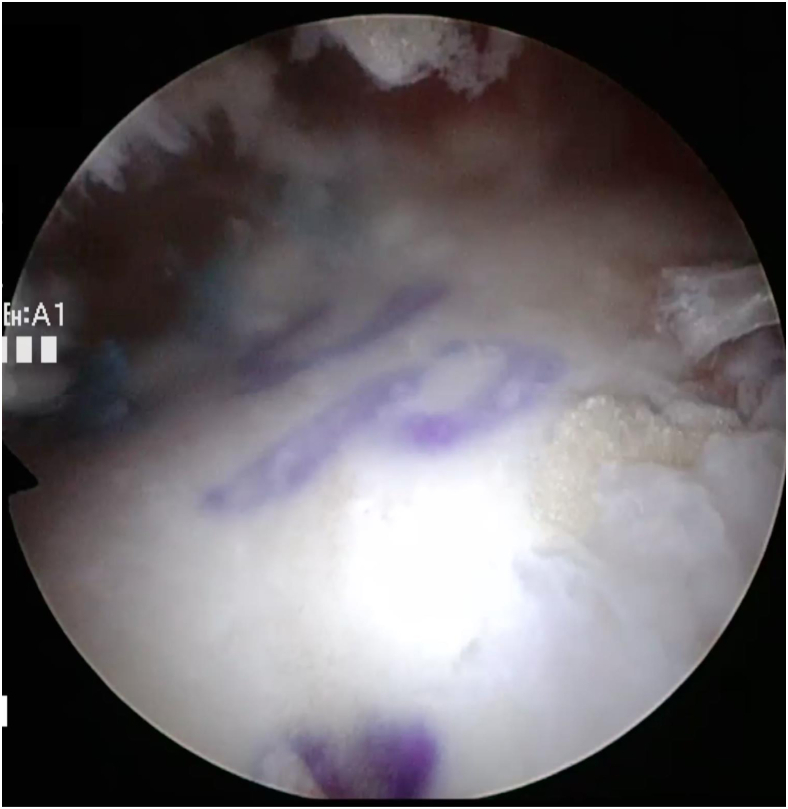
Figure 4.
Right shoulder arthroscopy viewing from the posterior portal to illustrate that the graft has completely covered the defect.
Postoperative rehabilitation
During the first six weeks, hand, wrist, and elbow range of motion were allowed. Passive external rotation was allowed with the arm at the side with no overhead motion. Sling use was discontinued after six weeks following which active range of motion was commenced. Beginning in the seventh postoperative week and progressing through the 12th postoperative week, patients performed passive overhead stretches. Strengthening was delayed until 16 weeks postoperatively. Full return to activity was not allowed until one year postoperatively. Return to work was based on the specific demands of each patient.
Statistical analysis
Data were summarized with routine descriptive statistics. Unpaired t tests were used to evaluate differences between primary and revision SCR groups and between intact and ruptured graft groups. Paired t tests were used to determine changes between preoperative and postoperative range of motion, ASES score, WORC Index, and acromiohumeral interval. A P value < .05 was considered to be statistically significant. We used logistic regression to determine whether SCR being undertaken as either a primary or revision procedure influenced patient-reported outcomes (ASES scores and WORC Index) or retear rate. The SPSS software package, version 22 (SPSS; IBM Corp., Armonk, NY, USA) was used to analyze data.
Results
The mean duration of follow-up in the revision SCR group was 41 (range, 27-65) months. Associated procedures performed at the time of revision included one upper subscapularis repair, six partial posterior rotator cuff repairs, six capsular releases, seven biceps tenodeses, and one biceps tenotomy. A further five full-thickness subscapularis tears were irreparable due to poor tissue quality, limited mobility, and retraction medial to the glenoid. Only one of these though was eventually associated with graft failure on MRI. No perioperative complications were noted and no further surgery was carried out. There were no cases of any inflammatory reactions, infections, or tissue rejection. The mean graft size was 2.4 (range, 1.5-3.5) cm medially, 2.3 (range, 1.5-3.5) cm laterally, 3.1 (range, 2.5-5) cm anteriorly, and 2.7 (range, 1.8-3.9) cm posteriorly.
All patients in the primary SCR group were followed up for two years. In this cohort, there were three subscapularis tears of which two were repairable. The mean graft size was 2.5 (range, 1.5-3.5) cm medially, 2.2 (range, 1.2-3.6) cm laterally, 2.9 (range, 2.2-3.5) cm anteriorly, and 2.8 (range, 1.8-3.5) cm posteriorly.
Range of motion
In the study group, forward flexion improved from a mean of 117° (range, 7°-180°) preoperatively to 140° (range, 45°-170°) postoperatively (P = .11), and external rotation increased from a mean of 31° (range, 0°-70°) preoperatively to 36° (range, 0°-60°) postoperatively (P = .23). In the primary SCR (control) group, forward flexion improved from a mean of 134° (range, 20°-160°) preoperatively to 172° (range, 150°-180°) postoperatively (P = .05), and external rotation increased from a mean of 45° (range, 25°-70°) preoperatively to 63° (range, 25°-90°) postoperatively (P = .35).
Functional outcome
Functional outcome scores were available for 17 patients in the study group. In these, the ASES score improved (P = 0) from a mean of 38 (range, 12-68) to 73 (range, 17-95), and the WORC Index improved (P = 0) from a mean of 29 (range, 7-58) to 59 (range, 30-97). Functional outcome scores were available for all patients in the primary SCR (control) group. The ASES score improved (P = .04) from a mean of 62 (range, 23-87) to 85 (range, 46-99), and the WORC Index improved (P = .01) from a mean of 46 (range, 19-93) to 78 (range, 62-97).
Radiological assessment
In the study group, preoperative radiographs demonstrated that 11 patients were Hamada grade 1, 6 were Hamada grade 2, and 5 were Hamada grade 3. Following SCR, there was no significant change (P = 1) in the acromiohumeral interval, which was a mean of 6 (range, 1-12) mm preoperatively and 6 (range, 2-12) mm postoperatively. The graft was intact in 42% (8 of 18) of patients on MRI. Out of 10 retears, no patients underwent further surgery.
In the primary SCR (control) group, preoperative radiographs demonstrated that 6 patients were Hamada grade 1, 6 were Hamada grade 2, and 1 was Hamada grade 3. Complete postoperative Hamada gradings were not recorded as not all patients had postoperative radiographs. The graft was intact in 91% (10 out of 11 patients who underwent MRI) of patients on MRI. The patient who had a retear did not have any further surgery (Table I). Following adjustment for age, subscapularis integrity, and infraspinatus integrity, the logistic regression model demonstrated that compared to primary surgery, SCR performed as a revision procedure was associated with a higher retear rate (P = .006) and worse forward flexion (P = .009) and external rotation (P = .008). However, it did not affect the ASES (P = .19) or WORC (P = .11) scores at 24 months.
Table I.
Comparison of clinical outcomes between primary (control group) and revision (study group) superior capsular reconstruction.
| Outcome measure | Study (revision superior capsular reconstruction) group |
Control (primary superior capsular reconstruction) group |
Comparison between study (revision cases) and control (primary cases) groups |
||||
|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | P value | Preoperative | Postoperative | P value | P value | |
| Forward flexion (°) | 117 (range, 7-180) | 140 (range, 45-170) | .11 | 134 (range, 20-160) | 172 (range, 150-180) | .05 | .001 |
| External rotation (°) | 31 (range, 0-70) | 36 (range, 0-60) | .23 | 45 (range, 25-70) | 63 (range, 25-90) | .35 | 0 |
| ASES score | 38 (range, 12-68) | 73 (range, 17-95) | 0 | 62 (range, 23-87) | 85 (range, 46-99) | .04 | .07 |
| WORC Index | 29 (range, 7-58) | 59 (range, 30-97) | 0 | 46 (range, 19-93) | 78 (range, 62-97) | .01 | .019 |
| Percentage of grafts that were intact on MRI postoperatively | 42 | 91 | |||||
ASES, American Shoulder and Elbow Surgeons; WORC, Western Ontario Rotator Cuff; MRI, magnetic resonance imaging.
Outcomes in intact and ruptured grafts in patients with superior capsular reconstruction in a revision setting
In the group with intact grafts (8 patients), forward flexion improved from a mean of 133° (range, 85°-150°) preoperatively to 142° (range, 120°-150°) postoperatively (P = .09), and external rotation increased from a mean of 33° (range, 0°-30°) preoperatively to 41° (range, 20°-60°) postoperatively (P = .07). The ASES score improved (P = .006) from a mean of 38 (range, 23-64) to 71 (range, 52-85), and the WORC Index improved (P = .024) from a mean of 26 (range, 15-40) to 57 (range, 30-73).
In the retear group (10 patients), forward flexion improved from a mean of 106° (range, 30°-150°) preoperatively to 137° (range, 45°-170°) postoperatively (P = .28), and external rotation increased from a mean of 30° (range, 0°-60°) preoperatively to 31° (range, 0°-60°) postoperatively (P = .86). The ASES score improved (P = .07) from a mean of 40 (range, 12-68) to 69 (range, 17-95), and the WORC Index improved (P = .006) from a mean of 28 (range, 7-58) to 59 (range, 16-97).
No significant differences were found in clinical outcomes when intact and ruptured grafts were compared (Table II).
Table II.
Comparison of clinical outcomes between intact and ruptured grafts.
| Outcome measure | Intact grafts in patients with superior capsular reconstruction in the revision setting |
Ruptured grafts in patients with superior capsular reconstruction in the revision setting |
Comparison between intact and ruptured grafts |
||||
|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | P value | Preoperative | Postoperative | P value | P value | |
| Forward flexion (°) | 133 (range, 85-150) | 142 (range, 120-150) | .09 | 106 (range, 30-150) | 137 (range, 45-170) | .28 | .70 |
| External rotation (°) | 33 (range, 0-30) | 41 (range, 20-60) | .07 | 30 (range, 0-60) | 31 (range, 0-60) | .86 | .15 |
| ASES score | 38 (range, 23-64) | 71 (range, 52-85) | .006 | 40 (range, 12-68) | 69 (range, 17-95) | .07 | .69 |
| WORC Index | 26 (range, 15-40) | 57 (range, 30-73) | .024 | 28 (range, 7-58) | to 59 (range, 16-97) | .006 | .92 |
ASES, American Shoulder and Elbow Surgeons; WORC, Western Ontario Rotator Cuff.
Outcomes in primary superior capsular reconstruction and revision superior capsular reconstruction groups
Compared to revision SCR, primary SCR was associated with a significantly higher rate of graft integrity (P = .015) and resulted in a significant improvement in forward flexion (P = .001), external rotation (P = 0), and the WORC Index (P = .019). No significant difference was observed in the ASES score (P = .07) between the two groups.
Discussion
This is one of the few studies to exclusively report the clinical outcomes and retear rates following arthroscopic SCR using human dermal allograft for the revision of massive rotator cuff retears.15,38,39 At a mean follow-up of 41 months, there was a significant improvement in functional outcome, a nonsignificant gain in range of motion, and no change in the acromiohumeral interval. The retear rate of 58% is higher than what has previously been reported in the literature, but no further surgery was required during the study period and the outcomes were no different to those with intact grafts.10,38 We postulate that the retear rate observed in this study was potentially attributable to the sole inclusion of massive rotator cuff retears, and due to the surgical cases being complex revision procedures as indicated in the regression analysis.12,15,43 When comparing this cohort of revision procedures to a group of primary SCRs (ie, patients who had not previously undergone a rotator cuff repair) used as a control, the primary group exhibited a significantly greater range of motion (forward flexion and external rotation), functional outcome score (WORC Index), and rate of graft integrity. Although the follow-up time period was different between the two groups, midterm results of SCR have demonstrated relative stability of functional outcomes.30
Revision rotator cuff repair leads to worse clinical outcomes than primary repair due to reduced circulation within the degenerative tendon, and dense fibrous tissue resulting in less neovascularization and limited tendon healing.6,43 Denard et al6 reported the outcomes after primary and revision rotator cuff repair of massive rotator cuff tears associated with pseudoparalysis. Primary operations were associated with greater gains in the ASES score and were more likely to reverse pseudoparalysis (90% vs. 43%). Similarly, Meshram et al27 reviewed their results of primary vs. revision repair of large and massive posterosuperior rotator cuff tears. In their study, patients undergoing revision RCR had poorer outcomes for pain, satisfaction, and ASES score when compared to primary RCR. In addition, the retear rate was 50% in patients undergoing revision rotator cuff repair.
The results of this study are consistent with the previous literature demonstrating that compared to primary surgery, revision SCR is significantly associated with a higher graft retear rate and worse range of motion. Functional outcomes though, do not appear to be influenced by revision status in the short term. Hammad et al15 analyzed registry data of 350 patients who underwent SCR to identify factors leading to a successful outcome. Approximately 11% of cases were revisions. Although a significant improvement in patient-reported outcomes measures was noted at two-year follow-up, worse results were demonstrated in those undergoing revision of a previously failed rotator cuff repair. Woodmass et al45 followed up 34 patients for an average of 12 months after SCR. Failure occurred in 80% (16/20) of revision cases and 43% of primary ones. Further surgery was required in eight patients and factors contributing to a poor outcome and reoperation included prior procedures, female gender, and low surgeon volume. The average time between SCR and further surgery was 10.2 months and the majority of failures (5 out of 8) were treated with RTSA. Polacek and Nyegaard39 reviewed 24 patients with massive irreparable rotator cuff tears treated with arthroscopic SCR using a 3-layered fascia lata autograft. Prior rotator cuff repair was performed in 11 cases. Although an improvement was demonstrated in functional outcome and range of motion one year after surgery, postoperative complications were noted in four patients, all of whom had undergone previous rotator cuff repair. Graft failure occurred in two cases and RTSA was performed for one patient.
Choice of graft may also influence the outcome of SCR because graft elongation, suture cutout, and persistent proximal migration of the humeral head may be less with thicker biomaterials (eg, 6-8 mm thick autologous fascia lata graft).29,31,42 Previous biomechanical studies have demonstrated that an 8 mm fascia lata autograft leads to an improvement in both subacromial contact pressure and superior stability when compared to a 4 mm fascia lata autograft.32 While donor site morbidity and increased surgical time are potential drawbacks of using an autograft, the overall failure and reoperation rates are still lower than for allografts.39 Based on this, it may be advantageous to specifically use the thicker fascia lata autograft for revision cases since it is more effective at resisting proximal humeral migration than thinner grafts, and owing to the fact that inferior clinical and radiographic outcomes have been associated with prior surgery preceding SCR.15,45 Biological enhancement of SCR has recently been reported with the use of a polypropylene mesh to augment the function of fascial lata autograft.1 In the short term, this has been demonstrated to improve both healing and remodeling of the graft although it remains to be seen whether this can be maintained in the long term and lead to a sustainable improvement in function.1 Nonetheless, in this study, no further surgery was required and the results did not differ between intact and ruptured grafts. This suggests that the integrity of the graft may not necessarily be the most important factor determining the results of SCR and that it may simply represent a temporary spacer that decreases pain so that rehabilitation can continue uninterrupted.10
In an effort to reduce the donor site morbidity associated with harvesting an autograft, allografts have gained in popularity.39 These though have higher failure and reoperation rates when compared to the fascia lata autograft used by those who conceived the procedure.22,31 The management of irreparable rotator cuff tears remains challenging. SCR works by providing a superior static restraint to proximal migration of the humeral head and thus optimizing the rotator cuff force couples and improving joint kinematics.20,31 When undertaken after previous surgery, the results of SCR are less reliable and characterized by worse clinical outcomes and high failure rates. Reasons for this include the presence of existing implants in the bone that may preclude optimal suture anchor insertion, tendon degeneration (as this may inhibit tendon-bone healing), poor bone quality, and the difficulty in discerning between the true tear margin and fibrous tissue overlying the retracted tendon. These factors pose several distinct challenges to an operation ie, already technically demanding. Patient selection is therefore crucial and should be based upon prognostic factors suggestive of potential failure. In this regard, Kwon et al24 developed a 15-point scoring system to predict rotator cuff healing comprising tear retraction, fatty infiltration of infraspinatus, and anteroposterior tear size. Although this was established for primary repairs, a tool similar to this would help stratify patients according to their risk of graft rupture and identify those most likely to achieve a favorable outcome.
Limitations to this study comprise the retrospective design, incomplete follow-up data, and short-term follow-up. The small sample size reflects the paucity of rotator cuff repair failures that are suitable for SCR and prevents detailed subgroup analysis, particularly regarding the influence of subscapularis tears. Subscapularis tears and infraspinatus dysfunction (reduced power and a positive lag sign) are often considered as a contraindication to SCR, and so their inclusion in this study limits a comparison to the existing literature on the subject.37 All procedures were undertaken by a single surgeon with a high-volume tertiary referral practice dedicated to complex rotator cuff tears and so this limits the external generalizability of our results.
Conclusion
This is one of the few studies to exclusively report the outcomes of SCR using human dermal allograft for the treatment of structural failure following a previous rotator cuff repair. Our findings indicate that SCR can lead to an improvement in functional outcome and range of motion. Compared to primary cases, though, revision surgery leads to a significantly higher graft retear rate and worse range of motion. Before SCR is routinely recommended for revision rotator cuff surgery, further studies are needed to evaluate its performance in the long term and determine whether the type (autograft vs. allograft) and thickness of the graft influence the outcome.
Acknowledgments
The authors would like to acknowledge Kristie More and Deanne Meredyk for setting up the database used to analyze the data.
Disclaimers
Funding: No funding was disclosed by the authors.
Conflicts of interests: The authors, their immediate families, and any research foundation with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
This study was approved by the University of Calgary Conjoint Health Research Ethics Board: IRB approval number REB15-1485_REN5.
References
- 1.Ben H., Kholinne E., Zeng C.H., So S.P., Lee J.B., Sun Y., et al. Early postoperative MRI evaluation of a fascia lata autograft with and without polypropylene mesh Augmentation after superior capsular reconstruction. Am J Sports Med. 2023;51:912–918. doi: 10.1177/03635465231151927. [DOI] [PubMed] [Google Scholar]
- 2.Boileau P., Gonzalez J.F., Chuinard C., Bicknell R., Walch G. Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elbow Surg. 2009;18:600–606. doi: 10.1016/j.jse.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 3.Brochin R.L., Zastrow R., Hussey-Andersen L., Parsons B.O., Cagle P.J. Revision rotator cuff repair: a systematic review. J Shoulder Elbow Surg. 2020;29:624–633. doi: 10.1016/j.jse.2019.06.023. [DOI] [PubMed] [Google Scholar]
- 4.Burkhart S.S., Danaceau S.M., Pearce C.E., Jr. Arthroscopic rotator cuff repair: analysis of results by tear size and by repair technique-margin convergence versus direct tendon-to-bone repair. Arthroscopy. 2001;17:905–912. doi: 10.1053/jars.2001.26821. [DOI] [PubMed] [Google Scholar]
- 5.Clark N.J., Elhassan B.T. The role of tendon transfers for irreparable rotator cuff tears. Curr Rev Musculoskelet Med. 2018;11:141–149. doi: 10.1007/s12178-018-9468-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Denard P.J., Lädermann A., Jiwani A.Z., Burkhart S.S. Functional outcome after arthroscopic repair of massive rotator cuff tears in individuals with pseudoparalysis. Arthroscopy. 2012;28:1214–1219. doi: 10.1016/j.arthro.2012.02.026. [DOI] [PubMed] [Google Scholar]
- 7.DeOrio J.K., Cofield R.H. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J bone Joint Surg Am. 1984;66:563–567. [PubMed] [Google Scholar]
- 8.Deranlot J., Herisson O., Nourissat G., Zbili D., Werthel J.D., Vigan M., et al. Arthroscopic subacromial spacer implantation in patients with massive irreparable rotator cuff tears: clinical and radiographic results of 39 retrospectives cases. Arthroscopy. 2017;33:1639–1644. doi: 10.1016/j.arthro.2017.03.029. [DOI] [PubMed] [Google Scholar]
- 9.Ek E.T., Neukom L., Catanzaro S., Gerber C. Reverse total shoulder arthroplasty for massive irreparable rotator cuff tears in patients younger than 65 years old: results after five to fifteen years. J Shoulder Elbow Surg. 2013;22:1199–1208. doi: 10.1016/j.jse.2012.11.016. [DOI] [PubMed] [Google Scholar]
- 10.Ferrando A., Kingston R., Delaney R.A. Superior capsular reconstruction using a porcine dermal xenograft for irreparable rotator cuff tears: outcomes at minimum two-year follow-up. J Shoulder Elbow Surg. 2020;30:1053–1059. doi: 10.1016/j.jse.2020.08.020. [DOI] [PubMed] [Google Scholar]
- 11.Gabbott B., Pearse Y., Arnander M., Tennent D. Superior capsule reconstruction is a viable option for patients with symptomatic, isolated, and irreparable supraspinatus tears. Arthrosc Sports Med Rehabil. 2022;4:e591–e597. doi: 10.1016/j.asmr.2021.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Galatz L.M., Ball C.M., Teefey S.A., Middleton W.D., Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86-a:219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Gerber C., Maquieira G., Espinosa N. Latissimus dorsi transfer for the treatment of irreparable rotator cuff tears. J Bone Joint Surg Am. 2006;88:113–120. doi: 10.2106/jbjs.E.00282. [DOI] [PubMed] [Google Scholar]
- 14.Hamada K., Fukuda H., Mikasa M., Kobayashi Y. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res. 1990:92–96. [PubMed] [Google Scholar]
- 15.Hammad A.M., Phillips C., Wijdicks C.A., Adams C.R., Denard P.J. Two-year retrospective patient-reported outcomes following superior capsular reconstruction. Arthroscopy. 2021;38:262–266. doi: 10.1016/j.arthro.2021.05.025. [DOI] [PubMed] [Google Scholar]
- 16.Hanada K., Fukuda H., Hamada K., Nakajima T. Rotator cuff tears in the patient with paraplegia. J Shoulder Elbow Surg. 1993;2:64–69. doi: 10.1016/1058-2746(93)90002-X. [DOI] [PubMed] [Google Scholar]
- 17.Harris P.A., Taylor R., Minor B.L., Elliott V., Fernandez M., O'Neal L., et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95 doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hockman D.E., Lucas G.L., Roth C.A. Role of the coracoacromial ligament as restraint after shoulder hemiarthroplasty. Clin Orthop Relat Res. 2004:80–82. doi: 10.1097/00003086-200402000-00014. [DOI] [PubMed] [Google Scholar]
- 20.Ishihara Y., Mihata T., Tamboli M., Nguyen L., Park K.J., McGarry M.H., et al. Role of the superior shoulder capsule in passive stability of the glenohumeral joint. J Shoulder Elbow Surg. 2014;23:642–648. doi: 10.1016/j.jse.2013.09.025. [DOI] [PubMed] [Google Scholar]
- 21.Keener J.D., Galatz L.M., Teefey S.A., Middleton W.D., Steger-May K., Stobbs-Cucchi G., et al. A prospective evaluation of survivorship of asymptomatic degenerative rotator cuff tears. J Bone Joint Surg Am. 2015;97:89–98. doi: 10.2106/jbjs.n.00099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kholinne E., Jeon I.H. Arthroscopic superior capsular reconstruction of the shoulder: a narrative review. Ann Transl Med. 2021;9:268. doi: 10.21037/atm-20-5925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kirkley A., Alvarez C., Griffin S. The development and evaluation of a disease-specific quality-of-life questionnaire for disorders of the rotator cuff: the Western Ontario Rotator Cuff Index. Clin J Sport Med. 2003;13:84–92. doi: 10.1097/00042752-200303000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Kwon J., Kim S.H., Lee Y.H., Kim T.I., Oh J.H. The rotator cuff healing index: a new scoring system to predict rotator cuff healing after surgical repair. Am J Sports Med. 2019;47:173–180. doi: 10.1177/0363546518810763. [DOI] [PubMed] [Google Scholar]
- 25.Lo I.K., Burkhart S.S. Arthroscopic revision of failed rotator cuff repairs: technique and results. Arthroscopy. 2004;20:250–267. doi: 10.1016/j.arthro.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 26.Malahias M.A., Kostretzis L., Chronopoulos E., Brilakis E., Avramidis G., Antonogiannakis E. Arthroscopic partial repair for massive rotator cuff tears: does it work? A systematic review. Sports Med Open. 2019;5:13. doi: 10.1186/s40798-019-0186-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Meshram P., Liu B., Kim S.W., Heo K., Oh J.H. Revision rotator cuff repair versus primary repair for large to massive tears involving the posterosuperior cuff: comparison of clinical and radiological outcomes. Orthop J Sports Med. 2021;9 doi: 10.1177/2325967121998791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Michener L.A., McClure P.W., Sennett B.J. American shoulder and elbow surgeons Standardized shoulder assessment form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg. 2002;11:587–594. doi: 10.1067/mse.2002.127096. [DOI] [PubMed] [Google Scholar]
- 29.Mihata T. Editorial Commentary: superior capsule reconstruction: grafts for superior capsular reconstruction must be thick and stiff. Arthroscopy. 2019;35:2535–2536. doi: 10.1016/j.arthro.2019.04.019. [DOI] [PubMed] [Google Scholar]
- 30.Mihata T., Lee T.Q., Hasegawa A., Fukunishi K., Kawakami T., Fujisawa Y., et al. Five-year follow-up of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. J Bone Joint Surg Am. 2019;101:1921–1930. doi: 10.2106/jbjs.19.00135. [DOI] [PubMed] [Google Scholar]
- 31.Mihata T., Lee T.Q., Watanabe C., Fukunishi K., Ohue M., Tsujimura T., et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29:459–470. doi: 10.1016/j.arthro.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 32.Mihata T., McGarry M.H., Kahn T., Goldberg I., Neo M., Lee T.Q. Biomechanical effect of thickness and tension of fascia lata graft on glenohumeral stability for superior capsule reconstruction in irreparable supraspinatus tears. Arthroscopy. 2016;32:418–426. doi: 10.1016/j.arthro.2015.08.024. [DOI] [PubMed] [Google Scholar]
- 33.Mihata T., McGarry M.H., Pirolo J.M., Kinoshita M., Lee T.Q. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: a biomechanical cadaveric study. Am J Sports Med. 2012;40:2248–2255. doi: 10.1177/0363546512456195. [DOI] [PubMed] [Google Scholar]
- 34.Misir A., Uzun E., Kizkapan T.B., Ozcamdalli M., Sekban H., Guney A. Factors associated with the development of early- to mid-term cuff-tear arthropathy following arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2021;30:1572–1580. doi: 10.1016/j.jse.2020.09.016. [DOI] [PubMed] [Google Scholar]
- 35.Neumann J.A., Zgonis M.H., Rickert K.D., Bradley K.E., Kremen T.J., Boggess B.R., et al. Interposition dermal matrix xenografts: a successful alternative to traditional treatment of massive rotator cuff tears. Am J Sports Med. 2017;45:1261–1268. doi: 10.1177/0363546516683945. [DOI] [PubMed] [Google Scholar]
- 36.Ono Y., LeBlanc J., Bois A.J., Tsuchiya S., Thangarajah T., More K.D., et al. Graft healing is more important than graft technique: superior capsular reconstruction versus bridging grafts - a prospective randomized controlled trial. Arthroscopy. 2022;38:3109–3117. doi: 10.1016/j.arthro.2022.06.033. [DOI] [PubMed] [Google Scholar]
- 37.Pashuck T.D., Hirahara A.M., Cook J.L., Cook C.R., Andersen W.J., Smith M.J. Superior capsular reconstruction using dermal allograft is a Safe and effective treatment for massive irreparable rotator cuff tears: 2-year clinical outcomes. Arthroscopy. 2021;37:489–496.e1. doi: 10.1016/j.arthro.2020.10.014. [DOI] [PubMed] [Google Scholar]
- 38.Pennington W.T., Bartz B.A., Pauli J.M., Walker C.E., Schmidt W. Arthroscopic superior capsular reconstruction with acellular dermal allograft for the treatment of massive irreparable rotator cuff tears: short-term clinical outcomes and the radiographic parameter of superior capsular distance. Arthroscopy. 2018;34:1764–1773. doi: 10.1016/j.arthro.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 39.Polacek M., Nyegaard C.P. Superior capsular reconstruction using 3-layered fascia lata autograft reinforced with a nonresorbable suture mesh. Arthrosc Sports Med Rehabil. 2020;2:e489–e497. doi: 10.1016/j.asmr.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rashid M.S., Novak M., Lo A., Lo I.K.Y. A technique using an easy-to-fabricate cannula to manage sutures and aid graft passage in arthroscopic superior capsular reconstruction. Arthrosc Tech. 2019;8:e847–e850. doi: 10.1016/j.eats.2019.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Samilson R.L., Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am. 1983;65:456–460. [PubMed] [Google Scholar]
- 42.Scheiderer B., Kia C., Obopilwe E., Johnson J.D., Cote M.P., Imhoff F.B., et al. Biomechanical effect of superior capsule reconstruction using a 3-mm and 6-mm thick acellular dermal allograft in a dynamic shoulder model. Arthroscopy. 2020;36:355–364. doi: 10.1016/j.arthro.2019.08.026. [DOI] [PubMed] [Google Scholar]
- 43.Shamsudin A., Lam P.H., Peters K., Rubenis I., Hackett L., Murrell G.A. Revision versus primary arthroscopic rotator cuff repair: a 2-year analysis of outcomes in 360 patients. Am J Sports Med. 2015;43:557–564. doi: 10.1177/0363546514560729. [DOI] [PubMed] [Google Scholar]
- 44.Sugaya H., Maeda K., Matsuki K., Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am. 2007;89:953–960. doi: 10.2106/jbjs.F.00512. [DOI] [PubMed] [Google Scholar]
- 45.Woodmass J.M., Wagner E.R., Borque K.A., Chang M.J., Welp K.M., Warner J.J.P. Superior capsule reconstruction using dermal allograft: early outcomes and survival. J Shoulder Elbow Surg. 2019;28:S100–S109. doi: 10.1016/j.jse.2019.04.011. [DOI] [PubMed] [Google Scholar]
- 46.Yoo J.C., Ahn J.H., Koh K.H., Lim K.S. Rotator cuff integrity after arthroscopic repair for large tears with less-than-optimal footprint coverage. Arthroscopy. 2009;25:1093–1100. doi: 10.1016/j.arthro.2009.07.010. [DOI] [PubMed] [Google Scholar]