Key Points
Question
What is the societal burden of unintentional opioid-related deaths in the US, and has it changed during the COVID-19 pandemic?
Findings
In this cross-sectional study of 422 605 unintentional deaths due to opioid toxicity, the years of life lost increased more than 3-fold, from 777 597 to 2 922 497, between 2011 and 2021. By 2021, 1 of every 22 deaths in the US was attributable to unintentional opioid toxicity.
Meaning
The findings of this study suggest that public health impacts of opioid-related toxicity in the US are broad and have worsened during the pandemic, underscoring the urgent need to support people at risk of substance-related harm, particularly men, younger adults, and adolescents.
Abstract
Importance
Opioid-related harms constitute a major public health crisis in the US, and this crisis has worsened during the COVID-19 pandemic.
Objectives
To characterize the societal burden of unintentional opioid-related deaths in the US and describe changing mortality patterns during the COVID-19 pandemic.
Design, Setting, and Participants
A serial cross-sectional study examined all unintentional opioid-related deaths in the US, evaluated annually from calendar years 2011 to 2021.
Main Outcomes and Measures
The public health burden of opioid toxicity–related deaths was estimated in 2 ways. First, the proportion of all deaths that were attributable to unintentional opioid toxicity by year (2011, 2013, 2015, 2017, 2019, and 2021) and age group (15-19, 20-29, 30-39, 40-49, 50-59, and 60-74 years) were calculated, using age-specific estimates of all-cause mortality as the denominator. Second, the total years of life lost (YLL) due to unintentional opioid toxicity was estimated, overall and by sex and age group, for each year studied.
Results
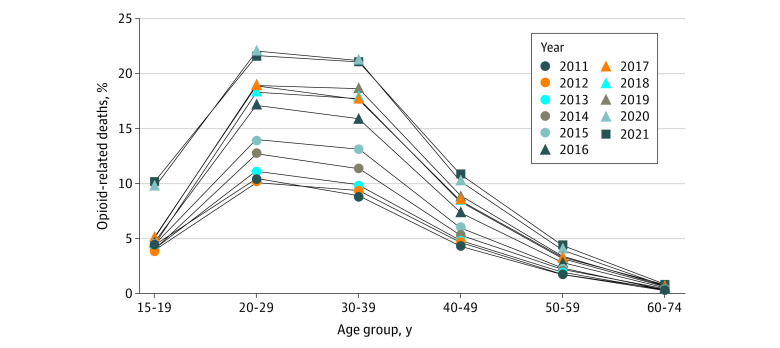
Among the 422 605 unintentional deaths due to opioid toxicity between 2011 and 2021, the median age of the individuals was 39 (IQR, 30-51) years, and 69.7% were male. The number of unintentional deaths due to opioid toxicity increased 289% over the study period, from 19 395 (2011) to 75 477 (2021). Similarly, the percentage of all deaths that were attributed to opioid toxicity increased from 1.8% in 2011 to 4.5% in 2021. By 2021, opioid toxicity was responsible for 10.2% of all deaths among those aged 15 to 19 years, 21.7% of deaths among those aged 20 to 29 years, and 21.0% of deaths among those aged 30 to 39 years. The YLL due to opioid toxicity increased 276% over the study period, from 777 597 in 2011 to 2 922 497 in 2021. While YLL plateaued between 2017 (7.0 YLL per 1000) and 2019 (7.2 YLL per 1000), it increased by 62.9% between 2019 and 2021 coincident with the COVID-19 pandemic, reaching 11.7 YLL per 1000 population. This relative increase was similar across all age groups and sexes with the exception of those aged 15 to 19 years, in whom the YLL nearly tripled, from 1.5 to 3.9 YLL per 1000 population.
Conclusions and Relevance
In this cross-sectional study, deaths due to opioid toxicity increased substantially during the COVID-19 pandemic. By 2021, 1 of every 22 deaths in the US was attributable to unintentional opioid toxicity, underscoring the urgent need to support people at risk of substance-related harm, particularly men, younger adults, and adolescents.
This cross-sectional study examines changes in death rates due to unintentional opioid toxicity between 2011 and 2021.
Introduction
Over the past 2 decades, opioid-related harms have emerged as a leading public health crisis in North America. In the US, the number of deaths due to opioid toxicity has increased from 21 088 in 2010 to nearly 70 000 in 2020, with the increase due primarily to fentanyl and its analogues.1,2 Younger adults represent a disproportionate number of these deaths,3 with early loss of life imparting a major toll on public health.1,3 Despite early signals that rates of death due to opioid toxicity slowed between 2017 and 2019,1 the COVID-19 pandemic carried with it major changes in societal priorities and access to health services that, along with the increasing dangers of the unregulated drug supply, were anticipated to aggravate opioid-related harms.4,5 In 2020, the US Centers for Disease Control and Prevention (CDC) reported 68 630 opioid-related deaths, a 47% increase from 2018.1
In 2016, deaths due to opioid toxicity resulted in an estimated 1.68 million years of life lost (YLL) in the US,3 and in 2019, it was estimated that more than half of all deaths due to drug toxicity worldwide occurred in the US.6 We sought to characterize the growing societal burden of unintentional opioid-related deaths in the US and examine patterns during the COVID-19 pandemic and across demographic subgroups of the population.
Methods
Study Design and Population
We conducted a serial cross-sectional study by extracting annual counts of deaths due to unintentional opioid toxicity in the US between calendar years 2011 and 2021. Informed consent was not required given the deidentified, aggregated nature of the data. The study received an exemption from the Unity Health Toronto Research Ethics Board, Toronto, Ontario, Canada. This study follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for cross-sectional studies.
Data Sources and Outcome Definition
We used data from the CDC Wide-Ranging Online Data for Epidemiologic Research (WONDER) Multiple Cause of Death database, which captures national-level mortality and population data for all US residents using information recorded on death certificates (eTable 1 in Supplement 1).7 Our main outcome was unintentional deaths in which prescribed or unregulated (principally heroin and analogues of fentanyl) opioids contributed to death. Consistent with CDC standards,1 we defined opioid toxicity–related deaths as those in which an underlying cause of death due to unintentional drug poisoning and a multiple cause of death code related to an opioid were recorded (eTable 2 in Supplement 1). To avoid data gaps due to suppressed data, we excluded all deaths among people younger than 15 years and older than 74 years.
Burden of Unintentional Opioid Toxicity–Related Deaths
We defined the burden of unintentional deaths due to opioid toxicity in 2 ways. First, we determined the proportion of all deaths attributable to unintentional opioid toxicity by year and age group (15-19, 20-29, 30-39, 40-49, 50-59, and 60-74 years) using age-specific estimates of all-cause mortality as the denominator. Second, we used methods adapted from the Global Burden of Disease Study8 to estimate the YLL due to unintentional opioid toxicity (eTable 3 in Supplement 1). We aggregated YLL by sex and age group for each year of the study period, reported as absolute numbers and population-adjusted rates.
In a sensitivity analysis to explore and contrast the findings with deaths related to COVID-19, we replicated the overall estimates of the proportions of deaths attributable to unintentional opioid toxicity, excluding all COVID-19–related deaths (underlying cause of death International Statistical Classification of Diseases and Related Health Problems, 10th Revision code U07.1) from the denominator in 2020 and 2021. Additionally, in a secondary analysis, we calculated the YLL due to COVID-19 in 2020 and 2021, using methods consistent with those outlined above.
Statistical Analysis
We used descriptive statistics to summarize demographic characteristics of unintentional deaths due to opioid toxicity and the Cochrane-Armitage test for trend to compare the percentage of deaths attributable to opioids by age group over time. All analyses used SAS, version 9.4 (SAS Institute) or Microsoft Excel (Microsoft Corp), and a 2-sided, type I error rate of .05 was the threshold for statistical significance.
Results
During the study period, among the 422 605 unintentional deaths due to opioid toxicity, the median age of the individuals was 39 (IQR, 30-51) years, 69.7% were male, and 30.3% were female. The number of unintentional deaths due to opioid toxicity increased 289% over the study period, from 19 395 (83.8 per million) in 2011 to 75 477 (302.9 per million) in 2021. The percentage of all deaths attributable to opioid toxicity increased from 1.8% in 2011 to 4.5% in 2021 (Figure 1), with a statistically significant trend observed in all age groups. For example, among those aged 30 to 39 years, the proportion increased from 8.9% (2011) to 21.0% (2021) (P < .001). By 2021, more than 20% of all deaths among individuals aged 20 to 29 years (21.7%) and 30 to 39 years (21.0%) were due to opioid toxicity; however, the largest relative increase occurred among those aged 15 to 19 years, in whom the proportion of deaths attributable to opioid toxicity more than doubled, from 5.0% in 2019 to 10.2% in 2021. In the sensitivity analysis excluding COVID-19–related deaths from the denominator, the percentage of deaths attributable to opioid toxicity increased to 5.3% in 2021.
Figure 1. Percentage of All-Cause Deaths Attributable to Unintentional Opioid Toxicity.
The percentage of all-cause deaths attributable to unintentional opioid toxicity increased between 2011 and 2021 across all age groups, with large increases observed between 2019 and 2020, coincident with the COVID-19 pandemic.
The YLL due to opioid toxicity in the US increased substantially over the study period, from 777 597 YLL (2011) to 2 922 497 YLL (2021)—a relative increase of 276% (Table 1; eTable 4 in Supplement 1). However, this increase was not consistent over the study period. While YLL increased from 2011 to 2017, it plateaued between 2017 (7.0 YLL per 1000 population) and 2019 (7.2 YLL per 1000 population) (Figure 2, Table 1). Over the ensuing 2 years, and coincident with the COVID-19 pandemic, the population-adjusted rate of YLL increased by 62.9%, reaching 11.7 YLL per 1000 population in 2021. This pattern was similar across age groups and sexes except among those aged 15 to 19 years, in whom the YLL nearly tripled, from 1.5 to 3.9 YLL per 1000 population (from 31 097 to 83 193 YLL) (Table 1).
Table 1. Years of Life Lost Due to Unintentional Opioid Toxicity in the US by Age and Sex, 2019 to 2021.
| Age groups, y | 2019, No. | 2020, No. | 2021, No. | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unintentional opioid-related deaths | Deaths per million | YLL | YLL per 1000 | Unintentional opioid-related deaths | Deaths per million | YLL | YLL per 1000 | Unintentional opioid-related deaths | Deaths per million | YLL | YLL per 1000 | |
| Overall | 45 315 | 184.9 | 1 772 030 | 7.2 | 63 946 | 259.9 | 2 521 813 | 10.2 | 75 477 | 302.9 | 2 922 497 | 11.7 |
| 15-19 | 515 | 24.5 | 31 097 | 1.5 | 1196 | 57.1 | 72 260 | 3.4 | 1371 | 63.6 | 83 193 | 3.9 |
| 20-29 | 8786 | 194.6 | 468 243 | 10.4 | 12 377 | 276.1 | 660 835 | 14.7 | 13 035 | 296.8 | 695 949 | 15.8 |
| 30-39 | 13 234 | 299.6 | 596 845 | 13.5 | 18 831 | 421.6 | 848 304 | 19.0 | 21 741 | 478.9 | 979 090 | 21.6 |
| 40-49 | 9623 | 238.7 | 347 225 | 8.6 | 13 741 | 341.1 | 497 694 | 12.4 | 16 650 | 407.2 | 604 488 | 14.8 |
| 50-59 | 8811 | 208.0 | 242 351 | 5.7 | 11 768 | 280.2 | 322 987 | 7.7 | 14 581 | 343.3 | 399 710 | 9.4 |
| 60-74 | 4346 | 83.5 | 86 269 | 1.7 | 6033 | 113.1 | 119 732 | 2.2 | 8099 | 147.5 | 160 068 | 2.9 |
| Males | 32 041 | 264.1 | 1 224 382 | 10.1 | 45 852 | 376.4 | 1 765 682 | 14.5 | 53 797 | 433.7 | 2 030 032 | 16.4 |
| 15-19 | 370 | 34.4 | 21 846 | 2.0 | 879 | 82.2 | 51 957 | 4.9 | 962 | 87.3 | 56 926 | 5.2 |
| 20-29 | 6388 | 276.9 | 332 428 | 14.4 | 9120 | 398.1 | 475 773 | 20.8 | 9475 | 423.9 | 493 409 | 22.1 |
| 30-39 | 9442 | 424.6 | 414 342 | 18.6 | 13 628 | 605.5 | 597 869 | 26.6 | 15 685 | 683.8 | 688 162 | 30.0 |
| 40-49 | 6878 | 344.0 | 241 137 | 12.1 | 9756 | 488.3 | 342 525 | 17.1 | 11 853 | 579.1 | 417 216 | 20.4 |
| 50-59 | 5947 | 286.9 | 157 236 | 7.6 | 8167 | 397.2 | 215 820 | 10.5 | 10 037 | 476.4 | 264 712 | 12.6 |
| 60-74 | 3016 | 122.8 | 57 394 | 2.3 | 4302 | 171.0 | 81 738 | 3.2 | 5785 | 220.8 | 109 606 | 4.2 |
| Females | 13 274 | 107.3 | 547 648 | 4.4 | 18 094 | 145.6 | 756 130 | 6.1 | 21 680 | 173.3 | 892 466 | 7.1 |
| 15-19 | 145 | 14.1 | 9251 | 0.9 | 317 | 30.9 | 20 303 | 2.0 | 409 | 38.8 | 26 266 | 2.5 |
| 20-29 | 2398 | 108.6 | 135 815 | 6.2 | 3257 | 148.6 | 185 062 | 8.4 | 3560 | 165.1 | 202 540 | 9.4 |
| 30-39 | 3792 | 172.9 | 182 503 | 8.3 | 5203 | 234.8 | 250 435 | 11.3 | 6056 | 269.6 | 290 928 | 13.0 |
| 40-49 | 2745 | 135.0 | 106 088 | 5.2 | 3985 | 196.3 | 155 169 | 7.6 | 4797 | 235.0 | 187 272 | 9.2 |
| 50-59 | 2864 | 132.4 | 85 114 | 3.9 | 3601 | 168.0 | 107 167 | 5.0 | 4544 | 212.3 | 134 998 | 6.3 |
| 60-74 | 1330 | 48.4 | 28 876 | 1.1 | 1731 | 61.4 | 37 994 | 1.3 | 2314 | 80.6 | 50 463 | 1.8 |
Abbreviation: YLL, years of life lost.
Figure 2. Years of Life Lost to Unintentional Opioid Toxicity in the US.
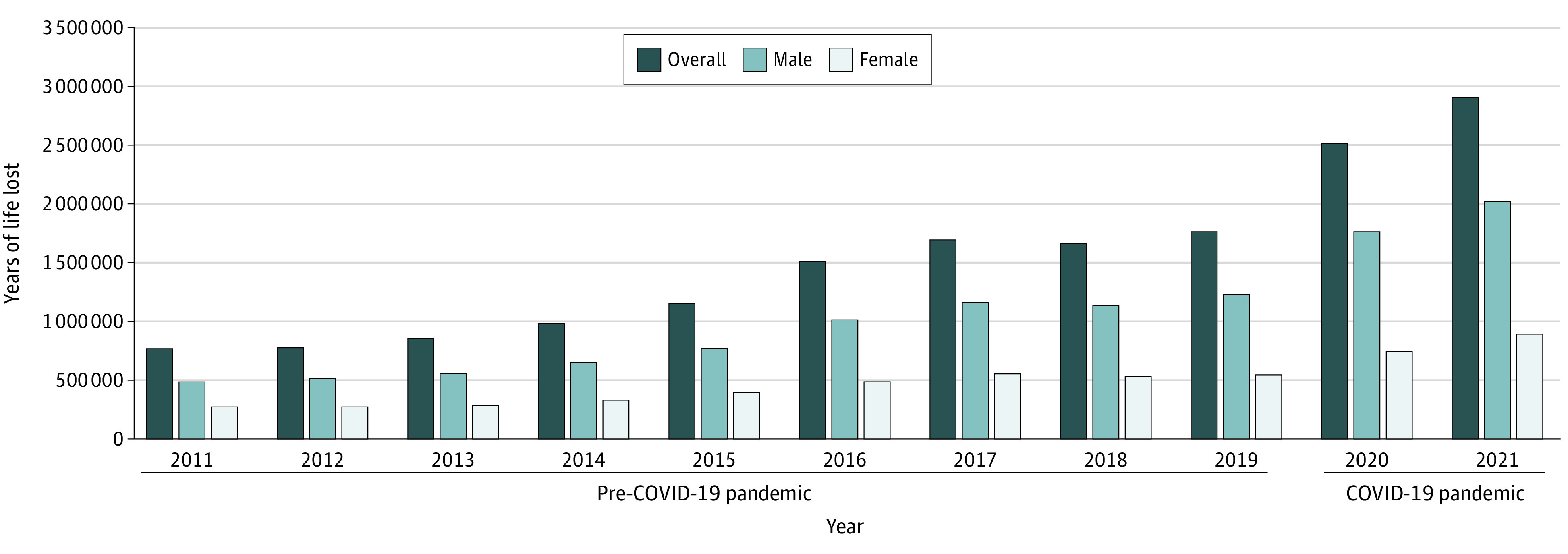
Years of life lost were calculated using methods adapted from the Global Burden of Disease Study.8 The years of life lost remained higher in males throughout the study.
In 2021, the total burden of deaths due to opioid toxicity was highest among men (16.4 vs 7.1 YLL per 1000 for men vs women) and those aged 30 to 39 years (21.6 per 1000). The highest burden was evident among men aged 30 to 39 years, with 15 685 individuals dying from opioid toxicity in 2021, leading to 688 162 YLL (30.0 YLL per 1000 population).
In the secondary analysis, there were 3 066 440 YLL due to COVID-19 in 2020, increasing to 5 512 380 YLL in 2021 (Table 2). Years of life lost was generally higher among men compared with women and among those aged 40 years and older. Among individuals aged 15 to 39 years, the YLL due to opioid toxicity in both 2020 and 2021 were higher than those attributable to COVID-19.
Table 2. Years of Life Lost to COVID-19 in the US by Age and Sex, 2020 and 2021.
| Age groups, y | 2020, No. | 2021, No. | ||||||
|---|---|---|---|---|---|---|---|---|
| COVID-19 related deaths | Deaths per million | YLL | YLL per 1000 | COVID-19 related deaths | Deaths per million | YLL | YLL per 1000 | |
| Overall | 144 165 | 585.8 | 3 066 440 | 12.5 | 236 862 | 950.7 | 5 512 380 | 22.1 |
| 15-19 | 118 | 5.6 | 7192 | 0.3 | 351 | 16.3 | 21 603 | 1.0 |
| 20-29 | 1175 | 26.2 | 62 892 | 1.4 | 3149 | 71.7 | 168 927 | 3.8 |
| 30-39 | 3729 | 83.5 | 166 078 | 3.7 | 10 330 | 227.5 | 462 340 | 10.2 |
| 40-49 | 10 410 | 258.5 | 367 648 | 9.1 | 24 412 | 597.1 | 870 494 | 21.3 |
| 50-59 | 26 997 | 642.8 | 723 631 | 17.2 | 53 384 | 1256.9 | 1 445 540 | 34.0 |
| 60-74 | 101 736 | 1907.0 | 1 738 999 | 32.6 | 145 236 | 2645.4 | 2 543 476 | 46.3 |
| Males | 91 239 | 749.0 | 1 871 371 | 15.4 | 142 827 | 1151.4 | 3 198 167 | 25.8 |
| 15-19 | 59 | 5.5 | 3449 | 0.3 | 215 | 19.5 | 12 828 | 1.2 |
| 20-29 | 763 | 33.3 | 39 550 | 1.7 | 1964 | 87.9 | 101 732 | 4.6 |
| 30-39 | 2500 | 111.1 | 107 682 | 4.8 | 6491 | 283.0 | 280 329 | 12.2 |
| 40-49 | 6953 | 348.0 | 236 695 | 11.8 | 15 237 | 744.4 | 521 104 | 25.5 |
| 50-59 | 17 751 | 863.2 | 456 289 | 22.2 | 33 525 | 1591.4 | 867 473 | 41.2 |
| 60-74 | 63 213 | 2512.3 | 1 027 705 | 40.8 | 85 395 | 3259.1 | 1 414 701 | 54.0 |
| Females | 52 926 | 425.9 | 1 195 069 | 9.6 | 94 035 | 751.7 | 2 314 213 | 18.5 |
| 15-19 | 59 | 5.7 | 3743 | 0.4 | 136 | 12.9 | 8775 | 0.8 |
| 20-29 | 412 | 18.8 | 23 342 | 1.1 | 1185 | 55.0 | 67 194 | 3.1 |
| 30-39 | 1229 | 55.5 | 58 396 | 2.6 | 3839 | 170.9 | 182 011 | 8.1 |
| 40-49 | 3457 | 170.3 | 130 953 | 6.5 | 9175 | 449.4 | 349 390 | 17.1 |
| 50-59 | 9246 | 431.4 | 267 342 | 12.5 | 19 859 | 927.6 | 578 068 | 27.0 |
| 60-74 | 38 523 | 1366.6 | 711 294 | 25.2 | 59 841 | 2085.1 | 1 128 776 | 39.3 |
Abbreviation: YLL, years of life lost.
Discussion
In 2021, 1 in 22 deaths in the US was attributable to unintentional opioid toxicity, resulting in nearly 3 million YLL. This burden was most pronounced among men aged 30 to 39 years but has been increasing, especially rapidly among those aged 15 to 19 years, with 1 in 10 deaths now opioid related. The overall burden increased considerably during the COVID-19 pandemic, increasing 63% between 2019 and 2021 despite stabilizing from 2017 to 2019.1
These findings highlight the enormous societal burden imparted by the overdose crisis in the US over the past decade, particularly among younger adults, a demographic cohort disproportionately impacted by substance-related harms.1,3,9 In addition, despite historically lower rates of opioid-related deaths among adolescents, this demographic cohort witnessed a more than doubling in death rates and YLL during the COVID-19 pandemic. Furthermore, the absolute number of unintentional deaths due to opioid toxicity and the associated YLL among those younger than 40 years far exceeded those attributable to COVID-19 in both 2020 and 2021, indicating the distinct impact of drug toxicity–related deaths among younger individuals. This aligns with previous observations of accelerating substance-related harm among adolescents10 and warrants further attention and expansion of harm reduction and treatment programs tailored to this demographic population.
It is important to place the findings of this study in context against other causes of death in the US. Specifically, these findings suggest that the YLL from unintentional opioid toxicity in 2020 (2 521 813 YLL) was comparable to the YLL from COVID-19 that same year (3 066 440 YLL) and amounted to 53% of the YLL attributable to COVID-19 in 2021 (2 922 497 YLL/5 512 380 YLL). Similarly, compared with estimates for other causes of death from the 2019 Global Burden of Disease study, the YLL attributable to opioid toxicity among those aged 15 to 74 years in the US (1 772 030 YLL in 2019) far exceeded those attributable to diabetes (1 115 879 YLL), road injuries (1 602 101 YLL), and stroke (1 442 702 YLL) in this population.11
Limitations
This study has limitations. Death investigations in the US are managed at the state level and may involve a medical examiner system, coroner system, or both.12 Therefore, while our definitions align with those of the CDC, some ascertainment bias may be present. Furthermore, cause of death data are not yet available for 2022; future research should explore the ongoing influence of the COVID-19 pandemic on drug toxicity–related deaths in the US.
Conclusions
The crisis of deaths due to opioid toxicity across the US worsened substantially during the COVID-19 pandemic, with 1 in 22 deaths in 2021 attributable to unintentional opioid toxicity. The findings noted in this cross-sectional study underscore the urgent need to support people at risk of substance-related harm, particularly men, younger adults, and adolescents.
eTable 1. Databases Used to Capture All-Cause and Opioid-Toxicity Deaths in the United States
eTable 2. International Classification of Diseases and Related Health Problems, 10th Revision Diagnosis Codes and Descriptions
eTable 3. Details on Calculation of Years of Life Lost
eTable 4. Years of Life Lost Due to Accidental Opioid Toxicities in the United States. Overall and by Age and Sex, 2011 to 2018
Data Sharing Statement
References
- 1.National Institute of Drug Abuse . Drug overdose death rates. 2022. Accessed February 2, 2023. https://nida.nih.gov/research-topics/trends-statistics/overdose-death-rates#:~:text=Opioid%2Dinvolved%20overdose%20deaths%20rose
- 2.Spencer MR, Minino AM, Warner M. Drug overdose deaths in the United States, 2001–2021. 2022. NCHS Data Brief. 2022;(457):1-8. [PubMed] [Google Scholar]
- 3.Gomes T, Tadrous M, Mamdani MM, Paterson JM, Juurlink DN. The burden of opioid-related mortality in the United States. JAMA Netw Open. 2018;1(2):e180217. doi: 10.1001/jamanetworkopen.2018.0217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Canadian Centre on Substance Use and Addiction . Changes related to COVID-19 in the illegal drug supply and access to services, and resulting health harms. 2020. Accessed February 2, 2023. https://www.ccsa.ca/changes-related-covid-19-illegal-drug-supply-and-access-services-and-resulting-health-harms
- 5.Chacon NC, Walia N, Allen A, et al. Substance use during COVID-19 pandemic: impact on the underserved communities. Discoveries (Craiova). 2021;9(4):e141. doi: 10.15190/d.2021.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diseases GBD, Injuries C; GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204-1222. doi: 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention . National Center for Health Statistics mortality data on CDC Wonder. 2022. Accessed February 2, 2023. https://wonder.cdc.gov/mcd.html
- 8.Department of Information Evidence and Research . Who Methods and Data Sources for Global Burden of Disease Estimates 2000-2015. World Health Organization; 2017. [Google Scholar]
- 9.Gomes T, Kitchen SA, Murray R. Measuring the burden of opioid-related mortality in Ontario, Canada, during the COVID-19 pandemic. JAMA Netw Open. 2021;4(5):e2112865. doi: 10.1001/jamanetworkopen.2021.12865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim S, Rajack N, Mondoux SE, Tardelli VS, Kolla NJ, Le Foll B. The COVID-19 impact and characterization on substance use–related emergency department visits for adolescents and young adults in Canada: practical implications. J Eval Clin Pract. 2023;29(3):447-458. doi: 10.1111/jep.13817 [DOI] [PubMed] [Google Scholar]
- 11.Institute for Health Metrics and Evaluation. Global Burden of Disease Collaborative Network . Global Burden of Disease Study. 2020. Accessed February 2, 2023. https://vizhub.healthdata.org/gbd-results/
- 12.Centers for Disease Control and Prevention . Death Investigation System. 2019. Accessed February 2, 2023. https://www.cdc.gov/phlp/publications/coroner/death.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Databases Used to Capture All-Cause and Opioid-Toxicity Deaths in the United States
eTable 2. International Classification of Diseases and Related Health Problems, 10th Revision Diagnosis Codes and Descriptions
eTable 3. Details on Calculation of Years of Life Lost
eTable 4. Years of Life Lost Due to Accidental Opioid Toxicities in the United States. Overall and by Age and Sex, 2011 to 2018
Data Sharing Statement