Abstract
Objectives:
Mechanically ventilated children post-hematopoietic cell transplant (HCT) have increased morbidity and mortality compared to other mechanically ventilated critically ill children. Tracheal intubation-associated adverse events (TIAE) and peri-intubation hypoxemia universally portend worse outcomes. We investigated whether adverse peri-intubation associated events occur at increased frequency in patients with HCT compared to non-HCT oncologic or other pediatric ICU patients and therefore might contribute to increased mortality.
Design:
Retrospective cohort between 2014 and 2019
Setting:
Single-center academic non-cardiac pediatric ICU
Patients:
Critically ill children who underwent tracheal intubation (TI)
Interventions:
None
Methods:
Data from the local airway management quality improvement databases and Virtual Pediatric Systems were merged. These data were supplemented with a retrospective chart review for HCT-related data, including HCT indication, transplant-related comorbidity status, and patient condition at the time of TI procedure. The primary outcome was defined as the composite of hemodynamic TIAE (hypo/hypertension, arrhythmia, cardiac arrest) and/or peri-intubation hypoxemia (SpO2<80%) events.
Results:
1,931 encounters underwent TI, of which 92 (4.8%) were post-HCT, while 319 (16.5%) had history of malignancy without HCT, and 1,520 (78.7%) had neither HCT nor malignancy. Children post-HCT were older more often had respiratory failure as an indication for intubation, use of catecholamine infusions peri-intubation, and use of non-invasive ventilation prior to intubation. Hemodynamic TIAE or peri-intubation hypoxemia were not different across 3 groups (HCT 16%, non-HCT with malignancy 10%, other 15). After adjusting for age, difficult airway feature, provider type, device, apneic oxygenation use, and indication for intubation, we did not identify an association between HCT status and the adverse TI outcome (OR:1.32 for HCT status vs. other, 95% CI, 0.72–2.41, p=0.37).
Conclusions:
In this single center study, we did not identify an association between HCT status and hemodynamic TIAE or peri-intubation hypoxemia during tracheal intubation.
Keywords: Critical care, hematopoietic stem cell transplantation, tracheal intubation, pediatric, mechanical ventilation
INTRODUCTION
Children post-HCT frequently require ICU care and have a high degree of resource utilization (1). They also have increased rates of complications, including infection, graft-versus-host disease (GVHD), veno-occlusive disease, transplant-associated thrombotic microangiopathy, or disease relapse (2–4). In particular, patients post-HCT suffer from frequent pulmonary complications (5–8).
Patients post-HCT who require mechanical ventilation (MV) have increased mortality compared to non-HCT oncologic patients (9). Factors contributing to the high rate of respiratory failure and ICU mortality in HCT patients have not been fully explored. Prolonged MV and elevated oxygen requirements have been associated with decreased long-term survival (10–11). Earlier MV in post-HCT has been associated with better survival, suggesting that earlier interventions may improve outcomes (12–13). Cardiac arrest has been reported in as high as 11% of patients post-HCT during tracheal intubation (TI) (14), indicating that delays in intubation may contribute to high mortality. Few studies have investigated the optimal timing of TI in HCT patients, and in the general ICU population, TIAE and peri-intubation hypoxemia have been associated with increased mortality and longer duration of invasive MV (15, 16). No studies, to our knowledge, have examined the occurrence of TIAE in critically ill patients post-HCT to determine if they have a higher rate of TIAE and peri-intubation hypoxemia compared to an oncologic population without HCT or to a population without HCT or malignancy.
Because of the known association between MV and increased mortality in patients post-HCT, and the known association between the TIAEs and ICU outcomes among critically ill children, we sought to investigate if peri-intubation adverse events are more common in patients post-HCT. These events could contribute to the increase in poor clinical outcomes and peri-intubation safety may be an important target to improve clinical outcomes. Our hypothesis for this study was that critically ill children post-HCT would have a higher frequency of hemodynamic TIAEs or peri-intubation hypoxemia during TI procedure compared to those without HCT.
MATERIALS AND METHODS
Study Design
This study was a retrospective analysis of single-center TI encounters performed in a quaternary pediatric non-cardiac ICU at a large children’s hospital in North America from January 2014 through December 2019. We included all critically ill patients from 6 months to 21 years of age who received primary TI procedure in the ICU. This study met exemption status as determined by the local Institutional Review Board (Children’s Hospital of Philadelphia IRB 20–017364, ‘Intubation-associated adverse events in hematopoietic stem cell transplant, oncologic, and non-oncologic patients’, 4/16/2020). Study procedures followed in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975.
Data Collection
We leveraged two databases: a local pediatric National Emergency Airway Registry (NEAR4KIDS) quality improvement database and the Virtual Pediatric Systems (VPS LLC, Los Angeles, CA) datasets to identify TI encounters in these patient populations. The TI encounter, rather than patient, was used as the unit of analysis because conditions for each TI are different when more than one TI occur in one patient during ICU stay. The NEAR4KIDS registry is an international quality improvement collaborative developed through the Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network (16). It collects patient, provider, and practice characteristics potentially associated with the quality and safety of TIs in pediatric ICUs. Patient demographics, airway characteristics, indication for TI, provider demographics, medications used, presence of difficult mask ventilation and difficult airway (DA) features, lowest procedural oxygen saturations, and occurrence of TIAE were collected. Consensus-driven, a priori developed, NEAR4KIDS Operational Definitions were followed, as described (15, 16).
VPS is a pediatric critical care quality improvement data registry which captures patient demographics, primary and secondary diagnoses, procedures performed, characteristics of mechanical ventilation, and ICU outcomes. The local NEAR4KIDS database was merged with the VPS dataset via patient identifier (medical record number). Using retrospective electronic health record (EHR) review by one investigator (KBL), we confirmed the TI took place during the ICU stay and confirmed the primary exposures. We collected the following data points from the EHR within 1 hour (peri-intubation) before intubation: chronic use of non-invasive positive pressure ventilation (NIPPV), use of NIPPV peri-intubation, NIPPV settings, fraction of inspired oxygen (FiO2), blood gas data within 1- and 4-hours pre-intubation, use of catecholamines and type peri-intubation, and continuous renal replacement peri-intubation. HCT data collected from the EHR included transplant date, source, type, and GVHD status. A randomly chosen 5% sample of the data abstraction was repeated and verified 97% of data accuracy. After merging of databases and EHR review, 1,931 distinct TI encounters from the Children’s Hospital of Philadelphia were identified (Figure 1).
Figure 1:
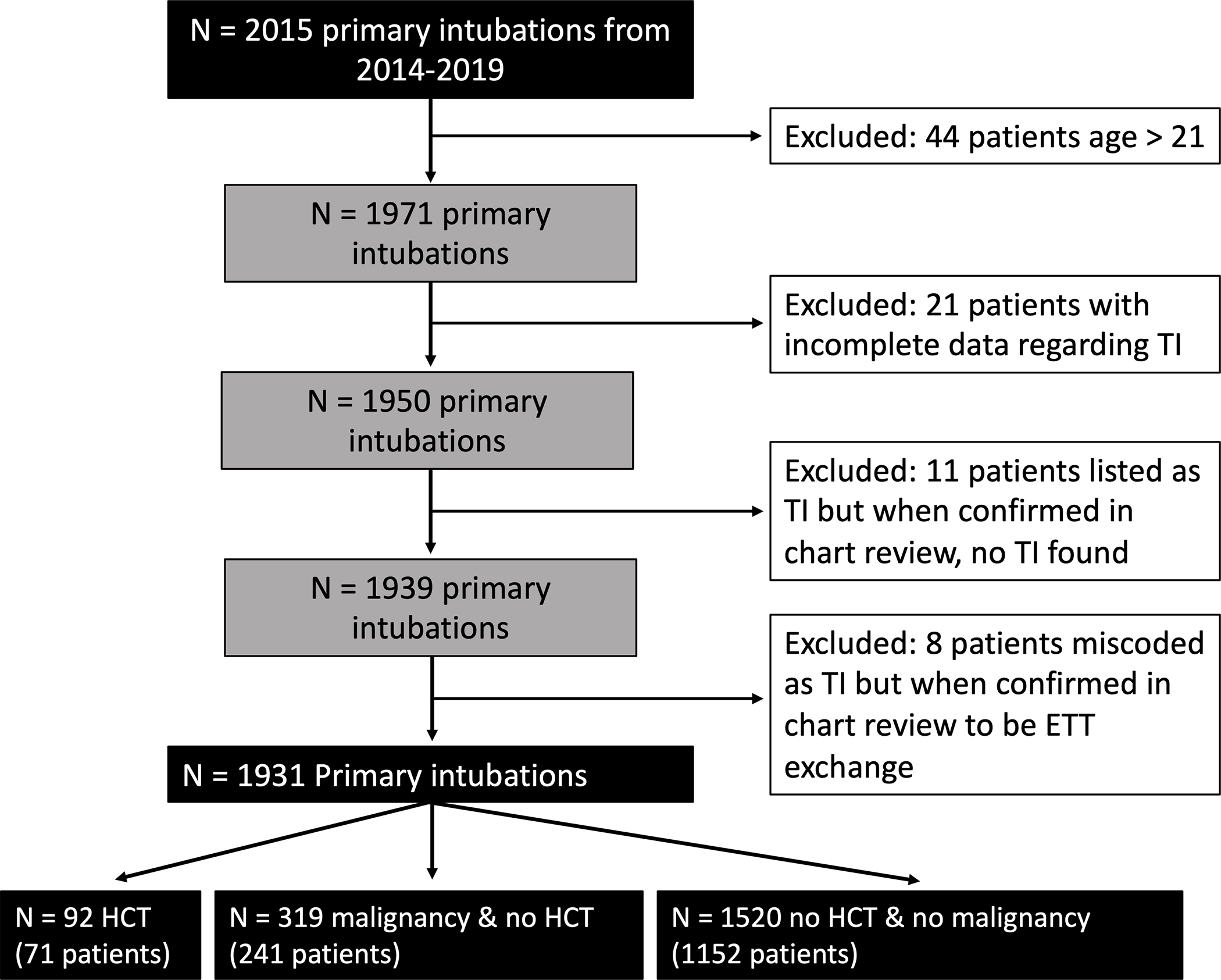
Flow diagram of patient inclusion and exclusion process before arriving at final study population. A Local NEAR4KIDS database was queried prior to manual chart review confirming selection criteria and accuracy.
Exposure and Outcome Measurement
We classified the exposure status into three categories: post-HCT, malignancy without HCT, and without either HCT or malignancy. HCT encounters included both allogeneic and autologous transplant and occurred prior to TI. Additional exposure variables such as age, sex, weight, difficult airway (DA) features, provider type, device use, number of intubation attempts, use of apneic oxygenation, TI indication, and use of catecholamines were also collected at the time of intubation. Detailed HCT data, including duration from transplant, cellular source of transplant, type of transplant, and GVHD status were analyzed as exposures for association with NIPPV.
The primary outcome was hemodynamic TIAE and/or peri-intubation hypoxemia (SpO2 <80%) during the TI procedure, as validated in other studies (15, 17–18). The hemodynamic TIAE were defined as hyper- or hypotension requiring intervention, dysrhythmia, or cardiac arrest with or without return of spontaneous circulation. These are considered as physiological consequences of prolonged apneic time associated with laryngoscopy, sympathetic response to laryngoscopy maneuver, or medication administration. Peri-intubation hypoxemia was defined as oxyhemoglobin desaturation as measured by pulse oximetry <80% where the saturation was greater than 90% after pre-oxygenation. The time window for the hemodynamic TIAEs was within 20 minutes of TI procedure, and the window for hypoxemia was from induction until endotracheal tube securing. A composite outcome of hemodynamic TIAE or hypoxemia was chosen to best account for all physiologic consequences of TI. Chronic NIPPV use was defined as NIPPV use prior to hospital admission. The remainder of peri-intubation data used the most recent value up until the moment of intubation with a maximum of 1 hour prior to intubation.
Statistical analysis
With an estimated 350 TI per year over 6 years, we have an 80% power if TIAEs occur in 25% of HCT patients and 15% in non-HCT patients with the proportion of intubation in HCT patients assumed at 5% among all intubations in the ICU. This assumption was based off previous studies noting 20% TIAE in a general population of pediatric ICU patients (16).
Univariate analyses were performed to assess the associations of the patient groups (HCT status) with the primary outcome via Chi square or Fisher’s exact test. Univariate analyses were also performed to compare patient, provider, and practice characteristics across the patient groups. Following our causal model, multivariable logistic regression was performed to evaluate the association of HCT or malignancy without HCT, relative to neither, with the primary outcome (Supplemental Figure A). A principal multivariable regression was performed without use of catecholamines, because catecholamines likely function as mediators between the HCT status and the primary outcome. Moreover, patients post-HCT have delayed ICU admission and are sicker upon ICU arrival (11–12). As a sensitivity analysis, we implemented use of catecholamines as covariates and assessed how the strength of association attenuates the association between the HCT status and primary outcome. Large attenuation of the association in this sensitivity analysis would indicate that use of catecholamines is mediating in the causal model. Other covariates (patient age, DA feature, provider type, device, apneic oxygenation use, and intubation indication) were identified as confounders based on prior knowledge (19). Subgroup analysis was performed to explore factors associated with bi-level non-invasive positive airway pressure (BLPAP) ventilation support among patients with HCT.
RESULTS
Patient characteristics across three groups
A total of 1,464 patients were intubated across 1,931 encounters. HCT and non-HCT with malignancy patients accounted for 92 (4.8%) and 319 (16.5%) of encounters, respectively (Table 1). 82/92 (89%) of HCT patients were post-allogenic HCT, and 10/92 (11%) were status post-autologous HCT. In patients post-HCT, there was a median of 101 (36–367) days from transplant to intubation. The patients without either HCT or malignancy were younger and had more frequent DA features than HCT groups and non-HCT malignancy. Chronic NIPPV use was less prevalent in patients with HCT (0% vs 11%; mean difference: 11.0% [95% CI, 9.4 to 12.5]) and non-HCT with malignancy patients (1% vs 11%; mean difference: 10% [95% CI, 8.6 to 12.2]) compared to those without either HCT or malignancy.
Table 1.
Patient demographics by exposure group
| Variable | All Encounters (n=1931) | Without Malignancy No HCT (n=1520) | With Malignancy No HCT (n=319) | HCT (n=92) |
|---|---|---|---|---|
|
| ||||
| Age category (count, %) | 422 (22%) | 390 (26%) | 25 (8%) | 7 (8%) |
| <1 year | 856 (44%) | 639 (42%) | 181 (57%) | 36 (39%) |
| 1–7 year | 565 (29%) | 429 (28%) | 97 (30%) | 39 (42%) |
| 8–17 year | 88 (5%) | 62 (4%) | 16 (5%) | 10 (11%) |
| ≥18 year | ||||
|
| ||||
| Male sex (count, %) | 1022 (53%) | 800 (53%) | 169 (53%) | 53 (58%) |
|
| ||||
| Weight in kg, median (IQR) | 16.8 (9.5–34.8) | 15.4 (8.7–32.5) | 19.9 (13.3–41.3) | 25.1 (12.8–54.7) |
|
| ||||
| Year | ||||
| 2014 | 329 (17%) | 243 (16%) | 69 (22%) | 17 (18%) |
| 2015 | 330 (17%) | 248 (16%) | 70 (22%) | 12 (13%) |
| 2016 | 325 (17%) | 276 (18%) | 35 (11%) | 14 (15%) |
| 2017 | 322 (17%) | 266 (18%) | 47 (15%) | 9 (10%) |
| 2018 | 353 (18%) | 273 (18%) | 55 (17%) | 25 (27%) |
| 2019 | 272 (14%) | 214 (14%) | 43 (13%) | 15 (16%) |
|
| ||||
| Use of chronic NIPPV | ||||
| None | ||||
| CPAP | 1757 (91%) | 1348 (89%) | 317 (99%) | 92 (100%) |
| BLPAP | 76 (4%) | 74 (5%) | 2 (1%) | 0 (0%) |
| 98 (5%) | 98 (6%) | 0 (0%) | 0 (0%) | |
|
| ||||
| Difficult airway features | 453 (23%) | 391 (26%) | 41 (13%) | 21 (23%) |
HCT: hematopoietic stem cell transplant; PIM2: Pediatric Index of Mortality 2; IQR: interquartile range; NIPPV: non-invasive positive pressure ventilation; CPAP: continuous positive airway pressure; BLPAP: bi-level positive airway pressure
Despite minimal chronic NIPPV use in HCT patients, HCT patients had the highest use of NIPPV peri-intubation (59% vs 42%; mean difference: 17% [95% CI, 7 to 27]) compared to those without either HCT or malignancy while non-HCT malignancy had slightly lower NIPPV peri-intubation use (19% vs 42%; mean difference: −23% [95% CI, −18 to −28]). Patients post-HCT were also supported with peri-intubation catecholamine infusions at an increased frequency (17% vs 7%; mean difference: 10% [95% CI, 2 to 18]) compared to patients without either of HCT or malignancy (7%), whereas those with non-HCT malignancy (10% vs 7%; mean difference: 3% [95% CI, −0.5 to 6.5]) were not. The use of CRRT peri-intubation was not different across the three groups, but the overall use was negligible (n=25, 1% of the entire cohort). There were differences across groups in provider type and indication for intubation (Table 2). At the time of intubation, there were no differences in intubation device, number of attempts, blood pH, or apneic oxygenation use.
Table 2.
Peri-intubation characteristics by exposure group
| Variable | All Patients (n=1931) | Without Malignancy No HCT (n=1520) | With Malignancy No HCT (n=319) | HCT (n=92) |
|---|---|---|---|---|
|
| ||||
| Provider type | ||||
| PCCM Attending | 103 (5%) | 77 (5%) | 21 (7%) | 5 (5%) |
| PCCM/EM fellow | 1202 (62%) | 926 (61%) | 200 (63%) | 76 (83%) |
| Peds/EM resident | 125 (6%) | 103 (7%) | 21 (7%) | 1 (1%) |
| Advanced provider | 354 (18%) | 284 (19%) | 65 (20%) | 5 (5%) |
| Subspecialist/Other | 147 (8%) | 130 (9%) | 12 (4%) | 5 (5%) |
|
| ||||
| Device | ||||
| DL | 1012 (52%) | 786 (52%) | 182 (57%) | 44 (48%) |
| VL | 887 (46%) | 707 (47%) | 133 (42%) | 47 (51%) |
| LMA/FO/Other | 31 (2%) | 26 (2%) | 4 (1%) | 1 (1%) |
|
| ||||
| Number of attempts, median (IQR) | 1 (1–1) | 1 (1–1) | 1 (1–1) | 1 (1–1) |
|
| ||||
| Use of apneic oxygenation | 911 (47%) | 728 (48%) | 141 (44%) | 42 (46%) |
|
| ||||
| pH peri-intubation, median (IQR)a | 7.28 (7.19–7.36) | 7.28 (7.19–7.36) | 7.31 (7.20–7.37) | 7.31 (7.23–7.35) |
|
| ||||
| Indication for intubationb | ||||
| Respiratory | 973 (50%) | 832 (55%) | 80 (25%) | 61 (66%) |
| Shock | 180 (9%) | 137 (9%) | 30 (9%) | 13 (14%) |
| Neurologic | 204 (11%) | 176 (12%) | 18 (6%) | 10 (11%) |
| Procedural | 807 (42%) | 554 (36%) | 228 (71%) | 25 (27%) |
|
| ||||
| Use of catecholamine infusion peri-intubation | 155 (8%) | 107 (7%) | 32 (10%) | 16 (17%) |
|
| ||||
| Use of any NIPPV peri-intubation | 813 (42%) | 699 (46%) | 60 (19%) | 54 (59%) |
|
| ||||
| Use of NIPPV peri-intubation | ||||
| None | 1125 (58%) | 828 (54%) | 259 (81%) | 38 (41%) |
| HFNC | 82 (4%) | 62 (4%) | 12 (4%) | 8 (9%) |
| CPAP | 159 (8%) | 133 (9%) | 15 (5%) | 11 (12%) |
| BLPAP | 565 (29%) | 497 (33%) | 33 (10%) | 35 (38%) |
pH data available in 437 patients
Indications are not mutually exclusive. Encounters with multiple indications for intubation had all indications listed
PCCM: pediatric critical care medicine; EM: emergency medicine; DL: direct laryngoscopy; VL: video laryngoscopy; LMA: laryngeal mask airway; FO: fiberoptic; IQR: interquartile range; NIPPV: non-invasive positive pressure ventilation; HFNC: high flow nasal cannula
Primary and secondary outcomes across three groups
Hemodynamic TIAE or hypoxemia occurred at similar frequency across patient populations: 15/92 of HCT encounters (16% vs 15%; mean difference: 1% [95% CI, −7 to 9]), 33/319 of non-HCT with malignancy encounters (10% vs 15%; mean difference: −5% [95% CI, −8 to −1]), and 229/1520 (15%) of encounters without either of HCT or malignancy (Univariate analysis, Supplemental Table B). Patients post-HCT also had a broader range of lowest SpO2 during intubation.
After accounting for patient and process variables unbalanced across the groups [age, indication for intubation, DA feature, provider type, device, apneic oxygenation use] with multivariable logistic regression, we did not identify an association between HCT status and the primary outcome (OR, 1.32 [95% CI, 0.72–2.41]; p=0.37). A repeated analysis with catecholamine use did not attenuate the response in HCT encounters (OR, 1.26 [95% CI 0.68–2.31]). Non-HCT with malignancy status was also not associated with TIAE or hypoxemia (OR, 1.13 [95% CI, 0.74–1.73]; p=0.61) and repeated analysis with catecholamine use yielded similar results (OR, 1.12 [95% CI, 0.73–1.70]) (Table 3).
Table 3:
Multivariable analysis for association of diagnosis category with hemodynamic tracheal intubation associated events or hypoxemia (SpO2<80%)
| Exposure (primary analysis) | Odds ratio | 95% Confidence interval | p-value |
|
| |||
| Diagnosis Category | |||
| Without malignancy or HCT | 1 (reference) | N/A | N/A |
| With malignancy, no HCT | 1.13 | 0.74–1.73 | 0.56 |
| HCT | 1.32 | 0.72–2.41 | 0.37 |
|
| |||
| Exposure (sensitivity analysis) | Odds ratio | 95% Confidence interval | p-value |
|
| |||
| Diagnosis Category | |||
| Without malignancy or HCT | 1 (reference) | N/A | N/A |
| With malignancy, no HCT | 1.12 | 0.73–1.70 | 0.61 |
| HCT | 1.26 | 0.68–2.31 | 0.46 |
Adjusted covariates included patient age, difficult airway feature, provider type, device, apneic oxygenation, and indication for intubation
Primary analysis performed without use of catecholamines while sensitivity analysis performed with it
N/A: not applicable, HCT: hematopoietic cell transplant
Subgroup analysis: HCT patients with or without bi-level non-invasive positive pressure ventilation support
BLPAP was commonly used prior to TI procedure in patients post-HCT (35/92, 38%). Patient age, sex, DA features, provider type, device, number of attempts, and use of catecholamines were not associated with the use of BLPAP peri-intubation (Supplemental Table C). Apneic oxygenation was more frequently used, and intubation was more often performed by critical care trained providers in post-HCT patients with BLPAP support versus patients without it. Transplant characteristics, graft source, presence of GVHD, and the median time from HCT were not associated with BLPAP use. Twenty percent of the HCT patients with BLPAP use had either hemodynamic TIAE or hypoxemia, while 14% of HCT patients without BLPAP use experienced the outcome. Nineteen percent of post-HCT patients with any form of NIPPV experienced hemodynamic TIAE or hypoxemia while 13% without NIPPV experienced the outcome (Supplemental Table D).
DISCUSSION
In this study of nearly 2,000 TI encounters in critically ill pediatric patients, we found that children post-HCT have increased respiratory failure and hemodynamic instability. Over half of patients post-HCT received NIPPV at the time of intubation. After adjustment for patient and practice factors, we did not find an association between HCT status and a higher rate of peri-intubation hemodynamic adverse events or hypoxemia. Subgroup analyses of HCT patients revealed that higher patient weight and respiratory indication for intubation was associated with BLPAP use.
Limited literature has assessed peri-intubation adverse events in the HCT population. Patients post-HCT have high mortality rates in the setting of MV, lower survival with prolonged MV, and elevated mortality rates with prolonged NIPPV prior to tracheal intubation (12–13). In patients post-HCT treated with NIPPV prior to intubation, there is higher mortality and fewer ventilator-free days (20) with as many as 11% of patients who failed NIPPV therapy experiencing cardiac arrest during TI (14). It is essential to determine if there is a higher occurrence of peri-intubation adverse events in patients post-HCT, which may potentially contribute to worse survival outcomes with prolonged MV. However, we did not identify a significant association between the HCT status and peri-intubation adverse events, and therefore cannot conclude that the worse clinical outcomes in patients post-HCT who receive MV can be attributed to peri-intubation adverse events. In Supplemental Table B, the lowest SpO2 was less for post-HCT patients compared to other groups, while the median value of the lowest SpO2 was similar. This indicates that a small proportion of these patients had extremes of hypoxemia.
A key discussion point is the timing to perform TI in patients post-HCT with respiratory failure. In our study, the majority of HCT patients who received TI were already on NIPPV. The timing of NIPPV implementation in this study reflects the practice at a single center and commonly functions an indication for PICU admission. Do PICU clinicians delay performing TI and initiating mechanical ventilation in children with HCT status? One recent study utilizing a large VPS database showed that in patients post-HCT, both exposure to and duration of NIPPV before TI were significantly associated with higher mortality (13) but it lacked a cohort of patients with HCT status who successfully received NIPPV and did not require TI. The study did not demonstrate causation, which is a known shortcoming of this type of analysis (21). In our study, the timing of TI intervention is confounded by the severity of disease by only including patients intubated in the ICU. Additional studies analyzing the timing of MV need to be prospectively studied in a randomized control fashion to identify the optimal approach.
Among the HCT cohort, BLPAP was implemented more frequently in heavier patients (Supplemental Table C). This is consistent with the results reported by Cater and colleagues who examined use of NIPPV prior to intubation in HCT patients (20). While BLPAP may be effective in larger patients with idealized triggered breaths, it is also possible that the patients or their guardians do not wish to endure the sedation required by mechanical ventilation if the risk of mortality is high. Given that exposure to and duration of NIPPV may be associated with poorer outcome, it is prudent to discuss with families the option for earlier TI and mechanical ventilation. Of note, the number of patients with HCT that required BLPAP was small, and we were not adequately powered to evaluate the difference in outcomes.
Our study demonstrated that the patients post-HCT who receive TI in the ICU are sicker and with more respiratory and hemodynamic instability. These patient conditions may likely explain previously reported high cardiac arrest rates in HCT patients undergoing TI. These post-HCT patients require more clinical resources and meticulous management until the time of intubation as exemplified by more frequent NIPPV and catecholamine use than the general ICU patients who require TI. Best practice to minimize apneic time, optimize first attempt success, and mitigate hemodynamic instability during TI may be critical to achieve best safety outcome. Use of apneic oxygenation and video laryngoscopy may be considered as well. Both a previous single center study and a large observational study showed the benefit of apneic oxygenation practice and video laryngoscopy for critically ill children undergoing TI (22, 23). Our study was conducted in a high volume PICU with experience managing patients with HCT; this pre-intubation preparation may contribute to the lack of difference in TIAE across groups that might be evident in a lower volume setting. For example, patients post-HCT on BLPAP prior to intubation were more often treated with apneic oxygenation during intubation, intubated by a provider with critical care training, and used video laryngoscopy more frequently compared to patients post-HCT not on BLPAP. These measures may have helped to optimize the safety of these TI encounters.
Our study has several strengths, including a large sample size, well-validated data sources, prospective TI data collection via local NEAR4KIDS registry, and description of key variables related to HCT status. However, this was a single-center observational study, which limits the generalizability. The majority of the ICU patients who require diagnostic MRI studies received TIs as a local practice, which is reflected in the large proportion of procedural TI indication in patients with malignancy. Procedural intubations may reduce the likelihood of TIAE in patients because they are frequently performed in clinically stable patients without cardiopulmonary dysfunction or on patients admitted for neurologic monitoring. This practice may vary depending on the sedation model. The HCT-related patient data were retrospectively collected from EHR and subject to reporting bias. The number of TI in HCT patients was limited, potentially making our study underpowered to detect an association of HCT status with peri-intubation adverse events. While our study showed the HCT patients undergoing TI procedure are sicker and managed more frequently with NIPPV, the optimal timing to transition to invasive mechanical ventilation cannot be determined due to the observational study design.
CONCLUSIONS
Patients post-HCT undergoing TI in the pediatric ICU are sicker compared to patients with malignancy without HCT status and compared to those without either malignancy or HCT status, demonstrating a need for additional clinical resources and management during TI to reduce peri-intubation adverse events. We were unable to identify an association between HCT status and peri-intubation adverse events, yet we cannot rule out a 2.4-fold association. Future studies are needed to optimize the timing of TI and invasive mechanical ventilation in patients post-HCT.
Supplementary Material
Supplemental Figure A: Directed acyclic graph (DAG) of the causal structure model including covariates. Catecholamine use was classified as a potential mediator of downstream effect.
Supplemental Table B: Adverse hemodynamic tracheal intubation associated events across three groups.
Supplemental Table C: HCT and BLPAP exposure characteristics. A retrospective chart review collected HCT characteristics prior to intubation. Exposure was divided into patient encounters with BLPAP and without BLPAP.
Supplemental Table D: HCT and NIPPV exposure characteristics. Exposure was divided into patient encounters with any form of NIPPV and those without NIPPV.
Research in Context.
Critically ill patients post-HCT have increased morbidity and mortality, especially as it relates to delayed or prolonged mechanically ventilation
Tracheal intubation adverse events create additional risk in the general critically ill population and add to respiratory complications
No studies have investigated the procedure of tracheal intubation in patients post-HCT to examine the association between HCT status and adverse events, and thereby potentially contribute to worse clinical outcomes in this population
At the Bedside.
The timing of tracheal intubation in HCT status patients remains a clinical dilemma and TIAE poses increased risk of morbidity and mortality in critically ill patients
HCT status does not appear to be associated with TIAE or peri-intubation hypoxemia, despite the increased mortality in MV patients post-HCT
Patients post-HCT require respiratory optimization prior to intubation as well as post-intubation to improve clinical outcomes
Source of Funding
This project is supported by Agency for Healthcare Research and Quality (AHRQ: R18HS024511) and Endowed Chair, Critical Care Medicine at The Children’s Hospital of Philadelphia, University of Pennsylvania Perelman School of Medicine.Dr. Nishisaki and Mrs. Napolitano are supported by AHRQ R18HS024511. Dr. Lindell is supported by the Thrasher Research Fund. Dr. Rowan is supported by NIH NHLBI (K23HL150244). Dr. Fitzgerald is supported by NIH NIDDK (K23DK119463). Mrs. Napolitano has research/consulting relationships with Dräger, Timpel, Philips/Respironics, Actuated Medical, and VERO-Biotech.
Footnotes
Conflict of Interest
Copyright Form Disclosure: Drs. Nishisaki and Napolitano’s institutions received funding from the Agency for Healthcare Research and Quality (AHRQ) (R18HS024511). Dr. Nishisaki’s institution received funding from Critical Care Medicine and Chiesi, Inc; she received support for article research from the AHRQ. Drs. Yehya and Fitzgerald’s institutions received funding from the National Institutes of Health (NIH). Dr. Yehya’s institution received funding from Pfizer. Drs. Yehya and Rowan received support for article research from the NIH. Dr. Napolitano’s institution received funding from Drager, Timpel, Philips/Respironics, Actuated Medical, and VERO-Biotech. Dr. Rowan’s institution received funding from the National Heart, Lung, and Blood Institute (K23HL150244). The remaining authors have disclosed that they do not have any potential conflicts of interest.
Article Twitter
Stem cell transplant is not associated with increased risk of peri-intubation adverse events. An analysis of intubations helps understand risk and airway management in this vulnerable patient population.
REFERENCES
- 1.Chima RJ, Daniels RC, Kim MO, et al. Improved outcomes for stem cell transplant recipients requiring pediatric intensive care. Pediatr Crit Car Med 2012;13(6): 336–e34 [DOI] [PubMed] [Google Scholar]
- 2.Lindell RB, Gertz SJ, Rowan CM, et al. High Levels of Morbidity and Mortality Among Pediatric Hematopoietic Cell Transplant Recipients With Severe Sepsis: Insights From the Sepsis PRevalence, OUtcomes, and Therapies International Point Prevalence Study. Pediatr Crit Care Med 2017;18(12):1114–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jacobe SJ, Hassan A, Veys P, Mok Q. Outcome of children requiring admission to an intensive care unit after bone marrow transplantation. Crit Care Med 2003;31(5):1299–1305. [DOI] [PubMed] [Google Scholar]
- 4.Majhail NS, Brazauskas R, Hassebroek RA, et al. Outcomes of allogeneic hematopoietic cell transplantation for adolescent and young adults compared with children and older adults with acute myeloid leukemia. Biol Blood Marrow Transplant 2012;18:861–873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spicer AC, Calfee CS, Zinter MS, et al. A Simple and Robust Bedside Model for Mortality Risk in Pediatric Patients With Acute Respiratory Distress Syndrome. Pediatr Crit Care Med. 2016;17(10):907–916. doi: 10.1097/PCC.0000000000000865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaya Z, Weiner DJ, Yilmaz D, et al. : Lung function, pulmonary complications, and mortality after allogeneic blood and marrow transplantation in children. Biol Blood Marrow Transplant 2009; 15:817–826 [DOI] [PubMed] [Google Scholar]
- 7.Rowan CM, Loomis A, McArthur J, et al. High-Frequency Oscillatory Ventilation Use and Severe Pediatric ARDS in the Pediatric Hematopoietic Cell Transplant Recipient. Respir Care. 2018;63(4):404–411. doi: 10.4187/respcare.05765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Duncan CN, Lehmann LE, Cheifetz IM, et al. Pediatric Acute Lung Injury and Sepsis (PALISI) Network: Clinical outcomes of children receiving intensive cardiopulmonary support during hematopoietic stem cell transplant. Pediatr Crit Care Med 2013; 14:261–267 [DOI] [PubMed] [Google Scholar]
- 9.Tamburro RF, Barfield RC, Shaffer ML, et al. Changes in outcomes (1996–2004) for pediatric oncology and hematopoietic stem cell transplant patients requiring invasive mechanical ventilation. Pediatr Crit Care Med. 2008;9(3):270–277. [DOI] [PubMed] [Google Scholar]
- 10.Aspesberro F, Guthrie KA, Woolfrey AE, Brogan TV, Roberts JS. Outcome of pediatric hematopoietic stem cell transplant recipients requiring mechanical ventilation. J Intensive Care Med 2014; 29(1):31–7. [DOI] [PubMed] [Google Scholar]
- 11.Rowan CM, McArthur J, Hsing DD, et al. Acute respiratory failure in pediatric hematopoietic cell transplantation: a multicenter study. Critical Care Medicine. 2018;46(10):e967–74. [DOI] [PubMed] [Google Scholar]
- 12.Rowan CM, Gertz SJ, McArthur J, et al. Invasive mechanical ventilation and mortality in pediatric hematopoietic stem cell transplantation: a multicenter study. Pediatr Crit Care Med 2016;17(4):294–302. [DOI] [PubMed] [Google Scholar]
- 13.Lindell RB, Fitzgerald JC, Rowan C, et al. Duration for Preintubation NIPPV is Associated with PICU Mortality in Immunocompromised Children. Critical Care Medicine 2022;50(1):246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rowan C, Fitzgerald JC, Agulnik A, et al. Risk Factors for Noninvasive Ventilation Failure in Children Post-Hematopoietic Cell Transplant. Front Oncol. 2021;11:653607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parker MM, Nuthall G, Brown C, et al. Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network (2017). Relationship Between Adverse Tracheal Intubation Associated Events and PICU Outcomes. Pediatr Crit Care Med 2017;18(4):310–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nishisaki A, Turner DA, Brown CA, et al. National Emergency Airway Registry for Children (NEAR4KIDS); Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network: A National Emergency Airway Registry for children: Landscape of tracheal intubation in 15 PICUs. Crit Care Med 2013; 41:874–885 [DOI] [PubMed] [Google Scholar]
- 17.Daigle CH, Fiadjoe JE, Laverriere EK, et al. Difficult Bag-Mask Ventilation in Critically Ill Children Is Independently Associated With Adverse Events. Crit Care Med. 2020;48(9):e744–e752. [DOI] [PubMed] [Google Scholar]
- 18.Conway JA, Kharayat P, Sanders RC Jr, et al. Ketamine Use for Tracheal Intubation in Critically Ill Children Is Associated With a Lower Occurrence of Adverse Hemodynamic Events. Crit Care Med. 2020;48(6):e489–e497 [DOI] [PubMed] [Google Scholar]
- 19.Slater A, Shann F, Pearson G et al. PIM2: a revised version of the Paediatric Index of Mortality. Intensive Care Med 2003; 29, 278–285. [DOI] [PubMed] [Google Scholar]
- 20.Cater DT, Fitzgerald JC, Gertz SJ, et al. Noninvasive Ventilation Exposure Prior to Intubation in Pediatric Hematopoietic Cell Transplant Recipients [published online ahead of print, 2022 May 31]. Respir Care. 2022;respcare.09776. doi: 10.4187/respcare.09776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hurley C, Zinter MS. Should We Intubate Pediatric Hematopoietic Cell Transplant Patients With Respiratory Failure Sooner?. Crit Care Med. 2022;50(7):1163–1167. doi: 10.1097/CCM.0000000000005548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Napolitano N, Laverriere EK, Craig N, et al. Apneic Oxygenation As a Quality Improvement Intervention in an Academic PICU. Pediatr Crit Care Med. 2019;20(12):e531–e537. doi: 10.1097/PCC.0000000000002123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grunwell JR, Kamat PP, Miksa M, et al. Trend and Outcomes of Video Laryngoscope Use Across PICUs. Pediatr Crit Care Med. 2017;18(8):741–749. doi: 10.1097/PCC.0000000000001175 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure A: Directed acyclic graph (DAG) of the causal structure model including covariates. Catecholamine use was classified as a potential mediator of downstream effect.
Supplemental Table B: Adverse hemodynamic tracheal intubation associated events across three groups.
Supplemental Table C: HCT and BLPAP exposure characteristics. A retrospective chart review collected HCT characteristics prior to intubation. Exposure was divided into patient encounters with BLPAP and without BLPAP.
Supplemental Table D: HCT and NIPPV exposure characteristics. Exposure was divided into patient encounters with any form of NIPPV and those without NIPPV.


