Abstract
Aims.
Alcohol biosensors, including the BACtrack Skyn, provide an objective and passive method of continuously assessing alcohol consumption in the natural environment. Despite the many strengths of the Skyn, six key challenges in the collection and processing of data include (1) identifying consumed alcohol; (2) identifying environmental alcohol; (3) identifying and determining the source of missing or invalid data; (4) achieving high participant adherence; (5) integrating Skyn and self-report data, and (6) implications for statistical inference. In this report we outline these challenges, provide recommendations to address them, and identify future needs.
Design and Settings.
Procedures from several laboratory and field-based pilot studies are presented to demonstrate practical recommendations for Skyn use. Data from a pilot study including a 7-day ecological momentary assessment period are also presented to evaluate effects of environmental alcohol on BACtrack Skyn readings.
Conclusions.
To address challenges in the collection and processing of data from the BACtrack Skyn alcohol biosensor, researchers should identify goals in advance of data collection to anticipate the processing necessary to interpret Skyn data. The Transdermal Alcohol Sensor Data Macro (TASMAC) Version 2.0 software can help process data rapidly; identify drinking events, missing data, and environmental alcohol; and integrate the sensor with self-report data. Thorough participant orientation and regular contact in field studies can reduce missing data and enhance adherence. Many recommended methods for Skyn use are applicable to other alcohol sensors and wearable devices.
Introduction
Transdermal alcohol biosensors provide an objective and passive method of continuously assessing alcohol consumption in controlled laboratory settings and the natural environment via transdermal alcohol concentration (TAC), a measurement derived from the small fraction (approximately 1%) of consumed alcohol excreted through the skin (1). Continuous monitoring of TAC via wearable sensors allows for minimally invasive biological assessment of drinking events, and provides quantitative details of those events (e.g., length of drinking event, rate of consumption). This method is valuable to alcohol research for numerous reasons, including limiting self-report burden and characterizing drinking behavior using metrics not available through other methods.
There has been recent growth in use of the commercially available BACtrack Skyn (https://skyn.bactrack.com), which won the National Institute on Alcohol Abuse and Alcoholism (NIAAA)-sponsored Wearable Alcohol Biosensor Challenge in 2016 (2). To date, wrist-worn biosensors such as the Skyn are the least invasive and most discrete of the few sensors that have been developed (3). The Skyn samples TAC every 20 seconds and connects via Bluetooth to a smartphone application which uploads data immediately upon syncing to a researcher portal. As recent work has clearly outlined the technical and procedural strengths and weaknesses of using the BACtrack Skyn in laboratory and field-based work (4–6), we will not summarize these issues here except to note that the Skyn manufacturer does not currently provide a set of rules for identifying alcohol consumption. While technical failures with early prototypes (7) appear to have improved (8,9), there remains a need to develop and disseminate optimal procedures for using these sensors in research and eventually clinical care. As such, the goal of the current report is to provide procedural recommendations that will support the growing body of research that uses the Skyn. We present several common challenges, followed by solutions that incorporate practical data collection and processing methods. Knowledge and example data from several laboratory and field-based pilot studies are presented to provide examples of these recommendations for use of the Skyn for a variety of purposes. Finally, we identify future directions necessary for optimizing the Skyn. We focus in this paper specifically on the Skyn, rather than other alcohol biosensors, as it is currently one only two that are broadly available. Many, though not all, of these recommendations can be applied to other alcohol biosensors.
Challenge #1: Identifying consumed alcohol
The primary data processing goal for most researchers using the Skyn is identifying and characterizing alcohol consumption. Skyn data are notoriously “noisy” as the data do not form a smooth curve from which a deviation (i.e., increase in TAC reflecting consumed alcohol) can be reliably detected. Moreover, a simple increase in TAC from a “baseline” level is not sufficient for identifying drinking episodes because: (a) environmental alcohol causes an increase in TAC (see Challenge #2) and (b) baseline TAC levels vary between- and within-person and between bracelets, often falling below zero (7,10). Given the variability of baseline, consumption is not always detectable at low levels of drinking (10,11).
Another widely used alcohol sensor, the Secure Continuous Remote Alcohol Monitoring (SCRAM) ankle monitor (Alcohol Monitoring Systems, Inc. [AMS]; Littleton, CO), provides access to a portal with individual reports confirming alcohol use for each monitor wearer. Revised criteria and additional rules for detecting alcohol use with the SCRAM have been developed and tested by researchers, resulting in detection of episodes with good sensitivity and specificity (12,13). For example, Barnett et al. adapted 1) Peak TAC, 2) absorption rate (i.e., the ascending limb of the TAC curve, calculated as peak TAC divided by time from last zero to peak), and 3) elimination rate (i.e., the descending limb: peak TAC divided by time from peak to next zero) criteria used by the SCRAM manufacturer to identify drinking episodes. Roache and colleagues (13) subsequently provide a set of rules that modify the rates and peak values and also identify outliers (e.g., implausibly high peaks, steep point-to-point changes) for exclusion or recoding. For the Skyn, Ash et al. (10) used area under the curve (AUC) to identify drinking days. Though promising, the results from Ash et al. were not consistent between cohorts, possibly due to differences in bracelet hardware versions. The lack of established and replicated criteria present a significant challenge for researchers who wish to use the Skyn for field-based data collections.
Recommendations:
In the absence of a well-tested set of criteria for determining drinking episodes, we recommend researchers consider adapting criteria such as those outlined in prior work (10,12,13). For example, the first rule from Roache et al. requires at least one positive TAC value preceded by at least two consecutive zero values. To use this rule with Skyn data it would need to be adapted to require (a) a larger number of positive TAC values, given the sampling rate is more frequent for Skyn (20 seconds versus 30 minutes for SCRAM) and (b) a higher value than zero (possibly tailored to the individual), as the baseline for Skyn often falls below or above zero during periods of known abstinence and is variable between persons and/or bracelets. Alternatively, this rule could be adapted to include a “changepoint” function such as those used by Fairbarn and colleagues (7) to identify a change in trend with reduced error. Until researchers identify the best set of criteria, it will be necessary to clearly describe the methods and calculations in research reports to allow for replication and additional tests of sensitivity and specificity. Recent work has adapted these rules for the Skyn to identify consumed alcohol in a small pilot study (14), providing an example of how this suggestion may be implemented. However, the sample was very small, and the methods for identifying cutoff values for temperature and various TAC metrics were not provided or were determined based on discussions with BACtrack personnel; additional criteria need to be considered in larger samples to empirically and efficiently determine the optimal criteria for identifying consumed alcohol.
We also recommend utilizing a standardized approach to processing Skyn data. For example, software previously developed by members of our team, the Transdermal Alcohol Sensor Data Macro (TASMAC) (15) was designed to accurately and efficiently process data from the SCRAM sensor and was recently updated to process Skyn data. The TASMAC (version 2.0)1 identifies alcohol episodes via user-defined criteria and produces figures and datasets with TAC parameters from each episode, including peak TAC, episode length, and area under the curve (AUC), allowing for faster data processing. The TASMAC 2.0 retains original features from the TASMAC that include producing datasets with variables of interest and plotting TAC at the day- or episode-level (see Figures 1–2). It also has new features, including a researcher-selected moving average to smooth TAC data at chosen intervals (e.g., 30 minutes) over time, which helps address “noise” in Skyn data (8). For biosensors that generate different output variables, these recommendations may need to be adapted.
Figure 1A. Example screenshots of datasets derived from TASMAC 2.0.
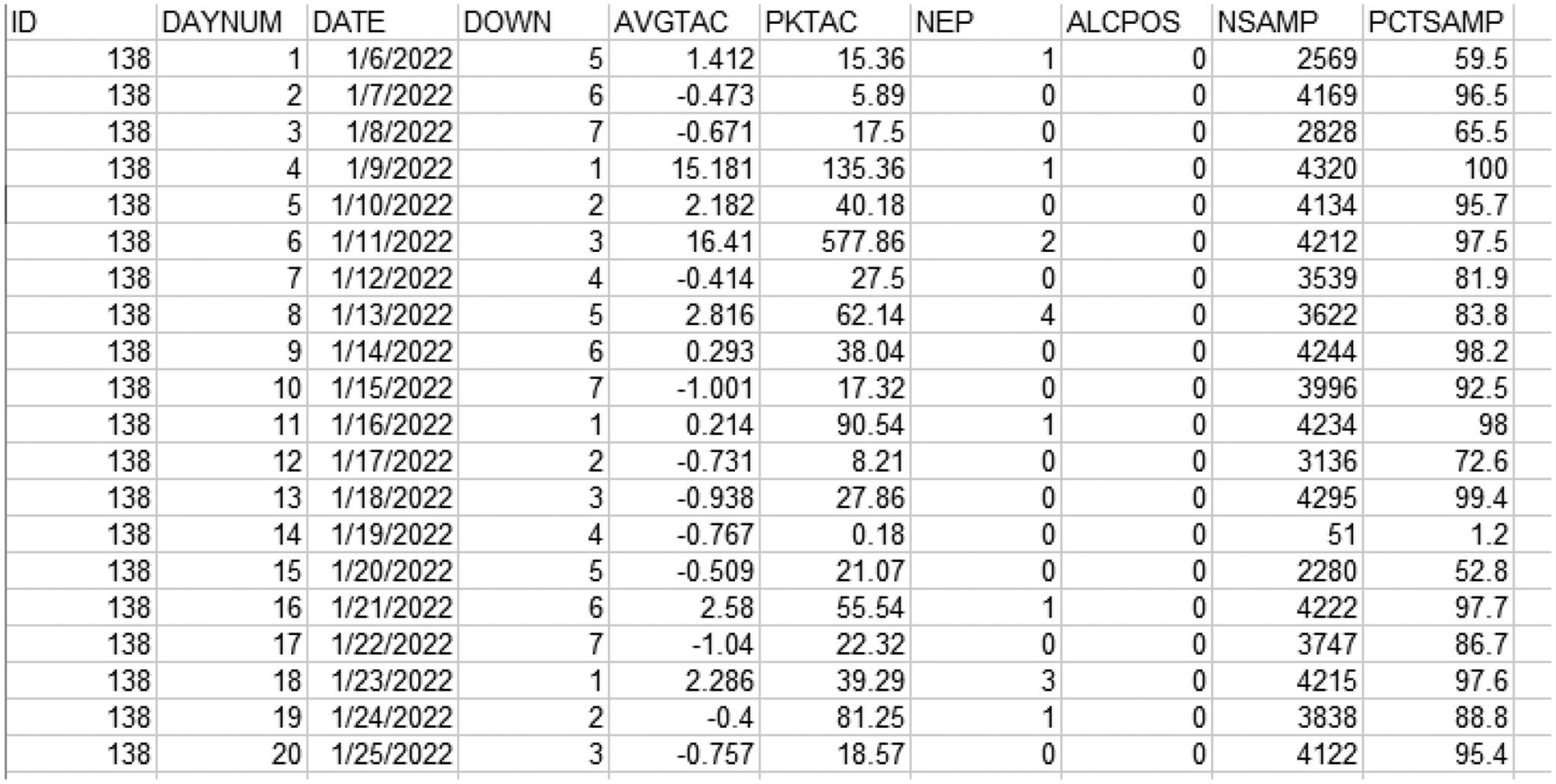
A: Day-level data for one participant across 20 days
Note. Example screenshot of dataset derived from the TASMAC where data is displayed at the day-level. ID = participant ID, DAYNUM = numbered day in the study, DATE = Date the data was collected, DOWN = day of week (numeric), AVGTAC = Average TAC (μg/L) from the full day (24 hour day defined by user), PKTAC = Peak TAC (μg/L) from the full day, NEP = number of potential drinking episodes detected, ALCPOS = whether day is considered alcohol positive (user-defined criteria), NSAMP = number of SKYN samples, PCTSAMP = percent samples of ideal day, at resolution. TAC values displayed here include raw data (PKTAC) and untransformed calculations from raw data (AVTAC), and may include extreme TAC values derived from potential environmental exposures (i.e., not necessarily reflecting consumed alcohol).
Figure 2A. Examples of known environmental alcohol.
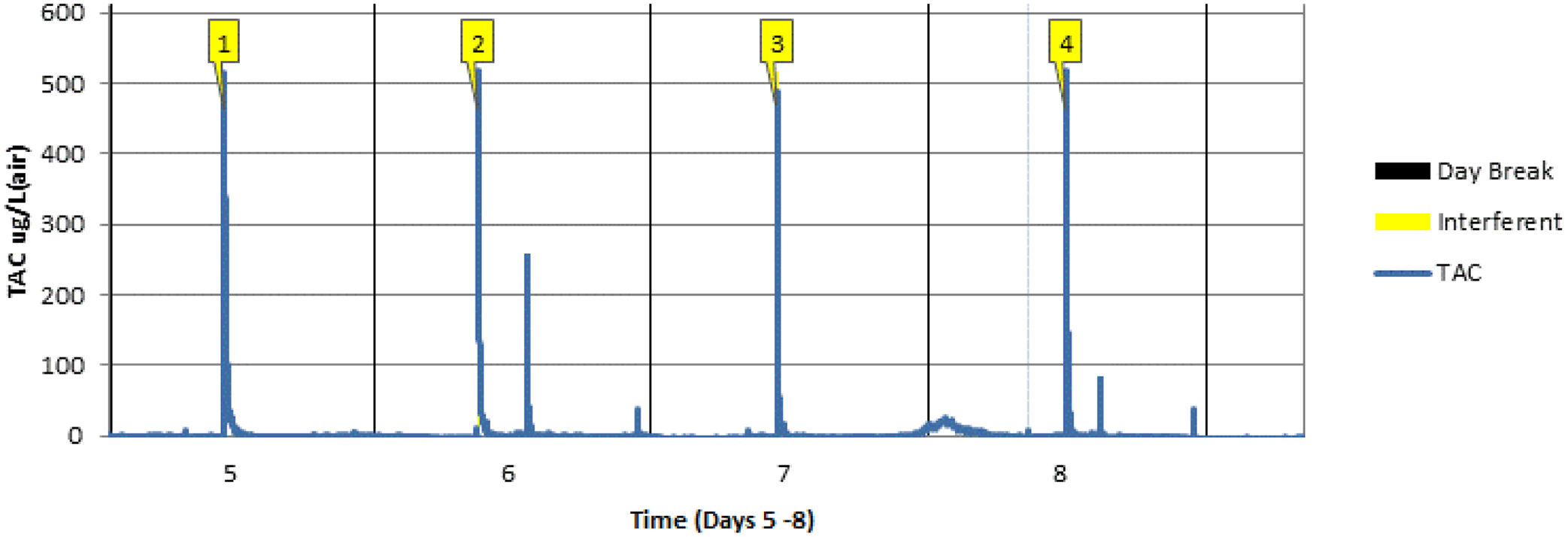
A: Outside of a drinking episode:
Note. Graph produced with TASMAC and displays selected known environmental alcohol (labeled and numbered in yellow) from a larger dataset.
Challenge #2: Identifying Environmental Alcohol
Alcohol-based products (e.g., hand sanitizer, spilled alcohol) can be detected and result in an elevated TAC. The incidence of environmental “interferents” is likely higher with wrist-worn biosensors such as the Skyn, compared to ankle-worn sensors, due to their more frequent exposure and closer proximity to one’s wrist (e.g., preparation of alcoholic drinks). Although environmental alcohol has been shown to have unique characteristics compared to consumed alcohol with the SCRAM, including steeper absorption and elimination rates and higher peaks (11,13,16), a protocol is required for systematically identifying and determining how to manage interferents detected by the Skyn (7,8). Figure 2A displays an example from pilot testing in which we interacted with environmental alcohol (e.g., hand sanitizer) and aligned the timing with TAC readings. As can be seen, environmental alcohol results in quick and dramatic increases in TAC. It is additionally challenging when incidental alcohol exposure occurs during drinking, impacting drinking data (including peak TAC and elimination or absorption rates; Figure 2B).
Figure 2B:
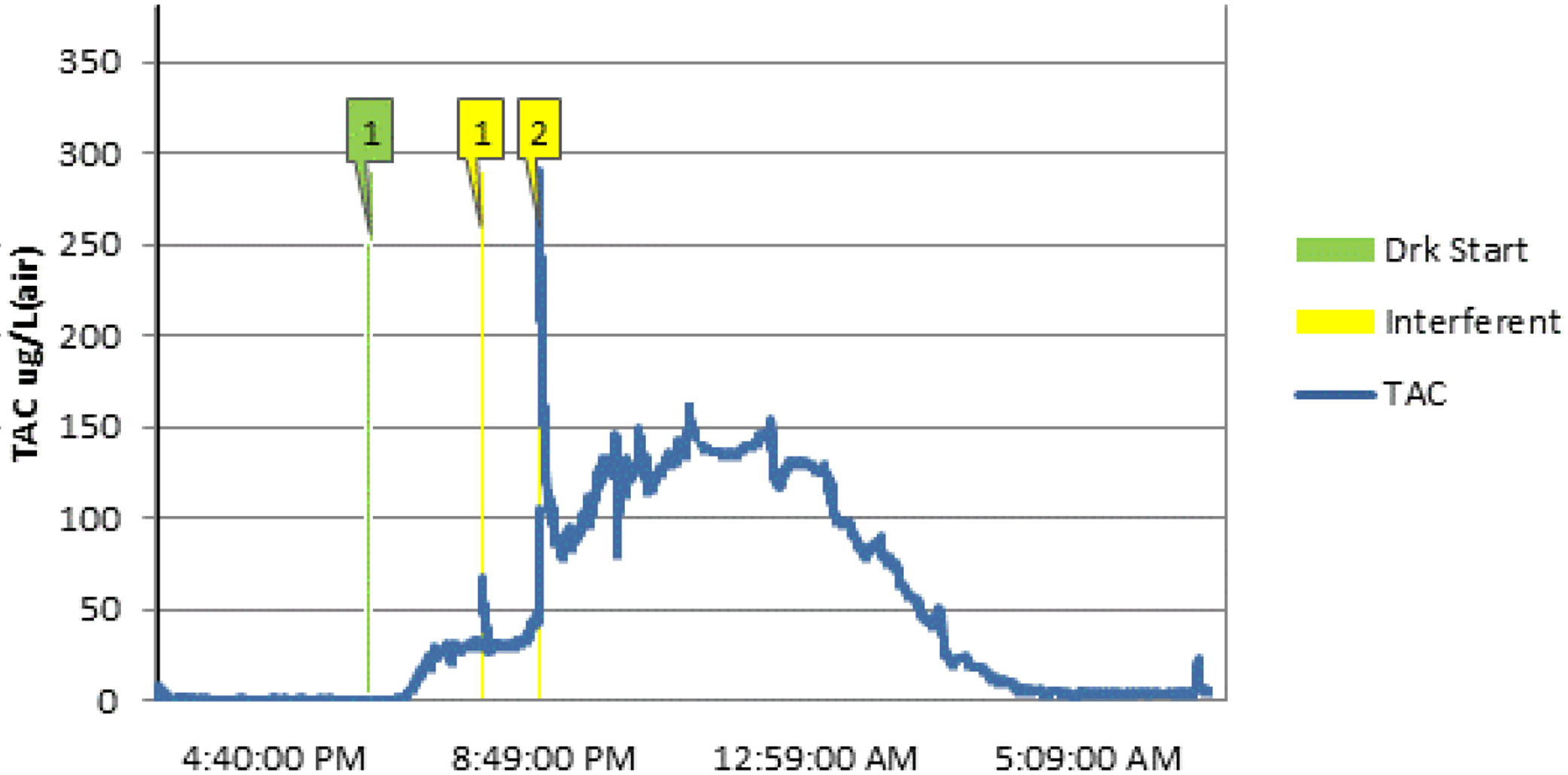
Known interferents (inside a drinking episode)
Note. Graph produced with TASMAC and displays selected known environmental alcohol interferents (labeled and numbered in yellow), from a larger dataset and self-reported drink start time (labeled in green).
Recommendations:
An automated approach (versus manual observation) for identifying and excluding sensor data that reflects environmental alcohol exposure is needed. The TASMAC 2.0 has the capacity for researchers to specify absorption, elimination, and peak rates that are outside of the range for consumed alcohol and therefore reflect environmental interferents. This allows researchers to either exclude data points labeled as outside of these ranges, or to replace them with temporally-near values that do not reflect interferents (see missing data consideration in Challenge #6). In Figure 2A, environmental alcohol is detected in the context of no consumed alcohol and could be replaced with lower (baseline) values. Exposure during a drinking event could be addressed by using a running average or eliminating data points reflecting the interferent, reducing its impact on metrics derived from TAC values during the drinking episode.
In addition to developing approaches to detect and minimize the impact of environmental interferents, we recommend researchers advise participants to avoid alcohol-based products when possible. Until parameters can be established for exposure to known interferents, it may also be valuable to collect self-reported timing of environmental alcohol exposure to confirm interferents by temporally aligning them with TAC values.
Challenge #3: Identifying and Determining the Source of Missing or Invalid Data
Wearable sensors inevitably result in missing data, some of which can be anticipated, and all of which must be identified and managed. Skyn missing data are expected when the bracelet is taken off for bathing or turned off for recharging (both currently recommended by the manufacturer). In addition, some participant non-adherence is expected; for example, participants may forget to charge the Skyn, or may remove it for reasons other than bathing or charging. Below we discuss distinctions between missing and invalid data and their sources.
Missing data (absence of data for some part of a time series), reflecting times when the bracelet is turned off and data therefore are not collected, will exist in many field-based protocols because the bracelet must be turned off during charging. Although the hardware has recently improved (the battery charge now lasts for seven days), protocols with data collection lasting more than seven days will require Skyn charging during participation. Lack of adherence to charging expectations, including failing to charge the bracelet or forgetting to power it on after charging, will result in missing data. Also, data may be missing if a participant does not consistently and properly sync their bracelet to the associated app, which is necessary for data to be accessible by researchers. Because the bracelet can only store approximately 72 hours of data in the current version, if syncing is not done in this time frame, data may be overwritten, leading to missing data. Finally, missing data may be due to unanticipated bracelet or app malfunctions.
Invalid data refers to data that are collected but are invalid due to the bracelet being powered on while not being worn. This can occur either as a function of a participant complying with the protocol (e.g., removing the bracelet prior to water exposure) or being non-compliant (e.g., removing the bracelet for reasons other than expected or instructed). This type of data is difficult to identify, as there is no objective way to determine whether a participant is wearing the bracelet. The current Skyn version provides measures of both temperature and motion, and the manufacturer has indicated that temperature values may assist with determining if the bracelet is being worn. However, we are not confident in using any particular temperature cutoff as a reliable indicator of bracelet removal, in part because body and ambient temperatures vary by day and season. Thus, there is currently no validated guidance on an objective measure of whether the bracelet is being worn at all times when data exist.
Although laboratory protocols can avoid most missing data, as bracelets need not be removed, field-based data collection is vulnerable to all types of missing or invalid data described above. In such studies, there is no clear approach to determining the nature of missing data. This poses problems for data analysis and for evaluating participant adherence, an essential step for many researchers conducting field-based studies using the Skyn.
Recommendations:
Researchers seeking to identify missing and invalid data should first consider how much missing data are expected to exist within a protocol (e.g., due to charging time needed based on protocol length). Knowing what to expect for missing data is the first step in categorizing it. We suggest that researchers using the Skyn in field work should engage in “active” field-based data collection. Incoming data should be checked frequently (we recommend daily) to ensure data are being received. If more data than expected are missing, it is critical to quickly follow up with participants to resolve the source, reinforce participant instructions, and consider how the missing data should be reflected in adherence calculations (see also Challenge #4).
Additionally, we suggest having participants self-report when the bracelet was removed for any reason. If powered on during these times (resulting in collected data), we recommend those data be categorized as missing, since alcohol consumption is unknown. If bracelet removal is not confirmed, researchers are at risk of incorrectly interpreting the absence of TAC values above baseline as evidence of no alcohol consumption. In protocols where there are contingencies (i.e., reinforcers) for not drinking, researchers will have to identify methods to ensure the bracelet is being worn by the participant (and not, for example, being worn by someone else or not being worn at all). Since we are aware of no methods for ensuring that a participant is wearing the device, we recommend researchers consider these limitations before using the Skyn for this type of research. This may not be necessary for biosensors that are not as easily removed as the Skyn or that have more objective indications of the wearer.
Challenge #4: Achieving High Participant Adherence
Participant adherence in studies using wearable sensors is critical to collecting the highest possible volume of quality data. While passive sensors may ultimately serve to reduce burden known to characterize other intensive longitudinal data collection approaches (e.g., ecological momentary assessment), their value will lie in the extent to which they are consistently and properly used by participants. Major sources of nonadherence in field research with alcohol sensors include not (a) understanding project expectations, (b) consistently recalling project expectations, (c) understanding the technology, and (d) being motivated to comply. Below we describe recommendations for each source.
Recommendations:
Solutions to non-adherence source (a), not understanding the project expectations, will depend somewhat on the population and the burden of the protocol. Regardless, it is critical to provide participants with a thorough study orientation where expectations for, and the importance of, following project procedures are established. We recommend repeating key points and using different training modalities (e.g., short videos; slide shows; personal demonstration; websites; providing screenshots, handouts, and emails for reference). Although we have conducted orientations remotely using conferencing software, it may not be advisable on all protocols or with all populations, as it is difficult to ensure participant engagement.
Instructional materials (e.g., handouts, tutorial videos) can guide and complement orientation sessions by providing clear directions for when and how to wear, charge, and sync the Skyn. Researchers may specify that the Skyn is meant to be worn overnight, especially following alcohol consumption. It is wise to require that participants wear the bracelet at all times except when charging, bathing, or swimming, to establish habit and ensure they will already have it charged and on their wrist when a drinking event occurs. Although the Skyn app is designed to sync automatically to the app via Bluetooth, it may not be advisable to rely on this feature. Rather, we recommend participants are instructed to sync their bracelet to the app at least once a day. Additionally, researchers should consult with the manufacturer for their latest troubleshooting techniques, and include these on participant instructional materials. Of note, these procedural recommendations and instructional materials will need to be adapted as new software and hardware are developed and would be unique for other biosensors.
To address non-adherence source (b), not remembering project expectations, it is critical to check incoming data frequently (e.g., daily) and to maintain regular participant contact. Daily adherence monitoring might include checking for long blocks of missing time (i.e., 6+ hours) and time of last data sync (the timestamp of the most recent sync appears in the BACtrack researcher portal). When data are not received, staff should troubleshoot in a timely fashion and remind participants to sync and/or charge their bracelet when necessary. We suggest scheduling a “check in” with participants a few days into a field-based protocol. Finally, sending automated reminders to participants to wear, charge, and sync the Skyn can be valuable.
To address source (c), not understanding the technology, we recommend repetitive demonstrations during orientation and providing participants with troubleshooting materials. Researchers should help participants understand common issues with the bracelet or application, and how to address them. During orientation, it is advisable to have participants practice and receive feedback on key tasks, such as how to properly turn on and off, wear and charge the bracelet, as well as troubleshooting potential issues (e.g., difficulties syncing the bracelet and app).
To address non-adherence source (d), not being motivated to comply, we recommend extra time screening, and considering excluding participants with questionable ability to comply. Participants might be asked whether they feel able to successfully complete the protocol, and whether they expect specific challenges to adherence (e.g., frequent traveling, swimming/hot tubs, beach trips). Participants also should be engaged early on, for example, by conveying the importance of the work and by treating them as a collaborator who is contributing to meaningful research. Likewise, establishing adherence-based compensation structures can motivate adherence. We recommend incentivizing Skyn adherence (including returning the bracelet to researchers at the end of study participation) separately from other parts of a protocol (e.g., daily surveys), and at short intervals (e.g., daily payments for wearing the Skyn). Researchers may also consider implementing a “matching bonus” that compensates participants for corroboration of self-report and TAC data above a certain percentage to reinforce both self-report and bracelet wearing.
In summarizing recommendations for enhancing adherence, it is important to note that conducting field research with wearable sensors can be time consuming for research staff. It is typical for such research to have multiple, frequent observations (baseline, field-based assessments, follow-ups) with different modalities (web-based, app-based in addition to wearable sensors), a need for managing technology inventory, overseeing participant screening, assessment and orientation, regular data checking, participant communications, and frequent troubleshooting. Depending on the number of participants and study-specific requirements for data tracking and participant contact, several staff members may be required to manage these tasks.
Challenge #5: Integrating self-report with Skyn data
Many current empirical applications of alcohol biosensors require integrating TAC and self-report (e.g., daily diary, ecological momentary assessment) data. It is often necessary to merge self-report data (e.g., drink start and stop time) with TAC data or to plot self-reported events onto TAC curves. Currently available statistical software can be used to merge datasets (17), but there are no best practices for viewing graphics and values from sensor and event-level data together.
Recommendations:
We recommend the use of standardized data processing to merge data from multiple sources. For example, the TASMAC 2.0 uploads event files containing user-defined information such as self-reports (e.g., drinking start/end time, number of drinks consumed, bracelet removal, interaction with an environmental interferent). Measures of breath alcohol concentration (BrAC) from a laboratory study can be defined and synced with TAC data by timestamp or plotted along TAC curves. Figure 3A–C displays TAC data seamlessly plotted with event file data, and the use of centered moving averages at 90 minutes. Researchers should pay particular attention to timestamp formatting when merging data from multiple sources, especially if participants are possibly crossing time zones, and specifically given the delay in TAC relative to BrAC (8).
Figure 3.
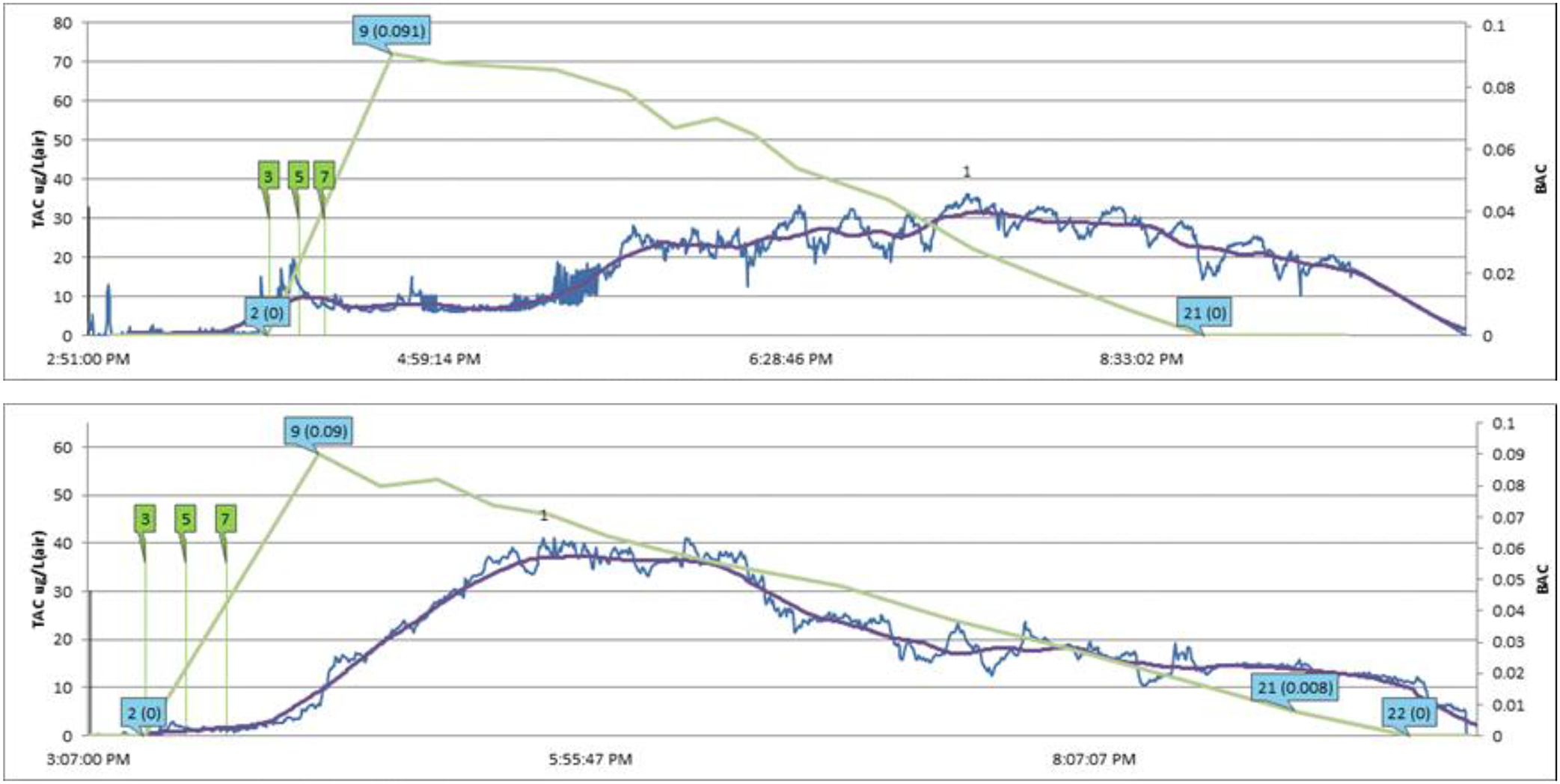
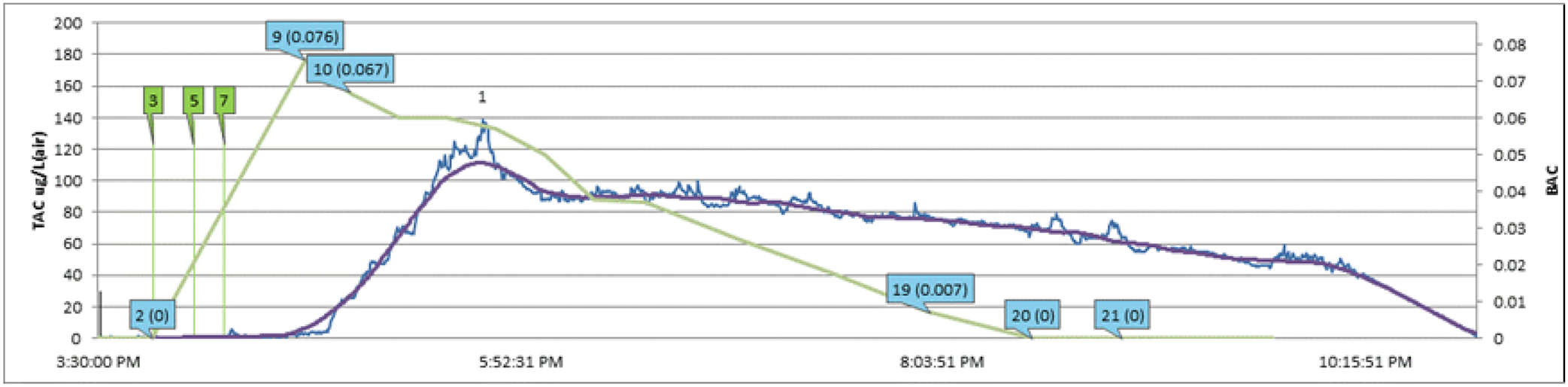
Example of TAC plots derived from TASMAC 2.0.
Note. Graphs produced with TASMAC and display raw TAC values (blue), TAC as centered running averages every 90 seconds (CAV 90, purple), laboratory measures BAC (green), observed drink start time (green vertical line) from three separate participants drinking within the same laboratory protocol.
Researchers should be mindful that although TAC data may reduce self-report burden, it does not eliminate the need for self-report in many research applications. Researchers may want to use sensor data to cross-validate self-report (or vice versa), or to capture drinking episodes that are not reported (18). Importantly, the strength of sensor data is that it can provide information about alcohol use that self-report data cannot validly or easily do (e.g., characterizing details of drinking episodes such as absorption or elimination rates). There also are numerous applications where self-report could measure affective or cognitive states, social contexts, or other constructs relevant for alcohol consumption. The TASMAC is a tool that allows the user to integrate self-report and sensor data for various purposes, including merging self-report data using date and timestamps. This merging can of course be done outside of the TASMAC, using standard statistical software, with data nested at the level appropriate for the research question. Researchers should consider using self-report and TAC data as complements to one another, as both have strengths and weaknesses. For instance, self-report data may be better suited for measuring precise timing (i.e., time of first drink or additional substance use within a drinking episode, since exact time of first drink cannot be derived from sensor data) or type of alcohol consumed. Self-report is also best for determining number of standard drinks, as TAC values vary greatly between-persons and do not readily translate to standard number of drinks. However, TAC data may be best used to measure length of drinking episode or pharmacokinetic factors like rates of alcohol absorption and metabolism (19).
Challenge #6: Implications for Statistical Inference
As many of the challenges reviewed above highlight, the time series data derived from the BACtrack Skyn require specialized attention and suggest specific analytic considerations, two of which we review here. Chief among the issues is the regular observation of missing data, and the reason for missing data should indicate how it should be managed analytically (20,21). An additional consideration is the between-person differences in TAC value ranges and baselines (7), which may impact distributional assumptions when modeling TAC data.
Recommendations:
Sources of data missingness are likely to vary significantly based on the type of biosensor being used (e.g., Skyn vs. non-removable devices such as the SCRAM). Regarding the analytic management of missing data, researchers should consider whether data are missing completely at random (MCAR), missing at random (MAR; missing systematically due to a known reason), or not missing at random (NMAR; missing data not predicted by available data or only by the variable of interest). As many analytic approaches assume data are MAR and the assumptions of MCAR are highly restrictive (and potentially violated if environmental interferent data are recoded as missing), researchers are urged to consider all potential predictors of missingness to ensure MAR assumptions are not violated before using common missing data approaches such as multiple imputation and full-information maximum likelihood (22). Regarding between-subject differences in TAC value ranges and baselines, it is suggested researchers always consider controlling for person-mean centered versus sample-mean centered between-person covariates within multilevel modeling approaches (23,24).
Summary/Recommendations
In summary, the BACtrack Skyn has great potential for researchers to collect objective behavioral drinking data. However, standard research guidelines for use of these devices in protocols and data analysis are needed. We aimed to identify a set of issues and provide associated “best practices” that researchers can use to guide their data collection (see Table 1). Although we have focused on research applications, many of these recommendations and procedures could ultimately be used in non-research applications, including clinical settings. For instance, providers of contingency-based interventions may be drawn to these devices as a method to passively measure drinking outcomes. However, given the limitations noted above regarding the inability to consistently identify the wearer of the Skyn, clinicians may need to consider secondary or additional methods upon which to base provision of reinforcers. Relatedly, depending on the desirability of an outcome in a contingency-based intervention, there may be differential impacts on the likelihood of behaviors intended to mislead the data collection (25). Some harm-reduction interventions may be more suited to utilizing a wearable alcohol sensor to review characteristics of consequential drinking events with patients, such as duration of drinking episode or rate of consumption. Research is needed in clinical treatment-seeking and treatment-engaged populations and controlled trials to determine the impact of the challenges noted here (5), and to identify other challenges within specific interventions or populations (26).
Table 1.
BACtrack Skyn data collection and analysis best practices
| Challenges | ||||||
|---|---|---|---|---|---|---|
| Recommendations | 1. Identifying consumed alcohol | 2. Identifying environmental alcohol | 3. Evaluating missing/invalid data | 4. Enhancing participant adherence | 5. Integrating self-report and TAC data | 6. Statistical Inference |
| Modify rules used for SCRAM drinking event detection for Skyn data | x | |||||
| Outline criteria used to identify drinking events | x | |||||
| Use standardized data processing (i.e., TASMAC 2.0) to identify drinking events in Skyn data | x | x | x | x | x | |
| Collect self-report of alcohol use | x | |||||
| Estimate expected amount of missing data based on protocol | x | |||||
| Collect self-report of bracelet removal | x | |||||
| Check incoming data frequently | x | x | ||||
| Establish protocols for frequent communication with participants | x | x | ||||
| Establish an adherence-based payment structure | x | |||||
| Send automated reminders to wear, charge, sync Skyn (to be complemented as needed by contact from a research staff member) | x | |||||
| Collect self-report of environmental interferents | x | |||||
| Thorough study orientation and instructional materials covering: | ||||||
| Importance of adherence | x | |||||
| How adherence impacts compensation | x | |||||
| How/when to charge Skyn | x | |||||
| How/when to properly wear Skyn | x | |||||
| Daily syncing to Skyn app | x | |||||
| Troubleshooting Skyn or Skyn app issues | x | |||||
| Avoid alcohol-based products when possible | x | x | ||||
| Examine sources of data missingness | x | |||||
| Consider controlling for between-person factors | x | |||||
One prominent message we hope to extend is that because of the relative infancy of this rapidly growing field, researchers will need to anticipate the cleaning and processing that will be necessary to interpret data prior to data collection and determine when self-reported data will add value to TAC readings. Further, use of different biosensors may have different implications for researchers. For example, since both the SCRAM and the Skyn have difficulty detecting low levels of alcohol consumption (10,11,16,27), researchers need to consider whether they will accept self-report of low-level drinking as a valid measure of alcohol consumption. Relatedly, when different representations of data exist (i.e., self-report and decisions about consumption from the sensor disagree), what will researchers use as the default value? Although TAC derived from confirmed drinking episodes can be used to draw important conclusions, such as rate of alcohol consumption or drinking episode length, data will be imperfect in determining whether drinking occurred due to its lower ability to detect low-level drinking, and the potential for bracelet removal. These and related important points need to be outlined prior to data collection and clearly described in research reports.
Future Directions
Several important future areas of research are needed to advance biosensor science for the Skyn or other wrist-worn devices. First, researchers should make use of the other information that the Skyn provides, including a systematic determination of how temperature or motion might be used to detect bracelet wear. Developing methods for reviewing and cleaning data are sorely needed to identify and categorize missing data as expected (e.g., compliant because of charging) or unexpected (e.g., noncompliant because no readings for an extended time). Another essential step for research is to examine data ranges for primary variables of interest (e.g., absorption rate, Peak TAC, elimination rate, AUC) to systematically identify both drinking episodes and environmental interferents confidently and rapidly during data analysis. Machine learning methods may be valuable towards this goal (5). Finally, while this manuscript focused on the challenges and recommendations associated with the sensor itself and the data it produces, the associated smartphone application has additional features (e.g., feedback on battery life, ability to see TAC curves) that are evolving and researchers must familiarize themselves with. As of this writing, the application provides no information on the user beyond TAC level. While observational studies may prefer to limit TAC feedback to participants to reduce the likelihood of reactivity, future research may use real-time feedback on TAC level for interventions. With these advancements, research with treatment- and non-treatment seeking samples holds tremendous potential to eliminate some limitations inherent to self-reported drinking data.
Figure 1B:
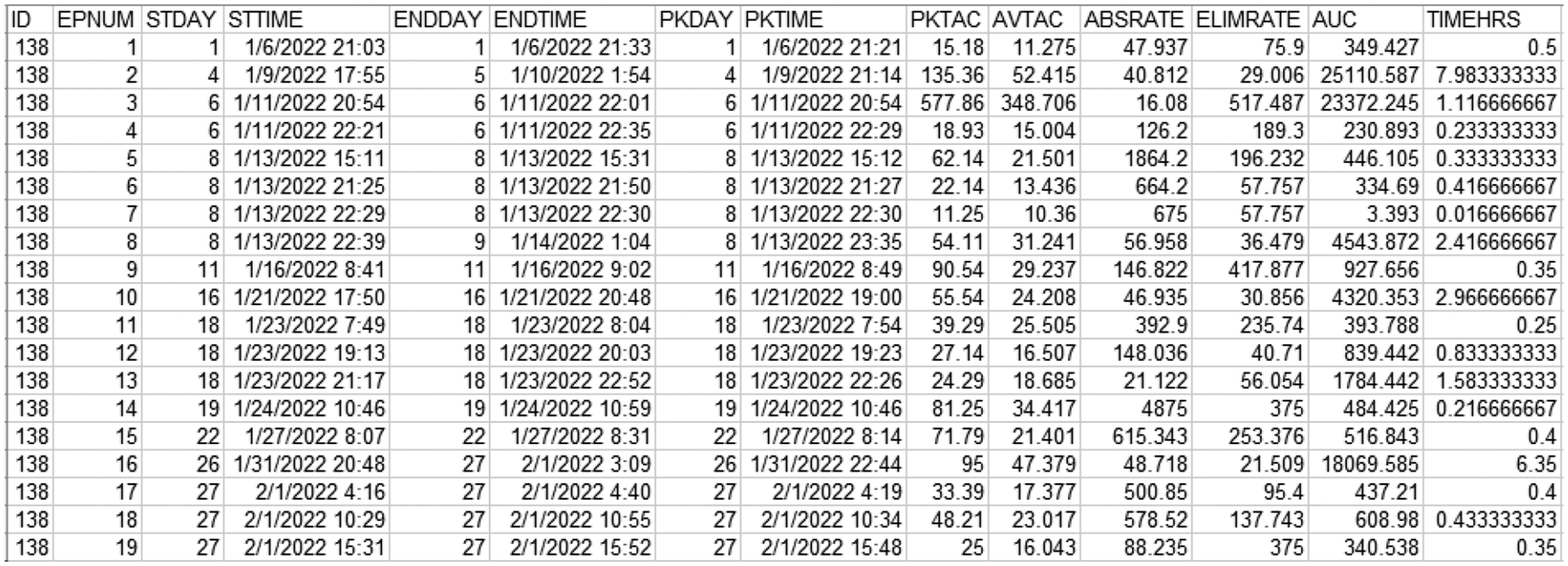
Episode-level data for one participant with 19 drinking episodes across 27 data collection days
Note. Example screenshot of dataset derived from TASMAC where data are displayed at the episode-level (defined by user-identified drinking criteria). EPNUM = sequentially numbered episode, STDAY = sequential day number of episode start, STTIME = timestamp of episode start, ENDDAY = sequential day number of episode end, ENDTIME = timestamp of episode end, PKDAY =sequential day number of episode peak TAC value, PKTIME = time of episode peak TAC value, PKTAC = Peak TAC (μg/L)of the episode, AVTAC = avg TAC (μg/L)of episode, ABSRATE = episode absorption rate, ELIMRATE = episode elimination rate, AUC = episode area-under-the-curve, TIMEHRS = elapsed episode time (hrs). TAC values displayed here include raw data (PKTAC) and untransformed calculations from raw data (AVTAC) and may include extreme TAC values derived from potential environmental exposures (i.e., not necessarily reflecting consumed alcohol).
Acknowledgments
This work was supported by the National Institute on Alcohol Abuse and Alcoholism: K08 AA027551 (PI Gunn), R01 AA027495 (PI Merrill), T32 AA007459 (PI Monti), R21 AA026918 (PI Leeman), R21 AA027191 (PI Wang) and a Center for Alcohol and Addiction Studies Research Excellence Award to Barnett, Gunn, and Merrill.
Footnotes
The authors have no conflicts of interest to declare (None).
Access to TASMAC 2.0 available at https://sites.brown.edu/tasmac/.
References
- 1.Swift R Direct measurement of alcohol and its metabolites. Addiction. 2003;98:73–80. [DOI] [PubMed] [Google Scholar]
- 2.NIAAA. NIAAA selects winners of its Wearable Alcohol Biosensor Challenge | National Institute on Alcohol Abuse and Alcoholism (NIAAA) [Internet]. [cited 2022 Jul 7]. Available from: https://www.niaaa.nih.gov/news-events/news-releases/niaaa-selects-winners-its-wearable-alcohol-biosensor-challenge [Google Scholar]
- 3.Davis-Martin RE, Alessi SM, Boudreaux ED. Alcohol Use Disorder in the Age of Technology: A Review of Wearable Biosensors in Alcohol Use Disorder Treatment. Front Psychiatry. 2021. Mar 22;12:642813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang Y, Fridberg DJ, Leeman RF, Cook RL, Porges EC. Wrist-worn alcohol biosensors: Strengths, limitations, and future directions. Alcohol. 2019;81(83–92). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fairbairn CE, Bosch N. A new generation of transdermal alcohol biosensing technology: practical applications, machine -learning analytics and questions for future research. Addiction. 2021. Oct;116(10):2912–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brobbin E, Deluca P, Hemrage S, Drummond C. Accuracy of Wearable Transdermal Alcohol Sensors: Systematic Review. J Med Internet Res. 2022. Apr 14;24(4):e35178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fairbairn CE, Kang D. Temporal dynamics of transdermal alcohol concentration measured via new-generation wrist-worn biosensor. Alcohol Clin Exp Res. 2019;43(10):2060–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang Y, Fridberg DJ, Shortell DD, Leeman RF, Barnett NP, Cook RL, et al. Wrist-worn alcohol biosensors: Applications and usability in behavioral research. Alcohol. 2021. May 1;92:25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ariss T, Fairbairn CE, Bosch N. Examining new-generation transdermal alcohol biosensor performance across laboratory and field contexts. Alcohol Clin Exp Res. 2022. Dec 12;acer.14977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ash GI, Gueorguieva R, Barnett NP, Wang W, Robledo DS, DeMartini KS, et al. Sensitivity, specificity, and tolerability of the BACTrack Skyn compared to other alcohol monitoring approaches among young adults in a field-based setting. Alcohol Clin Exp Res. 2022. May;46(5):783–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barnett NP, Meade EB, Glynn TR. Predictors of detection of alcohol use episodes using a transdermal alcohol sensor. Exp Clin Psychopharmacol. 2014;22(1):86–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barnett NP, Tidey J, Murphy JG, Swift R, Colby SM. Contingency Management for Alcohol Use Reduction: A Pilot Study using a Transdermal Alcohol Sensor. Drug Alcohol Depend. 2011;118(2–3):391–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roache AD, Karns-Wright JD, Goros TE, Hill-Kapturczak M, Mathias NW, Dougherty CW. Processing Transdermal Alcohol Concentration (TAC) data to Detect Low-Level Drinking. Alcohol. 2019;81:101–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Courtney JB, Russell MA, Conroy DE. Acceptability and validity of using the BACtrack skyn wrist-worn transdermal alcohol concentration sensor to capture alcohol use across 28 days under naturalistic conditions – A pilot study. Alcohol [Internet]. 2022. Dec 5 [cited 2023 Feb 7]; Available from: https://www.sciencedirect.com/science/article/pii/S0741832922001252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barnett NP, Souza T, Rosen IG, Luczak SE, Glynn TR, Swift R. Transdermal Alcohol Sensor Data Macro. Brown University; 2015. [Google Scholar]
- 16.Roache JD, Karns TE, Hill-Kapturczak N, Mullen J, Liang Y, Lamb RJ, et al. Using transdermal alcohol monitoring to detect low-level drinking. Alcohol Clin Exp Res Alcohol Clin Exp Res. 2015;39(7):1120–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Russell MA, Turrisi RJ, Smyth JM. Transdermal sensor features correlate with ecological momentary assessment drinking reports and predict alcohol-related consequences in young adults’ natural settings. Alcohol Clin Exp Res. 2022;46(1):100–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Richards VL, Barnett NP, Cook RL, Leeman RF, Souza T, Case S, et al. Correspondence between alcohol use measured by a wrist-worn alcohol biosensor and self-report via ecological momentary assessment over a 2-week period. Alcohol Clin Exp Res [Internet]. [cited 2023 Feb 20];n/a(n/a). Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/acer.14995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fridberg DJ, Wang Y, Porges E. Examining features of transdermal alcohol biosensor readings: A promising approach with implications for research and intervention. Alcohol Clin Exp Res. 2022;46(4):514–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hedeker D, Mermelstein RJ, Demirtas H. Analysis of binary outcomes with missing data: missing = smoking, last observation carried forward, and a little multiple imputation. Addiction. 2007;102(10):1564–73. [DOI] [PubMed] [Google Scholar]
- 21.Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychol Methods. 2002;7(2):147–77. [PubMed] [Google Scholar]
- 22.Sokolovsky AW, Mermelstein RJ, Hedeker D. Factors predicting compliance to ecological momentary assessment among adolescent smokers. Nicotine Tob Res. 2014;16(3):351–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang L (Peggy), Maxwell SE. On disaggregating between-person and within-person effects with longitudinal data using multilevel models. Psychol Methods. 2015;20:63–83. [DOI] [PubMed] [Google Scholar]
- 24.Hamaker EL The fixed versus random effects debate and how it relates to centering in multilevel modeling. - PsycNET. Psycholgical Methods [Internet]. [cited 2023 Feb 6];25(3). Available from: https://psycnet.apa.org/doiLanding?doi=10.1037%2Fmet0000239&errorCode=invalidAccess [DOI] [PubMed] [Google Scholar]
- 25.Barnett NP. Alcohol sensors and their potential for improving clinical care. Addiction. 2015;110(1):1–3. [DOI] [PubMed] [Google Scholar]
- 26.Richards VL, Rajendran S, Cook RL, Leeman RF, Wang Y, Prins C, et al. Identifying Desired Features That Would Be Acceptable and Helpful in a Wrist-Worn Biosensor–Based Alcohol Intervention: Interview Study Among Adults Who Drink Heavily. J Med Internet Res. 2023. Feb 2;25:e38713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Karns-Wright TE, Dougherty DM, Hill-Kapturczak N, Mathias CW, Roache JD. The correspondence between transdermal alcohol monitoring and daily self-reported alcohol consumption. Addict Behav. 2018. Oct;85:147–52. [DOI] [PMC free article] [PubMed] [Google Scholar]


