INTRODUCTION
Nonalcoholic fatty liver disease (NAFLD) is chronic hepatic steatosis which is not secondary to genetic/metabolic disorders, infections, use of steatogenic medications, ethanol consumption, or malnutrition (1). In the United States, NAFLD is the most prevalent pediatric liver disease and is more common in adolescents than younger children(2, 3). NAFLD is associated with many adverse health consequences including cirrhosis, liver transplantation, and cardiovascular and metabolic diseases(4, 5).
Societies including the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the American Academy of Pediatrics recommend that children at risk for NAFLD be screened using the enzyme alanine aminotransferase (ALT)(1). In the SAFETY study, the biological upper limit of normal (ULN) for ALT was determined to be 22 U/L for females and 26 U/L for males(6). A prior study using National Health and Nutrition Examination Survey (NHANES) data from 2007–2010 found that based on the ULN, 10.7% of adolescents had elevated ALT(7). Recently, our group found a substantial increase in the incidence of NAFLD diagnoses in children in Southern California from 2009 to 2018(8), thus we speculated that the prevalence of NAFLD increased nationally as well. Therefore, the first goal of this study was to determine the prevalence of elevated ALT as a measure of suspected NAFLD in adolescents in the U.S. for the years 2011–2018.
Additionally, this study sought to include data from Asian American adolescents, as previous national estimates of elevated ALT did not include this demographic group. Asian American children are currently the fastest growing racial group nationally, and there are emerging data that they may also be at an increased risk for NAFLD(9). Recently, we observed that 9.5% of Asian American children with obesity in Northern California had an ALT level that exceeded the clinical action threshold of twice the biological ULN (2X-ULN). (9). Asian American children have been understudied nationally. Therefore, the second goal was to determine the prevalence of elevated ALT among Asian American adolescents in the U.S.
Finally, there is debate surrounding the optimal ALT threshold that should be used to identify children with NAFLD(6, 10–12). Clinical guidelines recommend that following screening, children with ALT levels more than twice the biological ULN (2X-ULN; ALT >44 U/L for females and >52 U/L for males(1)) are at higher risk for more severe disease and thus should have further diagnostic evaluation for NAFLD. This is primarily targeted to patients with obesity. These guidelines supply a framework to aid clinical decision making; however, the practical implications of the specific ALT threshold used on the prevalence of elevated ALT has not been evaluated. Therefore, the third goal of this study was to evaluate the prevalence of ALT up to 2X-ULN in adolescents with obesity.
METHODS
Study Population
NHANES is a serial, cross-sectional study with interviews and physical examinations meant to assess the health and nutritional status of adults and children in the United States. Data are publicly available for download on the Centers for Disease Control and Prevention (CDC) website(13). For this study, we used NHANES data from 2011–2018. These years were chosen because prior analyses examining elevated ALT prevalence in children included data up to 2010(7), whereas 2011 was the first year that Asian children were specifically sampled in NHANES(14). Study inclusion criteria were age 12 to 19 years with available data for race and ethnicity, weight, height, and ALT level. Phlebotomy was not performed for children younger than age twelve years. Parents or guardians provided information on race and ethnicity. Participants were excluded if they had a potential cause for elevated ALT other than NAFLD, including viral hepatitis, toxin exposure, or use of potentially hepatotoxic medications [6].
Definitions for Elevated ALT
ALT was measured using an enzymatic rate method. Reference data from the CDC were used to determine BMI percentiles, with healthy or underweight classified as <85th percentile, overweight as 85th to <95th percentile, and obesity as ≥95th percentile(15). For the overall cohort, an elevated ALT level was defined using the biological (ULN) threshold as >22 U/L in females and >26 U/L in males. For the higher risk group of children with obesity, we additionally examined patterns in ALT elevation based on an ALT threshold ranging from the ULN to 2X-ULN.
Data Analysis
SAS statistical software (version 9.4) and R (version 4.1.1)(13) were used for data analyses. NHANES data uses weighting to account for the complex survey design, survey non-response, and post-stratification adjustment to match the total population counts from the US Census Bureau. A weight was assigned to each sample person allowing a single person to have the proper weight for the population they represent. The stratification and clustering in NHANES were accounted for using the strata SDMVSTRA and clusta SDMVPSU parameter of Proc survey frequency in SAS.
Chi-square tests were used to compare the proportion with elevated ALT by age, sex, race/ethnicity, and BMI level. The Cochran-Armitage test for trend was used to examine the relationship of elevated ALT with age and higher BMI category. Weighted frequencies of elevated ALT and the 95% confidence intervals (CI) were calculated for each group (race/ethnicity, sex, and BMI category) using the ALT cut-points. Multivariable logistic regression was used to examine the independent associations of race/ethnicity and elevated ALT, adjusting for age, sex, and BMI level, reported as odds ratios (OR) with 95% CI. For adolescents with obesity, we also examined the prevalence of elevated ALT defined by continuous ALT thresholds between the ULN and 2X-ULN to explore the global relationship between ALT cut-point and observed prevalence of ALT elevation.
RESULTS
Study Population
There were 6,083 adolescents ages 12 to 19 years evaluated in NHANES from 2011–2018. After inclusion and exclusion criteria were applied (Supplemental Figure 1), the final analytic cohort comprised 4,613 adolescents, representative of 25.7 million adolescents nationally (Table 1). The prevalence of overweight was 17.1% and obesity was 23.9%.
Table 1:
Study Population Characteristics
| Characteristics | All groups (n = 4,613) |
Asian (n = 519) |
Black (n = 1,153) |
Hispanic (n = 1,510) |
White (n = 1,431) |
|---|---|---|---|---|---|
| Age, y, mean (SD) | 15.4 (2.2) | 15.5 (2.1) | 15.4 (2.2) | 15.3 (2.3) | 15.4 (2.2) |
| Sex, % (n) | |||||
| Male | 51 (2,354) | 51 (273) | 51 (595) | 52 (737) | 50 (749) |
| Female | 49 (2,259) | 49 (246) | 49 (558) | 48 (773) | 50 (682) |
| BMI Percentile, % (n) | |||||
| < 85th | 61 (2,721) | 74 (382) | 55 (618) | 54 (816) | 64 (885) |
| ≥85th – < 95th | 17 (788) | 13 (66) | 18 (198) | 19 (293) | 16 (231) |
| ≥ 95th | 22 (1,104) | 12 (71) | 28 (317) | 27 (401) | 20 (315) |
| ALT U/L, mean (SD) | 19.1 (14.3) | 18.6 (12.9) | 17.1 (11.3) | 20.6 (15.7) | 18.9 (14.3) |
All data within the chart represent characteristics of the weighted population. The raw numbers of participants within each category are shown in parenthesis demarcated as (n).
Prevalence of ALT above the ULN
Prevalence estimates for elevated ALT for all adolescents as well as for the subsets by race/ethnicity and BMI category using the biological cut-point (ULN) are shown in Table 2. At the ULN, 16.5% (95% CI: 15.2–17.9%) of all individuals had an elevated ALT. The proportion with elevated ALT was higher with each year of age (Cochran-Armitage trend test, p<0.001) and ranged from 12.3% among 12-year-olds to 24.2% among 19-year-olds. Elevated ALT was more prevalent in males (20.7%) than females (12.2%, p<0.001), and was higher across increasing weight categories: healthy weight 8.8%, overweight 13.9%, and obesity 39.5% (p <0.001). Notably, among adolescents with elevated ALT, 30.4% had healthy weight, 14.0% had overweight, and 55.5% had obesity. The prevalence of elevated ALT also varied by race and ethnicity: 21.8% among Hispanic, 16.5% among Asian, 15.8% among White, and 10.7% among Black adolescents (overall Chi-square p<0.001). In those with obesity, the prevalence of elevated ALT was 43.1% (95% CI: 34.5–58.7%) in Asian adolescents, 43.5% (95% CI: 38.4–48.7%) in Hispanic adolescents, 43.0% (95% CI: 36.9–49.4%) in White adolescents, and much lower at 20.7% (95% CI:16.2–25.7%) in Black adolescents. Among adolescents with overweight, Asian participants had significantly higher prevalence of elevated ALT (27.0%) than White (12.8%) or Black (8.4%) adolescents (p<0.01), with a trend towards higher prevalence compared to Hispanic adolescents (17.7%, p=0.06).
Table 2:
Prevalence of elevated ALT stratified by Ethnicity, Race and BMI category
| Group | BMI Category | Percent Elevated ALT | 95% CI |
|---|---|---|---|
| All | |||
| All | 16.5 | 15.2 – 17.9 | |
| healthy | 8.8 | 7.6 – 10.2 | |
| overweight | 13.9 | 11.1 – 17.1 | |
| obesity | 39.5 | 35.8 – 43.3 | |
| Asian | |||
| All | 16.5 | 13.4 – 20.0 | |
| healthy | 10.2 | 7.3 – 13.8 | |
| overweight | 27.0 | 16.6 – 39.3 | |
| obesity | 43.1 | 34.5 – 58.7 | |
| Black | |||
| All | 10.7 | 8.9 – 12.6 | |
| healthy | 6.4 | 4.6 – 8.5 | |
| overweight | 8.4 | 5.0 – 12.7 | |
| obesity | 20.7 | 16.2 – 25.7 | |
| Hispanic | |||
| All | 21.8 | 19.7 – 24.0 | |
| healthy | 12.3 | 10.1 – 14.8 | |
| overweight | 17.7 | 13.2 – 22.8 | |
| obesity | 43.5 | 38.4 – 48.7 | |
| White | |||
| All | 15.8 | 13.8 – 18.0 | |
| healthy | 8.1 | 6.3 – 10.1 | |
| overweight | 12.8 | 8.5 – 18.0 | |
| obesity | 43.0 | 36.9 – 49.4 |
Numbers displayed in the chart reflect the weighted prevalence
In a multivariable logistic regression analysis, adjusting for race and ethnicity, age, sex, and BMI category, Hispanic ethnicity, older age and male sex were significantly associated with higher odds of elevated ALT (Table 3). Males had two-fold higher odds of elevated ALT compared to females (OR 2.2, CI 1.7–2.7). Hispanic adolescents had higher odds of elevated ALT (OR 1.3, CI 1.1–1.6) while Black adolescents had 50% lower odds (OR 0.5, CI 0.4–0.7) compared to White adolescents, whereas significant differences were not seen for Asian adolescents (OR 1.3, CI 1.0–1.8). Overweight (OR 1.8) and obesity (OR 7.9) compared to healthy weight were also strongly associated with greater odds of elevated ALT.
Table 3.
Adjusted Odds of having elevated ALT
| Effect | Odds Ratio | 95% Confidence Interval | P-Value |
|---|---|---|---|
| Age, y | 1.2 | 1.2—1.3 | P <0.001 |
| Sex | |||
| Female | Reference | ------ | ------ |
| Male | 2.2 | 1.7—2.7 | P <0.001 |
| Race and Ethnicity | |||
| White, non-Hispanic | Reference | ------ | ------ |
| Asian, non-Hispanic | 1.3 | 1.0—1.8 | P = 0.10 |
| Black, non-Hispanic | 0.5 | 0.4—0.7 | P <0.001 |
| Hispanic | 1.3 | 1.1—1.6 | P < 0.05 |
| Body Mass Index | |||
| Healthy | Reference | ------ | ------ |
| Overweight | 1.8 | 1.3—2.4 | P < 0.001 |
| Obesity | 7.9 | 6.2—10.1 | P <0.001 |
Prevalence of Elevated ALT in Adolescents with Obesity from the ULN through 2X-ULN
Figure 1 examines the prevalence of elevated ALT across a continuous threshold of elevated ALT from the ULN to 2X-ULN to show the proportion of subjects that would be identified at each possible ALT cut-point among all adolescents with obesity. Overall, 6.6% of adolescents with obesity had ALT 2X-ULN. When stratified by race and ethnicity, 10.5% (CI 7.6–14.0) of Hispanic adolescents, 6.3% (CI 3.9–9.6) of White adolescents, 5.6% (CI 3.3–8.6) of Asian adolescents, and 3.3% (CI 1.7–5.9) of Black adolescents had ALT 2X-ULN or greater.
FIGURE 1.
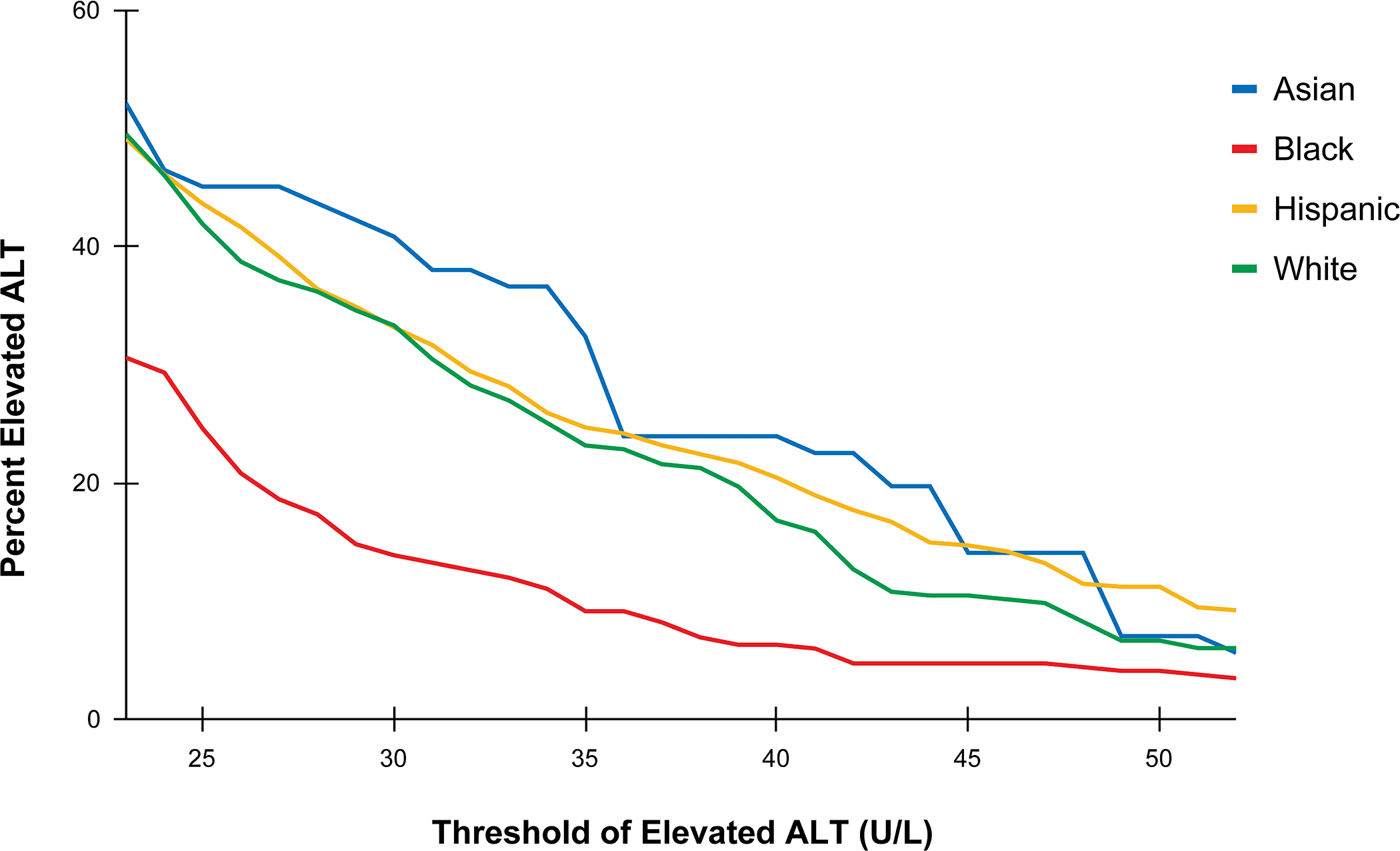
Figure shows the prevalence of elevated alanine aminotransferase (ALT) across a continuous threshold from the upper normal limit (ULN) to 2X-ULN of ALT for adolescents with obesity categorized by self-reported race or ethnicity.
DISCUSSION
In a nationally representative multiethnic cohort of adolescents ages 12 to 19 years (NHANES 2011–2018), the percentage of all adolescents with elevated ALT at the ULN was 16.5% but varied by race and ethnicity. The prevalence of elevated ALT was highest among Hispanic followed by Asian and White adolescents and lowest among Black adolescents. Among adolescents with overweight BMI, a higher proportion of Asian adolescents and lower proportion of Black adolescents had elevated ALT, whereas the prevalence of elevated ALT was similar among Asian, Hispanic, and White adolescents but lower for Black adolescents with obesity. Overall, the prevalence of elevated ALT was 39.5% at ULN and 6.6% at 2X-ULN among adolescents with obesity. Older age, male sex, overweight and obesity, and Hispanic ethnicity (vs. White race) were associated with greater odds of elevated ALT.
The prevalence of suspected NAFLD in adolescents has increased over time. Our research adds to prior studies using NHANES to evaluate the epidemiology of suspected NAFLD and how it has changed over time(7, 16, 17). Most recently, one study compared 1988–1994 and 2007–2010 NHANES cohorts and found that the prevalence of suspected NAFLD using the ULN increased substantially from 3.9% to 10.7% in adolescents (7). Our analyses identified much higher prevalence (16.5%) which in addition to the inclusion of adolescents with BMI < 85th percentile was also likely due to the higher proportion of NHANES participants with BMI in the obesity range in the current era and greater racial and ethnic diversity. While the previous study did not include adolescents with BMI in the underweight or normal weight percentile range (7), other studies have shown that 5.0–6.5% of children with normal and underweight BMI percentiles have NAFLD (3, 8). In our study, the prevalence of elevated ALT was 8.8% among adolescents with healthy weight. Given the vast number of children with normal BMI, even a small percentage with NAFLD is clinically relevant. Thus, although suspected NAFLD is increasing over time due to the increased prevalence of obesity, it is important to investigate the prevalence and risk factors for NAFLD in children of normal weight.
Asian Americans are one of the fastest growing ethnic groups, making up 6% of the total population in the United States(18, 19). However, NAFLD within Asian Americans is still understudied. The Study of Child and Adolescent Liver Epidemiology (SCALE) reported a high prevalence of NAFLD in Asian American children at 10.2% (95% CI 3.0–17.5%) (3). A 2015 study of 57 Chinese American children with obesity reported that 33% had an ALT greater than the ULN(20) and a meta-analysis encompassing many Asian countries reported a prevalence of NAFLD of 50.1% in children with obesity(21). A recent study from an integrated Northern California healthcare system found that 9.5% of Asian/Pacific Islander children and adolescents with obesity had elevated ALT above 2X-ULN (9). In the present study using NHANES data, the prevalence of elevated ALT at 2X-ULN was 5.6% among Asian Americans with obesity, however, due to a smaller number of Asian adolescents with obesity the confidence interval was wide ranging from 1.5 to 13.2%. It is unknown whether the composition of the Asian American population differed between studies. NHANES data on Asian Americans is self-reported and may include those with ancestry from Central, East, North, South, Southeast, and West Asia. Although the present data are more nationally representative than prior studies conducted using NHANES data, future studies would benefit from larger cohorts that can stratify Asian subgroups so that heterogeneity is not masked when Asian populations are combined for analyses (18).
Notably, there was a relatively high prevalence of elevated ALT at the ULN among Asian adolescents with overweight compared to White adolescents. This finding raises the question of whether Asian American adolescents are at increased risk for NAFLD at a lower BMI compared to other adolescents. Asian adults are known to have increased metabolic risk at lower BMI levels, including diabetes and cardiovascular disease(22), prompting a BMI threshold of BMI of >23 kg/m2 recommended for diabetes screening in these populations rather than a BMI of >25 kg/m2, the standard threshold for overweight or obesity (23, 24). Whether lower BMI intervention thresholds for Asian adolescents should be considered for metabolic screening of suspected NAFLD remains unaddressed in the pediatric population. Currently, children with overweight are only screened for NAFLD if there are added risk factors, which in one study of children with overweight in Southern California was only 24%(8). If Asian children with overweight are at increased risk for NAFLD, screening may be beneficial regardless of additional risk factors.
Our data also demonstrate that there may be a continuum of at-risk adolescents with obesity based on elevated ALT level, and that the number recommended for further workup for suspected NAFLD is substantially lower at 2X-ULN compared to ULN. Pediatric guidelines recommend using the clinical action threshold (2X-ULN) in children with obesity as a screening test for NAFLD; but it is unknown whether this is the best cut-point to use. There are major implications for selecting a specific screening value that may lead to widely different approaches for clinical care, emphasizing the need for more data to inform clinical action thresholds in different populations. Only a few studies have directly compared the ability of the ULN versus 2X-ULN to detect NAFLD in children (25) (26) and they demonstrate a notable compromise in sensitivity utilizing 2X-ULN (sensitivity 23–35%) compared to ULN (sensitivity 74–81%). Because 2X-ULN has a low sensitivity, its use may result in missed opportunity for further evaluation and potential diagnosis of NAFLD and its sequelae. Moreover, among children with NAFLD and ALT values between ULN and 2X-ULN, fibrosis is commonly reported(27). The degree of elevation of ALT is only moderately correlated with the severity of NAFLD(28–30). In cases series the mean ALT for those with steatohepatitis is approximately 30 U/L higher than those children who have NAFLD but not steatohepatitis, and the mean ALT is approximately 40 U/L higher in those with fibrosis than those without fibrosis. However, there is substantial person to person variation indicating there is no specific ALT level that correctly classifies disease severity.
Our study was limited by the cross-sectional nature of NHANES and the relatively small number of Asian American children included in NHANES when compared to adolescents of Black or White race, or Hispanic ethnicity. As such, the lower proportion of Asian adolescents with obesity limited the ability to fully examine the prevalence of elevated ALT at 2X-ULN within subgroups. Despite these limitations, our study is the first to address elevated ALT in Asian American adolescents at the national level and is further strengthened by the NHANES research sampling method which allows for best identification of a representative sample of individuals. Furthermore, despite the availability of only a single value of ALT given the cross-sectional nature of NHANES, we were able to exclude other causes of elevated aminotransferases, including known liver pathology, hepatotoxic medications, and viral hepatitis. To further determine a more precise screening threshold of ALT for NAFLD in adolescents, examination of both ALT and a reliable, non-invasive measure of steatosis such as magnetic resonance imaging proton density fat fraction (MRI-PDFF), a non-invasive quantitative and accurate measure of liver fat content(31) are needed. A study of sufficient ethnic diversity and magnitude will help assess where the most appropriate cut-point may be within the spectrum from the biological threshold/ULN to the clinical action threshold/2X-ULN.
Conclusions
The prevalence of elevated ALT, and thus suspected NAFLD, is high in U.S. adolescents and has increased over time. The choice of ALT threshold creates a vastly different number of adolescents who are recommended for further evaluation for suspected NAFLD. Our work also highlights the potential vulnerability of Asian American adolescents to NAFLD at a lower BMI level and this understudied population should be further investigated. Given the increasing prevalence of NAFLD and its disease burden, the optimal threshold of ALT that warrants further evaluation and diagnostic confirmation of NAFLD needs to be determined across different populations and has implications for epidemiologic studies and future clinical practice. Future work should continue to inform clinical guidelines as we further understand how elevated ALT relates to true NAFLD prevalence.
Supplementary Material
What is known:
Nonalcoholic liver disease (NAFLD) is a common liver disease in adolescents.
NAFLD is more common in Hispanic adolescents and less common in Black adolescents.
Asian American adolescents are a growing and understudied group who may be at risk for NAFLD.
What is new:
The prevalence of elevated ALT has increased to one in six adolescents in the U.S.
For Asian adolescents in the U.S., prevalence of elevated ALT was 16.5% overall, 27.0% in those with overweight, and 43.1% in those with obesity
Acknowledgement:
The University of California San Diego Institutional Review Board and the Research Determination Committee for the Kaiser Permanente Northern California region have determined the project does not meet the regulatory definition of research involving human subjects per 45 CFR 46.102(f)
Funding Sources:
The project was partially supported by the National Institutes of Health, Grant UL1TR001442. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
List of Abbreviations:
- NAFLD
Nonalcoholic fatty liver disease
- NHANES
National Health and Examination Survey
- ALT
alanine aminotransferase
- ULN
upper limit of normal
- 2X-ULN
twice the upper limit of normal
- BMI
body mass index
- CI
Confidence Interval
- OR
odds ratio
Footnotes
Disclosures: Authors report no conflicts of interest
REFERENCES
- 1.Vos MB, Abrams SH, Barlow SE, et al. NASPGHAN Clinical Practice Guideline for the Diagnosis and Treatment of Nonalcoholic Fatty Liver Disease in Children: Recommendations from the Expert Committee on NAFLD (ECON) and the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN). J Pediatr Gastroenterol Nutr 2017; 64:319–334. 10.1097/MPG.0000000000001482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fernandes DM, Pantangi V, Azam M, et al. Pediatric Nonalcoholic Fatty Liver Disease in New York City: An Autopsy Study. J Pediatr 2018; 200:174–180. 10.1016/j.jpeds.2018.04.047 [DOI] [PubMed] [Google Scholar]
- 3.Schwimmer JB, Deutsch R, Kahen T, et al. Prevalence of fatty liver in children and adolescents. Pediatrics 2006; 118:1388–1393. 10.1542/peds.2006-1212 [DOI] [PubMed] [Google Scholar]
- 4.Rubinstein E, Lavine JE, Schwimmer JB. Hepatic, cardiovascular, and endocrine outcomes of the histological subphenotypes of nonalcoholic fatty liver disease. Semin Liver Dis 2008; 28:380–385. 10.1055/s-0028-1091982 [DOI] [PubMed] [Google Scholar]
- 5.Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology 2015; 148:547–555. 10.1053/j.gastro.2014.11.039 [DOI] [PubMed] [Google Scholar]
- 6.Schwimmer JB, Dunn W, Norman GJ, et al. SAFETY Study: Alanine Aminotransferase Cutoff Values Are Set Too High for Reliable Detection of Pediatric Chronic Liver Disease. Gastroenterology 2010; 138:1357–1364.e2. 10.1053/j.gastro.2009.12.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Welsh JA, Karpen S, Vos MB. Increasing Prevalence of Nonalcoholic Fatty Liver Disease Among United States Adolescents, 1988–1994 to 2007–2010. J Pediatr 2013; 162:496–500.e1. 10.1016/j.jpeds.2012.08.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sahota AK, Shapiro WL, Newton KP, et al. Incidence of Nonalcoholic Fatty Liver Disease in Children: 2009–2018. Pediatrics 2020; 146. 10.1542/peds.2020-0771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu SJ, Darbinian JA, Schwimmer JB, et al. The Prevalence of Elevated Alanine Aminotransferase Levels Meeting Clinical Action Thresholds in Children with Obesity in Primary Care Practice. J Pediatr 2022; 240:280–283. 10.1016/j.jpeds.2021.09.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parker ML, Adeli K, Lévy É, et al. Are universal upper reference limits for alanine aminotransferase (ALT) appropriate for assessing pediatric liver injury? Clin Biochem 2018; 53:55–57. 10.1016/j.clinbiochem.2018.01.010 [DOI] [PubMed] [Google Scholar]
- 11.Fishbein MH, Miner M, Mogren C, et al. The Spectrum of Fatty Liver in Obese Children and The Relationship of Serum Aminotransferases to Severity of Steatosis. J Pediatr Gastroenterol Nutr 2003; 36:54–61. [DOI] [PubMed] [Google Scholar]
- 12.Stirnadel-Farrant HA, Galwey N, Bains C, et al. Children’s liver chemistries vary with age and gender and require customized pediatric reference ranges. Regul Toxicol Pharmacol 2015; 73:349–355. 10.1016/j.yrtph.2015.07.013 [DOI] [PubMed] [Google Scholar]
- 13.Anon. NHANES Questionnaires, Datasets, and Related Documentation. https://wwwn.cdc.gov/nchs/nhanes/Default.aspx. Accessed May 5, 2022
- 14.Paulose-Ram R, Burt V, Broitman L, et al. Overview of Asian American Data Collection, Release, and Analysis: National Health and Nutrition Examination Survey 2011–2018. Am J Public Health 2017; 107:916–921. 10.2105/AJPH.2017.303815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anon. SAS Program ( ages 0 to < 20 years ) | Resources | Growth Chart Training | Nutrition | DNPAO | CDC. https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. Published February 18, 2022. Accessed May 5, 2022
- 16.Strauss RS, Barlow SE, Dietz WH. Prevalence of abnormal serum aminotransferase values in overweight and obese adolescents. J Pediatr 2000; 136:727–733. [PubMed] [Google Scholar]
- 17.Fraser A, Longnecker MP, Lawlor DA. Prevalence of elevated alanine-aminotransferase (ALT) among US adolescents and associated factors: NHANES 1999–2004. Gastroenterology 2007; 133:1814–1820. 10.1053/j.gastro.2007.08.077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anon. NOT-HL-23–001: Notice of Special Interest (NOSI): Epidemiologic studies in Asian Americans, Native Hawaiians, and Pacific Islanders (Parent R01 Clinical Trial Not Allowed). https://grants.nih.gov/grants/guide/notice-files/NOT-HL-23-001.html. Accessed March 1, 2022
- 19.Budiman A, Ruiz NG. Key facts about Asian Americans, a diverse and growing population. Pew Research Center. https://www.pewresearch.org/fact-tank/2021/04/29/key-facts-about-asian-americans/. Accessed March 1, 2022 [Google Scholar]
- 20.Malespin M, Sleesman B, Lau A, et al. Prevalence and correlates of suspected nonalcoholic fatty liver disease in Chinese American children. J Clin Gastroenterol 2015; 49:345–349. 10.1097/MCG.0000000000000121 [DOI] [PubMed] [Google Scholar]
- 21.Zou Z-Y, Zeng J, Ren T-Y, et al. The burden and sexual dimorphism with nonalcoholic fatty liver disease in Asian children: A systematic review and meta-analysis. Liver Int n/a. 10.1111/liv.15080 [DOI] [PubMed] [Google Scholar]
- 22.Hsu WC, Araneta MRG, Kanaya AM, et al. BMI Cut Points to Identify At-Risk Asian Americans for Type 2 Diabetes Screening. Diabetes Care 2015; 38:150–158. 10.2337/dc14-2391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anon. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. The Lancet 2004; 363:157–163. 10.1016/S0140-6736(03)15268-3 [DOI] [PubMed] [Google Scholar]
- 24.American Diabetes Association. Introduction: Standards of Medical Care in Diabetes—2022. Diabetes Care 2021; 45:S1–S2. 10.2337/dc22-Sint [DOI] [PubMed] [Google Scholar]
- 25.Draijer LG, Feddouli S, Bohte AE, et al. Comparison of diagnostic accuracy of screening tests ALT and ultrasound for pediatric non-alcoholic fatty liver disease. Eur J Pediatr 2019; 178:863–870. 10.1007/s00431-019-03362-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lu Y, Wang Q, Yu L, et al. Revision of serum ALT upper limits of normal facilitates assessment of mild liver injury in obese children with non-alcoholic fatty liver disease. J Clin Lab Anal 2020; 34:e23285. 10.1002/jcla.23285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Molleston JP, Schwimmer JB, Yates KP, et al. Histological abnormalities in children with nonalcoholic fatty liver disease and normal or mildly elevated alanine aminotransferase levels. J Pediatr 2014; 164:707–713.e3. 10.1016/j.jpeds.2013.10.071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xanthakos S, Miles L, Bucuvalas J, et al. Histologic spectrum of nonalcoholic fatty liver disease in morbidly obese adolescents. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 2006; 4:226–232. 10.1016/s1542-3565(05)00978-x [DOI] [PubMed] [Google Scholar]
- 29.Schwimmer JB, Newton KP, Awai HI, et al. Paediatric gastroenterology evaluation of overweight and obese children referred from primary care for suspected non-alcoholic fatty liver disease. Aliment Pharmacol Ther 2013; 38:1267–1277. 10.1111/apt.12518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Newton KP, Hou J, Crimmins NA, et al. Prevalence of Prediabetes and Type 2 Diabetes in Children With Nonalcoholic Fatty Liver Disease. JAMA Pediatr 2016; 170:e161971. 10.1001/jamapediatrics.2016.1971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Middleton MS, Van Natta ML, Heba ER, et al. Diagnostic accuracy of magnetic resonance imaging hepatic proton density fat fraction in pediatric nonalcoholic fatty liver disease. Hepatol Baltim Md 2018; 67:858–872. 10.1002/hep.29596 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


