Abstract
There is expansive literature documenting the presence of health disparities, but there are disproportionately few studies describing interventions to reduce disparity. In this narrative review, we categorize interventions to reduce health disparity in pulmonary disease within the US health care system to support future initiatives to reduce disparity. We identified 211 articles describing interventions to reduce disparity in pulmonary disease related to race, income, or sex. We grouped the studies into the following four categories: biologic, educational, behavioral, and structural. We identified the following five main themes: (1) there were few interventional trials compared with the breadth of studies describing health disparities, and trials involving patients with asthma who were Black, low income, and living in an urban setting were overrepresented; (2) race or socioeconomic status was not an effective marker of individual pharmacologic treatment response; (3) telehealth enabled scaling of care, but more work is needed to understand how to leverage telehealth to improve outcomes in marginalized communities; (4) future interventions must explicitly target societal drivers of disparity, rather than focusing on individual behavior alone; and (5) individual interventions will only be maximally effective when specifically tailored to local needs. Much work has been done to catalog health disparities in pulmonary disease. Notable gaps in the identified literature include few interventional trials, the need for research in diseases outside of asthma, the need for high quality effectiveness trials, and an understanding of how to implement proven interventions balancing fidelity to the original protocol and the need to adapt to local barriers to care.
Key Words: asthma, COPD, health care disparities, health inequalities, lung cancer, lung cancer screening, racial disparity, social determinants of health
A growing body of literature highlights the morbidity and mortality of health disparities related to race,1 and socioeconomic status2,3 in pulmonary disease. These data have led to consistent calls from major pulmonary societies for increased efforts to reduce disparities in asthma,4 COPD,5 pulmonary hypertension,6 lung cancer screening,7 and respiratory disease in general.8 In contrast to the large body of work cataloging the existence of health disparities, there has been comparatively limited work on interventions to reduce these disparities. This gap in the literature undercuts statements calling for aggressive action to combat health inequity.
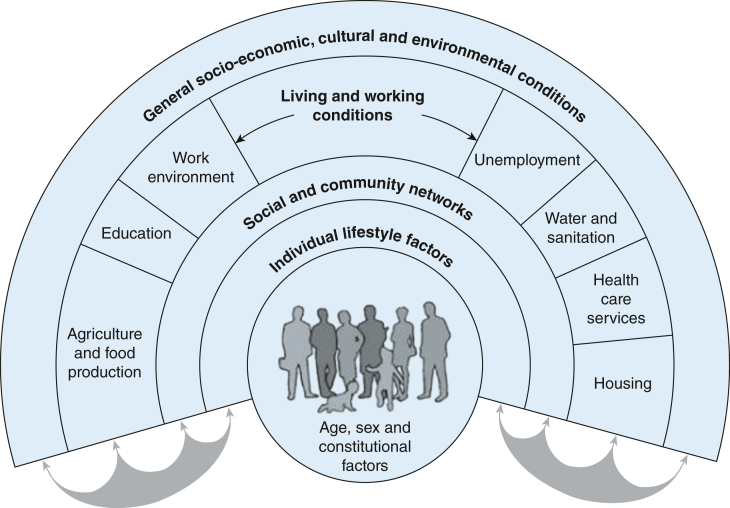
Developing interventions to mitigate health disparities is complicated by tangled interactions of disease biology, social factors, and structural racism and classism. Reducing health disparity requires selection and tailoring of interventions to address complex interactions of multiple drivers of disparity. The Whitehead model of social determinants of health (Fig 1)9 is an influential framework for conceptualizing this complex interplay because of its simplicity and broad applicability. The Whitehead model, similar to the many frameworks that have come after it, highlights the cross interaction of biologic, individual, social, environmental, and policy drivers on patient outcomes. Here, we review interventions focused on addressing health disparities in pulmonary disease through the lens of the Whitehead model (Table 1). We sought to catalog a broad range of intervention modalities and identify the social determinants of health targeted by each intervention as categorized by the Whitehead model. The goal of this work is to provide physicians and researchers a starting place for selecting an intervention for health disparities that meets local needs.
Figure 1.
Dahlgren-Whitehead model of social determinants of health.
Table 1.
Description of Categorization Strategy for Mediator of Heath Disparities Addressed by Each Intervention Based on the Dahlgren-Whitehead Model of Social Determinants of Health
| Dahlgren-Whitehead Mediators | Category Name | Included Trials |
|---|---|---|
| Age, sex, and constitutional factors | Biologic | Interventions aiming to target unique biology leading to health disparities (eg, differing dosing strategies for Black patients) |
| Individual lifestyle factors | Individual | Interventions aiming to change patient knowledge of disease, change adherence with treatment, and increase healthy behaviors |
| Social and community networks | Social | Interventions which improved patient interaction with local support networks (family, church, other patients) or facilitated access to existing community resources |
| Living and working conditions | Environment | Interventions which sought to improve access to resources, housing, education, food, and so forth |
| General socioeconomic, cultural, and environmental conditions | Societal | Interventions specifically tailored for the cultural experience of a patient population or seeking policy change |
Literature Search
The search strategy is detailed in e-Appendix 1. Briefly, a search was crafted by the first author to identify articles addressing interventions for health disparities in pulmonary disease (search conducted on July 21, 2021). In the first round, we noted that most interventions were for patients with asthma. Therefore, the first author crafted targeted follow-up searches focused on COPD, lung cancer, pulmonary hypertension, and interstitial lung disease (searches conducted on November 29, 2021, and February 22, 2022; search strategies detailed in e-Appendix 1). In total, 3,480 articles were screened by the first author with 130 articles selected for inclusion. An additional 81 articles were identified from the references of the included articles (e-Fig 1). Inclusion criteria (defined a priori) were as follows: (1) detailed an intervention; (2) addressed a disparity related to race, sex, or socioeconomic status; and (3) carried out in the United States. Reasons for article exclusion are detailed in e-Table 1. We focused on interventions from the United States given the unique nature of the US health care reimbursement system and its well-documented and persistent history of racial disparities.
We classified interventions into four categories (biologic, educational, behavioral, and structural) with subcategories in a framework we developed after review of the identified literature (Table 2). We categorized details of each intervention according to which components of the Whitehead model were most closely addressed, the population targeted by the study, and the intervention strategy for the 211 identified studies (e-Tables 2-11). Each study was reviewed by two independent reviewers. When disagreements arose, they were settled by consensus between the first and senior authors.
Table 2.
Characteristics of Interventions by Intervention Type
| Intervention Categories and Subcategories | No. of Articles | Dahlgren-Whitehead Mediators | Disease | Methodology | Population |
|---|---|---|---|---|---|
| Biologic | |||||
| e-Table 2: pharmacologic | 16 | Biologic: n = 16 | Asthma adult: n = 7 COPD: n = 2 Lung cancer: n = 7 |
RCT: n = 7 RCT re-analysis: n = 3 Prospective: n = 2 Retrospective: n = 4 |
Black: n = 13 Non-White: n = 1 Urban: n = 3 |
| e-Table 3: improved screening | 10 | Biologic: n = 6 Individual: n = 2 Environment: n = 10 |
Asthma: n = 2 Lung cancer: n = 8 |
Implementation: n = 1 Prospective: n = 5 Retrospective: n = 3 Pilot: n = 1 |
Black: n = 1 Low income: n = 4 Non-White: n = 2 Rural: n = 1 Urban: n = 3 |
| Education | |||||
| e-Table 4: telehealth | 8 | Individual: n = 8 Social: n = 1 Societal: n = 3 |
Asthma: n = 7 Lung cancer: n = 1 |
RCT: n = 5 Prospective: n = 1 Pilot: n = 2 |
Black: n = 2 Hispanic: n = 1 Rural: n = 1 Urban: n = 4 |
| e-Table 5: in-person | 25 | Individual: n = 25 Social: n = 12 Environment: n = 13 Societal: n = 14 |
Asthma: n = 21 COPD: n = 1 Lung cancer: n = 3 |
Implementation: n = 1 RCT: n = 12 RCT re-analysis: n = 2 Prospective: n = 6 Retrospective: n = 1 Pilot: n = 3 |
Black: n = 13 Chinese: n = 1 Hispanic: n = 5 Low income: n = 11 Low literacy: n = 1 Urban: n = 12 |
| Behavioral | |||||
| e-Table 6: telehealth | 17 | Biologic: n = 2 Individual: n = 17 Social: n = 1 Environment: n = 8 Societal: n = 10 |
Asthma: n = 15 COPD: n = 1 Lung cancer: n = 1 |
RCT: n = 6 RCT re-analysis: n = 2 Prospective: n = 1 Pilot: n = 8 |
Black: n = 10 Hispanic: n = 1 Low income: n = 2 Rural: n = 1 Urban: n = 10 Women: n = 2 |
| e-Table 7: in-person | 29 | Individual: n = 29 Social: n =15 Environment: n = 21 Societal: n = 7 |
Asthma: n = 26 COPD: n = 3 |
Implementation: n = 2 RCT: n = 15 RCT re-analysis: n = 2 Prospective: n = 5 Pilot: n = 5 |
Black: n = 13 Hispanic: n = 5 Low income: n = 13 Urban: n = 8 |
| e-Table 8: clinical trial inclusion | 14 | Social: n = 14 Environment: n = 14 Societal: n = 14 |
Asthma: n = 8 COPD: n = 1 Lung cancer: n = 5 |
RCT: n = 1 RCT re-analysis: n = 2 Prospective: n = 2 Retrospective: n = 8 Pilot: n = 1 |
Black: n = 3 Hispanic: n = 3 Low income: n = 1 Non-White: n = 2 Urban: n = 7 |
| e-Table 9: cleaning | 29 | Individual: n = 26 Social: n = 22 Environment: n = 29 Societal: n = 19 |
Asthma: n = 27 Asthma/COPD: n = 2 |
Implementation: n = 1 RCT: n = 15 RCT re-analysis: n = 3 Prospective: n = 9 Retrospective: n = 1 |
Black: n = 1 Hispanic: n = 1 Low income: n = 19 Non-White: n = 3 Urban: n = 18 |
| Structural | |||||
| e-Table 10: quality/access to care | 45 | Biologic: n = 1 Individual: n = 26 Social: n = 4 Environment: n = 43 Societal: n = 6 |
Asthma: n = 37 COPD: n = 1 Asthma/COPD: n = 1 Lung cancer: n = 4 Lung disease: n = 1 Pneumoconiosis: n = 1 |
Implementation: n = 2 RCT: n = 18 RCT re-analysis: n = 1 Prospective: n = 13 Retrospective: n = 8 Pilot: n = 3 |
Black: n = 12 Hispanic: n = 3 Low income: n = 24 Non-White: n =5 Rural: n = 3 Urban: n =20 |
| e-Table 11: policy | 18 | Biologic: n = 2 Individual: n = 5 Social: n = 5 Environment: n =18 Societal: n = 18 |
Asthma: n = 9 COPD: n = 1 Asthma/COPD: n = 1 Lung cancer: n = 7 |
RCT re-analysis: n = 1 Prospective: n = 1 Retrospective: n = 16 |
Black: n = 8 Hispanic: n = 1 Low income: n = 10 Non-White: n = 2 |
RCT = randomized controlled trial.
Evidence Review
Summary of Interventions
We describe the characteristics of the identified studies in Table 2. Most of the articles screened described a disparity rather than an intervention to reduce the disparity. The most common disease investigated was asthma (159 studies) followed by lung cancer (36 studies) and COPD (10 studies). The identified interventions often defined their population by either socioeconomic status (176 studies) or race (112 studies). Socioeconomic status was defined variably but typically focused on either income or locality. We grouped studies analyzing government insurance, uninsured, or low income as low income (84 studies). The most common location studied was urban (85 studies), with six studies investigating rural populations. The most common race studied was Black (76 studies) followed by Hispanic or Latino (20 studies). Only two studies addressed sex. We did not identify any studies addressing sex identity or sexuality.
Most studies addressed multiple domains from the Whitehead model. The most common domains addressed were social drivers of disparity, with 156 studies addressing environmental factors (eg, housing, access to care, quality of care) and 91 addressing societal issues (eg, policy, culture). Individual factors (eg, disease knowledge, medication compliance) were addressed in 138 studies. Many earlier studies addressed individual factors alone, whereas many recent studies also addressed societal drivers of disparity.
Pharmacologic Interventions
Pharmacologic studies sought to either confirm the efficacy of standard of care in diverse patient groups or determine if tailored therapy based on race could improve outcomes (e-Table 2). This was based on the hypothesis that socioeconomic status or biologic correlates of race might impact medication effect. All studies demonstrated that standard medical therapy was efficacious in non-White and low income populations. Multiple studies in lung cancer showed similar response to treatment between Black and White patients,10 despite observed real-world differences in outcomes.11 In COPD and asthma, standard therapies were effective in Black12 and inner city13 patients. The Best African American Response to Asthma Drugs (BARD) trial14 and the follow-up genomic study of its participants15 demonstrated that although unique alleles mediating the effect of inhaled beta-agonists are present in Black patients, ancestry alone is insufficient to predict individual treatment response. Self-reported race was not demonstrated to be a reliable marker of differential treatment response in multiple high-quality randomized controlled trials (RCTs) with low risk of bias.
Screening
Increased rates of advanced stage lung cancer11 and asthma2 in non-White and low income populations suggest that rigorous screening programs may be able to reduce disparate outcomes through earlier targeted interventions (e-Table 3). Interventions in asthma have focused on individual mediators (ie, patient knowledge, adherence), and used mail16 and internet17 asthma self-assessments. These strategies had low utilization and did not improve outcomes in low income and non-White patients.16 Lung cancer screening interventions expanded screening criteria in low income and non-White populations to address the biologic mediator of higher observed malignancy rate.18 Environmental factors (eg, poor access to care) were addressed through free screenings19 and mobile scanners.20 The identified screening studies were primarily prospective cohorts with moderate to high risk of bias because of historical controls and potential of selection bias.
Education: Telehealth
Telehealth educational interventions are appealing because they are rapidly scalable, flexible, and can address transportation barriers (e-Table 4). Early interventions focused primarily on individual mediators, seeking to increase knowledge of disease management in high-risk groups. Interventions consistently improved knowledge21 but had variable effect on outcomes.22 More recent studies have also sought to address societal factors by culturally tailoring interventions with patient input (eg, awareness campaign collaboratively designed with patients which increased lung cancer screening in a rural region).23 Conversely, a one-time viewing of an educational video tailored for urban people with asthma was ineffective at improving outcomes.24 The identified studies were primarily RCTs with risk of bias because of inability to blind participants and lack of description of blinding of reviewers. Taken together, educational telehealth interventions hold promise, but one-time interventions, or interventions that focus only on improving individual behaviors without tailoring for cultural background, may be less likely to succeed.
Education: In-person
In-person education allows for more tailored curriculum compared with telehealth, but comes with increased dissemination challenges (e-Table 5). In-person educational interventions had variable results that could not be consistently attributed to any one component. Successful interventions were delivered by a range of instructors, including community health workers,25 asthma educators,26 and peers.27 Educational interventions targeted a range of mediators of health disparities, most consistently individual factors related to knowledge and adherence,25 and societal factors by tailoring interventions to patient’s cultural backgrounds.26 Social mediators were leveraged in trials that sought to use peer instructors or group conversation.27 Interventions that involved captive audiences who had less ability to opt in (eg, school children,28 patients in the ED29) were less successful. The identified studies were a mix of prospective cohorts with moderate to high risk of bias because of selection and confounding and RCTs with variable risk of bias, often from challenges with blinding or lack of prespecified primary outcomes. Successful educational interventions take many forms, but the proportion of enrolled patients who have self-identified lack of knowledge as a barrier to their care may be an important driver of success.
Behavioral: Telehealth
Multiple telehealth interventions sought to change patient behavior through telemonitoring, treatment reminders, and counseling (e-Table 6). Treatment reminders30 and telemonitoring of compliance31 have been shown to be feasible, but sustained improvements in adherence or outcomes have yet to be demonstrated. One prospective cohort demonstrated reduced health care utilization with nurse coordinator phone calls triggered by rescue inhaler use tracked by remote monitoring.32 More work is needed to understand how to use telemonitoring and treatment reminders to improve outcomes.
Telehealth counseling interventions included higher-quality studies and were able to show improvements in outcomes. A telephone coaching program targeted for women with asthma reduced symptoms and improved quality of life.33 An internet-based program focused on improving adherence and smoking cessation improved symptoms and reduced missed school days when provided to school children.34 However, the true effect size is hard to estimate because of the identified studies having risk of bias because of variable challenges with lack of prespecified primary outcome, potential selection bias, and minimal description of blinding, despite most studies being RCTs.
Behavioral: In-person
Multiple studies investigated in-person behavioral counseling with encouraging results. In a pivotal early study, Evans et al35 demonstrated that a social worker teaching families asthma management and providing connection to community resources could increase symptom-free days (e-Table 7). This methodology of bundling education, counseling, and access to additional resources has proven effective across a range of studies, whether carried out by asthma educators,36 nurses,37 or parent mentors.38 This methodology likely finds success because of addressing the multifactorial causes of health disparities: individual factors of knowledge and motivation, social factors by connection to community resources, environmental factors by improving access to care, and societal factors by delivering an intervention which is culturally appropriate. Again, many studies were RCTs but had risk of bias from inability to blind.
Clinical Trial Enrollment
Development and validation of interventions to reduce health disparities will require effective patient recruitment techniques (e-Table 8). It is well established that non-White and low income patients are underrepresented in therapeutic trials,39 despite emerging evidence that they may be overrepresented in stage I safety trials.40 Multiple mediators of health disparities were addressed in interventions conducted across a range of pulmonary disease states to improve clinical trial enrollment: societal mediators (eg, mistrust of medical system because of past research malfeasance,41 language barriers)42 and environmental mediators (eg, transportation, challenges adhering to strict data collection schedules).43 Most frequently, these barriers were overcome using social mediators (eg, tapping into existing community networks,43 recruiting face to face with culturally competent staff).42 Intervention bundles that increase diversity in clinical trials have been described primarily in retrospective cohort studies with low to moderate risk of bias (often because of lack of comparator group); however, the impact of the individual components of these interventions is not fully understood.
Behavioral: Cleaning
The most described single intervention in our search was environmental mitigation for patients with asthma (e-Table 9). The studies identified by our search were highly heterogeneous in the allergen they aimed to reduce, the measures they used to reduce the allergen, and supplementary services offered in addition to allergen removal. Despite this, multiple studies demonstrated improvements in quality of life,44 health care utilization,45 and costs.46 Multifaceted interventions including in-home asthma education were often effective. It is unclear which components of an environmental mitigation strategy are essential, and which patients will benefit most. Detailed recommendations regarding allergen mitigation that describe study quality, acknowledge uncertainties, and describe populations that may benefit have been published.47 These recommendations serve as a model for future guidelines addressing interventions targeting health disparities by recognizing that a single intervention will not be appropriate for all patients, and tailoring to individual circumstances will be essential.
Quality and Access to Care
Provider behavior is an important intervention target given that non-White race and low socioeconomic status are associated with less guideline-based treatment in asthma,48 COPD,49 and lung cancer (e-Table 10).50 Provider educational interventions improved quality of care in asthma51 and expanded access to care for pneumoconiosis in rural populations.52 Standardization of care with paper53 or electronic medical record reminders54 improved quality of care and outcomes in asthma. Focusing on quality of care can address causes of health care disparities that are most under physician control.
In contrast to successful interventions targeting the provider, well-designed interventions focused on improving patient utilization of office visits with nurse educators55 or patient advocates56 did not improve outcomes in the two such trials identified. One study hypothesized that office visit quality would not be improved because of complex social situations (eg, homelessness).55 In qualitative interviews with patients involved in the second study, patients in both the test and control group reported improved communication with provider leading to improved adherence, suggesting the intervention may have changed provider behavior.57 This suggests that provider behavior may be a higher yield target for intervention.
Multiple studies improved outcomes with expanded access to care. Free care58 or improved access to care through care coordination59 improved outcomes in multiple studies. The intensity of programing may be important; for example, a high-quality study was unable to improve asthma control with pediatric school children with observed inhaled corticosteroid therapy, potentially because of not providing medication on weekends or holidays and high rates of school absences by the study participants.60 A wide range of study types were used, including high bias risk retrospective studies and RCTs with variable risk of bias (often because of blinding or multiple outcomes).
Policy
An essential component of tackling health care disparities is addressing the societal factors contributing to differing access to resources between groups with varying levels of socioeconomic and political power (e-Table 11). A private health care system aiming to provide equitable care still saw Black patients underusing specialists and overusing the ED compared with White patients.61 Multiple studies investigated the role of Medicaid expansion through the Affordable Care Act with variable results,62,63 perhaps because of persistent cost barriers despite Medicaid coverage.2 In contrast, equitable outcomes in lung cancer were shown in the Veterans’ health system.64 More practically for health practitioners, multiple studies described the ability of a coalition of health care providers, patients, and community representatives to increase access to care locally, and lobby for improvements to health care.65 Interventions at the level of policy are challenging to evaluate rigorously, and most of the described studies were moderate to high risk of bias retrospective cohorts and a few pre/post prospective cohorts. Although work in this area may be traditionally outside of the purview of the physician at the bedside, developing coalitions of providers, patients, and communities provides a pathway to instigate necessary change.
Conclusions
Five main themes emerged in our review.
-
•
There were few interventional trials compared with the breadth of studies describing health disparities. Trials involving patients with asthma who were Black, low income, and living in an urban setting were overrepresented.
-
•
Race or socioeconomic status was not an effective marker of individual pharmacologic treatment response.
-
•
Telehealth enabled scaling of care, but more work is needed to understand how to leverage telehealth to improve outcomes in marginalized communities.
-
•
Future interventions must explicitly target societal drivers of disparity, rather than focusing on individual behavior alone.
-
•
Individual interventions will only be maximally effective when specifically tailored to local needs.
Of the 3,480 articles screened, 2,270 articles cataloged disparities and only 130 described interventional trials. Future studies seeking to document disparity should be paired with studies to address the uncovered disparity. Despite asthma being overrepresented, intervention classes with equal representation of asthma and nonasthma pulmonary disease (pharmacologic, clinical trial recruitment, policy) demonstrated similar findings, suggesting the lessons learned in asthma may be transferable to other pulmonary diseases. The most common population targeted in the identified interventions was urban, low income, and identified as Black, often correlating with the underserved population in closest proximity to the study institution. Although tailoring was required, similar successes and hurdles were seen in interventions targeting Hispanic and rural patients. It will be important for future work to include other marginalized groups (women, immigrants, rural, LGBTQIA+, etc) to have the widest impact.
Although there are therapeutically important alleles with differential expression between racial groups, self-reported race was not effective for tailoring pharmacologic therapy in pulmonary disease. It is likely that observed racial disparities are related to external social factors rather than genetic factors, given that race is a poor marker of genetics,66 and multiple studies demonstrate racial differences are heavily influenced by social factors (eg, residential segregation,67 unequal care).68 Self-reported race has an important role in future genetic studies to ensure that study populations reflect the full range of genetic diversity, but genetically defined ancestry may be a more valid way to assess biologic contributors to disparities.
Telehealth could improve access to care and help disseminate interventions to reduce health disparity. Telehealth interventions that did not include direct interaction between the patient and a person (peer, nurse educator) were often unsuccessful. In comparison, personal interactions delivered in a telehealth format (eg, telemonitoring of inhaler compliance paired with nurse coordinator calls for noncompliance,38 culturally competent telephone counseling for Black women with asthma39) were often effective. Much work is needed to understand how to best deliver health care virtually to vulnerable populations, but the available literature suggests that a human touch is still a powerful tool.
Important progress has been made over the last 40 years. Early studies often focused on inner rings of the Whitehead model (patient knowledge or adherence), whereas recent studies were often explicit in targeting the outer rings of the Whitehead model (improving access to health care, cultural tailoring of intervention). Using the framework put forth by Thomas et al,69 this could be seen as moving from third generation interventions (addressing the individual but not the social context causing disparity) to fourth generation interventions (interventions that address the societal inequity at the root of disparity). Future interventions should be explicit in addressing not just individual but societal drivers of disparity.
Dissemination was challenging for even well-designed interventions.35,70,71 A challenge in implementation of health disparity interventions comes from the impact of unmeasured social factors (health policy, access to services, housing and food insecurity, education, etc) on intervention efficacy. Because of this, an intervention effective in a high-quality RCT could have disappointing results when applied in a different social context. Understanding which mediators of health disparities are most related to observed outcomes within a structured conceptual frame work will help investigators tailor interventions to their local communities.72
Future Directions
A key component of addressing root causes of health disparities will be robust inclusion of patients in the design, testing, and implementation of interventions. Most of the descriptive papers identified were investigator driven and did not include the patient voice, suggesting mediators of disparity important to patients may still have been missed. Although many of the earlier interventions were investigator driven, many of the more recent studies went to great lengths to include patient input. Community-based participatory research methodology could help form collaborative partnerships between health professionals, academics, and the communities they serve to tailor interventions to local barriers and strengths, to address root causes of disparity.73 Rather than focusing on consistency, a focus on flexibility and modifications to address the local barriers to care will be important for successful dissemination of health disparity interventions.
Limitations
Our review has several important limitations. We carried out a structured search restricted to PubMed and not a systematic review of the literature. However, with our described search we were able to achieve our goal of presenting a framework for physicians who are seeking to address health disparities and identify characteristics of successful studies. We focused on interventions trialed within the United States to examine interventions developed in a similar social and economic context. Although this provided consistency, we certainly missed important work done internationally that could be applied in the United States, and illuminate the impact of differing social and economic structures. Finally, although we describe in brief the quality of the studies, we did not complete a formal assessment of bias on all included studies.
Summary
There are well-documented health disparities in pulmonary disease related to factors such as race, socioeconomic status, and sex. A wide range of interventions have been trialed to address these disparities with varying results. The main driver of success is likely how well the intervention addresses the most pertinent local drivers of disparity. Future work is needed to rigorously validate interventions to reduce disparity and to understand how to tailor validated interventions to local needs to facilitate dissemination.
Funding/Support
This work was supported by the National Institutes of Health National Center for Advancing Translational Sciences [Grant UL1TR002548] and National Institute on Minority Health and Health Disparities [Grants U54MD002265, K23MD017284].
Financial/Nonfinancial Disclosures
None declared.
Acknowledgments
Author contributions: L. J. H. is the guarantor of the content of the manuscript. Articles were reviewed by L. J. H., P. K., and J. M. K. The article was drafted by L. J. H., with substantial input by P. K., J. M. K., J. D. T., S. B. K., and D. A. C.
Role of sponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Additional information: The e-Appendix, e-Figure, and e-Tables are available online under “Supplementary Data.”
Supplementary Data
References
- 1.Kunitomo Y., Bade B., Gunderson C.G., et al. Racial differences in adherence to lung cancer screening follow-up: a systematic review and meta-analysis. Chest. 2022;161(1):266–275. doi: 10.1016/j.chest.2021.07.2172. [DOI] [PubMed] [Google Scholar]
- 2.Suri R., Macinko J., Inkelas M., Needleman J. The relationship between insurance status and the Affordable Care Act on asthma outcomes among low-income US adults. Chest. 2022;16(1):1465–1474. doi: 10.1016/j.chest.2022.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harper L.J., Gerke A.K., Wang X.F., et al. Income and other contributors to poor outcomes in U.S. patients with sarcoidosis. Am J Respir Crit Care Med. 2020;201(8):955–964. doi: 10.1164/rccm.201906-1250OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Asthma and Allergy Foundation of America 2020 Asthma disparities in America: a roadmap to reducing burden on racial and ethnic minorities. https://www.aafa.org/wp-content/uploads/2022/08/asthma-disparities-in-america-burden-on-racial-ethnic-minorities.pdf
- 5.Patel M.R., Gerald J.K., Gerald L.B., et al. Improving the affordability of prescription medications for people with chronic respiratory disease. An official American Thoracic Society policy statement. Am J Respir Crit Care Med. 2018;198(11):1367–1374. doi: 10.1164/rccm.201810-1865ST. [DOI] [PubMed] [Google Scholar]
- 6.Talwar A., Garcia J.G.N., Tsai H., et al. Health disparities in patients with pulmonary arterial hypertension: a blueprint for action. An official American Thoracic Society statement. Am J Respir Crit Care Med. 2017;196(8):e32–e47. doi: 10.1164/rccm.201709-1821ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patricia Rivera M., Aldrich M.C., Henderson L.M., et al. Addressing disparities in lung cancer screening eligibility and healthcare access: an official American Thoracic Society statement. Am J Respir Crit Care Med. 2020;202(7):E95–E112. doi: 10.1164/rccm.202008-3053ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Celedón J.C., Burchard E.G., Schraufnagel D., et al. An American Thoracic Society/National Heart, Lung, and Blood Institute workshop report: addressing respiratory health equality in the United States. Ann Am Thorac Soc. 2017;14(5):814–826. doi: 10.1513/AnnalsATS.201702-167WS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dalhlgren G., Whitehead M. Policies and strategies to promote social equity in health. Background document to WHO – strategy paper for Europe. https://www.iffs.se/media/1326/20080109110739filmZ8UVQv2wQFShMRF6cuT.pdf
- 10.Reynolds C.H., Patel J.D., Garon E.B., et al. Exploratory subset analysis of African Americans from the PointBreak Study: pemetrexed-carboplatin-bevacizumab followed by maintenance pemetrexed-bevacizumab versus paclitaxel-carboplatin-bevacizumab followed by maintenance bevacizumab in patients with stage IIIB/IV nonsquamous non-small-cell lung cancer. Clin Lung Cancer. 2015;16(3):200–208. doi: 10.1016/j.cllc.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 11.Evans N., Grenda T., Alvarez N.H., Okusanya O.T. Narrative review of socioeconomic and racial disparities in the treatment of early stage lung cancer. J Thorac Dis. 2021;13(6):3758–3763. doi: 10.21037/jtd-20-3181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spector S.L., Martin U.J., Uryniak T., O’Brien C.D. Budesonide/formoterol pressurized metered-dose inhaler versus budesonide: a randomized controlled trial in black patients with asthma. J Asthma. 2012;49(1):70–77. doi: 10.3109/02770903.2011.633788. [DOI] [PubMed] [Google Scholar]
- 13.Busse W.W., Morgan W.J., Gergen P.J., et al. Randomized trial of omalizumab (anti-IgE) for asthma in inner-city children. N Engl J Med. 2011;364(11):1005–1015. doi: 10.1056/NEJMoa1009705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wechsler M.E., Szefler S.J., Ortega V.E., et al. Step-up therapy in black children and adults with poorly controlled asthma. N Engl J Med. 2019;381(13):1227–1239. doi: 10.1056/NEJMoa1905560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ortega V.E., Daya M., Szefler S.J., et al. Pharmacogenetic studies of long-acting beta agonist and inhaled corticosteroid responsiveness in randomised controlled trials of individuals of African descent with asthma. Lancet Child Adolesc Heal. 2021;5(12):862–872. doi: 10.1016/S2352-4642(21)00268-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu A.C., Glauber J., Gay C., Lieu T.A. Asthma self-assessment in a Medicaid population. BMC Public Health. 2009;9:244. doi: 10.1186/1471-2458-9-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wong-McGrath K., Denlinger L.C., Bleecker E.R., et al. Internet-based monitoring in the severe asthma research program identifies a subgroup of patients with labile asthma control. Chest. 2018;153(2):378–386. doi: 10.1016/j.chest.2017.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pasquinelli M.M., Tammemägi M.C., Kovitz K.L., et al. Risk prediction model versus United States Preventive Services Task Force lung cancer screening eligibility criteria: reducing race disparities. J Thorac Oncol. 2020;15(11):1738–1747. doi: 10.1016/j.jtho.2020.08.006. [DOI] [PubMed] [Google Scholar]
- 19.Simmerman E.L., Thomson N.B., Dillard T.A., et al. Free lung cancer screening trends toward a twofold increase in lung cancer prevalence in the underserved Southeastern United States. South Med J. 2017;110(3):188–194. doi: 10.14423/SMJ.0000000000000619. [DOI] [PubMed] [Google Scholar]
- 20.Raghavan D., Wheeler M., Doege D., et al. Initial results from mobile low-dose computerized tomographic lung cancer screening unit: improved outcomes for underserved populations. Oncologist. 2020;25(5):e777–e781. doi: 10.1634/theoncologist.2019-0802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Guendelman S., Meade K., Benson M., Chen Y.Q., Samuels S. Improving asthma outcomes and self-management behaviors of inner-city children: a randomized trial of the Health Buddy interactive device and an asthma diary. Arch Pediatr Adolesc Med. 2002;156(2):114–120. doi: 10.1001/archpedi.156.2.114. [DOI] [PubMed] [Google Scholar]
- 22.Huss K., Winkelstein M., Nanda J., Naumann P.L., Sloand E.D., Huss R.W. Computer game for inner-city children does not improve asthma outcomes. J Pediatr Heal Care. 2003;17(2):72–78. doi: 10.1067/mph.2003.28. [DOI] [PubMed] [Google Scholar]
- 23.Cardarelli R., Reese D., Roper K.L., et al. Terminate lung cancer (TLC) study—a mixed-methods population approach to increase lung cancer screening awareness and low-dose computed tomography in Eastern Kentucky. Cancer Epidemiol. 2017;46:1–8. doi: 10.1016/j.canep.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zorc J.J., Chew A., Allen J.L., Shaw K. Beliefs and barriers to follow-up after an emergency department asthma visit: a randomized trial. Pediatrics. 2009;124(4):1135–1142. doi: 10.1542/peds.2008-3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baek J., Huang K., Conner L., Tapangan N., Xu X., Carrillo G. Effects of the home-based educational intervention on health outcomes among primarily Hispanic children with asthma: a quasi-experimental study. BMC Public Health. 2019;19(1):1–8. doi: 10.1186/s12889-019-7272-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martin M.A., Pugach O., Mosnaim G., et al. Community health worker asthma interventions for children: results from a clinically integrated randomized comparative effectiveness trial (2016‒2019) Am J Public Health. 2021;111(7):1328–1337. doi: 10.2105/AJPH.2021.306272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rhee H., Belyea M.J., Hunt J.F., Brasch J. Effects of a peer-led asthma self-management program for adolescents. Arch Pediatr Adolesc Med. 2011;165(6):513–519. doi: 10.1001/archpediatrics.2011.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Clark N.M., Shah S., Dodge J.A., Thomas L.J., Andridge R.R., Little R.J. An evaluation of asthma interventions for preteen students. J Sch Heal. 2010;80(2):80–87. doi: 10.1111/j.1746-1561.2009.00469.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith S.R., Jaffe D.M., Highstein G., Fisher E.B., Trinkaus K.M., Strunk R.C. Asthma coaching in the pediatric emergency department. Acad Emerg Med. 2006;13(8):835–839. doi: 10.1197/j.aem.2006.03.565. [DOI] [PubMed] [Google Scholar]
- 30.Britto M.T., Rohan J.M., Dodds C.M., Byczkowski T.L. A randomized trial of user-controlled text messaging to improve asthma outcomes: a pilot study. Clin Pediatr (Phila) 2017;56(14):1336–1344. doi: 10.1177/0009922816684857. [DOI] [PubMed] [Google Scholar]
- 31.Otsuki M., Eakin M.N., Rand C.S., et al. Adherence feedback to improve asthma outcomes among inner-city children: a randomized trial. Pediatrics. 2009;124(6):1513–1521. doi: 10.1542/peds.2008-2961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alshabani K., Attaway A.A., Smith M.J., et al. Electronic inhaler monitoring and healthcare utilization in chronic obstructive pulmonary disease. J Telemed Telecare. 2020;26(7-8):495–503. doi: 10.1177/1357633X19850404. [DOI] [PubMed] [Google Scholar]
- 33.Clark N.M., Gong Z.M., Wang S.J., Valerio M.A., Bria W.F., Johnson T.R. From the female perspective: long-term effects on quality of life of a program for women with asthma. Gend Med. 2010;7(2):125–136. doi: 10.1016/j.genm.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Joseph C.L., Ownby D.R., Havstad S.L., et al. Evaluation of a web-based asthma management intervention program for urban teenagers: reaching the hard to reach. J Adolesc Heal. 2013;52(4):419–426. doi: 10.1016/j.jadohealth.2012.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Evans R., Gergen P.J., Mitchell H., et al. A randomized clinical trial to reduce asthma morbidity among inner-city children: results of the national cooperative inner-city asthma study. J Pediatr. 1999;135(3):332–338. doi: 10.1016/s0022-3476(99)70130-7. [DOI] [PubMed] [Google Scholar]
- 36.Walders N., Kercsmar C., Schluchter M., Redline S., Kirchner H.L., Drotar D. An interdisciplinary intervention for undertreated pediatric asthma. Chest. 2006;129(2):292–299. doi: 10.1378/chest.129.2.292. [DOI] [PubMed] [Google Scholar]
- 37.Greineder D.K., Loane K.C., Parks P. A randomized controlled trial of a pediatric asthma outreach program. J Allergy Clin Immunol. 1999;103(3 pt 1):436–440. doi: 10.1016/s0091-6749(99)70468-9. [DOI] [PubMed] [Google Scholar]
- 38.Flores G., Bridon C., Torres S., et al. Improving asthma outcomes in minority children: a randomized, controlled trial of parent mentors. Pediatrics. 2009;124(6):1522–1532. doi: 10.1542/peds.2009-0230. [DOI] [PubMed] [Google Scholar]
- 39.Loree J.M., Anand S., Dasari A., et al. Disparity of race reporting and representation in clinical trials leading to cancer drug approvals from 2008 to 2018. JAMA Oncol. 2019;5(10) doi: 10.1001/jamaoncol.2019.1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fisher J.A., Kalbaugh C.A. Challenging assumptions about minority participation in US clinical research. Am J Public Health. 2011;101(12):2217. doi: 10.2105/AJPH.2011.300279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pinsky P.F., Ford M., Gamito E., et al. Enrollment of racial and ethnic minorities in the prostate, lung, colorectal and ovarian cancer screening trial. J Natl Med Assoc. 2008;100(3):291–298. doi: 10.1016/s0027-9684(15)31241-4. [DOI] [PubMed] [Google Scholar]
- 42.Tenorio S.L., O’Donnell C.I., Hernandez J., Rozjabek H.M., Lynch D., Marcus P.M. Culturally sensitive approaches to recruitment and retention of Hispanics in the National Lung Screening Trial. J Immigr Minor Heal. 2014;16(4):761–764. doi: 10.1007/s10903-013-9862-0. [DOI] [PubMed] [Google Scholar]
- 43.Huang B., Vore D De, Chirinos C., et al. Strategies for recruitment and retention of underrepresented populations with chronic obstructive pulmonary disease for a clinical trial. BMC Med Res Methodol. 2019;19(1):39. doi: 10.1186/s12874-019-0679-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sweet L.L., Polivka B.J., Chaudry R.V., Bouton P. The impact of an urban home-based intervention program on asthma outcomes in children. Public Health Nurs. 2014;31(3):243–252. doi: 10.1111/phn.12071. [DOI] [PubMed] [Google Scholar]
- 45.Morgan W.J., Crain E.F., Gruchalla R.S., et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351(11):1068–1080. doi: 10.1056/NEJMoa032097. [DOI] [PubMed] [Google Scholar]
- 46.Campbell J.D., Brooks M., Hosokawa P., Robinson J., Song L., Krieger J. Community health worker home visits for medicaid-enrolled children with asthma: effects on asthma outcomes and costs. Am J Public Health. 2015;105(11):2366–2372. doi: 10.2105/AJPH.2015.302685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cloutier M.M., Baptist A.P., Blake K.V., et al. 2020 Focused updates to the asthma management guidelines: a report from the National Asthma Education and Prevention Program Coordinating Committee Expert Panel Working Group. J Allergy Clin Immunol. 2020;146(6):1217. doi: 10.1016/j.jaci.2020.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Riekert K.A., Butz A.M., Eggleston P.A., Huss K., Winkelstein M., Rand C.S. Caregiver-physician medication concordance and undertreatment of asthma among inner-city children. Pediatrics. 2003;111(3):e214–e220. doi: 10.1542/peds.111.3.e214. [DOI] [PubMed] [Google Scholar]
- 49.Blanc P.D., Eisner M.D., Yelin E.H., et al. Socioeconomic gradients in tiotropium use among adults with COPD. Int J Chron Obs Pulmon Dis. 2008;3(3):483–490. doi: 10.2147/copd.s3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Blom E.F., Haaf K.T., Arenberg D.A., de Koning H.J. Disparities in receiving guideline-concordant treatment for lung cancer in the United States. Ann Am Thorac Soc. 2020;17(2):186–194. doi: 10.1513/AnnalsATS.201901-094OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Evans D., Mellins R., Lobach K., et al. Improving care for minority children with asthma: professional education in public health clinics. Pediatrics. 1997;99(2):157–164. doi: 10.1542/peds.99.2.157. [DOI] [PubMed] [Google Scholar]
- 52.Sood A., Assad N., Jarrell W., et al. A virtual community-of-practice approach by rural stakeholders in managing pneumoconiosis in the USA: a cross-sectional analysis. Rural Remote Health. 2020;20(3):5784. doi: 10.22605/RRH5784. [DOI] [PubMed] [Google Scholar]
- 53.Grant R., Bowen S.K., Neidell M., Prinz T., Redlener I.E. Health care savings attributable to integrating guidelines-based asthma care in the pediatric medical home. J Health Care Poor Underserved. 2010;21(2 suppl):82–92. doi: 10.1353/hpu.0.0308. [DOI] [PubMed] [Google Scholar]
- 54.Shapiro A., Gracy D., Quinones W., Applebaum J., Sarmiento A. Putting guidelines into practice: improving documentation of pediatric asthma management using a decision-making tool. Arch Pediatr Adolesc Med. 2011;165(5):412–418. doi: 10.1001/archpediatrics.2011.49. [DOI] [PubMed] [Google Scholar]
- 55.Butz A., Kub J., Donithan M., et al. Influence of caregiver and provider communication on symptom days and medication use for inner-city children with asthma. J Asthma. 2010;47(4):478–485. doi: 10.3109/02770901003692793. [DOI] [PubMed] [Google Scholar]
- 56.Apter A.J., Perez L., Han X., et al. Patient advocates for low-income adults with moderate to severe asthma: a randomized clinical trial. J Allergy Clin Immunol Pract. 2020;8(10):3466–3473.e11. doi: 10.1016/j.jaip.2020.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Korwin A., Black H., Perez L., et al. Exploring patient engagement: a qualitative analysis of low-income urban participants in asthma research. J Allergy Clin Immunol Pract. 2017;5(6):1625–1631.e2. doi: 10.1016/j.jaip.2017.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gerald L.B., McClure L.A., Mangan J.M., et al. Increasing adherence to inhaled steroid therapy among schoolchildren: randomized, controlled trial of school-based supervised asthma therapy. Pediatrics. 2009;123(2):466–474. doi: 10.1542/peds.2008-0499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Halterman J.S., Szilagyi P.G., Fisher S.G., et al. Randomized controlled trial to improve care for urban children with asthma: results of the school-based asthma therapy trial. Arch Pediatr Adolesc Med. 2011;165(3):262–268. doi: 10.1001/archpediatrics.2011.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gerald J.K., Fisher J.M., Brown M.A., et al. School-supervised use of a once-daily inhaled corticosteroid regimen: a cluster randomized trial. J Allergy Clin Immunol. 2019;143(2):755–764. doi: 10.1016/j.jaci.2018.06.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zoratti E.M., Havstad S., Rodriguez J., Robens-Paradise Y., Lafata J.E., McCarthy B. Health service use by African Americans and Caucasians with asthma in a managed care setting. Am J Respir Crit Care Med. 1998;158(2):371–377. doi: 10.1164/ajrccm.158.2.9608039. [DOI] [PubMed] [Google Scholar]
- 62.Liu Y., Colditz G.A., Kozower B.D., et al. Association of Medicaid expansion under the patient protection and Affordable Care Act with non-small cell lung cancer survival. JAMA Oncol. 2020;6(8):1289–1290. doi: 10.1001/jamaoncol.2020.1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nguyen D.-D., Paciotti M., Marchese M., et al. Effect of Medicaid expansion on receipt of definitive treatment and time to treatment initiation by racial and ethnic minorities and at minority-serving hospitals: a patient-level and facility-level analysis of breast, colon, lung, and prostate cancer. JCO Oncol Pract. 2021;17(5):e654–e665. doi: 10.1200/OP.21.00010. [DOI] [PubMed] [Google Scholar]
- 64.Zheng L., Enewold L., Zahm S.H., et al. Lung cancer survival among black and white patients in an equal access health system. Cancer Epidemiol Biomarkers Prev. 2012;21(10):1841–1847. doi: 10.1158/1055-9965.EPI-12-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sommer S.J., Queenin L.M., Nethersole S., et al. Children’s hospital boston community asthma initiative: partnerships and outcomes advance policy change. Prog Community Heal Partnersh. 2011;5(3):327–335. doi: 10.1353/cpr.2011.0044. [DOI] [PubMed] [Google Scholar]
- 66.Tishkoff S.A., Kidd K.K. Implications of biogeography of human populations for ‘race’ and medicine. Nat Genet. 2004;36(11 suppl):S21–S27. doi: 10.1038/ng1438. [DOI] [PubMed] [Google Scholar]
- 67.Woo H., Brigham E.P., Allbright K., et al. Racial segregation and respiratory outcomes among urban black residents with and at risk of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2021;204(5):536–545. doi: 10.1164/rccm.202009-3721OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mulligan C.R., Meram A.D., Proctor C.D., Wu H., Zhu K., Marrogi A.J. Unlimited access to care: effect on racial disparity and prognostic factors in lung cancer. Cancer Epidemiol Biomarkers Prev. 2006;15(1):25–31. doi: 10.1158/1055-9965.EPI-05-0537. [DOI] [PubMed] [Google Scholar]
- 69.Thomas S.B., Quinn S.C., Butler J., Fryer C.S., Garza M.A. Toward a fourth generation of disparities research to achieve health equity. Annu Rev Public Health. 2011;32:399–416. doi: 10.1146/annurev-publhealth-031210-101136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Spiegel J., Love A.S., Wood P.R., et al. The inner-city asthma intervention: description of a community-based implementation of an evidence-based approach to asthma management. Ann Allergy Asthma Immunol. 2006;97(1 suppl 1):S6–S10. doi: 10.1016/s1081-1206(10)60778-8. [DOI] [PubMed] [Google Scholar]
- 71.Portnoy J.M., Jennings D. Utilization patterns in an asthma intervention. Ann Allergy Asthma Immunol. 2006;97(1 suppl 1):S25–S30. doi: 10.1016/s1081-1206(10)60782-x. [DOI] [PubMed] [Google Scholar]
- 72.Harper L.J., Love G., Singh R., Smith A., Culver D.A., Thornton J.D. Barriers to care among patients with sarcoidosis: a qualitative study. Ann Am Thorac Soc. 2021;18(11):1832–1838. doi: 10.1513/AnnalsATS.202011-1467OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Harris D.A., Pensa M.A., Redlich C.A., Pisani M.A., Rosenthal M.S. Community-based participatory research is needed to address pulmonary health disparities. Ann Am Thorac Soc. 2016;13(8):1231–1238. doi: 10.1513/AnnalsATS.201601-054PS. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.