Abstract
Background:
Insufficient heat acclimatization is a risk factor for heat-related illness (HRI) morbidity, particularly during periods of sudden temperature increase. We sought to characterize heat exposure on days before, and days of, occupational HRIs.
Methods:
A total of 1241 Washington State workers’ compensation State Fund HRI claims from 2006 to 2021 were linked with modeled parameter-elevation regressions on independent slopes model (PRISM) meteorological data. We determined location-specific maximum temperatures (Tmax,PRISM) on the day of illness (DOI) and prior days, and whether the Tmax,PRISM was ≥10.0°F (~5.6°C) higher than the average of past 5 days (“sudden increase”) for each HRI claim. Claims occurring on days with ≥10 HRI claims (“clusters”) were compared with “non-cluster” claims using t tests and χ2 tests.
Results:
Seventy-six percent of analyzed HRI claims occurred on days with a Tmax,PRISM ≥ 80°F. Claims occurring on “cluster” days, compared to “non-cluster” days, had both a significantly higher mean DOI Tmax,PRISM (99.3°F vs. 85.8°F [37.4°C vs. 29.9°C], t(148) = −18, p < 0.001) and a higher proportion of “sudden increase” claims (80.2% vs. 24.3%, χ2[1] = 132.9, p < 0.001). Compared to “cluster” days, HRI claims occurring during the 2021 Pacific Northwest “heat dome” had a similar increased trajectory of mean Tmax,PRISM on the days before the DOI, but with higher mean Tmax,PRISM.
Conclusions:
Occupational HRI risk assessments should consider both current temperatures and changes in temperatures relative to prior days. Heat prevention programs should include provisions to address acclimatization and, when increases in temperature occur too quickly to allow for sufficient acclimatization, additional precautions.
Keywords: heat stress, heat wave, heat-related illness, illness cluster, workers’ compensation
1 |. INTRODUCTION
Occupational heat exposure is associated with substantial morbidity and mortality from heat-related illnesses (HRIs).1,2 Data from the US Bureau of Labor Statistics Census of Fatal Occupational Injuries database from 2000 to 2010 indicate a heat-related fatality rate of 0.22 per 1 million workers, with workers in agriculture and construction industries at the highest risk.2 Workers’ compensation claims analyses provide additional insight into nonfatal occupational HRIs. In Washington State (WA) from 2006 to 2017, there were 918 confirmed workers’ compensation HRI claims. The highest claims rates during the third quarter (July–September) occurred in the public administration and agriculture industry sectors (131.3 per 100,000 full-time employees [FTE] and 102.6 per 100,000 FTE, respectively).3 Estimates of HRI cases from workers’ compensation claims are likely underestimates, as occupational HRIs are not always identified and reported.3
There are several factors that contribute to occupational heat stress, including environmental heat exposure, clothing that insulates or prevents the body from cooling through evaporative heat loss, and physical activity that generates internal body heat. In addition to heat stress, lack of heat acclimatization can also increase the risk of HRI. Acclimatization is an improvement in heat tolerance that comes from repeated physical activity in hot, real-world settings (as opposed to “acclimation,” which occurs in laboratory settings).4 Physiological acclimatization involves increased skin blood flow, a greater maximum sweat rate, improved fluid balance, lower body temperature, reduced cardiovascular strain, and enhanced cellular protection. Physiological acclimatization takes up to 14 consecutive days to fully develop, with a substantial amount occurring in the first 5 days of activity in the heat.4 In the United States, between 2011 and 2016, 79% of outdoor worker heat deaths occurred among unacclimatized workers, defined as beginning a new job within the past 2 weeks or returning to work from an absence of more than 1 week.5 In WA, workers’ compensation claims occurring within 1 week of employment were more than four times more frequent for HRIs than for workers suffering from injuries from all causes.6
From a physiological perspective, an increase in heat exposure that occurs faster than a worker can acclimatize may pose a particular risk for adverse occupational health effects from heat, yet many established extreme heat definitions do not account for the rate of change of heat exposure in the days before extreme heat or provide a comparable metric from location to location. The US National Weather Service (NWS) excessive heat warning, excessive heat watch, heat advisory, and excessive heat outlook definitions depend on predicted heat thresholds and the likelihood of their onset and duration, with definitions that vary from jurisdiction to jurisdiction.7,8 The US NWS week-2 global probabilistic extreme forecasts tool, which informs the Climate Prediction Center’s official forecasts, utilizes daily forecasts of meteorological parameters exceeding the 85th percentile of 30-year historical distributions.9
Though the US Occupational Safety and Health Administration has published an Advance Notice of Proposed Rulemaking for heat, there is currently no federal occupational health and safety standard in effect to protect workers from heat exposure.10 Several US states, including California (CA), WA, Oregon, Maryland, and Nevada, have or are developing occupational outdoor heat rules that require protections for workers above different heat exposure levels (“triggers”).11–17 However, of currently active rules, only CA’s heat rule includes additional protections for workers exposed to changes in temperature, defined as above the trigger and “at least 10 degrees Fahrenheit higher than the average high daily temperatures in the preceding 5 days,” the latter of which we refer to as “sudden increase” conditions in this manuscript.
Days in which aggregations of HRI cases (“clusters”) occur represent days with a higher burden of HRI and an opportunity for additional preventive measures.18 HRI clusters derived from workers’ compensation data may represent the “tip of the iceberg” for HRI risk given that estimates of HRI cases from workers’ compensation claims are likely underestimates.3 A better understanding of claim characteristics and environmental conditions leading up to cluster days may help with the identification of particularly concerning conditions for workers and targeted prevention efforts. A prior analysis of WA workers’ compensation HRI claims raised the question of whether poor acclimatization may contribute to workers’ compensation HRI claims clusters.6
In the summer of 2021, the Pacific Northwest experienced unprecedented increases in temperature and temperature extremes during a “heat dome” event, in which heat was trapped by high-pressure atmospheric circulation. Although existing research in WA has separately demonstrated spatiotemporal variability in heat exposure19 and characterized HRI workers’ compensation claims,3,6 there is a gap in the characterization of spatiotemporal variability in changes in heat exposure on days leading up to HRIs among workers. Given the potential physiological and occupational health significance of insufficient acclimatization and the projected increase in the frequency and intensity of heat events in the future,20 we sought to characterize heat exposure on days leading up to the day of illness (DOI), including “sudden increase,” lagged, and cumulative exposure, among WA HRI workers’ compensation claims and clusters over space and time and by claim characteristics, including during the 2021 Pacific Northwest heat dome event.
2 |. MATERIALS AND METHODS
WA workers’ compensation HRI claims data from 2006 to 2021 were spatiotemporally joined with modeled gridded meteorological data to allow for the characterization of claims by heat exposure on prior days and the DOI.
2.1 |. HRI workers’ compensation claims
The WA Department of Labor and Industries (L&I) administers a single-payer workers’ compensation insurance system. WA employers are required to purchase workers’ compensation insurance through the L&I State Fund unless they meet financial and statutory requirements to self-insure or are covered by the federal government or other workers’ compensation systems. L&I’s State Fund covers approximately two-thirds of WA workers. HRI workers’ compensation claims and claim characteristics were identified using L&I insurance claim and employer data, as previously described.3 HRI claims occurring both indoors and outdoors were included and characterized, as described below. L&I has statutory obligations to compile and evaluate data for the purpose of controlling occupational injuries and illnesses, including HRI. WA L&I is a public health authority, and as such is allowed by 45 CFR 46.102(/)(2) to conduct public health surveillance to identify, monitor, assess, or investigate conditions of public health importance. The work presented here, which falls within public health surveillance activities as covered by the Common Rule, was performed in conjunction with L&I’s Division of Occupational Safety and Health rulemaking to update the requirements for controlling occupational heat exposure hazards, and approval by an institutional review board is not required.
HRI claims were identified using Occupational Injury and Illness Classification System (OIICS) codes21 and International Classification of Diseases Clinical Modification (ICD-CM) codes, as previously described.3 OIICS codes for which claims were identified corresponded to “exposure to environmental heat,” “effects of heat and light,” “heat-environmental,” or “sun,” and ICD-CM codes corresponded to “hyperosmolality and hypernatremia,” “volume depletion,” “acute renal failure,” “acute renal failure-unspecified,” “prickly heat,” “effects of heat and light,” “exhaustion due to exposure,” “exposure to excessive heat of man-made origin,” “exposure to excessive natural heat,” or “occupational exposure to extreme temperature.” Both ICD-9-CM and ICD-10-CM codes were used because WA L&I switched from using ICD-9 to ICD-10 on October 1, 2015. ICD codes are assigned by healthcare providers on the initial claim initiation form and subsequent healthcare bills and by claim adjudicators for allowed diagnoses. To improve the specificity of HRI claim identification, claims where the service dates of the first medical bill that identified treatment for dehydration and kidney failure were not within 1 day of the date of illness and where either dehydration or kidney failure was the sole means of identification were excluded.3 A total of 1330 WA State Fund claims with a date of illness between January 1, 2006 and December 31, 2021 were extracted on February 2, 2022. The date of the illness is derived from the “injury date” on the claim initiation form, which is presumed to be the date the worker experienced the HRI. Self-insured claims were not analyzed because of limitations in data, including limitations in ICD-CM code availability.
Additional data elements were extracted for each HRI claim. These elements included the claimant’s sex and date of birth (to compute age at the date of illness), six-digit North American Industrial Classification System (NAICS) codes,22 six-digit Standard Occupational Classification (SOC) codes,23 claim status (compensable vs. noncompensable for accepted claims), accident address (from the initial claim report), employer business location address, and address of the first healthcare provider visited by the claimant (from the first healthcare provider bill). Compensable claims are eligible for wage replacement (e.g., time-loss payments if the worker is unable to work after a 3 calendar-day waiting period), death, or disability benefits. We extracted both rejected and accepted claims. Claims may be rejected if there is insufficient information about the association between the HRI and the exposure. Previous analyses found that rejected claims occur in industries with high rates of HRI and therefore may be an important indicator of unmitigated heat stress.3 We also extracted the worker and employer “injury event description,” “job title/duty description,” and injury/accident site (e.g., job site, employer premises, other) from the initial claim form, and SOC description, NAICS description, and risk class description to determine whether the work setting where the claim occurred was “definitely outdoors,” “probably outdoors,” “unlikely outdoors,” or “uncertain,” using the procedure described in Supporting Information: Methods and Supporting Information: Table I. Workers’ compensation insurers group employers into insurance risk pools based on the type of work, with the assumption that employers performing similar work have a similar claim experience, and these risk classes are used to determine insurance premiums.
2.2 |. Heat exposure and linkage to claims data
The wet bulb globe temperature (WBGT), which considers dry air temperature, humidity, wind, and solar radiation, is considered the gold standard occupational heat exposure metric and is used by National Institute for Occupational Safety and Health (NIOSH)24 and American Conference of Governmental Industrial Hygienists (AC-GIH®)25 heat stress guidance. The original development of WA “trigger” temperatures implemented in the current WA occupational heat rule considered WBGT, clothing, and workload.26 Data on dew points in several WA cities were analyzed, and a dew point of 50°F (10.0°C), along with moderate metabolic rate work and work in the sun with different clothing ensembles were assumed to calculate corresponding dry air trigger temperatures for WBGT-based ACGIH® heat stress action limits. Given its policy relevance in WA, we focused on dry air temperature as the metric of heat exposure for our analysis.
We used maximum daily temperatures (Tmax,PRISM) derived from the parameter-elevation regressions on independent slopes model (PRISM),27 an accurate source of gridded weather data.28 PRISM was developed by the PRISM Climate Group at Oregon State University and incorporates climate observations from monitoring networks, applies quality-control measures and features spatial datasets at a 4 km pixel resolution for free downloading.29 PRISM models consider the location, elevation, topographic facet orientation, topographic position, orographic effectiveness of the terrain, coastal proximity, and vertical atmospheric layer.
We assigned one location per claim to link to environmental data for the analysis. We first geocoded the accident address, employer business location address, and address of the first healthcare provider using ArcGIS Pro 3.0 (ESRI), which assigns geocoding scores reflecting the accuracy of the match, from 0% to 100%. The Tmax,PRISM value corresponding to the PRISM grid cell that contained each location on the date of illness was then assigned to that location. The Tmax,PRISM was also extracted for the 5 days preceding the illness date in the same location. A single location was assigned to each claim using the previously published30 procedure outlined in Figure 1. Of the 1321 HRI claims with an accident location, business location, or first provider location in WA, 1241 (94%) HRI claims had a geocoding accuracy of at least 70%. Of these, 982 used the accident location (74%), 145 used the business location (11%), and 114 used the first provider location (9%). A spatial comparison of Tmax,PRISM with a previously published approach to generate linked maximum daily temperatures for WA HRI workers’ compensation claims on the DOI from weather station data,3 rather than modeled gridded data, is shown in Supporting Information: Figure 1. The mean (SD) difference in daily maximum temperature for all HRI claims on the DOI using the two maximum daily temperature identification methods was 1.3°F (6.5) (0.72°C [3.6]). In general, the largest discrepancy in values was in Western WA, where temperatures are generally cooler. A comparison of the 1241 claims included and the 89 claims not included in the analysis is presented in Supporting Information: Table II. Excluded claims were more likely to be rejected and be characterized by uncertainty about whether they occurred indoors versus outdoors.
FIGURE 1.
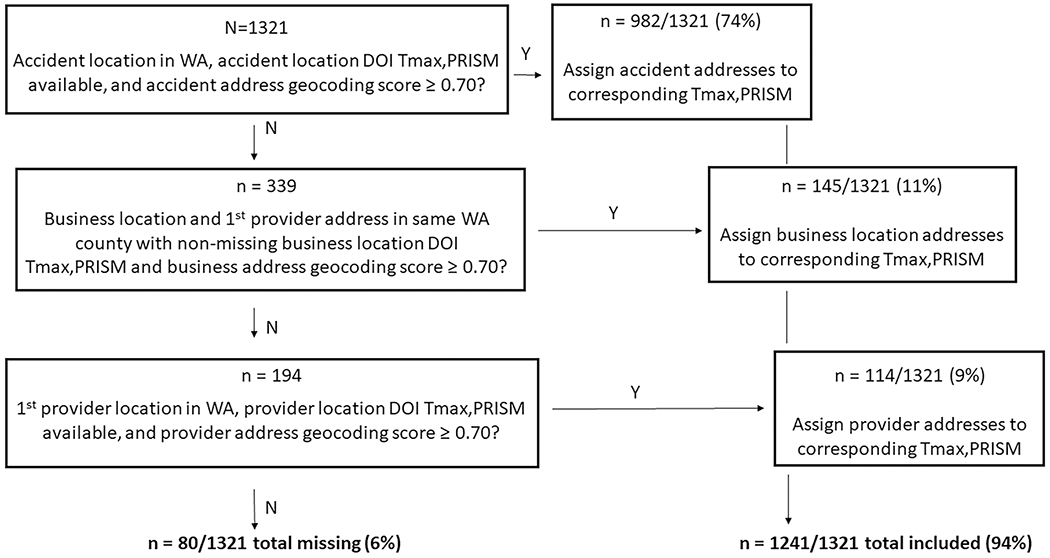
Study flow. DOI, day of injury/illness; PRISM, parameter-elevation regressions on independent slopes model; Tmax,PRISM, daily maximum temperature; WA, Washington State.
2.3 |. Analyses
We examined exceedances of Tmax,PRISM thresholds of 80°F (27°C) and 90°F (32°C) as these correspond to “trigger” and “high heat” thresholds, respectively, in the proposed updated WA heat rule for workers not wearing vapor barrier clothing.15 We also examined lagged temperatures (Tmax,PRISM on the 2 days before the date of illness) and cumulative exposure (average of temperatures on the prior 2 days and the DOI). We defined a “sudden increase” in temperatures to be consistent with CA’s occupational heat rule, and the proposed updated WA heat rule, as a day when Tmax,PRISM was at least 10.0°F (~5.6°C) greater than the average of the past 5 days.17 This definition is comparable to NIOSH’s heat stress guidance (“A heat wave is indicated when … the daily maximum temperature … is 5°C … or more above the maximum reached on the preceding days”).24
We summarized the characteristics of all HRI claims, HRI claims “clusters,” and HRI claims that occurred during the 2021 Pacific Northwest heat dome event (June 25–30, 2021).31 “Clusters” were defined based on the data as days with a frequency of claims at or above the 98th percentile (among days with more than one HRI claim), which corresponded to days with 10 or more claims. The mean Tmax,PRISM and the proportion of “sudden increase” claims by “cluster” size (number of HRI claims per day) is shown in Supporting Information: Figure 2. Venn diagrams, bar charts, line plots, and box plots were used to visualize HRI claims by claim characteristics, time, Tmax,PRISM, exceedances of thresholds, “sudden increase” exposures, and “clusters.” We developed county-level maps displaying the proportion of all HRI claims occurring on “cluster” days and days with a Tmax,PRISM at or above 80°F, excluding counties with fewer than five claims. We conducted unpaired Student’s t tests, assuming unequal variances, to compare DOI, the prior day, and cumulative Tmax,PRISM distributions of cluster versus noncluster claims. We assumed HRI claims were independent occurrences, as claims occurring on the same date at the same address are not commonly expected to occur. We used χ2 tests to compare the proportions of sudden increase “cluster” versus “non-cluster” claims. A p < 0.05 was considered statistically significant. Analyses were conducted using R studio, Version 1.3.1073.
3 |. RESULTS
3.1 |. HRI claim characteristics
Characteristics of all HRI claims and “cluster” claims are shown in Table 1. More than half of all HRI claims (65.4%) were accepted, and, of those, the majority (91.4%) were noncompensable. Claims were most common among workers aged 25–34 years (28.6%), males (80.1%), and those occurring from May to September (95.2%). 17.1% of claims were unlikely to have occurred outdoors. Characteristics of all HRI and HRI claims occurring on “cluster” days were similar, except “cluster” HRI claims were more likely to occur from May to September (no “cluster” claims occurred from October to April). There was a similar proportion of “definitely/probably” outdoor claims among “cluster” HRI claims and all HRI claims. There were 68 heat dome HRI claims, 38 (56%) of which were accepted and 17 (25%) of which were “unlikely outdoor.”
TABLE 1.
Included 2006–2021 HRI claim characteristics.
| Characteristic | Number of HRI claims (N = 1241) | Percent of HRI claims, % | Number of “cluster” (≥10/day) claims (n = 96) | Percent of “cluster” claims, % |
|---|---|---|---|---|
| Claim status | ||||
| Rejected | 430 | 34.6 | 32 | 33.3 |
| Accepted | 811 | 65.4 | 64 | 66.7 |
| Noncompensable | 741 | 91.4 | 59 | 92.2 |
| Compensable | 70 | 8.6 | 5 | 7.8 |
|
| ||||
| Age (years) | ||||
| <25 | 308 | 24.8 | 25 | 26.0 |
| 25–34 | 355 | 28.6 | 27 | 28.1 |
| 35–44 | 271 | 21.8 | 25 | 26.0 |
| 45–54 | 190 | 15.3 | 10 | 10.4 |
| 55–64 | 100 | 8.1 | 7 | 7.3 |
| 65+ | 17 | 1.4 | 2 | 2.1 |
|
| ||||
| Sex | ||||
| Male | 994 | 80.1 | 72 | 75.0 |
| Female | 247 | 19.9 | 24 | 25.0 |
|
| ||||
| Time of year | ||||
| May–Sep | 1181 | 95.2 | 96 | 100.0 |
| Oct-Apr | 60 | 4.8 | 0 | 0.0 |
|
| ||||
| Work setting a | ||||
| Definitely outdoor | 651 | 52.5 | 48 | 50.0 |
| Probably outdoor | 85 | 6.9 | 10 | 10.4 |
| Unlikely outdoor | 212 | 17.1 | 22 | 22.9 |
| Uncertain | 291 | 23.5 | 16 | 16.7 |
Abbreviation: HRI, heat-related illness.
Two observations missing.
3.2 |. Relationship of Tmax,PRISM ≥ 80°F (27°C), “sudden increase,” and “cluster” HRI claims
Figure 2 shows a Venn diagram detailing the relationship among Tmax,PRISM ≥ 80°F (27°C), “sudden increase,” and “cluster” HRI claims. The majority of all HRI claims occurred on days with a Tmax,PRISM at or above 80°F (27°C) (n = 938, 76%), with 29% classified as “sudden increase” days (n = 355), and 8% as “cluster” days (n = 96). Twenty-six (7%) of HRI claims that occurred on “sudden increase” days occurred on days below a Tmax,PRISM 80°F (27°C). When restricting to HRI claims “definitely” or “probably” occurring outdoors, 79% occurred on days at or above Tmax,PRISM 80°F (27°C), with 30% classified as “sudden increase” days, 8% as “cluster” days, and 6% of those occurring on “sudden increase” days occurring on days below a Tmax,PRISM 80°F (27°C). Of the 26 HRI claims occurring on “sudden increase” days when the Tmax,PRISM was below 80°F (27°C), the mean (SD) Tmax,PRISM was 77°F (3) (25°C [1.7]), with 46% of claims occurring in April and 54% occurring in May-August. All “cluster” claims occurred on days at or above Tmax,PRISM 80°F (27°C), and 90% occurred on days at or above Tmax,PRISM 90°F (32°C). Fifty-five (81%) of the 68 heat dome HRI claims occurred on “cluster” days.
FIGURE 2.
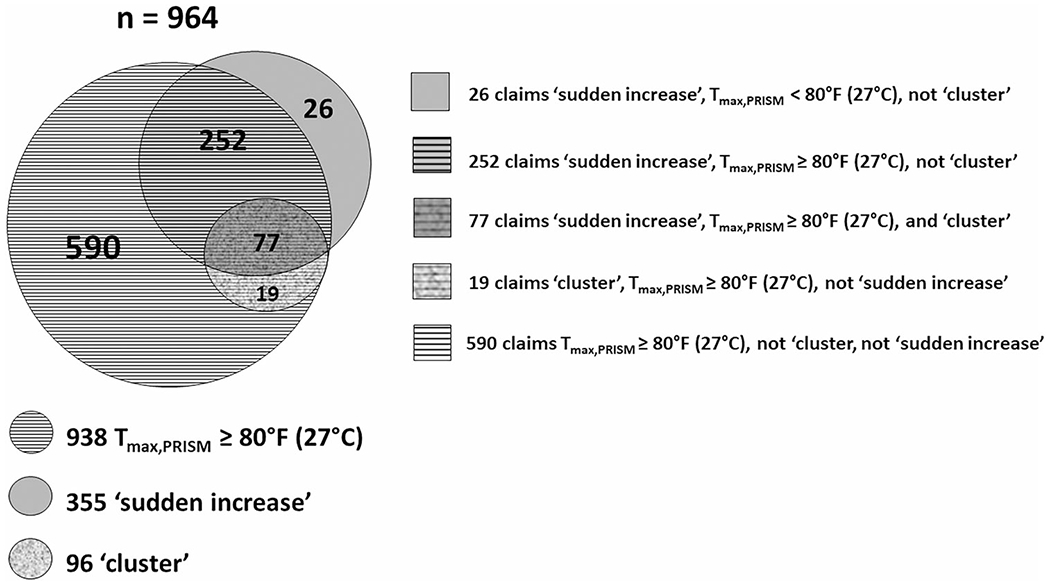
Venn diagram of the number of all 2006–2021 HRI claims occurring on “sudden increase,” “cluster” days, and/or days with Tmax,PRISM threshold exceedances ≥80°F (27°C), N = 964. HRI, heat-related illness; Tmax,PRISM, daily maximum temperature.
3.3 |. Time trends
The proportion of HRI claims occurring on “sudden increase” days and the mean Tmax,PRISM by year is shown in Figure 3. The number of all HRI claims, accepted HRI claims, and “definitely” or “probably” outdoor claims occurring on “sudden increase” days by year is shown in Supporting Information: Figure 3. The proportion of all HRI claims occurring on “sudden increase” days varied between 11.5% in 2017 and 47.0% in 2006, with an average of 28.6%. Among claims “definitely” or “probably” occurring outdoors, the proportion of HRI claims occurring on “sudden increase” days was 13.1% in 2017 and 45.0% in 2006. Following the implementation of the WA heat rule in 2008,11,12 several years had both elevated proportions of claims occurring on “sudden increase” days and with high mean Tmax,PRISM, including 2009 and 2021.
FIGURE 3.
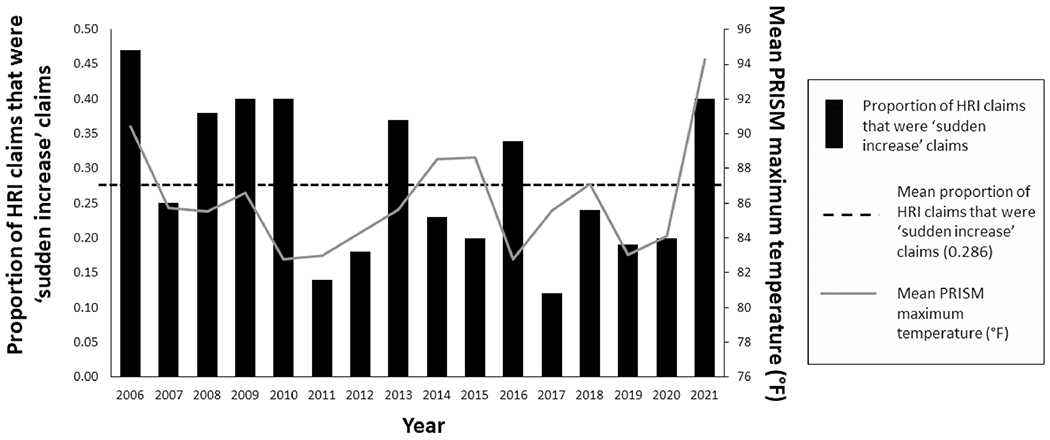
Proportion of all HRI claims occurring on “sudden increase” days by year, and corresponding yearly mean PRISM maximum temperature, N = 1241. HRI, heat-related illness; PRISM, parameter-elevation regressions on independent slopes model.
The number of HRI claims by month is shown in Figure 4 for “sudden increase” (Figure 4A) and “cluster claims” (Figure 4B). Claims occurring on “sudden increase” days were observed to have occurred as early as April (Figure 4A). During the 2021 heat dome year, the number of all HRI claims occurring on “sudden increase” days was the highest of all the study years and peaked in June. A similar pattern was observed for accepted HRI claims. Ninety percent of all HRI claims, and 88% of accepted HRI claims, occurring on “sudden increase” days in 2021 occurred in the month of June. “Cluster” claims, which occurred in 2007, 2009, and 2021, showed similar patterns of monthly peaks as “sudden increase” claims (Figure 4B). The number of all HRI claims by heat dome date in 2021 was 3 on June 25, 2 on June 26, 14 on June 27, 31 on June 28, 10 on June 29, and 8 on June 30.
FIGURE 4.
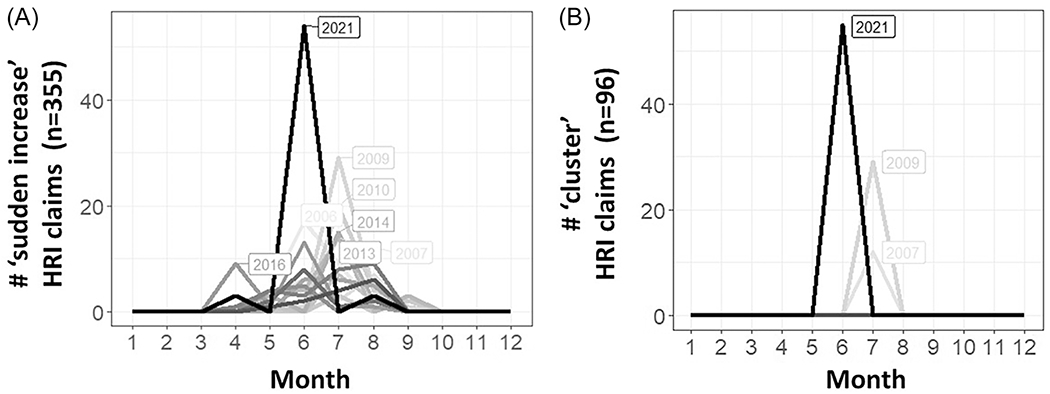
Number of 2006–2021 HRI claims by month and year for: (A) “sudden increase” claims (n = 355); (B) “cluster” claims (n = 96). HRI, heat-related illness.
3.4 |. Industry and occupation
The distribution of “sudden increase” HRI claims by industry, for industries with more than one HRI claim, is shown in Supporting Information: Table III. Compared to the percentage of all HRI claims occurring on “sudden increase” days (28.6%), among the industries with the top five number of all HRI claims, almost a third of HRI claims occurred on “sudden increase” days in construction and agriculture while the lowest proportion occurred in public administration (16%). When examining only HRI claims deemed to be “definitely” or “probably” outdoor, similar percentages of claims occurring on “sudden increase” days were seen for these industries (33% construction, 29% agriculture, 16% public administration), with an overall percentage of claims occurring on “sudden increase” days for “definitely” or “probably” outdoor HRI claims of 29.6%. When examining only accepted HRI claims, the percentage of claims occurring on “sudden increase” days for these industries was 35% for construction, 30% for agriculture, and 15% for public administration, with an overall percentage of claims occurring on “sudden increase” days for accepted HRI claims of 31.3%. Among the 96 “cluster” HRI claims, industries with the top number of claims on all “cluster” days together were administrative and support and waste management and remediation (n = 13 claims), construction (n = 13 claims), and agriculture (n = 11 claims). Among the 68 heat dome HRI claims, industries with the top number of claims on all heat dome days together were administrative and support and waste management and remediation (n = 10 claims) and agriculture (n = 8 claims).
Among HRI claims with available SOC codes, the proportion of all HRI claims occurring on “sudden increase” days for the occupations with the top number of HRI claims was 23% for farmworkers and laborers, 31% for construction craft laborers, and 34% for laborers and freight workers. Twelve percent of HRI claims occurred on “sudden increase” days for firefighters. When examining only HRI claims “definitely” or “probably” outdoor claims, similar proportions of “sudden increase” claims were seen for these occupations (24% farmworkers and laborers, 30% construction craft laborers, 34% laborers and freight workers, 13% firefighters). When examining only accepted HRI claims, the percentage of claims occurring on “sudden increase” days for these occupations was 25% for farmworkers and laborers, 31% for construction craft laborers, 41% for laborers and freight workers, and 10% for firefighters. The occupations with the highest number of claims on all “cluster” days together were farmworkers and laborers (n = 7 claims) and laborers and freight workers (n = 7). Among the 68 heat dome HRI claims, the occupation with the top number of claims on all heat dome days together was farmworkers and laborers (n = 6 claims).
3.5 |. Heat exposure characteristics
Exposure characteristics of days with a cluster of 10 or more HRI claims are shown in Table 2 for all HRI claims and, for claims “definitely” or “probably” occurring outdoors, in Supporting Information: Table IV. The percent of HRI claims that occurred on “sudden increase” days was significantly higher for “cluster” claims compared to “non-cluster” claims (80.2% vs. 24.3%, χ2(1) = 132.9, p < 0.001). The mean Tmax,PRISM on the DOI and the day prior were significantly higher for “cluster” claims compared to “non-cluster” claims (99.3°F vs. 85.8°F [37.4°C vs. 29.9°C], t(148) = −18, p < 0.001 and 94.0°F vs. 83.6°F [34.4°C vs. 28.7°C], t(128) = −11, p < 0.001), respectively. These significant mean Tmax,PRISM differences between “cluster” and “non-cluster” claims held true for 2 days prior (87.7°F vs. 81.7°F [30.9°C vs. 27.6°C], t(139) = −7, p < 0.001) and the average of the 2 consecutive previous days and DOI (93.7°F vs. 83.7°F [34.3°C vs. 28.7°C], t(137) = −13, p < 0.001, respectively). Similar inferences were seen in a sensitivity analysis that included only claims “definitely” or “probably” occurring outdoors and sensitivity analyses that considered “cluster” claims as those occurring on days with seven, three, and two or more claims (days with a frequency of claims at or above the 95th, 70th, and 45th percentiles, among days with more than one HRI claim) (Supporting Information: Figure 4 and Table V). The latter sensitivity analyses raise the question of whether larger “cluster” sizes exhibit steeper increases in and higher absolute Tmax,PRISM leading up to the DOI. These sensitivity analyses also suggest that “clusters” with as few as two or more HRI claims exhibit higher mean Tmax,PRISM than “non-cluster” claims (Supporting Information: Table V). The mean daily heat exposure metrics on heat dome HRI claim DOI, prior 2 days, and cumulative exposure were higher than the means for all “cluster” days (Table 2).
TABLE 2.
Characteristics of days with a cluster of 10 or more HRI claims among all 2006–2021 HRI claims.
| Dates | # HRI claims | # “Sudden increase” claims | % HRI claims that were “sudden increase” claims | Mean (SD) DOI Tmax,PRISM (°F) | Mean (SD) DOI-1 Tmax,PRISM (°F) | Mean (SD) DOI-2 Tmax,PRISM (°F) | Mean (SD) cumulative 3 day average (DOI, DOI-1, DOI-2) Tmax,PRISM (°F) |
|---|---|---|---|---|---|---|---|
| 7/11/2007 | 12 | 10 | 83.3 | 91.0 (4.7) | 81.2 (6.5) | 76.9 (7.1) | 83.0 (5.9) |
| 7/28/2009 | 15 | 10 | 66.7 | 94.6 (4.1) | 89.2 (3.4) | 87.1 (2.9) | 90.3 (3.3) |
| 7/29/2009 | 14 | 13 | 92.9 | 95.0 (3.8) | 92.1 (3.4) | 86.2 (3.8) | 91.1 (3.3) |
| 6/27/2021 | 14 | 11 | 78.6 | 100.3 (2.2) | 89.6 (3.6) | 84.1 (4.3) | 91.3 (2.9) |
| 6/28/2021 | 31 | 27 | 87.1 | 104.1 (3.7) | 100.9 (3.1) | 90.4 (3.9) | 98.4 (3.1) |
| 6/29/2021 | 10 | 6 | 60.0 | 106.6 (4.9) | 104.1 (5.7) | 100.7 (3.6) | 103.8 (4.7) |
| All above “cluster” dates | 96 | 77 | 80.2 | 99.3 (6.5) | 94.0 (8.4) | 87.7 (7.4) | 93.7 (7.0) |
| All heat dome dates | 68 | 49 | 72.1 | 103.0 (6.9) | 98.7 (8.2) | 92.1 (8.3) | 98.0 (7.2) |
| All “non-cluster” dates | 1145 | 278 | 24.3 | 85.8 (11.3) | 83.6 (11.6) | 81.7 (11.7) | 83.7 (11.0) |
Abbreviations: DOI, day of illness; HRI, heat-related illness; SD, standard deviation; Tmax,PRISM, daily maximum temperature.
The mean (±standard error) Tmax,PRISM on the DOI and 5 days prior, stratified by whether or not claims occurred on “cluster” days, whether or not claims occurred during the 2021 heat dome, and whether or not claims occurred on the first day (e.g., 7/11/2007, 7/ 28/2009, 6/27/2921) of a “cluster” are shown in Figure 5. For claims occurring on “cluster” days, the mean Tmax,PRISM appeared to increase more rapidly in the 2–3 days before the HRI but was more similar to “non-cluster” days on the fourth and fifth days before illness (Figure 5A). Compared to “cluster” days, claims occurring on heat dome days had a similar trajectory of mean Tmax,PRISM on the days before the DOI, but with higher mean Tmax,PRISM, including on the fourth and fifth days before illness (Figure 5B). Compared to non-first-day “cluster” claims, the mean Tmax,PRISM for first-day “cluster” claims appeared to increase most rapidly in the day before the HRI (Figure 5C). Similar patterns were seen in a sensitivity analysis that included only claims deemed to be “definitely” or “probably” outdoor.
FIGURE 5.
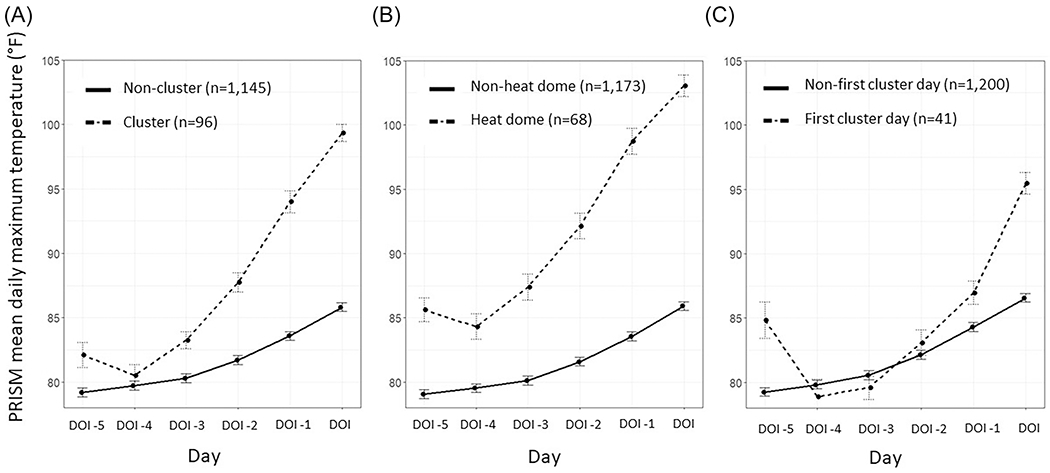
Mean (±standard error) maximum daily PRISM temperatures on 2006–2021 HRI claims DOI and 5 days prior, stratified by: (A) whether or not claims occurred on cluster days; (B) whether or not claims occurred during the 2021 heat dome; (C) whether or not claims occurred on the first day (e.g., 7/11/2007, 7/28/2009, 6/27/2921) of a cluster. Error bars are ±standard errors. Workers were not directly observed on each day leading up to the DOI. DOI, day of illness (DOI - X denotes the DOI minus X days); HRI, heat-related illness; PRISM, parameter-elevation regressions on independent slopes model.
3.6 |. Geographical distributions
Maps of the proportion of HRI claims by county for claims occurring on “cluster” days and days at or above a Tmax,PRISM of 80°F are shown in Figure 6. While higher proportions of HRI claims occurring on “cluster” days were prominent in Western WA, higher proportions of HRI claims occurring on days at or above 80°F (27°C) were prominent in Central WA. These geographical patterns in proportions were generally similar when examining accepted HRI claims and claims deemed “definitely” or “probably” outdoor. The proportion of HRI claims occurring on “sudden increase” days is shown in Supporting Information: Figure 5a and was not more prominent in Central WA. For the absolute number of HRI claims, which also reflects employment patterns, the highest number of HRI claims occurred in agriculture in Yakima County in Central WA and in construction in King County in Western WA (Supporting Information: Figure 6). The number of HRI claims occurring on “cluster” days by county is shown in Supporting Information: Figure 5b and was highest in King, Pierce, Whatcom, Clark, and Grant Counties.
FIGURE 6.
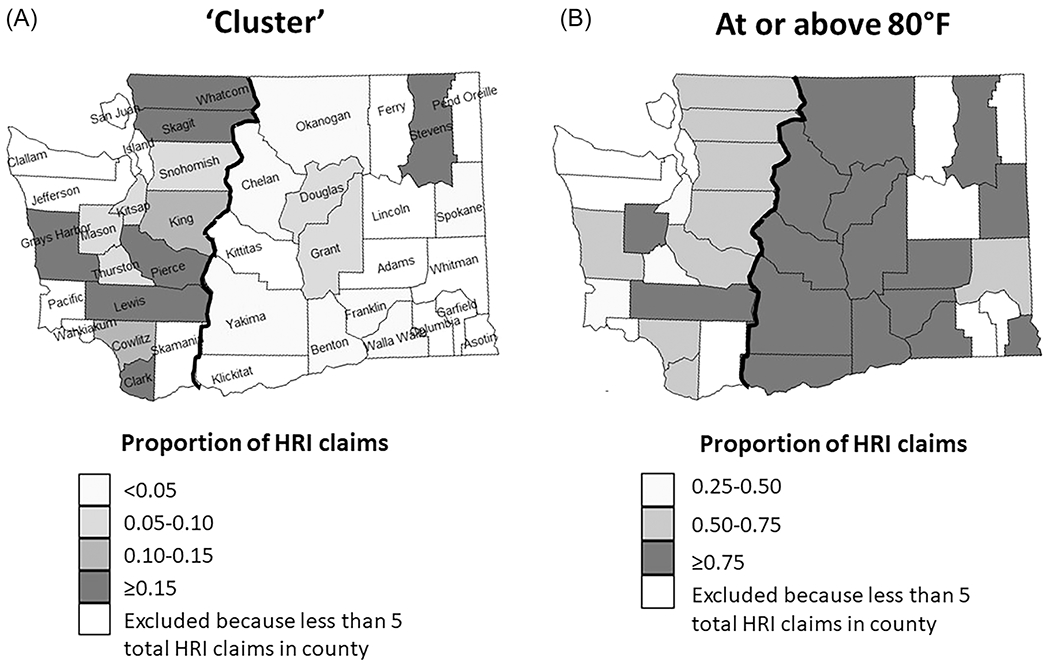
Maps of the proportion of 2006–2021 HRI claims by county in Washington State for claims occurring on: (A) “cluster” days; (B) days at or above 80°F (27°C). Black line: Central/Eastern Washington and Western Washington regions are defined using county borders nearest the Cascade Ridge line.32 HRI, heat-related illness.
4 |. DISCUSSION
In this study of WA HRI workers’ compensation claims and ambient temperature exposures from 2006 to 2021, we found that days with multiple HRI claims (“cluster” days) were characterized by a combination of high mean maximum temperatures on the DOI and apparent steeper increases on days leading up to HRIs, compared to other days that HRI claims occurred. A similar trajectory in mean maximum temperatures was seen on the days leading up to the DOI for 2021 heat dome claims, but the absolute mean maximum temperatures on these days were higher than for “cluster” claims. We found a small but extant proportion of HRI claims that occurred on days with increases in temperature of at least 10.0°F (~5.6°C), compared to the average of the prior 5 days (“sudden increase”), but that did not reach a maximum daily temperature at or above 80°F (27°C) on the DOI. We also identified variation in the proportion of HRI claims occurring on “sudden increase” days by industry and occupation, with higher proportions in high-risk industries of construction and agriculture compared to lower proportions among firefighters, whose work environments may include point sources of heat, in addition to ambient environmental heat exposure. We found that HRI claims occurring on “cluster” days did not simply follow the geographical distribution of counties with higher proportions of threshold temperature exceedances (Central WA). Overall, our findings provide useful information to guide the identification of high-risk workers as well as the prioritization and tailoring of HRI prevention efforts.
Heat exposure on “cluster” days, or days in which 10 or more HRI claims occurred, was characterized by significantly higher proportions of “sudden increase” claims, higher mean ambient temperatures on the DOI, 1- and 2-day lag temperatures, and cumulative 3-day (including DOI) temperatures. These findings are consistent with the observed potential steeper increase in temperatures for “cluster” claims compared to noncluster claims, particularly for larger “cluster” sizes, and in the day before the first “cluster” day. However, even for small “cluster” sizes of two claims per day in which mean temperatures were lower than for smaller “cluster” sizes, mean temperatures were still significantly higher than for noncluster days. These findings should be further evaluated in future studies to disentangle the effects of DOI, lagged, and cumulative exposure, and the rate of temperature increase and other factors on the development, severity, and clustering of occupational HRIs. Understanding the characteristics of days when clusters occur offers an opportunity to anticipate these characteristics and optimize prevention to reduce the burden of HRI.
Exposure risk was not fully captured by the DOI temperature alone. Our findings are consistent with earlier analyses of WA HRI claims data from 1995 to 2005,6 which reported that 42% of HRI claims occurred on days with an increase in the daily maximum temperature of 10.0°F (~5.6°C) and that this variation in temperature more commonly occurred on days with more than one claim. Our overall proportion of “sudden increase” claims (28.6%) is lower than in the 1995–2005 analysis likely because our “sudden increase” definition compared the DOI maximum temperature to the average maximum temperature over the prior 5 days, which smooths out very brief (e.g., 1 day) temperature extremes. Our findings are also consistent with studies of heat-related occupational traumatic injuries, which suggest that in addition to the ambient conditions on the day of injury, there may be a lagged effect of 1–2 days and a cumulative effect over several days of warm temperatures on the risk of occupational traumatic injury.33–38
While most HRI claims on “sudden increase” days occurred on days with a maximum daily temperature at or above 80°F (27°C), 7% occurred on days less than 80°F (27°C), with 46% of these latter claims occurring in April. This observation may result from an elevated risk of HRI among less acclimatized workers performing physical work early in the season, even below 80°F (27°C). “Cluster” days tended to occur in years in which HRI claims had both high mean maximum temperatures and high proportions of “sudden increase” days (e.g., 2009, 2021).
A large number of HRI claims occurred in WA during the 2021 Pacific Northwest heat dome, with a peak on June 28, 2021 (31 claims). This is consistent with reports in the general population. An analysis of HRI emergency department (ED) visits in the Northwest (Alaska, Idaho, Oregon, and Washington) reported that the mean daily number of HRI ED visits during June 25–30, 2021 (n = 424) was 69 times higher than that during the same days in 2019 (n = 6), with a peak detected on June 28 (n = 1090).31 We found that heat dome HRI claims had higher DOI, lagged, and cumulative mean maximum daily temperatures than “cluster” claims. June 27–29, 2021 also fell into the classification of HRI “cluster” days, which could be consistent with a several-day lag in the development of 10 or more claims occurring on a given day. Heat dome claims had a similar trajectory of increase in mean maximum temperatures on the days leading up to the DOI, but higher absolute mean maximum temperatures on each day leading up to the DOI, including on the fourth and fifth days before the DOI. Heat dome and “cluster” claim groups’ proportions of “sudden increase” claims (72.1% and 80.2%, respectively) were higher than for all HRI claims (28.6%). These results suggest that the combination of “sudden increase” and very high temperatures warrants particular and rapid anticipation and response to reduce the HRI burden.
During the heat dome event of 2021, the largest peak in WA HRI claims was in June, whereas WA HRI claims analyses in prior years indicate the largest number of HRI claims in July.3 “Sudden increase” claims were observed to occur as early as April. An attribution analysis of the heat dome event indicated that the heat dome would have been highly unlikely without climate change and could occur about every 5–10 years in a future world with 2°C of global warming.39 Given trends in climate change, designating heat exposure criteria as triggers for occupational HRI prevention policies, rather than times of year historically considered hottest, may increase the protection of workers covered by these policies over time. HRI training and heat prevention planning should occur in advance of these anticipated triggers. Heat exposure criteria should incorporate an element of change in temperature relative to prior days, in addition to how hot the current conditions are or will be, to better account for risks associated with insufficient acclimatization.
We found variation in the proportion of HRI claims occurring on “sudden increase” days by industry and occupation. For example, public administration had a lower percentage (15.6%) of “sudden increase” HRI claims than for all industries (28.6%). Firefighters, who are within the public administration sector, also had a low proportion (12.0%) of “sudden increase” claims. Firefighters work in environments where point sources of heat and nonbreathable personal protective equipment may contribute to net heat stress, in addition to the ambient environment. For firefighters and workers with similar heat exposure profiles, changes in ambient temperatures may be less important for the assessment of heat risk than for workers in other high-risk industries (e.g., construction and agriculture). While state-level initial prioritization of HRI prevention activities could be targeted to days forecasted to exceed temperature thresholds and those forecasted to have substantial increases in temperature over several days, certain occupations that have a high number of HRI claims3 and a unique exposure profile, such as firefighters, should also be specially accounted for in heat prevention prioritization. Additional tailoring of prevention strategies must also be made for indoor workers who work in environments with point sources of heat and humidity for which ambient temperatures may not be as representative.
Among “cluster” and heat dome claims, industries with top numbers of claims included administrative and support and waste management and remediation, agriculture, and construction. Construction and agriculture were reported in previous WA workers’ compensation HRI claims analyses to have the highest rates of HRI3 in WA. Construction and agriculture, particularly farmworkers and laborers, should continue to be among the industries and occupations prioritized, along with administrative and support and waste management and remediation, for HRI prevention when sudden increases in temperatures are forecasted.
Our analysis provided information about the geographical distribution of HRI claims and their exposure characteristics by WA county. We found higher proportions of HRI claims occurring on “cluster” days in Western WA and higher proportions of HRI claims occurring on days at or above 80°F (27°C) in Central WA. We found similar geographic patterns for the frequency of HRI claims across WA as previous research that identified the average number of days and employment days at or above PRISM maximum daily temperature thresholds of 80°F (27°C) in WA.19 The concordance of these findings underlines the importance of both the geographical distribution of the workforce and ambient temperature exposures on the risk of occupational HRI. The geographical pattern of the absolute number of HRI claims occurring on “cluster” days, however, did not simply follow the geographical distribution of counties with high employment or those more commonly exceeding temperature thresholds. Rather, WA counties with a high number of “cluster” claims (King, Pierce, Whatcom, Clark, and Grant) likely represent a combination of factors, including employment; industry, occupation, and task characteristics; and both ambient temperature and temperature change characteristics. These characteristics should be considered in the prioritization of heat prevention activities.
Heat prevention programs should include provisions to optimize workers’ acclimatization status. Acclimatization allows for protection from about an additional ~2.5–3°C WBGT of heat exposure.25 Military and laboratory studies suggest that physiological heat acclimatization is associated with reduced inflammation and heat stroke incidence,40 improved cognition,41 and increased heat shock protein levels,42 which can protect against systemic inflammatory response syndrome associated with heat stroke.1 NIOSH recommendations include 4- or 5-day acclimatization schedules, depending on the level of experience.43 These schedules involve gradually increasing exposure time in hot environments by 20% on each successive day. Acclimatization protocols should be considered for new workers and those returning from an absence, as acclimatization can be lost after only about 1 week away from working in the heat.43 Additional research is also needed to address gaps in how to practically assess acclimatization status in real-world settings, given individual variability,44,45 the time course and physical requirements needed to achieve physiological adaptations in different environments and populations outside of controlled laboratory environments, and factors that influence heat acclimatization decay and reacclimatization.4,46 When sudden increases in temperature occur beyond the level that a worker may be acclimatized to, additional “high heat” protections are needed to prevent HRI. In addition to hydration, shade, and training, workers should be observed by supervisors or work closely with coworkers (“buddy system”), who can detect and respond to early HRI signs. In addition, appropriate duration of paid rest breaks and reduced work pace given the intensity of heat exposure should be provided, and procedures for contacting emergency medical services with precise directions to the worksite should be in place.
Given the overlap in ambient exposure and risk in the community and workplace, as observed during the Pacific Northwest 2021 heat dome event, as well as the potential for heat exposure outside of work to increase the risk of occupational HRI,47 public health and occupational health agencies should coordinate on heat prevention messaging during heat events. Additionally, these prevention messages should be tailored to specific high-risk communities and worker populations. An initial step in an approach that is likely to be effective and adopted requires strategic partnerships between public health and occupational health agencies and communities, for example, as part of extreme heat mitigation planning, at the local and regional levels.
4.1 |. Strengths and limitations
This is the first study that we are aware of that has systematically described trajectories of heat exposure leading up to days on which occupational HRIs occur and among HRI case clusters using modeled meteorological data. However, this study has several important limitations. First, occupational HRIs are likely to be underestimated, and less severe HRIs may not be reported or identified.3 It is possible that HRIs occurring on “sudden increase” days were more likely to be recognized and reported, thereby leading to higher proportions of “sudden increase” claims. However, we do not have reason to believe there would be differential increased identification or reporting by claim characteristics or geographical area. Second, for prior-day exposure estimates, workers were assumed to be at the same location as on the DOI. It is possible that exposure misclassification occurred for workers moving from job site to job site or who were not working on the days before illness, though this is difficult to systematically ascertain with the data available. Exposure misclassification may also have occurred when assigning exposures to claims where HRI may have occurred indoors, though claims unlikely to occur outdoors accounted for less than one-fifth of all HRI claims. Third, for nearly a quarter of claims, there was not enough information upon manual claim review to determine whether the claim occurred indoors or outdoors. It is possible that worker patterns of exposure to outdoor ambient temperatures (and potential interaction with indoor temperatures and access to cooling) may differ among those claims classified as “definitely” or “probably” occurring outdoors versus those that were “unlikely” outdoors or uncertain. However, results of sensitivity analyses restricting to “definitely” or “probably” outdoor claims were not substantially different, suggesting that this effect was minimal, perhaps in part as a result of the effect of the outdoor ambient environment on indoor environments that are open to the outdoors or that lack climate control. Additional work is needed to better characterize the work environment among workers experiencing HRI, for example, by surveying workers who have experienced an HRI, and, ideally, through better administrative capture of relevant information to inform tailored prevention approaches. Fourth, we were not able to systematically characterize other important elements of heat stress. These elements include clothing and workload and important risk factors for HRI. Individual risk factors include underlying chronic diseases that affect the ability to respond to heat stress (e.g., cardiovascular disease and diabetes mellitus); pregnancy; medications that dehydrate, inhibit heat loss, or increase heat gain; and acclimatization status. Modifiable workplace factors include suboptimal access to beverages and restrooms, payment type (e.g., piece-rate payment may incentivize faster-paced work and minimize breaks), and absence of shade. Further research in actual workplace settings is needed to characterize these factors and how they relate to “sudden increase” exposures, acclimatization status, and occupational health outcomes. In addition, future research should aim to evaluate the effectiveness of existing policies. Finally, we used an exposure assessment approach based on modeled meteorological data. Different heat exposure assessment approaches have different strengths and limitations.19 Although gridded meteorological data are efficient and provide reasonable spatial resolution, they may not reflect smaller-scale microclimates. Conversely, weather stations may provide more accurate estimates at their locations, but gaps in weather station spatial coverage may lead to misclassification of exposure in areas with sparse weather station coverage. However, we expect variability due to potential exposure misclassification to be smaller than variability in heat exposure by claim characteristics and geography.
4.2 |. Conclusions
Identification of high-risk heat exposure conditions for occupational HRI should consider changes in temperature relative to prior days, in addition to how hot the current conditions are or will be, with additional considerations for occupations involving point sources of heat and for indoor workers who may be exposed to conditions that differ from outdoor ambient conditions. Heat prevention programs should include provisions to optimize workers’ acclimatization status and, when increases in temperature occur too quickly to allow for sufficient acclimatization, additional “high heat” protections. Public health and occupational health agencies should coordinate heat prevention efforts during heat events. Further research in real workplace settings is needed to characterize how heat stress and “sudden increase” exposures, HRI risk factors, acclimatization status, and occupational health outcomes relate, and to disentangle the effects of DOI, lagged, and cumulative exposure and the rate of temperature increase on the development, severity, and clustering of occupational HRIs, to better inform prevention efforts. This work is urgently needed given projected increases in future mean ambient temperatures and in the frequency and duration of extreme events.20
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to thank Amanda Robinson for her assistance with the manual claims review, Jihoon Jung and Danièle Todorov for their assistance with geographic information systems and PRISM data linkage methods, and Nayak Polissar and Nirnaya Mil for their consultation on statistical methods. This study was supported in part by an appointment to the Applied Epidemiology Fellowship Program administered by the Council of State and Territorial Epidemiologists (CSTE) and funded by the Centers for Disease Control and Prevention (CDC) Cooperative Agreement Number 1NU38OT000297-03-00. This study was also supported in part by the University of Washington National Institute of Environmental Health Sciences (NIEHS) sponsored Biostatistics, Epidemiologic and Bioinformatic Training in Environmental Health (BEBTEH) Training Grant, Grant # NIEHS T32ES015459.
Footnotes
CONFLICTS OF INTEREST STATEMENT
The authors declare that there are no conflicts of interest.
DISCLOSURE BY AJIM EDITOR OF RECORD
John D. Meyer declares that he has no conflict of interest in the review and publication decision regarding this article.
ETHICS APPROVAL AND INFORMED CONSENT
The Washington State Department of Labor and Industries (L&I) is a public health authority, and as such is allowed by 45 CFR 46.102(/)(2) to conduct public health surveillance to identify, monitor, assess, or investigate conditions of public health importance. The work presented here, which falls within public health surveillance activities as covered by the Common Rule, was performed in conjunction with L&I’s Division of Occupational Safety and Health rulemaking to update the requirements for controlling occupational heat exposure hazards; approval by an institutional review board is not required.
DISCLAIMER
This content is solely the responsibility of the authors and does not necessarily represent the official views of the Centers for Disease Control and Prevention, the National Institutes of Health, or the Washington State Department of Labor and Industries.
SUPPORTING INFORMATION
Additional supporting information can be found online in the Supporting Information section at the end of this article.
REFERENCES
- 1.Sawka MN, Leon LR, Montain SJ, Sonna LA. Integrated physiological mechanisms of exercise performance, adaptation, and maladaptation to heat stress. Compr Physiol. 2011;1(4):1883–1928. doi: 10.1002/cphy.c100082 [DOI] [PubMed] [Google Scholar]
- 2.Gubernot DM, Anderson GB, Hunting KL. Characterizing occupational heat-related mortality in the United States, 2000-2010: an analysis using the census of fatal occupational injuries database. Am J Ind Med. 2015;58(2):203–211. doi: 10.1002/ajim.22381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hesketh M, Wuellner S, Robinson A, Adams D, Smith C, Bonauto D. Heat related illness among workers in Washington State: a descriptive study using workers’ compensation claims, 2006-2017. Am J Ind Med. 2020;63(4):300–311. doi: 10.1002/AJIM.23092 [DOI] [PubMed] [Google Scholar]
- 4.Pèriard JD, Racinais S, Sawka MN. Adaptations and mechanisms of human heat acclimation: applications for competitive athletes and sports. Scand J Med Sci Sports. 2015;25(s1):20–38. doi: 10.1111/sms.12408 [DOI] [PubMed] [Google Scholar]
- 5.Tustin AW, Lamson GE, Jacklitsch BL, et al. Evaluation of occupational exposure limits for heat stress in outdoor workers—United States, 2011-2016. MMWR Morb Mortal Wkly Rep. 2018;67(26):733–737. doi: 10.15585/mmwr.mm6726a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bonauto D, Anderson R, Rauser E, Burke B. Occupational heat illness in Washington State, 1995-2005. Am J Ind Med. 2007;50(12): 940–950. doi: 10.1002/ajim.20517 [DOI] [PubMed] [Google Scholar]
- 7.National Weather Service. Heat watch vs. warning. Accessed April 9, 2023. https://www.weather.gov/safety/heat-ww
- 8.Hondula DM, Meltzer S, Balling RC, Iñiguez P. Spatial analysis of United States National Weather Service excessive heat warnings and heat advisories. Bull Am Meteorol Soc. 2022;103(9): E2017–E2031. doi: 10.1175/BAMS-D-21-0069.1 [DOI] [Google Scholar]
- 9.National Weather Service. Week-2 global probabilistic extremes forecast tool description. 2009. Accessed April 9, 2023. https://www.cpc.ncep.noaa.gov/products/predictions/threats/extremesToolAbout.php
- 10.US Occupational Safety and Health Administration (OSHA). Heat injury and illness prevention in outdoor and indoor work settings rulemaking. Accessed April 9, 2023. https://www.osha.gov/heat-exposure/rulemaking
- 11.Washington State Legislature. Chapter 296-307 WAC: safety standards for agriculture. 2009. Accessed April 9, 2023. https://apps.leg.wa.gov/WAC/default.aspx?cite=296-307%26full=true#.296-307-097
- 12.Washington State Legislature. Chapter 296-62 WAC: general occupational health standards. 2008. Accessed April 9, 2023. http://app.leg.wa.gov/WAC/default.aspx?cite=296-62%26full=true#296-62-095
- 13.Oregon OSHA. Rules to address employee and labor housing occupant exposure to high ambient temperatures. 2022. Accessed April 9, 2023. https://osha.oregon.gov/OSHARules/adopted/2022/ao3-2022-text-alh-heat.pdf
- 14.Nevada Department of Business and Industry, Division of Industrial Relations, Occupational Safety & Health Administration. Agency draft of proposed regulation R053-20. 2022. Accessed April 9, 2023. https://dir.nv.gov/uploadedFiles/dir.nv.gov/content/OSHA/Features/R053-20%20Proposed%20Heat%20Illness%20Regulation%20-%202.28.22(3).pdf
- 15.Washington State Department of Labor and Industries. Ambient heat exposure rulemaking. Accessed April 9, 2023. https://lni.wa.gov/ safety-health/safety-rules/rulemaking-stakeholder-information/ambient-heat-exposure-rulemaking
- 16.Hogan LJ. House Bill 722, Labor and employment–occupational safety and health-heat stress standards. Title 5, subtitle 12 of the labor and employment article, annotated code of Maryland, chapter 308. 2020. Accessed April 9, 2023. https://mgaleg.maryland.gov/2020RS/Chapters_noln/CH_308_hb0722t.pdf
- 17.California Division of Occupational Safety and Health. California code of regulations. Title 8, section 3395, heat illness prevention. 2020. Accessed April 9, 2023. http://www.dir.ca.gov/Title8/3395.html
- 18.United States Centers for Disease Control and Prevention. Guidelines for investigating clusters of health events. 1998. Accessed April 9, 2023. https://www.cdc.gov/mmwr/preview/mmwrhtml/00001797.htm
- 19.Flunker JC, Zuidema C, Jung J, et al. Potential impacts of different occupational outdoor heat exposure thresholds among Washington State crop and construction workers and implications for other jurisdictions. Int J Environ Res Public Health. 2022;19(18):11583. doi: 10.3390/IJERPH191811583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.IPCC. Pörtner H-O, Roberts DC, Tignor M, eds. Climate Change 2022: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge University Press; 2022:3056. doi: 10.1017/9781009325844 [DOI] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Occupational injury and illness classification system. 2021. Accessed April 9, 2023. https://wwwn.cdc.gov/wisards/oiics/Trees/MultiTree.aspx?Year=2007
- 22.US Census Bureau. North American Industry Classification System. 2023. Accessed April 9, 2023. https://www.census.gov/naics/
- 23.US Department of Labor. Standard occupational classification. Accessed April 9, 2023. https://www.bls.gov/soc/
- 24.Jacklitsch B, Williams W, Musolin K, Coca A, Kim JH, Turner N. NIOSH criteria for a recommended standard: occupational exposure to heat and hot environments. 2016. Accessed April 9, 2023. https://www.cdc.gov/niosh/docs/2016-106/pdfs/2016-106.pdf
- 25.American Conference of Governmental Industrial Hygienists (AC-GIH®). Heat Stress and Strain: TLV® Physical Agents. ACGIH®; 2023. [Google Scholar]
- 26.Washington State Department of Labor and Industries. Outdoor heat exposure concise explanatory statement (report required by the Revised Code of Washington [RCW] 34.050.325[6][a]). 2008. [Google Scholar]
- 27.Daly C, Halbleib M, Smith JI, et al. Physiographically sensitive mapping of climatological temperature and precipitation across the conterminous United States. Int J Climatol. 2008;28(15):2031–2064. doi: 10.1002/JOC.1688 [DOI] [Google Scholar]
- 28.Behnke R, Vavrus S, Allstadt A, Albright T, Thogmartin WE, Radeloff VC. Evaluation of downscaled, gridded climate data for the conterminous United States. Ecol Appl. 2016;26(5):1338–1351. doi: 10.1002/15-1061 [DOI] [PubMed] [Google Scholar]
- 29.PRISM Climate Group; Oregon State University. PRISM climate data. 2023. Accessed April 9, 2023. https://www.prism.oregonstate.edu/
- 30.Spector JT, Bonauto DK, Sheppard L, et al. A case-crossover study of heat exposure and injury risk in outdoor agricultural workers. PLoS One. 2016;11(10):e0164498. doi: 10.1371/journal.pone.0164498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schramm PJ, Vaidyanathan A, Radhakrishnan L, Gates A, Hartnett K, Breysse P. Heat-related emergency department visits during the Northwestern heat wave—United States, June 2021. MMWR Morb Mortal Wkly Rep. 2021;70(29):1020–1021. doi: 10.15585/MMWR.MM7029E1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.WSDOT. Boundary between eastern and western Washington for the wetland rating system. 2013. Accessed April 9, 2023. https://wsdot.wa.gov/sites/default/files/2021-10/Env-Wet-EastWestBoundary.pdf
- 33.Fatima SH, Rothmore P, Giles LC, Varghese BM, Bi P. Extreme heat and occupational injuries in different climate zones: a systematic review and meta-analysis of epidemiological evidence. Environ Int. 2021;148:106384. doi: 10.1016/J.ENVINT.2021.106384 [DOI] [PubMed] [Google Scholar]
- 34.McInnes JA, Akram M, MacFarlane EM, Keegel T, Sim MR, Smith P. Association between high ambient temperature and acute work-related injury: a case-crossover analysis using workers’ compensation claims data. Scand J Work Environ Health. 2017;43(1):86–94. doi: 10.5271/sjweh.3602 [DOI] [PubMed] [Google Scholar]
- 35.Garzon-villalba XP, Mbah A, Wu Y, et al. Exertional heat illness and acute injury related to ambient wet bulb globe temperature. Am J Ind Med. 2016;59:1169–1176. doi: 10.1002/ajim.22650 [DOI] [PubMed] [Google Scholar]
- 36.Riccò M Air temperature exposure and agricultural occupational injuries in the autonomous province of Trento (2000-2013, NorthEastern Italy). Int J Occup Med Environ Health. 2017;31(3):317–331. doi: 10.13075/ijomeh.1896.01114 [DOI] [PubMed] [Google Scholar]
- 37.Martínez-Solanas È, Lòpez-Ruiz M, Wellenius GA, et al. Evaluation of the impact of ambient temperatures on occupational injuries in Spain. Environ Health Perspect. 2018;126(6):067002. doi: 10.1289/EHP2590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marinaccio A, Scortichini M, Gariazzo C, et al. Nationwide epidemiological study for estimating the effect of extreme outdoor temperature on occupational injuries in Italy. Environ Int. 2019;133:105176. doi: 10.1016/J.ENVINT.2019.105176 [DOI] [PubMed] [Google Scholar]
- 39.Philip SY, Kew SF, van Oldenborgh GJ, et al. Rapid attribution analysis of the extraordinary heatwave on the Pacific Coast of the US and Canada June 2021. 2021. Accessed April 9, 2023. https://www.worldweatherattribution.org/western-north-american-extreme-heat-virtually-impossible-without-human-caused-climate-change/
- 40.Li Q, Sun R, Liu S, et al. Effect of heat acclimatization training on inflammatory reaction and multiple organ dysfunction syndrome in patients with exertional heat stroke. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2018;30(6):599–602. doi: 10.3760/CMA.J.ISSN.2095-4352.2018.06.019 [DOI] [PubMed] [Google Scholar]
- 41.Radakovic SS, Maric J, Surbatovic M, et al. Effects of acclimation on cognitive performance in soldiers during exertional heat stress. Mil Med. 2007;172(2):133–136. doi: 10.7205/MILMED.172.2.133 [DOI] [PubMed] [Google Scholar]
- 42.McClung JP, Hasday JD, He J, et al. Exercise-heat acclimation in humans alters baseline levels and ex vivo heat inducibility of HSP72 and HSP90 in peripheral blood mononuclear cells. AmJ Physiol Regul Integr Comp Physiol. 2008;294(1):R185–R191. doi: 10.1152/AJPREGU.00532.2007 [DOI] [PubMed] [Google Scholar]
- 43.National Institute for Occupational Safety and Health. Acclimatization. 2018. Accessed April 9, 2023. https://www.cdc.gov/niosh/topics/heatstress/acclima.html
- 44.Corbett J, Rendell RA, Massey HC, Costello JT, Tipton MJ. Interindividual variation in the adaptive response to heat acclimation. J Therm Biol. 2018;74:29–36. doi: 10.1016/J.JTHERBIO.2018.03.002 [DOI] [PubMed] [Google Scholar]
- 45.Alkemade P, Gerrett N, Eijsvogels TMH, Daanen HAM. Individual characteristics associated with the magnitude of heat acclimation adaptations. Eur J Appl Physiol. 2021;121(6):1593–1606. doi: 10.1007/S00421-021-04626-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Daanen HAM, Racinais S, Périard JD. Heat acclimation decay and reinduction: a systematic review and meta-analysis. Sports Med. 2018;48(2):409–430. doi: 10.1007/S40279-017-0808-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Quandt SA, Wiggins MF, Chen H, Bischoff WE, Arcury TA. Heat index in migrant farmworker housing: implications for rest and recovery from work-related heat stress. Am J Public Health. 2013;103(8):e24–e26. doi: 10.2105/AJPH.2012.301135 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


