Abstract
Objective:
We examined associations between criminal-legal involvement and serious psychological distress (SPD), and how these associations differ by racial/ethnic group.
Methods:
Conducting a retrospective analysis of multiple cross-sections from the National Survey on Drug Use and Health (2015–2019) and using multivariable linear probability regression models, we assessed criminal-legal involvement (having a lifetime arrest or conviction of a crime, being on probation or parole in the past-year, or being on supervised release, or other conditional release from prison in the past year) among a nationally representative sample of non-institutionalized US adults, that were 18 years or older (n=214,505), with and without SPD.
Results:
Adults with SPD had higher rates of criminal-legal involvement than adults without SPD (+4.1%, 95%CI: 3.3%−4.8%, p<0.001). The rate of criminal-legal involvement increased as psychological distress severity increased from mild (+3.2%, 95%CI: 2.6%−3.8%, p<0.00) to high (+7.2%, 95%CI: 6.4%−8.0%, p<0.001), relative to none. The risk of criminal-legal involvement for those with SPD was even greater for Black and Latinx adults compared with White adults (+1.8%, 95%CI: 0.1%−3.5%, p<0.05 and +3.2%, 95%CI: 1.3%−5.2%, p<0.01, respectively).
Conclusions:
Rates of criminal-legal involvement are higher for adults with SPD. Efforts are needed to equitably triage individuals with acute mental health needs to timely psychiatric care as opposed to carceral settings. State and federal governments should consider increased investment in collaborative models of care that commingle resources from mental health and law enforcement organizations to prevent the unnecessary incarceration of individuals experiencing mental health crises and increase their likelihood of obtaining community-based treatment.
Introduction
The US incarceration rate is more than five times the rate of other developed countries (1) and individuals with mental illness are disproportionately represented among the incarcerated. As many as 31% of incarcerated adults have a mental illness (2), compared to 19% of adults in the general population (3). According to the US Department of Justice, the rate of serious psychological distress is more than five times higher among the incarcerated than the general population (4,5). Serious psychological distress refers to a high-level of nonspecific symptoms of stress such as anxiety and depression and is used as a nonspecific proxy indicator of a probable serious mental illness (SMI) (6–8). People with serious psychological distress demonstrate characteristics of decreased daily functioning, lower socioeconomic status, and higher comorbidities and health care utilization rates similar to those with SMI (9).
Importantly, no prior nationally representative study evaluates the association of having a history of criminal-legal involvement (CLI) and mental illness in the general adult population (most studies report on the prevalence of mental illness among the currently arrested or incarcerated adult population). Quantifying this association is important given that incarceration has been shown to result in long-term adverse outcomes of people with serious psychological distress. Individuals receive poorer quality of care while incarcerated, which leads to higher admission of intensive crisis-oriented services after their release (10). Additionally, young adults age 23–29 who have been formerly incarcerated have low rates of health insurance coverage, with 57% uninsurance among individuals with incarceration experience compared to 20% of those without incarceration experience, reducing their access to affordable mental health treatment (11).
A disproportionate share of the incarcerated are Black and Latinx adults. According to the Federal Bureau of Prisons (12), as of April 2021, 39% of inmates are Black adults while accounting for 13% of the US population (13). Similarly, Latinx adults comprise 30% of inmates (12) but account for 18% of the nation’s population (13). One study showed that non-Latinx Black men have seven times the incarceration rate as non-Latinx White men and the incarceration rate of non-Latinx Black women is almost three times as high as the incarceration rate of non-Latinx White women (14). Structural racism, differential policing, and unjust criminal punishment are salient contributors to the higher rates of incarceration among Black and Latinx adults (15). Structural racism refers to the manner in which societal policies, institutional practices, and cultural norms reinforce and perpetuate racial/ethnic inequality.
Though the rates of mental illness among racial/ethnic minority groups are similar or lower than non-Latinx White individuals, (16) they experience greater persistence and severity. (15,17,18) Despite the burden of disease, racial/ethnic minorities are less likely to access mental health treatment than White individuals (19,20) and unmet need for mental health services is associated with higher odds of interacting with the criminal-legal system (21). One study assessing incarceration rates in the state of California found higher rates of mental illness among Black and Latinx inmates, relative to White inmates (22). Research among those who have been involved in the criminal-legal system demonstrates that being of Black race and having a non-psychotic mental health disorder are associated with higher odds of re-arrest and longer jail time (21).
Building on this body of literature, the objective of this study is to assess the association between serious psychological distress and CLI and examine differences among racial/ethnic groups using nationally representative survey data. Identifying the association between CLI and serious psychological distress and how this association differs amongst racial and ethnic minorities in the U.S. fills a gap in evidence needed to build interventions that disrupt the link between inequitable mental health care and a criminal-legal system that disproportionately targets people of color. We hypothesize: 1) adults with serious psychological distress will have higher rates of CLI than adults without serious psychological distress; and 2) the risk of CLI for those with serious psychological distress will be even greater for Black and Latinx adults compared with White adults.
Methods
Data
In this retrospective analysis, we used multiple cross-sections (2015–2019) of the annual National Survey on Drug Use and Health (NSDUH) from the Substance Abuse and Mental Health Services Administration. We pooled five years of data to increase the precision of estimates. The NSDUH is a nationally representative survey that collects information from the non-institutionalized population on their illicit drug use, alcohol use, CLI, behavioral health treatment, and sociodemographic characteristics. Additionally, the NSDUH uses validated diagnostic instruments matching criteria from the Diagnostic and Statistical Manual of Mental Health Disorders (DSM) to identify behavioral health disorders (23). The analytic sample included adults who were 18 years and older (n= 214,505). This study was approved by the Institutional Review Board.
Dependent variables
Our primary outcome, CLI, was a dichotomous variable operationalized as having experienced any of the following: a lifetime arrest or conviction of a crime, past-year probation or parole, supervised release, or other conditional release from prison in the past year.
Independent variables
Our primary independent variable of interest was an indicator for serious psychological distress where K-6 scores ≥ 13 were assigned a value of 1 and K-6 scores ≤ 12 were assigned a value of 0. The K-6 scale has a sensitivity of 90% and specificity of 89% for identifying any mood or anxiety disorder (K-6 scores ≥ 13) as defined by the DSM-IV and can distinguish cases from non-cases with consistency across sociodemographic subsamples (24). A cut-point of ≤12 versus ≥13 is optimal as an indicator of clinically significant psychiatric disorder (8,24). To assess the differential association between CLI and mental illness by race/ethnicity, we focus on the interaction between the serious psychological distress indicator variable and the race/ethnicity categorical variable. We recognize that race/ethnicity are socially constructed categories and a proxy for the experience of racism. We examine disparities between racial/ethnic minority groups and the referent majority White group to generate evidence demonstrating unfair and unjust distributions of CLI, recognizing that racial/ethnic disparities are driven by racism and longstanding structural inequities. Based on self-report, we categorized race/ethnicity as non-Latinx White (hereafter referred to as White), non-Latinx Black (hereafter referred to as Black), Latinx, and non-Latinx Asian (hereafter referred to as Asian). In secondary analysis, we assessed associations between criminal legal involvement and levels of psychological distress grouped into no (K-6 score = 0), low (K-6 scores 1–5), moderate (K-6 scores 6–10), or high psychological distress (K-6 scores ≥ 11) (7,24). This categorization allows us to ascertain the relationship between CLI and more moderate levels of mental distress, which may also warrant preventative mental health intervention. We adjusted regression models for covariates that potentially confound the relationship between serious psychological distress and CLI. Covariates included age (18–25, 26–35, 36–49, 50–64, or 65+), sex (female or male), race/ethnicity, marriage status (married or single), education (less than high school, high school graduate, some college, or college graduate), federal poverty level (FPL) (100–124% FPL, 125–199% FPL, 200–399% FPL, or ≥400% FPL) insurance status (private, Medicaid, Medicare, other insurance, or uninsured), physical health status (excellent, very good, good, fair, or poor), any substance use disorder (yes or no), survey year (2015, 2016, 2017, 2018, or 2019).
Statistical analysis
First, we compared adults’ demographic characteristics and CLI by serious psychological distress status using chi-square tests and t-tests for dichotomous and continuous variables, respectively. Next, we estimated multivariable linear probability regression models to assess the association between serious psychological distress and CLI conditional on previously mentioned covariates. This linear regression modeling approach enables regression coefficients to be directly interpreted as percentage-point differences (e.g., Black adults vs. White adults) in rates of CLI.
Next, to obtain a better understanding of the relationship between psychological distress severity and CLI, we re-estimated our regression model with a categorical variable illustrating levels of psychological distress that ranged from no to high psychological distress. To assess the differential effects of serious psychological distress and race/ethnicity, we re-estimated regression models with an interaction between the serious psychological distress indicator variable and the race/ethnicity (referent White) categorical variable. In secondary analyses, we disaggregated our primary outcome into two dichotomous variables, any lifetime arrest or conviction of a crime (hereafter lifetime arrest/conviction) and any past-year probation or parole, supervised release, or other conditional release from prison (hereafter past-year community supervision), to assess the robustness of our primary findings. We used predictive margins methods (25) to assess within and between group differences. All rates and model estimates were weighted to be nationally representative and account for sample design and survey nonresponse. We present magnitudes of differences with confidence intervals that allow for comparisons across all racial/ethnic groups. Results are considered statistically significant at p<0.05 (2-tailed). Analyses were conducted using Stata release 16 (26).
Results
Table 1 compares the demographic characteristics and CLI for adults by serious psychological distress status. There were higher rates of CLI among adults with serious psychological distress than adults without serious psychological distress (24% vs. 16%, p<0.001). Relative to adults without serious psychological distress, adults with serious psychological distress were more likely to be White (70% vs 65%, p<0.001), younger (e.g., 18–25: 29% vs. 12%, p<0.001), female (62% vs. 51%, p<.001), single (31% vs. 54%, p<0.001), have some college education (37% vs. 30%, p<0.001), low-income (e.g., >100% FPL: 25% vs 15%, p<0.001), Medicaid insured (21% vs. 10%, p<0.001), poor self-rated physical health (6% vs. 2%, p<0.001), and have a substance use disorder (11% vs. 2%, p<0.001).
Table 1.
Demographics and criminal-legal involvementa for adults (18+) by serious psychological distressb status, National Survey on Drug Use and Health, 2015–2019
| Serious Psychological Distress | ||
|---|---|---|
|
|
||
| Yes | No | |
|
| ||
| Sample Size (N) | 33,487 | 181,018 |
|
| ||
| % | % | |
| Criminal-legal Involvement | ||
| Yes | 23.8*** | 15.9 |
| Race/ethnicity | ||
| White | 69.1*** | 65.2 |
| Black | 11.0*** | 12.3 |
| Latino | 15.8* | 16.6 |
| Asian | 4.1*** | 6.0 |
| Age | ||
| 18–25 | 29.0*** | 12.0 |
| 26–35 | 22.6*** | 15.1 |
| 36–49 | 24.1 | 24.7 |
| 50–64 | 17.4*** | 26.3 |
| 65+ | 6.9*** | 21.9 |
| Sex | ||
| Female | 61.9*** | 50.5 |
| Married | ||
| Yes | 30.8*** | 54.4 |
| Education | ||
| Less than high school | 13.3 | 12.6 |
| High school graduate | 25.4 | 24.8 |
| Some college | 37.3*** | 30.0 |
| College graduate | 24.0*** | 32.6 |
| Federal poverty level (FPL) | ||
| >100% FPL | 24.8*** | 14.5 |
| 100–124% FPL | 6.4*** | 4.8 |
| 125–199% FPL | 17.3*** | 14.5 |
| 200–399% FPL | 20.89*** | 22.1 |
| ≥400% FPL | 30.6*** | 44.1 |
| Insurance | ||
| Private | 50.5*** | 53.8 |
| Medicaid | 20.7*** | 10.3 |
| Medicare | 13.2*** | 24.1 |
| Other Insurance | 2.5** | 2.1 |
| None | 13.1*** | 9.7 |
| Self-rated health | ||
| Excellent | 12.1*** | 22.2 |
| Very good | 31.1*** | 36.4 |
| Good | 31.7*** | 29.0 |
| Fair | 18.7*** | 10.3 |
| Poor | 6.4*** | 2.2 |
| Any substance use disorder | ||
| Yes | 11.40*** | 1.8 |
| Year | ||
| 2015 | 18.3 | 19.9 |
| 2016 | 18.9 | 19.9 |
| 2017 | 19.9 | 20.1 |
| 2018 | 20.5 | 20.1 |
| 2019 | 22.4 | 20.0 |
p<0.05
p<0.01
p<0.001
Criminal-legal involvement: a lifetime arrest or conviction of a crime, past-year probation or parole, supervised release, or other conditional release from prison in the past year
Serious psychological distress: Kessler-6 (K6) scale scores ≥ 13
In our adjusted regression analysis, the rate of CLI was 4 percentage-points higher (Table 2, See Online Supplement for Full Regression Results) for adults with serious psychological distress compared to adults without serious psychological distress (95%CI: 3.3%−4.8%, p<0.001). Examining the association between different levels of psychological distress and CLI (Table 2, See Online Supplement for Full Regression Results), rates of CLI demonstrates a gradient that increased in percentage-points with higher levels of psychological distress (mild (increase 3.2 percentage-points, 95%CI: 2.6%−3.8%, p<0.001), moderate (increase 5.6 percentage-points, 95%CI:4.8%−6.4%, p<0.001), and high psychological distress (increase 7.2 percentage-points, 95%CI:6.4%- 8.0%, p<0.001), relative to no psychological distress.
Table 2.
Adjusted regression results of criminal-legal involvement by serious psychological distress, National Survey on Drug Use and Health, 2015–2019 a
| Criminal-Legal Involvement b | |||
|---|---|---|---|
|
| |||
| Difference | 95%CI | Sig | |
|
|
|||
| Serious psychological distress c (Reference No) | |||
| Yes | 4.1% | 3.3 – 4.8 | *** |
| Kessler-6 scale scores (Reference 0 (None)) | |||
| 1–5 (Mild) | 3.2% | 2.6 – 3.8 | *** |
| 6–10 (Moderate) | 5.6% | 4.8 – 6.4 | *** |
| 11–24 (High) | 7.2% | 6.4 – 8.0 | *** |
p<0.05
p<0.01
p<0.001
Regression model adjusted for the following covariates: age, sex, race/ethnicity, marriage status, education, insurance status, physical health status, substance use disorder, and year
Criminal-legal involvement: a lifetime arrest or conviction of a crime, past-year probation or parole, supervised release, or other conditional release from prison in the past year
Serious psychological distress: Kessler-6 (K6) scale scores ≥ 13
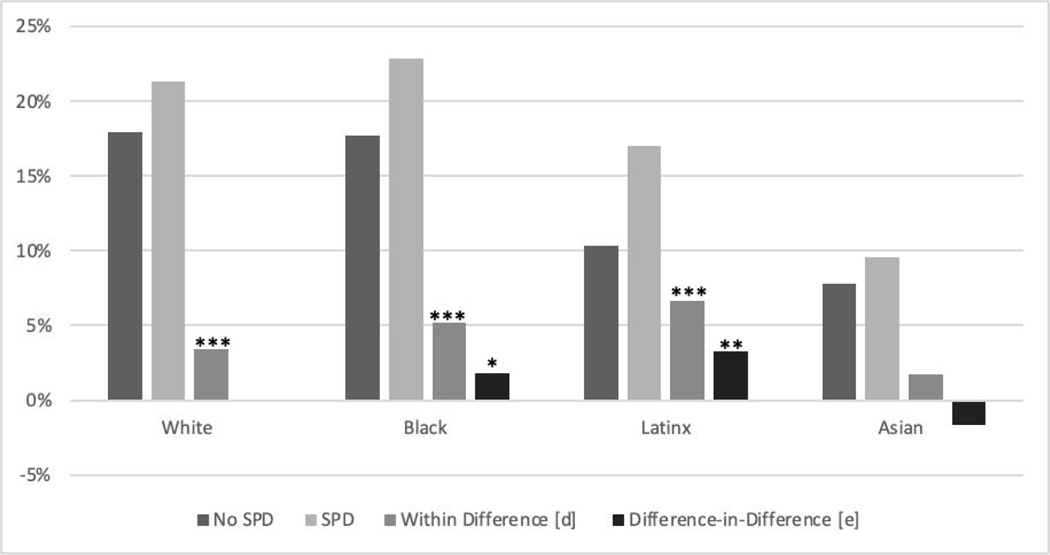
When estimating the differential associations between CLI and serious psychological distress by race/ethnicity (Figure 1, See Online Supplement for Full Regression Results), we identified that the increased risk of CLI for those with serious psychological distress was even greater for Black and Latinx adults than White adults (interaction= increase 1.8 percentage-points, 95%CI: 0.1%−3.5%, p<0.05 and interaction= increase 3.2 percentage-points, 95%CI: 1.3%−5.2%, p<0.01, respectively).
Figure 1.
Adjusted rates of criminal-legal involvement by serious psychological distress and race/ethnicity, National Survey on Drug Use and Health, 2015–2019 a,b,c
*p<0.05; **p<0.01; ***p<0.001
a. Regression model adjusted for the following covariates: age, sex, race/ethnicity, marriage status, education, insurance status, physical health status, substance use disorder, year
b. Criminal-legal involvement: experiencing any of the following: a lifetime arrest or conviction of a crime, past-year probation or parole, supervised release, or other conditional release from prison in the past year
c. Serious psychological distress: Kessler-6 (K6) scale scores ≥ 13
d. Within Difference: Difference between SPD and no SPD within racial/ethnic group
e. Difference-in-Difference: Difference between SPD and no SPD among Black (Latinx or Asian) adults minus the difference between SPD and no SPD among White adults
Similar to primary results, in secondary analyses (See Online Supplement) serious psychological distress was positively associated with both lifetime arrest/convection and past-year community supervision.
Discussion
As hypothesized, greater psychological distress was associated with greater CLI, with CLI increasing on a gradient with increased psychological distress. This was expected given studies showing higher rates of mental illness among those in carceral settings compared to the general population (2,4,5), but the current study provides new data specifically showing that, in the general population, CLI is greater for those with serious psychological distress than for those without serious psychological distress. To our knowledge, this is the first study to evaluate the risk of CLI among adults with psychological distress using nationally representative household survey data. This is a needed contribution to the literature as most studies have focused on mental illness among incarcerated populations and not on the heightened risk of incarceration among people with serious psychological distress in the general population, and how the association within this population varies by racial/ethnic group.
The persistence of racial discrimination within both behavioral health and criminal-legal systems is exemplified by the fact that the increased risk of CLI among those with serious psychological distress is greater for Black and Latinx adults compared to White adults. Institutional systemic racism and implicit biases have perpetuated the differential treatment for these populations in both mental health and criminal-legal systems (15). Underlying these results are multiple healthcare factors, such as poor access to mental health treatment (27) lower help-seeking (17), and inadequacy of available treatment (20), combined with criminal-legal system factors, such as racial differentiation in incarceration rates, and lower likelihood of mental health treatment diversion among Black and Latinx adults.
Efforts to successfully reduce CLI and recidivism or to improve mental health service access are often racialized and closely associated with socioeconomic status. For example, drug court programs have demonstrated success in decreasing recidivism rates for participants compared to non-participants (28,29). Drug courts, the most common form of civil problem-solving courts, were first established in the U.S. in 1989 as a means for reducing recidivism for reoffending individuals with substance use disorder by focusing on treatment and rehabilitation for participants as an alternative to criminal prosecution and incarceration (30,31). However, studies have shown that many drug courts across the United States are less effective for Black participants than for White participants (32,33). Negative social and environmental factors are a likely source for the racial disparities in drug court graduation rates (34). For example, participants of drug court programs are more likely to be of White race with no criminal history, with research suggesting that drug court eligibility criteria and implicit biases of prosecuting attorneys and other legal staff may select against non-White participants (35). This is a result of institutional bias closely associated with poverty as well as co-indicators of CLI and mental health issues (35–37). Future research should assess the intersection of serious psychological distress, illicit drug use, and CLI to elucidate the mechanisms that contribute to racial disparities.
Additionally, studies have indicated no differences in psychological distress amongst racial/ethnic minorities as compared to White majorities when matched by socioeconomic status (16) but only 9% of Black adults in the US receive any mental health services, nearly half that of White adults (16.6%) (38). Studies have shown that people of color are more likely to attribute symptoms of psychological distress to circumstances and life stressors rather than psychological disorders, contributing to less help-seeking and service utilization (17,39). A history of segregation and discrimination toward people of color, perpetuates the disproportionate chronic poverty that results in inequitable effects on mental health (15, 40).
The advantages of living in the US as a non-Latinx White person is evidenced through more favorable sociodemographic outcomes such as housing status, education levels, and socioeconomic status- variables which are negatively associated with CLI and represent systemic privilege. Conversely, the disadvantages of living in the U.S. as a Black or Latinx adult with mental illness is complex and intersects to create a greater risk of criminal-legal involvement. The compounded consequences for people who are members of multiple stigmatized social groups results in public perception and attitudes of discrimination that have implications for the effectiveness and accessibility of appropriate interventions (36,41). Solutions for these systemic issues would require a multi-tiered approach tailored to the challenges specific to these populations which extend beyond the initiation of mental health services to also include initiatives directed toward improving other social determinants of health for underprivileged populations. Efforts for improved mental health services should concurrently prioritize support and equitable opportunity for housing, education, transportation, and employment- determinants which promote access, utilization, and sustainability of behavioral health services while also mitigating the racially disproportionate disadvantage that amplifies the impacts of serious psychological distress and criminal-legal involvement.
Our study had several limitations. First, the NSDUH is cross-sectional and precludes casual inferences. Nonetheless, our study illustrates significant associations between serious psychological distress and CLI among a nationally representative sample of adults. Second, data are based on survey respondent’s self-reports and dependent on their recall and truthfulness. To increase survey response accuracy, answers to sensitive questions are collected using Audio-Computer Assisted Self-Interview methods, where respondents listen to prerecorded questions using headphones and respond directly into a NSDUH laptop computer without NSDUH interviewers knowing their answers (23). Third, the survey population is limited to non-institutionalized U.S. civilians and excludes the unhoused, incarcerated, or those in residential treatment. Consequently, estimates may be conservative as the aforementioned groups are likelier to experience high-levels of serious psychological distress and have prior CLI. Fourth, we used a psychological distress measure that captures the frequency an individual feels distressed (e.g., hopeless, restless or fidgety, everything was an effort) in the previous year and does not capture a specific mental disorder. However, the K-6 captures symptoms commonly associated with depression and anxiety and can reliably, with high sensitivity and specificity (7,24), distinguish cases from non-cases with consistency across sociodemographic subsamples. The K-6 scale was validated against DSM-IV criteria for determining SMI or any mental illness prior to changes in the diagnostic criteria for the more recent DSM-V (8,42). Fifth, NSDUH does not capture the type of infraction that led to CLI, contact frequency with the criminal-legal system, or living situation during community supervision
Conclusion
Despite these limitations, our study suggests that adults with serious psychological distress experience higher rates of CLI and that this association is even greater among Black and Latinx individuals. Illuminating incarceration disparities can inform efforts at the state and federal levels to incentivize incarceration alternatives for people experiencing behavioral health issues. Importantly, our findings underscore a need for the unlearning and dismantling of racial stereotyping and racist heuristics that inform the prosecution of racial/ethnic minorities in the criminal-legal system. The disproportionate CLI resulting from historic and systemic racism may be most successfully mitigated through efforts to improve interdisciplinary collaboration amongst system of care stakeholders including law enforcement and criminal-legal court systems but extending to behavioral health providers and even educational institutions. The findings from this study underscore the disparate social determinants which confound higher rates of CLI especially for adults with serious psychological distress who are racial/ethnic minorities. Enlisting the attention and action of cross-sectoral stakeholders to ensure early identification of need, access, and affordability to mental health services as well as establishing equitable opportunities for education, employment, and housing may serve as holistic incarceration prevention for this population. It is critical for individuals experiencing psychological distress to avoid unnecessary interaction with the criminal-legal system and to have timely access to evidence-based treatment that improves their mental health status and enables them to maintain their presence in the community.
Supplementary Material
Highlights:
Adults with serious psychological distress had higher rates of criminal-legal involvement than adults without serious psychological distress.
Rates of criminal-legal involvement increased as psychological distress severity increased from mild, moderate, and high.
Black and Latinx adults with serious psychological distress, who experience systemic and structural inequities, had even higher rates of criminal-legal involvement compared to White adults with serious psychological distress.
Funding:
This work was supported by the National Institute on Minority Health and Health Disparities (R01MD010456)
Footnotes
Disclosures: Drs. F, S, F, R, C, and Ms. M have no conflict of interests to declare.
References
- 1.Wagner P. and Sawyer W, States of incarceration: The global context 2018. Prison Policy Initiative, 2018. 1. [Google Scholar]
- 2.Prins SJ, Prevalence of mental illnesses in US state prisons: A systematic review. Psychiatric Services, 2014. 65(7): p. 862–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration, Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (HHS Publication No. PEP19–5068, NSDUH Series H-54) Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, 2019. [Google Scholar]
- 4.Bronson J. and Berzofsky M, Indicators of mental health problems reported by prisoners and jail inmates, 2011–12. Bureau of Justice Statistics, 2017: p. 1–16. [Google Scholar]
- 5.Howell BA, Wang EA, and Winkelman TN, Mental health treatment among individuals involved in the criminal justice system after implementation of the Affordable Care Act. Psychiatric Services, 2019. 70(9): p. 765–771. [DOI] [PubMed] [Google Scholar]
- 6.Swartz JA and Jantz I, Association between nonspecific severe psychological distress as an indicator of serious mental illness and increasing levels of medical multimorbidity. Am J Public Health, 2014. 104(12): p. 2350–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Furukawa TA, et al. , The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychol Med, 2003. 33(2): p. 357–62. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, et al. , Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res, 2010. 19 Suppl 1(Suppl 1): p. 4–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pratt LA, Dey AN, and Cohen AJ, Characteristics of adults with serious psychological distress as measured by the K6 scale: United States, 2001–04. Adv Data, 2007(382): p. 1–18. [PubMed] [Google Scholar]
- 10.Hawthorne WB, et al. , Incarceration Among Adults Who Are in the Public Mental Health System: Rates, Risk Factors, and Short-Term Outcomes. Psychiatric Services, 2012. 63(1): p. 26–32. [DOI] [PubMed] [Google Scholar]
- 11.Wilkinson LL, et al. , Psychological Distress and Health Insurance Coverage among Formerly Incarcerated Young Adults in the United States. AIMS public health, 2015. 2(3): p. 227–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Federal Bureau of Prisons, Inmate Race. 2021.
- 13.United States Census Bureau, QuickFacts; United States. 2019.
- 14.Guerino P, Harrison PM, and Sabol WJ, Prisoners in 2010. Washington, DC: Bureau of Justice Statistics, 2011. [Google Scholar]
- 15.Williams DR and Mohammed SA, Racism and Health I: Pathways and Scientific Evidence. The American behavioral scientist, 2013. 57(8): p. 10.1177/0002764213487340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mouzon DM, et al. , Serious psychological distress among African Americans: findings from the national survey of American life. Journal of Community Psychology, 2016. 44(6): p. 765–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Breslau J, et al. , Racial/ethnic differences in perception of need for mental health treatment in a US national sample. Soc Psychiatry Psychiatr Epidemiol, 2017. 52(8): p. 929–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Flores MW, et al. , Major Depressive Episode Severity Among Adults from Marginalized Racial and Ethnic Backgrounds in the US. JAMA Psychiatry, 2021. 78(11): p. 1279–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Biener AI and Zuvekas SH, Do Racial and Ethnic Disparities in Mental Health Treatment Vary With Underlying Mental Health? Med Care Res Rev, 2021. 78(4): p. 392–403. [DOI] [PubMed] [Google Scholar]
- 20.Cook BL, et al. , Assessing racial/ethnic disparities in treatment across episodes of mental health care. Health services research, 2014. 49(1): p. 206–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Constantine R, et al. , Characteristics and experiences of adults with a serious mental illness who were involved in the criminal justice system. Psychiatr Serv, 2010. 61(5): p. 451–7. [DOI] [PubMed] [Google Scholar]
- 22.Appel O, et al. , Differential Incarceration by Race-Ethnicity and Mental Health Service Status in the Los Angeles County Jail System. Psychiatr Serv, 2020. 71(8): p. 843–846. [DOI] [PubMed] [Google Scholar]
- 23.Center for Behavioral Health Statistics and Quality, 2019 National Survey on Drug Use and Health Public Use File Codebook, . 2020, Substance Abuse and Mental Health Services Administration,: Rockville, MD. [Google Scholar]
- 24.Kessler RC, et al. , Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med, 2002. 32(6): p. 959–76. [DOI] [PubMed] [Google Scholar]
- 25.Graubard BI and Korn EL, Predictive margins with survey data. Biometrics, 1999. 55(2): p. 652–9. [DOI] [PubMed] [Google Scholar]
- 26.StataCorp., Stata Statistical Software: Release 16. . 2019, StataCorp LLC.: College Station, TX. [Google Scholar]
- 27.Cook BL, et al. , Trends in Racial-Ethnic Disparities in Access to Mental Health Care, 2004–2012. Psychiatr Serv, 2017. 68(1): p. 9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mitchell O, et al. , Assessing the effectiveness of drug courts on recidivism: A meta-analytic review of traditional and non-traditional drug courts. Journal of Criminal Justice, 2012. 40(1): p. 60–71. [Google Scholar]
- 29.Shaffer DK, et al. , Outcomes among drug court participants: does drug of choice matter? Int J Offender Ther Comp Criminol, 2011. 55(1): p. 155–74. [DOI] [PubMed] [Google Scholar]
- 30.U.S. Department of Justice, Drug Courts. Office of Justice Programs. 2021. [Google Scholar]
- 31.National Association of Drug Court Professionals (NADCP), Adult Drug Court Best Practice Standards. 2018. [Google Scholar]
- 32.Marlowe DB, Achieving Racial and Ethic Fairness in Drug Courts. Ct. Rev, 2013. 49: p. 40. [Google Scholar]
- 33.McKean J. and Warren-Gordon K, Racial Differences in Graduation Rates From Adult Drug Treatment Courts. Journal of Ethnicity in Criminal Justice, 2011. 9: p. 41–55. [Google Scholar]
- 34.Gallagher JR and Wahler EA, Racial Disparities in Drug Court Graduation Rates: The Role of Recovery Support Groups and Environments. Journal of Social Work Practice in the Addictions, 2018. 18(2): p. 113–127. [Google Scholar]
- 35.Gallagher JR, Wahler EA, and Lefebvre E, Further Evidence of Racial Disparities in Drug Court Outcomes: Enhancing Service-Delivery to Reduce Criminal Recidivism Rates for Non-White Participants. Journal of Social Service Research, 2020. 46(3): p. 406–415. [Google Scholar]
- 36.Villatoro AP, et al. , Perceived Need for Mental Health Care: The Intersection of Race, Ethnicity, Gender, and Socioeconomic Status. Soc Ment Health, 2018. 8(1): p. 1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fazel S, et al. , Mental health of prisoners: prevalence, adverse outcomes, and interventions. Lancet Psychiatry, 2016. 3(9): p. 871–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Substance Abuse and Mental Health Services Administration, Racial/ Ethnic Differences in Mental Health Service Use among Adults. , in HHS Publication No. SMA-15–4906. . 2015. Substance Abuse and Mental Health Services Administration.: Rockville, MD: . [Google Scholar]
- 39.Hines-Martin V, et al. , Barriers to mental health care access in an African American population. Issues Ment Health Nurs, 2003. 24(3): p. 237–56. [DOI] [PubMed] [Google Scholar]
- 40.Khullar D. and Chokshi DA, Health, income, & poverty: Where we are & what could help. Health affairs, 2018. 4. [Google Scholar]
- 41.Oexle N. and Corrigan PW, Understanding Mental Illness Stigma Toward Persons With Multiple Stigmatized Conditions: Implications of Intersectionality Theory. Psychiatric Services, 2018. 69(5): p. 587–589. [DOI] [PubMed] [Google Scholar]
- 42.Substance Abuse and Mental Health Services Administration, CBHSQ Methodology Report, in Impact of the DSM-IV to DSM-5 Changes on the National Survey on Drug Use and Health. 2016, Substance Abuse and Mental Health Services Administration (US): Rockville (MD). [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.