Abstract
The superior lateral incisors are primarily affected by the developmental deformity known as dens invaginatus (DI). Oehler’s type III DI has the highest complexity rendering a root canal treatment (RCT) an arduous challenge for this type, so early diagnosis and treatment before pulp involvement are important. This report presents two maxillary lateral incisors with type IIIb DI, the left one being associated with a periapical lesion and the right one with normal pulp. A nine-year-old boy was referred to our clinic complaining of mobility of the maxillary left lateral incisor (LLI) associated with gumboil throughout the previous two months. Periapical radiolucency was visible on radiographs, as well as an invagination that crosses the apical foramen from the pulp chamber in both maxillary lateral incisors. The pulp of the main canal of LLI was vital and pseudo canals were necrotized and associated with chronic apical abscess. Based on the condition of the main pulp of maxillary lateral incisors, two separate treatments were carried out. RCT was done only for the pseudo canals in the LLI, while the main root canal was preserved. The right maxillary lateral incisor (RLI) had vital pulp with normal periapical tissue So the invagination was sealed as the tooth was erupting. During the one-year follow-up period, the development of the root in LLI with a thick root wall and closed apex was observed in the periapical radiograph but pseudo canals became infected and the tooth became symptomatic, therefore retreatment for pseudo canals was carried out. The RLI root was developed and the tooth was clinically asymptomatic, so it didn’t need further treatment. Maintaining pulp vitality is crucial for type III Dens invaginated young permanent teeth since it could support root formation and improve long-term prognosis, and in cases with pulp involvement, non-surgical RCT is clinically predictable.
Key Words: Cone-beam Computed Tomography, Dens Invaginatus, Endodontic Treatment, Immature Permanent Teeth, Maxillary Lateral Incisors
Introduction
Adevelopmental dental abnormality called dens invaginatus (DI) may be caused by the enamel organ folding into the tooth papilla prior to the calcification stage in tooth development [1, 2]. DI is not a common dental malformation and affects the size and shape of both the crown and root in a variety of ways[3]. The maxillary Lateral incisors are the most commonly affected teeth [4]. Although the specific cause of DI is still unknown, environmental and genetic variables such as infection, trauma, alterations in tissue pressure, or geographic variations in cellular hyperplasia seem to contribute to DI [5]. Oehler has used the degree of enamel invagination found on radiographs to classify DI into four groups [6]:
Type I: A partial invagination restricted only to the crown, leaving the cementoenamel junction (CEJ) and the pulp intact.
Type II: partial invagination exists beyond the crown and CEJ, although the pulp may be affected, the periodontal ligament (PDL) is not associated with the lesion.
Type III: A second foramen into the periodontal tissue is visible as the invagination extends apically along the root.
Type IIIa: This complete invagination penetrates the root. It communicates to the PDL via a second foramen on the tooth's lateral surface, creating a pseudo canal.
Type IIIb: This entire invagination spreads through the root and forms a pseudo canal at the apical foramen where it connects to the periodontal ligament.
Regardless of pulp vitality, a periodontal tissue inflammatory reaction brought on by an infection within the Oehler's Type III invagination may result in peri-invagination periodontitis [7]. When the invagination ends in an apical or lateral foramen of its own, it is of paramount importance to maintain the vitality of the main root canal pulp, especially in young permanent teeth with an open apex. Traditional root canal treatment (RCT) cannot completely seal the canal in open apex teeth. Moreover, the tooth becomes more susceptible to fracture because of the weak resistance and thin root canal wall [8]. Despite considering that there are several management alternatives for these situations, the goal of the treatment should be to preserve the tooth's pulp vitality for subsequent root development [9]. The advantage of vital pulp therapy (VPT) is that the root will develop and the danger of root fracture due to a thin root canal wall will be reduced even if the pulp goes through necrosis in the future and requires RCT.
This case study presents two cases of type III DI in immature permanent maxillary lateral incisors with open apex, with the left incisor being associated with peri-invagination periodontitis and the right one was vital and asymptomatic. In the left lateral incisor (LLI) treatment was limited to the invagination area. Preserving pulp vitality of the main canal helped heal the peri-invagination lesion and facilitated subsequent root development. In the right one, the invagination was sealed with composite resin, and the tooth was planned for follow-up during the eruption.
Case Presentation
A 9-year-old boy with no relevant medical history was referred to the dental clinic at Shahid Beheshti University, with the chief complaint of having big gumboil on the gingiva of the left maxillary lateral permanent incisor for the past 2 weeks (Figure 1A). There was no history of trauma. There was no abnormality on the extraoral examination. The Intra-oral examination revealed conic-shape permanent lateral incisors, without any caries, restorations, or color alteration (Figure 1A). Permanent LLI was erupting and two fluctuant swellings with one sinus tract on the attached gingiva, proximal to the coronal area between the permanent LLI and central incisors. Response to pulp sensibility tests was normal and similar to each other in both teeth. The LLI was slightly sensitive to both vertical and horizontal percussion and the depth of probing in mesiobuccal, mid-buccal, and distobuccal aspects were approximately 4 mms, with a grade 1 mobility.
Figure 1.
Preoperative photos and radiographs of the dens invaginatus in maxillary left and right lateral incisors; A) The gumboil on attached gingiva related to left lateral incisor (white arrow), the right lateral incisor was not erupted yet; B) The frontal view of CBCT showed left lateral incisor with dens in dent anomaly that associated with a peri-apical lesion (white arrow); also the right lateral incisor had this anomaly (yellow arrow)
An evaluation of the panoramic radiograph revealed the presence of DI (Figure 1B) in the LLI (Oehlers’ type IIIa) and RLI (Oehlers’ type II). The invagination extended through the root and associated with lateral radiolucent lesion around the root (Figure 1B). Cone-beam computed tomography (CBCT) (NewTom Vgi; Quantitative Radiology, Verona, Italy) was used to scan the affected tooth at 110 kVp, 100 micron voxel size, and a field of view of 6 cm×6 cm to get more precise anatomical information and a diagnosis (Figure 2A). CBCT image indicated that type IIIa invaginatus was present and showed a C-shaped orifice making 3 pseudo canals (Figure 2B); mesiobuccal (MB), mid buccal (midB) and distobuccal (DB). MB and midB canals were merging and communicating with the PDL making a second apical foramen. DB canal was a cul-de-sac. CBCT also revealed a 6.3 mm periapical radiolucency associated with the LLI which had perforated the labial cortical plate (Figure 2C). In this case, it seemed that the sinus tract of the tooth may be related to the infection of the invagination communicating with the PDL space. This assumption would relate the periapical lesion to the DI and justifies the pulp of the main canal remaining vital. To sum up, the diagnosis was DI type IIIb with partial necrotic pulp (The main canal was vital and the pseudo canals were necrotic) and chronic apical abscess related to the infected pseudo canals (MB and mid) of the LLI, with the main canal maintaining a normal pulp. Treatment options including non-surgical RCT (NSRCT) of pseudo canals+follow-up, NSRCT of main & pseudo canals+Follow Up, surgical & NSRCT+Follow Up and extraction, were described for the parents [10, 11]. Who consented to a conservative approach with the probability of further treatment becoming necessary in the future. The final treatment which was agreed upon constituted an orthograde endodontic treatment for pseudo canals+follow up for LLI and sealing the invagination with resin soon after eruption for RL.
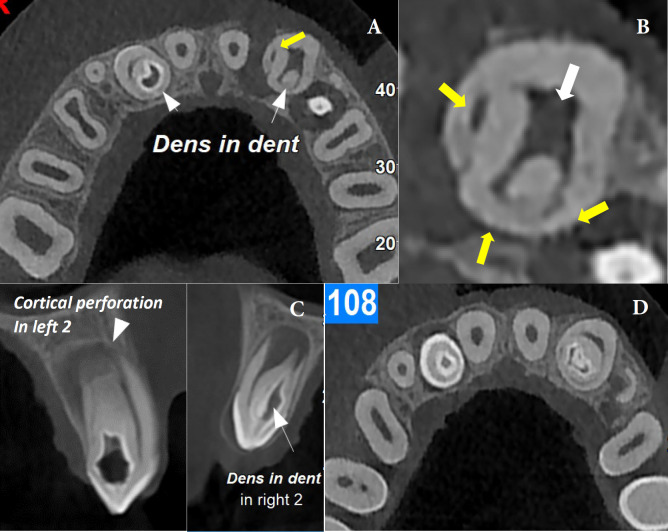
Figure 2.
A) Axial view of CBCT showed both maxillary lateral incisors with dens invaginatus (white arrows), the left lateral associated with a large lesion which perforated buccal cortical plate (yellow arrow); B) Axial view of the left lateral incisor with three pseudo canals; C) Sagittal view of the left and right lateral incisors; D) Axial view of maxillary arch
In preparation for the proposed treatment a laser soft tissue crown lengthening was planned due to the lack of tooth structure for access cavity preparation and isolation with a rubber dam [12].
The written informed consent form was signed by the patient's parent. Local anesthesia was completed with infiltration of (1.8 mL) 2% lidocaine HCL (1:80000 epinephrine; darupakhsh, Tehran, Iran) in the buccal vestibule of the LLI. The 808-nm diode soft tissue laser (Pluser; Doctor Smile, Vicenza, Italy Italy) was used to remove 2 mm of gingiva from the buccal and palatal of the tooth. The laser was operated in continuous mode for 60 sec at a 2-watt amplitude. The laser was switched to pulsing mode and 0.6-watt amplitude after being initiated. Low, brush-like movements were made using the laser [12, 13].
One week later when the first signs of coronal soft tissue healing is noticed, endodontic treatment was initiated. Local anesthesia with infiltration technique was completed with 1.8 mL of 2% lidocaine (1:80000 epinephrine, Darupakhsh, Tehran, Iran) in the buccal vestibule of the LLI tooth. A rubber dam was used, the cavity was prepared by a small round bur, and the invaginated orifice and three pseudo canals were located using a dental operating microscope (DOM) (12.5×) (Carl Zeiss, Oberkochen, Germany). An apex locator (Root ZX II, Morita, Arizona, USA) was used to measure the working length, which was confirmed by an X-ray examination. The pseudo canals were instrumented to size 50 through a crown down technique, with K-file (Mani, Tochigi, Japan) instruments and Gates Glidden drills #3 (Kerr, CA) according to Bishop’s recommendation [10].
To reinforce canal wall cleanliness after mechanical instrumentation in complex root canal system, root canals were irrigated with 1% Sodium Hypochlorite (NaOCl) [10]. The 30 gauge needle used for delivering NaOCl into the canals was side-vented and beveled and placed 3 mm short of the WL in the root [14]. The irrigation fluid wrenewed several times. Also, Passive ultrasonic irrigation (PUI) (NSK, Japan) was performed for 30 sec to improve its effectiveness.
NaOCl irrigation was followed by 5 mL ethylenediaminetetraacetic acid 17% (EDTA) (Ariadent, Tehran, Iran) to dissolve residual debris. The canals were then rinsed with 5 mL of sterile saline solution to rinse out the residual EDTA and dried by paper points. Finally, Ca (OH)2 paste was applied into the canals and the access cavity was sealed with cavity temporary restorative material (3m, USA). After one week, regression of the sinus tract and primary healing of the soft tissue was observed and the tooth became asymptomatic and the canals were dried, confirming that avoiding a root canal therapy for the main root canal and its vital pulp was indeed a correct decision as infection. The pseudo canals were obturated with MTA cement (AGM, Tehran, Iran) (Figure 3A). After the initial setting of MTA cement, the access cavity was restored using universal composite (Filtek Z250; 3M ESPE, St Paul MN, USA).
Figure 3.
Peri-apical radiographs (PA) after treatment; A) immediate after RCT of pseudo canals LLI, The main root was immature with open apex; B) 6 months after treatment, the lesion was going to be heal and main root was developed;. C-D) One year follow-up, a lesion was appeared at the apex of the main root; E) RLI was sealed with resin composite after eruption
At 6 months follow up, normal response to sensibility tests (cold, heat, electrical pulp test) was observed. Radiographic assessment revealed root formation, thickening of the root canal walls and significant osseous healing of the preoperative lesion (Figure 3B). At 12 months follow up, the LLI became slightly painful in palpation and percussion. Probing and mobility tests were within normal limits, but the tooth did not respond to sensibility tests. Radiographic evaluation showed an osseous lesion forming around the main apical foramen affirming the main canal had become necrotic after one year (Figure 3C). The diagnosis was previous endodontic treatment with an infected root canal system and secondary acute apical periodontitis. At this follow up (12 months) the RL was emerging into the oral cavity. It was responding to the sensibility tests and no abnormal evidence was noticed in radiographs.
Once the patient’s informed consent was obtained, local anesthesia was completed with infiltration of 1.8 mL of 2% lidocaine (1:80000 epinephrine, Darupakhsh, Tehran, Iran) in the buccal vestibule of the maxillary left lateral incisor. A rubber dam was applied, coronal disassembly was done. The main canal was located using DOM and previous CBCT. Since no acute symptoms had been observed, RCT was performed in a single visit. The canals were irrigated with NaOCl 5.25% activated by PUI and a final irrigation with 17% EDTA was performed for 1 min to remove Smear layers. In order to complete obturation in this session, we used calcium-enriched mixture (CEM) cement (BioniqueDent, Tehran, Iran). An apical plug of about 3 mm CEM cement was placed in the main canal and confirmed radiographically, after initial setting, the canal was obturated with thermoplastic back fill technique by Meta obtura system (Meta-Biomed _south Korea) with AH-26 sealer (Dentsply, Germany). The access cavity was sealed with glass ionomer for the tooth to be permanently restored at a later visit. Prophylactic treatment include acid-etched and flowable composite resin material (3M filtek, USA) to seal the entrance to the invagination, was done for RLI [10].
A follow-up program was set up for 6, 12, 18, and 24 months. 2 years after treatment, the teeth responded normally to palpation and percussion. Depth of probing was normal, in periapical radiography healing of the lesion of the left lateral was found (Figure 4). The RLI responded normally to sensibility tests. It had erupted completely and esthetic restoration was performed due to patient demand (Figure 4).
Figure 4.
Post-operative photo and radiographs of the dens invaginatus in maxillary left and right lateral incisors; A) esthetic treatment for LLI and RLI; B) The panoramic image showed the lesion of LLI was healed and the root of RLI was completely developed after 3 years; C) PA radiograph after retreatment of the left lateral incisor; D-E) PA radiograph and CBCT image after 3 years follow up (LLI); F-G) PA radiograph and CBCT images after 3 years follow up (RLI)
Discussion
For any endodontic treatment to be successful, thorough debridement of the infected root canal system is obligatory. In the case of a type III DI, the complex anatomy of the canals and the painstaking task to gain access to the invaginated canals [4, 15] makes a proper RCT quite the challenge to overcome. A competent endodontic treatment can avoid unneeded surgical operations and greatly increase the likelihood of a long-term favorable prognosis [16, 17]. Consequently, depending on the severity of the infection, different therapeutic modalities such as RCT, replantation, endodontic surgery, and even extraction may be considered [18].
M Forghani [19] reported a successful non-surgical RCT of type III DI with a C-shape canal in a lateral maxillary incisor. N Norouzi [20] reported a case of type III DI of maxillary central incisor that was treated with MTA. Mabrouk [21] reported a surgical endodontic treatment for a maxillary canine with type II of DI and open apex.
According to the American Academy of Oral and Maxillofacial Radiology (AAOMR) and the American Association of Endodontists (AAE) Joint Position Statement, for the diagnosis and treatment planning of teeth with these developmental anomalies, CBCT with limited fields of view is advised as an adjunctive technique, especially for pediatric patients [22, 23].
It's crucial to accurately assess the main pulp's condition for treatment planning. If the main pulp is intact, treating the infected invaginated canal alone will probably be sufficient to keep the main pulp vital [24], especially in immature cases to let complete the root maturation. Apexification and regenerative endodontic therapy for the main canal are advised when the tooth is immature and the pulp is necrotic [25]. Alani [1] recommended that when the pulp of the main canal is vital and there is peri-invagination periodontitis, the pulp vitality should be preserved. Lee [9] reported a mandibular left central incisor with type III DI and peri-invagination periodontitis, in which only the invagination was treated.
In order to clean this complicated root canal system, the use of adjunctive irrigation is suggested. Some areas may not be completely accessible by instruments, so it is required to employ copious NaOCl irrigation along with an ultrasonic-activated device [26, 27].
When root canal preparation has been completed, gutta-percha can typically be used for obturation. However, because of their high sealing ability and improved adaptability, bioceramics are occasionally a preferred option when the apical morphology of the root canal is complex [9, 10]. In the case presented here, the RLI was vital, hence we prevent pulp involvement by sealing the invagination area. This allows the tooth to remain vital and root development to proceed as planned.
In this case report, a type IIIa DI with a periapical lesion in an immature permanent lateral incisor of the maxilla was described. To ensure the root will continue to mature it was crucial to keep the pulp vital. The distinction between the canals related to the invagination and the main root canal was made with the help of CBCT, so those canals were treated first. Preservation of the main root pulp would lead to the natural closing of the apex and thickening of the root’s thin walls. During the first year of follow-up, the root of LLI became necrotic, and was treated by non-surgical RCT. After 2 years of follow-up, radiographic examination revealed bone neoformation that indicated healing had occurred.
Conclusions
This case report demonstrated a complicated root canal treatment with communication between two abnormal pulp chambers and root canals due to the occurrence of gemination. Thus, endodontic treatment was performed on both parts of the tooth. Successful treatment of teeth with unusual anatomy requires adherence to biomechanical principles of canal preparation and coronal restoration.
Conflict of Interest:
‘None declared’.
References
- 1.Alani A, Bishop K. Dens invaginatus Part 1: classification, prevalence and aetiology. Int Endod J. 2008;41(12):1123–36. doi: 10.1111/j.1365-2591.2008.01468.x. [DOI] [PubMed] [Google Scholar]
- 2.Hülsmann M. Dens invaginatus: aetiology, classification, prevalence, diagnosis, and treatment considerations. Int Endod J. 1997;30(2):79–90. doi: 10.1046/j.1365-2591.1997.00065.x. [DOI] [PubMed] [Google Scholar]
- 3.Monteiro-Jardel CC, Alves FR. Type III dens invaginatus in a mandibular incisor: a case report of a conventional endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111(4):e29–32. doi: 10.1016/j.tripleo.2010.11.023. [DOI] [PubMed] [Google Scholar]
- 4.Zhang P, Wei X. Combined Therapy for a Rare Case of Type III Dens Invaginatus in a Mandibular Central Incisor with a Periapical Lesion: A Case Report. J Endod. 2017;43(8):1378–82. doi: 10.1016/j.joen.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Zhu J, Wang X, Fang Y, Von den Hoff JW, Meng L. An update on the diagnosis and treatment of dens invaginatus. Aust Dent J. 2017;62(3):261–75. doi: 10.1111/adj.12513. [DOI] [PubMed] [Google Scholar]
- 6.Oehlers FA. Dens invaginatus (dilated composite odontome) I Variations of the invagination process and associated anterior crown forms. Oral Surg Oral Med Oral Pathol. 1957;10(11):1204–18 contd. doi: 10.1016/0030-4220(57)90077-4. [DOI] [PubMed] [Google Scholar]
- 7.Keleş A, Cakici F. Endodontic treatment of a maxillary lateral incisor with vital pulp, periradicular lesion and type III dens invaginatus: a case report. Int Endod J. 2010;43(7):608–14. doi: 10.1111/j.1365-2591.2010.01736.x. [DOI] [PubMed] [Google Scholar]
- 8.Ok E, Altunsoy M, Tanriver M, Capar ID, Kalkan A, Gok T. Fracture resistance of simulated immature teeth after apexification with calcium silicate-based materials. Eur J Dent. 2016;10(2):188–92. doi: 10.4103/1305-7456.178301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee JK, Hwang JJ, Kim HC. Treatment of peri-invagination lesion and vitality preservation in an immature type III dens invaginatus: a case report. BMC Oral Health. 2020;20(1):29. doi: 10.1186/s12903-020-1008-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bishop K, Alani A. Dens invaginatus Part 2: clinical, radiographic features and management options. Int Endod J. 2008;41(12):1137–54. doi: 10.1111/j.1365-2591.2008.01469.x. [DOI] [PubMed] [Google Scholar]
- 11.Oliveira Fonseca F, Canal Vasconcellos B, Martins Costa M, Ribeiro Sobrinho AP, Fonseca Tavares WL. Combined Endodontic and Surgical Therapy for Resolution of Type III Dens Invaginatus. Iran Endod J. 2020;15(2):117–23. doi: 10.22037/iej.v15i2.26882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boj JR, Poirier C, Hernandez M, Espassa E, Espanya A. Case series: laser treatments for soft tissue problems in children. Eur Arch Paediatr Dent. 2011;12(2):113–7. doi: 10.1007/BF03262790. [DOI] [PubMed] [Google Scholar]
- 13.Goldstep F. Diode Lasers for Periodontal Treatment: The Story So Far. Oral health. 2009:44–6. [Google Scholar]
- 14.Boutsioukis C, Psimma Z, van der Sluis LW. Factors affecting irrigant extrusion during root canal irrigation: a systematic review. Int Endod J. 2013;46(7):599–618. doi: 10.1111/iej.12038. [DOI] [PubMed] [Google Scholar]
- 15.Abazarpour R, Parirokh M, Farhadi A, Jalali Z, Kheirabadi N. Successful ultra-conservative management of a mandibular premolar with dens invaginatus. Iran Endod J. 2017;12(3):390–5. doi: 10.22037/iej.v12i3.16559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Oliveira NG, da Silveira MT, Batista SM, Veloso SRM, Carvalho MV, Travassos RMC. Endodontic Treatment of Complex Dens Invaginatus Teeth with Long Term Follow-Up Periods. Iran Endod J. 2018;13(2):263–6. doi: 10.22037/iej.v13i2.19302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moazami F, Sobhnamayan F, Malekzadeh P, Naseri M. Nonsurgical Treatment of Unusual Dens Invaginatus with MTA Based Filler in Immature Maxillary Lateral Incisor: A Case Report. Iran Endod J. 2021;16(1):60–4. doi: 10.22037/iej.v16i1.30581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Steffen H, Splieth C. Conventional treatment of dens invaginatus in maxillary lateral incisor with sinus tract: one year follow-up. J Endod. 2005;31(2):130–3. doi: 10.1097/01.don.0000137637.94281.82. [DOI] [PubMed] [Google Scholar]
- 19.Forghani M, Moghim Farooji E, Abuchenari J, Bidar M, Eslami N. Conservative Treatment of an Invaginated Maxillary Lateral Incisor with a C-shaped Canal Using Cone-Beam Computed Tomography. Iran Endod J. 2015;10(4):281–3. doi: 10.7508/iej.2015.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Norouzi N, Kazem M, Gohari A. Nonsurgical Management of an Immature Maxillary Central Incisor with Type III Dens Invaginatus Using MTA Plug: A Case Report. Iran Endod J. 2017;12(4):521–6. doi: 10.22037/iej.v12i4.17769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aguir Mabrouk N. Successful management of a type II Dens invaginatus with an open apex and a large periapical lesion A case report of a permanent maxillary canine Dent Oral Craniofac Res, 2018, Volume 4(6): 1-5. Dental, Oral and Craniofacial Research. 2018;4(6):1–5. [Google Scholar]
- 22.AAE and AAOMR Joint Position Statement: Use of Cone Beam Computed Tomography in Endodontics 2015 Update. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120(4):508–12. doi: 10.1016/j.oooo.2015.07.033. [DOI] [PubMed] [Google Scholar]
- 23.Bahmani M, Adl A, Javanmardi S, Naghizadeh S. Diagnosis and Treatment of a Type III Dens Invagination Using Cone-Beam Computed Tomography. Iran Endod J. 2016;11(4):341–6. doi: 10.22037/iej.2016.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heydari A, Rahmani M. Treatment of Dens Invagination in a Maxillary Lateral Incisor: A Case Report. Iran Endod J. 2015;10(3):207–9. doi: 10.7508/iej.2015.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Agrawal PK, Wankhade J, Warhadpande M. A Rare Case of Type III Dens Invaginatus in a Mandibular Second Premolar and Its Nonsurgical Endodontic Management by Using Cone-beam Computed Tomography: A Case Report. J Endod. 2016;42(4):669–72. doi: 10.1016/j.joen.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 26.Kato H. Non-surgical endodontic treatment for dens invaginatus type III using cone beam computed tomography and dental operating microscope: a case report. Bull Tokyo Dent Coll. 2013;54(2):103–8. doi: 10.2209/tdcpublication.54.103. [DOI] [PubMed] [Google Scholar]
- 27.Afkar M, Gholamshahi M, Mohammadi M. Nonsurgical Treatment of Type II Dens Invaginatus in a Maxillary Lateral Incisor Using Cone-Beam Computed Tomography. Iran Endod J. 2018;13(1):132–4. doi: 10.22037/iej.v13i1.19091. [DOI] [PMC free article] [PubMed] [Google Scholar]