Abstract
The incidence and prevalence of end-stage kidney disease (ESKD) in Korea are increasing, and ESKD constitutes a very important medical and social issue. Elderly dialysis patients have the highest risk of early mortality within 3 months after initiating dialysis, and geriatric syndromes such as aging, frailty, functional impairment, and cognitive impairment are crucial for the prognosis of elderly patients. Shared decision-making (SDM) is an approach through which clinicians and patients can achieve informed preferences, thereby yielding better clinical outcomes and quality of life. Through SDM-based, close consultation among patients, families, and healthcare providers, an ESKD Life-Plan for elderly patients should be established. A multidisciplinary approach led by nephrologists can help them to provide proper vascular access for dialysis at the right time, with the right evidence, and to the right patient. Strategies that can improve peritoneal dialysis in elderly patients include assisted peritoneal dialysis, homecare support programs, and automated peritoneal dialysis. In order to enhance the role of kidney transplantation in elderly patients with ESKD, it is necessary to accurately identify patients’ clinical conditions before transplantation and to perform active rehabilitation activities and postoperative management to promote recovery after transplantation. With the aging population and the increase in ESKD in the elderly, clinicians must identify factors affecting the mortality and quality of life of elderly dialysis patients.
Keywords: Elderly, Renal replacement therapy, Hemodialysis, Peritoneal dialysis, Kidney transplantation, End-Stage Kidney Disease Life-Plan, Shared decision making
1. Current status of elderly ESKD
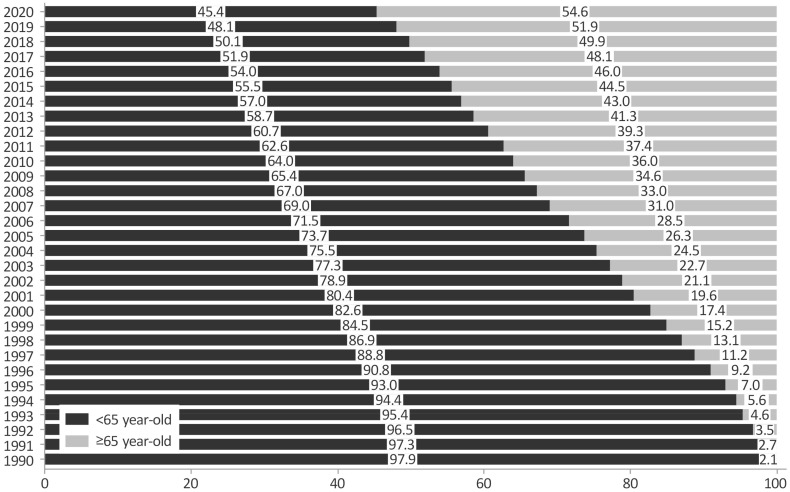
The increasing prevalence of diabetes and hypertension, in combination with population aging, has led to a drastic increase in end-stage kidney disease (ESKD). The prevalence of chronic kidney disease is 8%-11% worldwide and 10.8% in South Korea1). According to the 2020 United States Renal Data System, during 2008-2018, the prevalence of ESKD steadily increased among people aged 65 years or older2). South Korea is the country with the fourth highest ESKD prevalence rate in Asia after Taiwan, Japan, and Singapore. In 2020, the Korean Society of Nephrology reported that the prevalence of ESKD continues to increase and that the elderly (aged 65 years or older) account for 54.6% of these patients (Fig. 1). 1 The mean age of dialysis patients is 65.9 years in 2019, and the mean age of hemodialysis patients (60.5±15.0 years old) is higher than that of peritoneal dialysis patients (56.0±14.8 years old)1).
Fig. 1. The prevalence of ESKD among people aged 65 years or older in South Korea was 54.6% in 2020 and has steadily increased since the 1990s. X-axis, age; Y-axis, year (adopted from KORDS, 2020). Abbreviations: KORDS, Korean Renal Data System.
2. Considerations for dialysis in elderly patients with ESKD
All dialysis patients have the highest early mortality rate within 3 months of initiating dialysis, and elderly patients have a higher early mortality rate than others3). Geriatric syndromes such as aging, frailty, functional impairment, and cognitive impairment play a crucial role in the prognosis of elderly hemodialysis patients4,5). In addition, predicting the prognosis and likelihood of early death before and during dialysis is helpful for determining whether to perform dialysis in elderly patients. In 2018, the Act on Hospice and Palliative Care and Decisions on Life-Sustaining Treatment for Patients at the End of Life (hereinafter referred to as the Act on Decisions on Life-Sustaining Treatment) included hemodialysis as a life-sustaining treatment. Most nephrologists also have positive opinions about withholding or withdrawing dialysis of patients in end-of-life or dying process according to the Act on Decisions on Life-Sustaining Treatment and are trying to establish and apply appropriate guidelines6).
3. Choice of renal replacement therapy for elderly patients with ESKD through shared decision-making
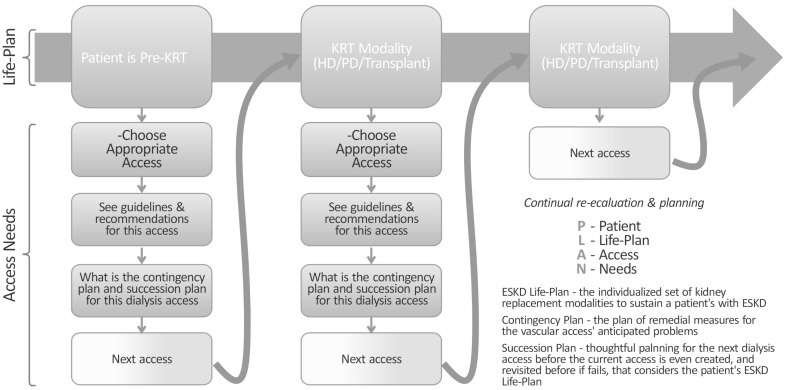
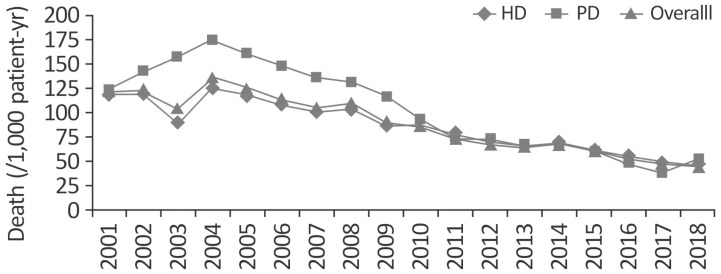
The first problem that elderly patients with ESKD encounter is deciding whether to undergo renal replacement therapy7). According to the End Stage Kidney Disease Life-Plan (ESKD Life-Plan) provision in the 2019 K/DOQI guidelines, it is necessary to establish an individualized plan considering patients’ conditions, medical/living environment, and preferences (Fig. 2.). Patients who choose conservative treatment require treatment of comorbidities, symptom control, and psychological support8). In addition, in 2020, the Korean Society of Nephrology reported that Since 2010, the mortality gap between peritoneal dialysis and hemodialysis has gradually narrowed (Fig. 3)9) in patients aged 65 years or older1). Therefore, the choice of a dialysis method according to patients’ characteristics and preferences became more important than the mortality rate10). Shared decision-making (SDM) has been defined as “an approach where clinicians and patients share the best available evidence when faced with the task of making decisions, and where patients are supported to consider options, to achieve informed preferences11)”. Increasingly many older patients face the need to decide between conservative care and dialysis as a treatment plan for advanced chronic kidney disease. SDM is recommended for preference-sensitive decisions of this type12). Although there is debate regarding the survival rate after dialysis, a study reported that the 1-year survival rate increased when dialysis was performed in patients aged 80 years or older5). Moreover, elderly patients aged 75 years or older were satisfied with life after dialysis and adapted better to dialysis than younger people13). Furthermore, a substantial majority of elderly patients aged 80 years or older who were undergoing dialysis recommended dialysis to others, with only 12.5% of them recommending against dialysis14). In order to apply the concept of the ESKD Life-Plan to elderly patients with ESKD, SDM with close consultation between patients, families, and healthcare providers is required.
Fig. 2. ESKD Life-Plan and Associated Access Needs: What’s the PLAN? (modified from the Figure 1.1 of 2019 K/DOQI guidelines Abbreviations: HD, hemodialysis: PD, peritoneal dialysis, KRT, kidney replacement therapy.
Fig. 3. Mortality rate for dialysis patients in Korea. In 2018, the unadjusted mortality rate for dialysis patients was 45.18 per 1,000 patient-years, and mortality rates by dialysis modality were 45.10 for HD patients and 51.33 for PD patients per 1,000 patient-years. (adopted from KORDS, 2020) Abbreviations: HD, hemodialysis: PD, peritoneal dialysis, KORDS, Korean Renal Data System.
1) Conservative treatment
Since the implementation of the Act on Decisions on Life-Sustaining Treatment, the number of registrants among people in their 70s has increased. Clinicians could consider conservative treatment for patients who are >75 years old, those with extensive comorbidities, or those who have poor functional status, because non-conservative treatment results in little survival benefit for these populations15). Although there is little consensus on conservative treatment for ESKD, this concept includes not performing renal replacement therapy in a clinical situation where renal replacement therapy would otherwise be initiated, as well as interventions to delay the progression of kidney disease, reduce complications to the extent possible, and facilitate in-depth communication. These interventions include medications to correct anemia and alleviate symptoms, consultations, blood tests, advance care planning, and psychological, environmental, and familial support15,16). Dialysis is a life-sustaining treatment17) and can be withdrawn among patients in the end-of-life or dying process. However, dialysis for elderly patients is distinctive from other life-sustaining treatments due to a lack of consensus regarding whether dialysis itself is categorized as an end-of-life care, the meaning of maintenance dialysis, and whether dialysis is helpful for the survival rate or quality of life of elderly patients8). The consideration of symptoms, quality of life, hospital-free days, and cost-effectiveness is sometimes more important for patients and families than survival gain. Meanwhile, patient-centered and holistic care can be maximized by providing comprehensive conservative care and basing interventions on existing evidence regarding survival, symptoms, quality of life, and experiences15). Before starting renal replacement therapy, careful consideration should be given to ensuring that patients understand the prognosis and the potential benefits and harms of therapy, as well as patients’ values, goals, and preferences18). Since patients and their family members decide whether to undergo dialysis without previously experiencing it, careful SDM with healthcare providers is needed5,10). Moreover, using a standard definition of conservative care will help clinicians to understand conservative care and select it when appropriate for their elderly patients18).
2) Hemodialysis
Most elderly patients with ESKD choose hemodialysis3,19,20,21,22). The formation, maturation, and maintenance of well-functioning vascular access, such as an arteriovenous fistula or arteriovenous graft, are very important in hemodialysis for elderly patients. Since, in particular, dialysis with a catheter can cause higher cardiovascular, infectious, or all-cause mortality in elderly patients, planned surgery for vascular access is essential as the best method that can optimize the success rate and maintain stable survival8). Several clinical practice guidelines recommend an arteriovenous fistula over an arteriovenous graft. However, it is unclear whether this recommendation must be applied to elderly patients because of the need to consider urgent hemodialysis, the life expectancy, and the maturation time of arteriovenous fistula in elderly patients23). Therefore, elderly patients with ESKD who should receive renal replacement therapy according to the new K/DOQI guidelines should also make short- and long-term life-plans and prepare vascular access accordingly8). A carefully prepared vascular access for dialysis should undergo minimal intervention for its maturation and maintenance. If dialysis is performed with a central venous catheter, the infection risk must be minimized. Considerations for vascular access include life expectancy and prognosis, patients’ health conditions, patients’ preferences, vascular condition, possibility of maturation of arteriovenous fistula, the possibility of continuing interventions, and quality of life of patients and families. Ultimately, in an ESKD Life-Plan, individualized vascular access should be planned according to the individual patient’s needs24,25). Furthermore, it is important for healthcare providers to prepare vascular access at the right time and initiate and perform stable dialysis that can improve the survival rate and quality of life of elderly patients. This choice should be made through SDM, with appropriate consideration of the characteristics of the elderly, the speed of progression to ESKD, surgical problems, the policies of dialysis institutions, and the type of dialysis that family members want4,8,23,26). Moreover, The 2019 KDOQI guidelines recommend that nephrologists have extensive experience and insight in coordinating and integrating multidisciplinary vascular access teams based on the patient’s ESKD Life-Plan17).
3) Peritoneal dialysis
According to the Korean Society of Nephrology report in 2020, the number of peritoneal dialysis patients, unlike that of hemodialysis patients, continues to decrease (prevalence of peritoneal dialysis, 2015, 6%; 2016, 5%; 2017 onwards, 4%)1). This trend is thought to be affected by autonomy, comorbidities, and the performance status of elderly patients with ESKD, as well as economic issues, the level of resource utilization, cultural issues, patients’ preferences, late referrals to nephrology, educational level, sex, living alone, and age27,28). The peritoneum does not significantly change due to aging, but in elderly individuals, changes in peritoneal mesothelial cells may occur and they may be vulnerable to inflammation. Diverticulosis, intestinal obstruction, and constipation are common in the elderly, and these conditions can affect the physiology of the peritoneum and worsen the function of a peritoneal catheter. In addition, patients with a history of abdominal surgery are at an elevated risk of adhesions and abdominal wall leaks27). Because most elderly patients with ESKD are immobile due to malnutrition or frailty and have a high risk of cardiovascular disease due to underlying diseases such as hypertension and diabetes, peritoneal dialysis as a maintenance dialysis method for elderly patients with ESKD can be used appropriately.
Therefore, peritoneal dialysis should not be determined according to the physician’s preference, and healthcare providers should provide proper and individualized information so that patients make an unbiased decision28). In addition, when chronic kidney disease has progressed to a severe degree, timely dialysis education is also important because cognitive impairment or uremia can prevent patients from being able to make an appropriate choice. Although the prevalence of peritoneal dialysis is decreasing and its survival rate is slightly less favorable than that of hemodialysis, peritoneal dialysis nevertheless has advantages that distinguish it from hemodialysis. The following considerations shed light on cases where it may be preferable to perform peritoneal dialysis in elderly patients. First, if peritoneal dialysis is used as emergency dialysis29), maintenance peritoneal dialysis becomes more likely. Second, assisted peritoneal dialysis, homecare support programs, and automated peritoneal dialysis can be used30). Third, in the US and Europe, insurance fees for peritoneal dialysis are cheaper than those for hemodialysis. If a separate healthcare delivery system and fee system are applied to peritoneal dialysis, the frequency of peritoneal dialysis may increase. Finally, it is important to decide whether to perform peritoneal dialysis on an individualized basis, considering elderly patients’ conditions31).
4) Kidney transplantation
Kidney transplantation is known as the best treatment for ESKD, with advantages including a prolonged life expectancy, improved quality of life, and reduced opportunity cost compared to dialysis treatment32). According to the Korean Society of Nephrology report in 2020, the number of patients undergoing transplantation due to ESKD reached 21,153 in South Korea. In particular, the proportion of elderly kidney transplant recipients (aged 60 years or older) increased from 7.4% in 2008 to 18.4% in 2016. According to the Korea Organ Transplantation Registry data from the Korean Society for Transplantation, the 1-year and 5-year patient and allograft survival rates in kidney transplant recipients over the age of 60 were 96.5% 90.4%, 94.8%, and 85.5%, respectively. Due to population aging, the donors and recipients of living donor kidney transplantation are also gradually becoming older. Due to the lack of donor kidneys in deceased donors, the number of patients on the waiting list for brain death donors is rapidly increasing and the waiting period is becoming longer, resulting in an increase in the recipients’ ages1).
Since elderly patients with ESKD have several conditions, such as malnutrition, chronic inflammation, chronic kidney disease - mineral bone disease, and vascular calcification, before transplantation, their circumstances should be considered when determining kidney transplantation. After transplantation, precautions are necessary to minimize the following problems: decreased muscle mass, bone density, and muscle strength in the upper and lower limbs; increased fatigue; a reduced ability to engage in aerobic activities; malnutrition; sarcopenia; cardiopulmonary dysfunction; and frailty33,34). Both dialysis recipients themselves and healthcare providers should solve social adaptation issues after transplantation through active rehabilitation activities for symptoms occurring post-transplantation32,35,36,37). For this, it is necessary for healthcare providers to accurately identify the clinical conditions of elderly patients before transplantation, continue active rehabilitation activities and postoperative management to promote the patients’ recovery, and control medications and monitor clinical conditions after discharge34,35,36,37,38).
Conclusion
With the aging population and the increase in ESKD in the elderly, clinicians must identify factors affecting the mortality and quality of life of elderly dialysis patients, and through SDM based on close consultation between patients, families, and medical staff, an ESKD Life-Plan should be established.
Acknowledgement
This research was supported by a grant from the National Research Foundation of Korea (grant number: NRF-2021R1I1A3057140).
References
- 1.Trends in epidemiologic characteristics of end-stage renal disease from 2020 KORDS (Korean Renal Data System) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.2020 Annual Data Report, USRDS. [Google Scholar]
- 3.Zhao X, Wang M, Zuo L. Early mortality risk in incident Chinese hemodialysis patients: a retrospective cohort study. Ren Fail. 2017;39(1):526–532. doi: 10.1080/0886022X.2017.1337583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Canaud B, Tong L, Tentori F, et al. Clinical practices and outcomes in elderly hemodialysis patients: results from the Dialysis Outcomes and Practice Patterns Study (DOPPS) Clin J Am Soc Nephrol. 2011;6(7):1651–1662. doi: 10.2215/CJN.03530410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jassal SV, Watson D. Dialysis in late life: benefit or burden. Clin J Am Soc Nephrol. 2009;4(12):2008–2012. doi: 10.2215/CJN.04610709. [DOI] [PubMed] [Google Scholar]
- 6.Hong YA, Chung S, Park WY, et al. Nephrologists' Perspectives on Decision Making About Life-Sustaining Treatment and Palliative Care at End of Life: A Questionnaire Survey in Korea. J Palliat Med. 2021;24(4):527–535. doi: 10.1089/jpm.2020.0248. [DOI] [PubMed] [Google Scholar]
- 7.Berger JR, Hedayati SS. Renal replacement therapy in the elderly population. Clin J Am Soc Nephrol. 2012;7(6):1039–1046. doi: 10.2215/CJN.10411011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lok CE, Huber TS, Lee T, et al. KDOQI clinical practice guideline for vascular access: 2019 update. Am J Kidney Dis. 2020;75(4):S1–S164. doi: 10.1053/j.ajkd.2019.12.001. [DOI] [PubMed] [Google Scholar]
- 9.Hong YA, Ban TH, Kang C-Y, et al. Trends in epidemiologic characteristics of end-stage renal disease from 2019 Korean Renal Data System (KORDS) Kidney Res Clin Pract. 2021;40(1):52. doi: 10.23876/j.krcp.20.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Song Y-H, Cai G-Y, Xiao Y-F, Chen X-M. Risk factors for mortality in elderly haemodialysis patients: a systematic review and meta-analysis. BMC Nephrol. 2020;21(1):1–10. doi: 10.1186/s12882-020-02026-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27(10):1361–1367. doi: 10.1007/s11606-012-2077-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Verberne WR, Stiggelbout AM, Bos WJW, van Delden JJ. Asking the right questions: towards a person-centered conception of shared decision-making regarding treatment of advanced chronic kidney disease in older patients. BMC Med Ethics. 2022;23(1):1–8. doi: 10.1186/s12910-022-00784-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lamping DL, Constantinovici N, Roderick P, et al. Clinical outcomes, quality of life, and costs in the North Thames Dialysis Study of elderly people on dialysis: a prospective cohort study. The Lancet. 2000;356(9241):1543–1550. doi: 10.1016/S0140-6736(00)03123-8. [DOI] [PubMed] [Google Scholar]
- 14.Buemi M, Lacquaniti A, Bolignano D, et al. Dialysis and the elderly: an underestimated problem. Kidney Blood Press Res. 2008;31(5):330–336. doi: 10.1159/000164277. [DOI] [PubMed] [Google Scholar]
- 15.Murtagh FE, Burns A, Moranne O, Morton RL, Naicker S. Supportive care: comprehensive conservative care in end-stage kidney disease. Clin J Am Soc Nephrol. 2016;11(10):1909–1914. doi: 10.2215/CJN.04840516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Okamoto I, Tonkin-Crine S, Rayner H, et al. Conservative care for ESRD in the United Kingdom: a national survey. Clin J Am Soc Nephrol. 2015;10(1):120–126. doi: 10.2215/CJN.05000514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee HS, Kim SG. A Korean perspective on the 2019 Kidney Disease Outcomes Quality Initiative guidelines for vascular access: what has changed and what should be changed in practice? Kidney Res Clin Pract. 2021;40(1):29. doi: 10.23876/j.krcp.20.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams AW, Dwyer AC, Eddy AA, et al. Critical and honest conversations: the evidence behind the “Choosing Wisely” campaign recommendations by the American Society of Nephrology. Clin J Am Soc Nephrol. 2012;7(10):1664–1672. doi: 10.2215/CJN.04970512. [DOI] [PubMed] [Google Scholar]
- 19.Han SS, Park JY, Kang S, et al. Dialysis modality and mortality in the elderly: a meta-analysis. Clin J Am Soc Nephrol. 2015;10(6):983–993. doi: 10.2215/CJN.05160514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park JY, Yoo KD, Kim YC, et al. Early dialysis initiation does not improve clinical outcomes in elderly end-stage renal disease patients: a multicenter prospective cohort study. PloS One. 2017;12(4):e0175830. doi: 10.1371/journal.pone.0175830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim H, An JN, Kim DK, et al. Elderly peritoneal dialysis compared with elderly hemodialysis patients and younger peritoneal dialysis patients: Competing risk analysis of a Korean prospective cohort study. PLoS One. 2015;10(6):e0131393. doi: 10.1371/journal.pone.0131393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brown EA, Finkelstein FO, Iyasere OU, Kliger AS. Peritoneal or hemodialysis for the frail elderly patient, the choice of 2 evils? Kidney Int. 2017;91(2):294–303. doi: 10.1016/j.kint.2016.08.026. [DOI] [PubMed] [Google Scholar]
- 23.Liu P, Pang SC, Li H, et al. Outcomes of arteriovenous fistula in elderly patients on maintenance haemodialysis. Int Urol Nephrol. 2021;53(9):1923–1931. doi: 10.1007/s11255-021-02822-w. [DOI] [PubMed] [Google Scholar]
- 24.Shah S, Chan MR, Lee T. Perspectives in Individualizing Solutions for Dialysis Access. Adv Chronic Kidney Dis. 2020;27(3):183–190. doi: 10.1053/j.ackd.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vachharajani TJ, Moist LM, Glickman MH, et al. Elderly patients with CKD-dilemmas in dialysis therapy and vascular access. Nat Rev Nephrol. 2014;10(2):116–122. doi: 10.1038/nrneph.2013.256. [DOI] [PubMed] [Google Scholar]
- 26.Qian JZ, McAdams-DeMarco M, Ng DK, Lau B. Arteriovenous fistula placement, maturation, and patency loss in older patients initiating hemodialysis. Am J Kidney Dis. 2020;76(4):480–489.e481. doi: 10.1053/j.ajkd.2020.02.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brown E. Peritoneal dialysis for older people: overcoming the barriers. Kidney Int. 2008;73:S68–S71. doi: 10.1038/sj.ki.5002604. [DOI] [PubMed] [Google Scholar]
- 28.Wright S, Danziger J. Peritoneal Dialysis in Elderly Patients. Am Soc Nephrol. 2009 [Google Scholar]
- 29.Arramreddy R, Zheng S, Saxena AB, Liebman SE, Wong L. Urgent-start peritoneal dialysis: a chance for a new beginning. Am J Kidney Dis. 2014;63(3):390–395. doi: 10.1053/j.ajkd.2013.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oliver M-J, Quinn R, Richardson E-P, Kiss A-J, Lamping D-L, Manns B-J. Home care assistance and the utilization of peritoneal dialysis. Kidney Int. 2007;71(7):673–678. doi: 10.1038/sj.ki.5002107. [DOI] [PubMed] [Google Scholar]
- 31.Figueiredo AE, Bernardini J, Bowes E, et al. A syllabus for teaching peritoneal dialysis to patients and caregivers. Perit Dial Int. 2016;36(6):592–605. doi: 10.3747/pdi.2015.00277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dreyer GJ, De Fijter JW. Transplanting the elderly: mandatory age-and minimal histocompatibility matching. Front Immunol. 2020;11:359. doi: 10.3389/fimmu.2020.00359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ozkayar N, Altun B, Halil M, et al. Evaluation of sarcopenia in renal transplant recipients. Nephrourol Mon. 2014;6(4):e20055. doi: 10.5812/numonthly.20055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.So S, Au EH, Lim WH, Lee VW, Wong G. Factors Influencing Long-Term Patient and Allograft Outcomes in Elderly Kidney Transplant Recipients. Kidney Int Rep. 2021;6(3):727–736. doi: 10.1016/j.ekir.2020.11.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lehner L, Staeck O, Halleck F, Liefeldt L, Bamoulid J, Budde K. Need for optimized immunosuppression in elderly kidney transplant recipients. Transplant Rev. 2015;29(4):237–239. doi: 10.1016/j.trre.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 36.Korabiewska L, Lewandowska M, Juskowa J, Białoszewski D. Need for rehabilitation in renal replacement therapy involving allogeneic kidney transplantation. Transplant Proc. 2007:2776–2777. doi: 10.1016/j.transproceed.2007.08.082. Elsevier. [DOI] [PubMed] [Google Scholar]
- 37.Cho W, Kim H, Park U, et al. Rehabilitation of transplantee and Transplant Games. J Korean S Transplant. 2017;31(1):6–15. [Google Scholar]
- 38.Messias AA, Reichelt AJ, Dos Santos EF, et al. Return to work after renal transplantation: a study of the Brazilian Public Social Security System. Transplantation. 2014;98(11):1199–1204. doi: 10.1097/TP.0000000000000418. [DOI] [PubMed] [Google Scholar]