Abstract
Objectives:
People who attend nightclubs and dance festivals—particularly those that feature electronic dance music (EDM), are at high risk for use of cocaine and other party drugs. Given that cocaine is now sometimes adulterated with fentanyl, this study examines trends in people’s knowledge about such risk of adulteration to inform prevention and harm reduction efforts.
Methods:
Adults were surveyed entering randomly selected EDM events (including dance festivals) in New York City in 2018, 2019, 2021, and 2022 (n=2,107). They were asked whether they agree that some dealers sell cocaine containing fentanyl, and trends in agreement were estimated.
Results:
Prevalence of agreement that cocaine can be adulterated increased from 42.1% (95% CI: 36.8–47.6) in 2018 to 65.6% (95% CI: 54.1–75.4) in 2022—a 55.8% increase (p<.001). Between 2018 and 2022, particular increases occurred among those not reporting past-year cocaine use (by 61.6%, p<.001), among white individuals (by 68.1%, p<.001), those with some college (by 68.5%, p=.021), and those age ≥26 (by 83.8%, p=.001)
Conclusions:
Awareness that cocaine can contain fentanyl is increasing in this high-risk population. Continued education is needed for high-risk populations regarding both opioid overdose response and test strips that can test drugs for the presence of fentanyl.
Keywords: cocaine, fentanyl, adulteration, drug education, drug checking
1. Introduction
The United States is experiencing an increase in deaths related to use of synthetic opioids and psychostimulants such as cocaine (Ahmad et al., 2021; Hedegaard et al., 2021). Specifically, deaths related to synthetic opioids, primarily fentanyl and its analogs, increased from 9,580 in 2015 to 56,516 in 2020, and deaths related to use of cocaine increased from 6,784 to 19,447 during the same period (Hedegaard et al., 2021). While co-use of fentanyl and psychostimulants appears to be more common as it has been driving the fourth wave of the opioid crisis (Ciccarone, 2021; Mattson et al., 2021), the extent to which cocaine is currently adulterated or contaminated with fentanyl or its analogs is unknown. National drug seizure data indicate that in 2016, 0.6% of seized cocaine samples contained fentanyl, but fentanyl adulteration of cocaine was found to be most common in New Hampshire (in 7.2% of cocaine samples tested), Connecticut (5.4%), Ohio (2.6%), and Massachusetts (2.1%) (Park et al., 2021). A more recent study of cocaine seizures in Ohio found that up to 11.3% of cocaine seized in 2017 contained fentanyl (Zibbell et al., 2019), suggesting increases in adulteration. More recent state- and national-level data are not yet available, however.
While the extent of unintentional exposure to fentanyl through adulterated or contaminated cocaine is unknown, there have been clusters of poisonings and deaths related to such unknown exposure. In Buenos Aires in early 2022, a single individual sold cocaine adulterated with carfentanil, a fentanyl analog 10,000 times more potent than morphine, which led to 98 hospitalizations including 24 deaths (Ferrari et al., 2022). In New York City (NYC), there have also been clusters of overdoses in which people were unintentionally exposed to fentanyl present in their cocaine (DiSalvo et al., 2020). Such instances led the NYC Department of Health and Mental Hygiene to issue alerts to nightlife attendees and to pilot an education program about potential cocaine contamination (Allen et al., 2020).
Past-year cocaine use is particularly prevalent among nightlife attendees (Palamar et al., 2022), with an estimated 35.2% of electronic dance music (EDM) nightclub and festival attendees in NYC using in 2019 (Palamar & Keyes, 2020). As such, this population is at high risk for unintentional exposure to fentanyl. Given that little is known regarding user knowledge about the potential for cocaine to be adulterated or contaminated with fentanyl, this study examined repeated cross-sectional data from EDM nightclub and dance festival attendees in NYC to estimate trends in knowledge about the risk of cocaine containing fentanyl. Results are intended to provide information to people in the fields of nursing and public health who develop or implement prevention and harm reduction programs.
2. Methods
2.1. Sample Recruitment
Adults (age ≥18) were surveyed as they were about to enter randomly selected EDM events in NYC during the summers of 2018 (n=1,018), 2019 (n=546), 2021 (n=222), and 2022 (n=321), with a combined sample of 2,107 participants. Each week, events (featuring live DJs) were randomly selected using R 3.1 software (R Core Team) based on an ongoing list of events listed on a popular EDM party ticket website. Events were typically held at nightclubs, but participants were also surveyed outside of 1–2 large dance festivals each year. While hundreds or even thousands of people attend nightclub events, tens of thousands of people attend festivals (Ridpath et al., 2014). The majority of events were in Brooklyn and in Manhattan (as very few events occur in other NYC boroughs) and recruitment typically occurred 1–2 nights per week between Thursday and Sunday. Participants were surveyed at a total of 84 events between 2018 and 2022 although data could not be collected in 2020 due to the COVID-19 pandemic. To determine eligibility, individuals approached by study staff were asked their age and asked if they were about to attend the event. Anonymous surveys were taken on tablets on the sidewalk outside of venues after informed consent was provided (on the first page of the anonymous survey). Survey completers were compensated $10 USD. Study staff tried their hardest to ensure the privacy of those taking the survey. Response rates for 2018, 2019, 2021, and 2022 were 73%, 65%, 63%, and 82%, respectively.
2.2. Data Collection and Analysis
While the survey focused on use of a wide variety of drugs and some other correlates of use, this analysis focuses specifically on the item asking about level of agreement to the following statement: “Some dealers sell cocaine containing fentanyl”. Answer options were “strongly disagree”, “disagree”, “neutral”, “agree”, and “strongly agree”, and responses were recoded into “agree” (including “strongly agree”) versus other responses. This question was piloted during an earlier phase of the study to determine participants’ beliefs about adulteration of various drugs (Palamar et al., 2021). Participants were also asked their age, sex, race/ethnicity, and education level. They were also asked about how often they attended such events in the past year and whether they used cocaine in the past year (yes/no). A previous study of this population including a follow-up survey to test response consistency determined that responses regarding past-year cocaine use had high test-retest reliability (κ=0.93) (Palamar et al., 2019).
Logistic regression was used to estimate the odds of the outcome (agreement that cocaine can contain fentanyl) as a linear function of time (survey year) as a continuous predictor. Year was coded as 0, 1, 3, and 4 for 2018, 2019, 2021, and 2022, respectively. Analyses were then repeated, stratified by participant characteristics. Then, a generalized linear model using Poisson and log link was used to examine associations between independent variables and agreement for the full sample, controlling for survey year. Survey weights were used in all analyses. These were computed based on response rates and self-reported level of nightlife attendance because frequent attendees have a higher likelihood of being sampled across venues. As such, weights were applied to make results more generalizable to all nightlife attendees in NYC, rather than to frequent party attendees (Palamar & Keyes, 2020).
2.3. Ethical Considerations
Before taking the anonymous surveys, potential participants were informed about the study aims and nature of this research project. Informed consent was provided on the first page of the survey. The New York University Langone Medical Center institutional review board approved all methods (s16-00702 and s18-00331).
3. Results
Table 1 presents sample characteristics and results stratified by participant characteristics. The majority of the sample was male (53.2%) and age 18–25 (55.4%), with 63.3% having earned a college degree. A quarter (24.5%) of EDM venue attendees in NYC are estimated to have used cocaine in the past year. Prevalence of agreement that cocaine can be adulterated increased from 42.1% (95% CI: 36.8–47.6) in 2018 to 65.6% (95% CI: 54.1–75.4) in 2022—a 55.8% increase (p<.001; Figure 1). Between 2018 and 2022, adults not reporting past-year use increased agreement by 61.6% (p<.001) and agreement among males and females increased by 46.1% (p=.010) and 61.2% (p=.009), respectively, with knowledge among females in 2022 being 11.7% lower than among males. Agreement increased among those age ≥26 (by 83.8%, p=.001) and among white individuals (by 68.1%, p<.001). These increases demonstrated current discrepancies in knowledge by age (i.e., 72.6% among those age ≥26 vs. 60.9% among those age 18–25) and race/ethnicity, with knowledge of adulteration among white individuals being 36.8% higher than Asians and 25.0% higher than Hispanics. Agreement increased among those with some college (by 68.5%, p=.021) and those with a college degree (by 51.3%, p=.006), with those with only a high school education having the highest prevalence of knowledge, particularly compared to those with a college degree. Finally, agreement also increased among participants surveyed entering nightclubs (by 65.3%, p=.007) and festivals (by 52.5%, p=.001). In the multivariable model (Table 2), Asians were at low probability for agreeing that cocaine can be adulterated (aPR=0.69, 95% CI: 0.51–0.93). No other independent variables were significant.
Table 1.
Trends in Estimated Prevalence of Agreement that Cocaine can be Adulterated with Fentanyl by Subgroups, 2018–2022
| Sample Characteristics (N=2,107) Weighted % (SE) |
2018 (N=1,018) Weighted % (SE) |
2019 (N=546) Weighted % (SE) |
2021 (N=222) Weighted % (SE) |
2022 (N=321) Weighted % (SE) |
% Relative Change | P | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Full Sample | 55.4 (2.5) | 42.1 (2.8) | 58.6 (3.5) | 66.5 (6.0) | 65.6 (5.0) | 55.8 | <0.001 |
| Cocaine Use | |||||||
| No Past-Year Use | 75.5 (2.2) | 40.9 (3.4) | 52.0 (6.0) | 64.6 (7.8) | 66.1 (6.3) | 61.6 | <0.001 |
| Past-Year Use | 24.5 (2.2) | 45.6 (4.8) | 70.5 (6.9) | 81.2 (7.2) | 63.8 (11.7) | 39.9 | 0.232 |
| Sex | |||||||
| Male | 53.2 (2.6) | 41.9 (3.6) | 58.7 6.3) | 66.7 (9.9) | 61.2 (7.2) | 46.1 | 0.010 |
| Female | 46.8 (2.6) | 42.3 (4.3) | 58.3 (7.1) | 66.0 (8.8) | 68.2 (7.8) | 61.2 | 0.009 |
| Age | |||||||
| 18–25 | 55.4 (2.5) | 43.9 (3.7) | 61.8 (6.1) | 56.0 (9.5) | 60.9 (7.4) | 38.7 | 0.057 |
| ≥26 | 44.6 (2.5) | 39.5 (4.2) | 56.4 (7.0) | 75.1 (8.7) | 72.6 (8.0) | 83.8 | 0.001 |
| Race/Ethnicity | |||||||
| White | 43.2 (2.5) | 46.7 (4.1) | 61.1 (6.7) | 77.2 (9.1) | 78.5 (5.6) | 68.1 | <0.001 |
| Hispanic | 22.4 (2.1) | 37.6 (5.5) | 61.7 (10.5) | 76.5 (9.4) | 53.5 (12.1) | 42.3 | 0.196 |
| Asian | 16.3 (1.8) | 33.4 (5.8) | 59.1 (11.0) | 57.2 (14.3) | 41.7 (12.2) | 24.9 | 0.698 |
| Other Race | 18.1 (2.3) | 43.8 (8.1) | 49.5 (11.4) | 42.0 (14.7) | 71.3 (16.4) | 62.8 | 0.197 |
| Education | |||||||
| High School or Less | 15.8 (1.8) | 43.8 (8.0) | 65.3 (13.3) | 45.4 (14.4) | 73.6 (12.4) | 68.0 | 0.177 |
| Some College | 20.9 (2.0) | 42.6 (5.4) | 70.5 (9.7) | 79.8 (7.1) | 71.8 (9.8) | 68.5 | 0.021 |
| College Degree | 63.3 (2.4) | 41.3 (3.5) | 53.7 (6.0) | 74.0 (7.4) | 62.5 (6.9) | 51.3 | 0.006 |
| Where Surveyed | |||||||
| Nightclub | 47.6 (1.9) | 39.2 (4.1) | 66.5 (8.1) | 69.5 (8.0) | 64.8 (7.1) | 65.3 | 0.007 |
| Festival | 52.4 (1.9) | 44.4 (3.7) | 54.9 (6.) | 65.4 (9.1) | 67.7 (5.6) | 52.5 | 0.001 |
Note. Relative change represents the relative difference between the 2022 prevalence and 2018 prevalence. Given that individuals identifying as Black are underrepresented in the NYC club scene (6.6%, SE=1.1), there were too few cases per cell to examine this race as its own category. It therefore was combined with the other race category. SE = standard error.
Figure 1.
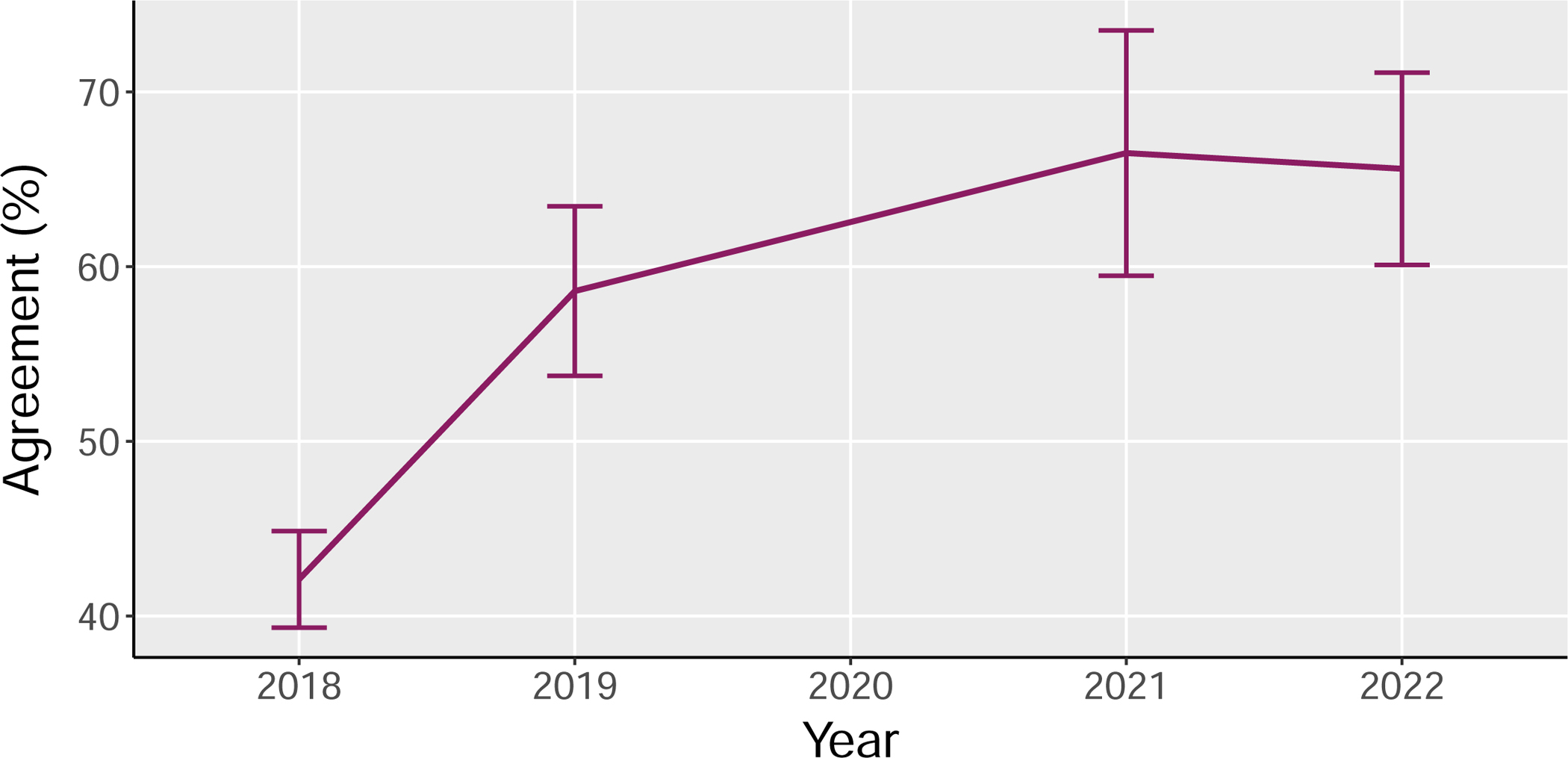
Estimated Prevalence of Agreement that Cocaine can be Adulterated with Fentanyl, 2018–2022
Table 2.
Multivariable Model Examining Correlates of Reporting Agreement that Cocaine can Contain Fentanyl
| aPR (95% CI) | |
|---|---|
|
| |
| Survey Year | 1.11 (1.06–1.16)b |
| Cocaine Use | |
| No Past-Year Use | 1.00 |
| Past-Year Use | 1.06 (0.89–1.27) |
| Sex | |
| Male | 1.00 |
| Female | 1.04 (0.88–1.22) |
| Age | |
| 18–25 | 1.00 |
| ≥26 | 1.08 (0.91–1.27) |
| Race/Ethnicity | |
| White | 1.00 |
| Hispanic | 0.81 (0.65–1.01) |
| Asian | 0.69 (0.51–0.94)a |
| Other Race | 0.84 (0.64–1.10) |
| Education | |
| High School or Less | 1.00 |
| Some College | 1.05 (0.81–1.37) |
| College Degree | 0.94 (0.73–1.21) |
| Where Surveyed | |
| Nightclub | 1.00 |
| Festival | 0.97 (0.83–1.13) |
Note. aPR = adjusted prevalence ratio; CI = confidence interval
p < .05
p < .001
4. Discussion
In 2022, two-thirds of individuals in this high-risk population were estimated to be aware that cocaine can be adulterated with fentanyl, and this is a 55.8% increase compared to 2018. Increases were detected among various subgroups including those who have not used cocaine in the past year. Overall, while Asians were the only subpopulation at low probability for reporting this knowledge, there were other notable but nonsignificant subgroup discrepancies. For example, agreement was visibly lower among males (compared to females), those age 18–25 (compared to those age ≥26), white individuals (compared Hispanic individuals), and those with a college degree (compared to those with only a high school education). These subgroups at higher risk can benefit from more targeted education about the potential for cocaine to be adulterated with fentanyl. Nonetheless, these findings can inform prevention and harm reduction efforts overseen by public health practitioners, nurses, and other medical practitioners.
First, general education that party drugs such as cocaine can be adulterated with fentanyl is still needed. Indeed, the majority (65.6%) of this high-risk population now appears to be aware of such adulteration potential, but there is still a sizable gap in knowledge with over a third (34.4%) of attendees not being aware that cocaine can contain fentanyl. Another notable gap is that in 2022, 36.2% of attendees using cocaine in the past year were unaware that cocaine can be adulterated with fentanyl. Among those who are aware about adulteration potential, it is unknown whether such knowledge was derived from drug checking, from peers who use, from media coverage of fentanyl being present in drugs such as cocaine, or from recent public health messaging in NYC (Allen et al., 2020). Such messaging was largely limited to bar scenes, not nightclubs (Allen et al., 2020), but there was some media coverage. However, despite such increasing knowledge in this population, education about potential adulteration needs to continue, with dissemination needing to reach other populations at high risk (e.g., bar attendees, people who inject drugs, homeless populations) (Allen et al., 2020; Hayashi et al., 2018; Krieger et al., 2018; Tilhou et al., 2022).
Second, given that this EDM venue-attending population is becoming increasingly aware that they are at risk for unintentional exposure to fentanyl, it is important that such individuals are educated about naloxone which can reverse opioid overdoses. While formal education programs are likely not necessary, presenting individuals information about naloxone can lead to increased knowledge and self-efficacy with respect to use (Carter & Caudill, 2020; Febres-Cordero et al., 2022). Many US cities now have formal naloxone training courses and centers that provide free access to naloxone (Lambdin et al., 2020). Even without formal training, laypersons can learn how to administer naloxone, and naloxone packets are often accompanied with information packets explaining how to use the product (Wheeler et al., 2015). When possible, people who use cocaine or people accompanying people who are using cocaine should have naloxone available.
Finally, more widespread information is needed about the availability and efficacy of fentanyl test strips. People who use cocaine or other illegal or illegally manufactured drugs can test their drugs for the presence of fentanyl prior to consumption. Fentanyl test strips, for example, tend to have high sensitivity and specificity in detecting fentanyl, but the caveat is that cannot detect all of the fentanyl analogs that continue to shift in availability (Palamar et al., 2020; Ti et al., 2020). They also cannot detect the presence of other drugs including other novel opioids. Since test strips can lead to a false sense of security, testing and use needs to continue with caution (Bergh et al., 2021). However, such testing has great potential to help prevent people who use cocaine from being unknowingly exposed to fentanyl. Historically, drug testing has been more commonplace and more accepted in some other countries (Brunt et al., 2016), but testing for fentanyl has recently gained acceptance throughout much of the US. In fact, as of 2021, federal government funds can be used to purchase test strips (Substance Abuse and Mental Health Services Administration, 2021). Regardless, drug checking—whether conducted by an organization or someone who plans on using the drug—increases knowledge of potential adulteration. As such, drug checking may be seen as a leading tool not only to detect the presence of fentanyl in drugs but also to educate people at risk.
This study is not without limitations. Results are not generalizable to the general population, and it is unknown to what extent these results are generalizable outside of NYC. The study was cross-sectional so changes could not be observed among participants over time. Data could not be collected in 2020 due to the COVID-19 pandemic and the sample size each year decreased over time, limiting precision of estimates in later years. Despite Black individuals comprising of 7.6% of the sample, within models, the number of Black individuals was too small, so these cases had to be included in the other race category. It is possible that the survey being limited to summer months affected estimates.
In conclusion, knowledge that cocaine can be adulterated with fentanyl is increasing in this high-risk population. There are still knowledge gaps, including among people who use cocaine. More research is needed to determine what has been driving these shifts in knowledge. People in this scene and the general public can benefit from more expansive information regarding fentanyl as an adulterant, about overdose response (e.g., naloxone), and about use of drug checking kits among those who use cocaine or other illegal drugs.
Acknowledgments:
Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Numbers R01DA044207 and K01DA038800. The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Declaration of Interest: The author has no conflicts to declare.
Data Sharing/Availability:
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- Ahmad FB, Rossen LM, & Sutton P. (2021). Provisional drug overdose death counts. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm#citation
- Allen B, Sisson L, Dolatshahi J, Blachman-Forshay J, Hurley A, & Paone D (2020). Delivering Opioid Overdose Prevention in Bars and Nightclubs: A Public Awareness Pilot in New York City. J Public Health Manag Pract, 26(3), 232–235. 10.1097/phh.0000000000001014 [DOI] [PubMed] [Google Scholar]
- Bergh MS, Øiestad Å ML, Baumann MH, & Bogen IL (2021). Selectivity and sensitivity of urine fentanyl test strips to detect fentanyl analogues in illicit drugs. Int J Drug Policy, 90, 103065. 10.1016/j.drugpo.2020.103065 [DOI] [PubMed] [Google Scholar]
- Brunt TM, Nagy C, Bucheli A, Martins D, Ugarte M, Beduwe C, & Ventura Vilamala M. (2016). Drug Testing in Europe: Monitoring Results of the Trans European Drug Information (TEDI) Project. Drug Testing and Analysis. 10.1002/dta.1954 [DOI] [PubMed] [Google Scholar]
- Carter G, & Caudill P (2020). Integrating naloxone education into an undergraduate nursing course: Developing partnerships with a local department of health. Public Health Nurs, 37(3), 439–445. 10.1111/phn.12707 [DOI] [PubMed] [Google Scholar]
- Ciccarone D (2021). The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Curr Opin Psychiatry, 34(4), 344–350. 10.1097/yco.0000000000000717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiSalvo P, Cooper G, Tsao J, Romeo M, Laskowski LK, Chesney G, & Su MK (2020). Fentanyl-contaminated cocaine outbreak with laboratory confirmation in New York City in 2019. Am J Emerg Med, 40, 103–105. 10.1016/j.ajem.2020.12.002 [DOI] [PubMed] [Google Scholar]
- Febres-Cordero S, Smith DJ, Wulkan AZ, Béliveau AJ, Gish A, Zine S, Fugitt L, & Giordano NA (2022). It’s what the community demands: Results of community-based emergency opioid overdose trainings. Public Health Nurs. 10.1111/phn.13151 [DOI] [PubMed] [Google Scholar]
- Ferrari L, Gerardo B, Rodriguez CR, Cases GG, Escudero P, Zar G, Pomies D, & Giannuzzi L. (2022). Massive intoxication due to cocaine adulterated with carfentanil. Toxicologie Analytique et Clinique, 34(3), S39. [Google Scholar]
- Hayashi K, Milloy MJ, Lysyshyn M, DeBeck K, Nosova E, Wood E, & Kerr T (2018). Substance use patterns associated with recent exposure to fentanyl among people who inject drugs in Vancouver, Canada: A cross-sectional urine toxicology screening study. Drug Alcohol Depend, 183, 1–6. 10.1016/j.drugalcdep.2017.10.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedegaard H, Miniño AM, Spencer MR, & Warner M (2021). Drug Overdose Deaths in the United States, 1999–2020. NCHS Data Brief(426), 1–8. [PubMed] [Google Scholar]
- Krieger MS, Goedel WC, Buxton JA, Lysyshyn M, Bernstein E, Sherman SG, Rich JD, Hadland SE, Green TC, & Marshall BDL (2018). Use of rapid fentanyl test strips among young adults who use drugs. Int J Drug Policy, 61, 52–58. 10.1016/j.drugpo.2018.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambdin BH, Bluthenthal RN, Wenger LD, Wheeler E, Garner B, Lakosky P, & Kral AH (2020). Overdose Education and Naloxone Distribution Within Syringe Service Programs - United States, 2019. MMWR Morb Mortal Wkly Rep, 69(33), 1117–1121. 10.15585/mmwr.mm6933a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, & Davis NL (2021). Trends and Geographic Patterns in Drug and Synthetic Opioid Overdose Deaths - United States, 2013–2019. MMWR Morb Mortal Wkly Rep, 70(6), 202–207. 10.15585/mmwr.mm7006a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, & Keyes KM. (2020). Trends in Drug Use among Electronic Dance Music Party Attendees in New York City, 2016–2019. Drug and Alcohol Dependence, 209, 107889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Le A, Acosta P, & Cleland CM. (2019). Consistency of Self-Reported Drug Use among Electronic Dance Music Party Attendees. Drug and Alcohol Review, 38(7), 798–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Fitzgerald ND, & Cottler LB (2021). Shifting awareness among electronic dance music party attendees that drugs may contain fentanyl or other adulterants. Int J Drug Policy, 97, 103353. 10.1016/j.drugpo.2021.103353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Rutherford C, Cleland CM, & Keyes KM (2022). Concerts, bars, parties, and raves: Differential risk for drug use among high school seniors according to venue attendance. Subst Abus, 43(1), 785–791. 10.1080/08897077.2021.2010253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamar JJ, Salomone A, & Barratt MJ (2020). Drug checking to detect fentanyl and new psychoactive substances. Curr Opin Psychiatry, 33(4), 301–305. 10.1097/yco.0000000000000607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park JN, Rashidi E, Foti K, Zoorob M, Sherman S, & Alexander GC (2021). Fentanyl and fentanyl analogs in the illicit stimulant supply: Results from U.S. drug seizure data, 2011–2016. Drug Alcohol Depend, 218, 108416. 10.1016/j.drugalcdep.2020.108416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ridpath A, Driver CR, Nolan ML, Karpati A, Kass D, Paone D, Jakubowski A, Hoffman RS, Nelson LS, & Kunins HV. (2014). Illnesses and Deaths Among Persons Attending an Electronic Dance-Music Festival - New York City, 2013. Morbidity and Mortality Weekly Report, 63(50), 1195–1198. [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2021). Federal Grantees May Now Use Funds to Purchase Fentanyl Test Strips https://www.samhsa.gov/newsroom/press-announcements/202104070200
- Ti L, Tobias S, Lysyshyn M, Laing R, Nosova E, Choi J, Arredondo J, McCrae K, Tupper K, & Wood E (2020). Detecting fentanyl using point-of-care drug checking technologies: A validation study. Drug Alcohol Depend, 212, 108006. 10.1016/j.drugalcdep.2020.108006 [DOI] [PubMed] [Google Scholar]
- Tilhou AS, Birstler J, Baltes A, Salisbury-Afshar E, Malicki J, Chen G, & Brown R (2022). Characteristics and context of fentanyl test strip use among syringe service clients in southern Wisconsin. Harm Reduct J, 19(1), 142. 10.1186/s12954-022-00720-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheeler E, Jones TS, Gilbert MK, & Davidson PJ (2015). Opioid Overdose Prevention Programs Providing Naloxone to Laypersons - United States, 2014. MMWR Morb Mortal Wkly Rep, 64(23), 631–635. [PMC free article] [PubMed] [Google Scholar]
- Zibbell JE, Aldridge AP, Cauchon D, DeFiore-Hyrmer J, & Conway KP (2019). Association of Law Enforcement Seizures of Heroin, Fentanyl, and Carfentanil With Opioid Overdose Deaths in Ohio, 2014–2017. JAMA Netw Open, 2(11), e1914666. 10.1001/jamanetworkopen.2019.14666 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


