Abstract
Liagmentum flavum hematoma (LFH) is a rare cause of radiculopathy and low back pain, sharing similar symptomatology with disc herniation. It predominantly affects the lumbar thoracic spine. The underlying mechanism of LFH remains unclear; however, surgical removal of the hematoma has consistently demonstrated excellent outcomes.
The objective of this case report is to emphasize the significance of diagnosing LFH. We present a surgically confirmed lumbar LFH case that mimicked a lumbar tumor, highlighting the challenges encountered during diagnosis and subsequent management.
Keywords: Ligamentum Flavum Hematoma, Lumbar, Case report, Differential diagnosis
Introduction
The ligamentum flavum can undergo various pathological changes, such as hypertrophy, calcification, ossification, and cyst formation, which may lead to compression of the spinal cord [1,2]. One rare but significant cause of spinal nerve compression is ligamentum flavum hematoma (LFH). Although approximately 30 cases of lumbar LFH have been previously documented in the literature, the exact underlying pathogenesis of this condition remains unclear [3,4]. Moreover, diagnosing LFH using magnetic resonance imaging (MRI) poses challenges due to the dynamic nature of hematoma intensity on imaging [4].
In this study, we present a case of lumbar LFH in a 74 years old man who presented with back pain and sciatica. We discuss the clinical features, radiological findings, surgical management, and histopathological examination results of the patient. Additionally, we review the existing literature on lumbar LFH to enhance our understanding of this rare condition and highlight the diagnostic and therapeutic considerations associated with it. The aim of this case report is to contribute valuable insights into the diagnosis and management of lumbar LFH, further expanding our knowledge on this intriguing clinical entity.
Case report
We present the case of a 74-year-old man who was admitted to our hospital with complaints of low backache and right-sided sciatica. The patient had been in good health until approximately 1 month prior to admission when he experienced back strain while lifting, resulting in backache and right sciatic pain. He initially recovered within 4 days and resumed his daily activities. However, 1 week before admission, he experienced a severe recurrence of backache. Three days later, the pain began radiating to his buttock, the back of his right thigh, and down to his ankle and big toe. The pain was nearly constant and exacerbated by strenuous activities. The patient reported no paresthesia, similar pain on the opposite side, or bladder dysfunction. His past medical history was unremarkable, with no history of back trauma, smoking, drinking, or drug use. He was not on anticoagulation or antiplatelet medications at the time of presentation.
Neurological examination revealed a steppage gait on the right side, while the range of motion of the spine was normal. Straight leg raising test was not limited. Sensory depression corresponding to the L4 and L5 dermatomes was observed, along with weakness in dorsiflexion of the right foot. Routine laboratory tests yielded normal results.
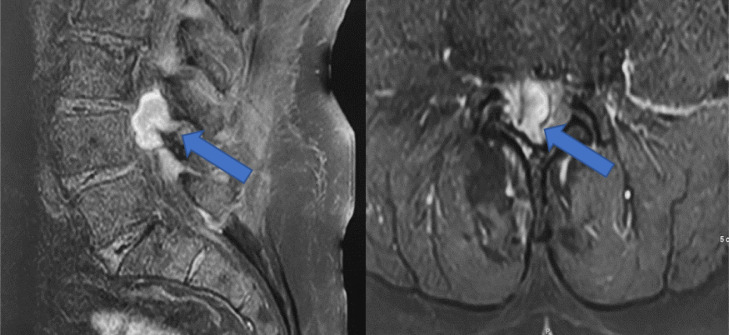
An urgent magnetic resonance imaging (MRI) of the lumbar spine was performed, revealing a well-defined dorsal extradural lesion at the L3-L4 levels. The MRI demonstrated a relatively large mass posterior to the L4 vertebral body, with L3-L4 disc protrusion and a connection between the mass and the L3-L4 level. T1-weighted images showed heterogeneous intermediate to high signal intensity equivalent to the disc, while T2-weighted images exhibited high signal intensity greater than that of the disc. Gadolinium-DTPA-enhanced MRI demonstrated rim enhancement of the lesion (Fig. 1, Fig. 2, Fig. 3).
Fig. 1.
Sagittal T1-weighted.
Fig. 2.
Sagittal T2-weighted.
Fig. 3.
Extra medullary intradural lesion (Blue Arrow) opposite the L3L4 interbody disc, paramedian and right foraminal, compressing the cauda equina roots, iso to intermediate signal T1, iso to high signal T2, taking contrast after injection and measuring approximately 27 × 22 mm.
Based on the clinical and radiological features, the differential diagnosis included disc herniation, tumor, or hematoma as potential causes of the space-occupying lesion. Due to the severity of the patient's pain, surgery was planned.
A partial laminectomy of L3 and L4 on the right side, along with resection of the mass, was performed. During the surgery, an encapsulated brownish soft tissue mass measuring approximately 25 mm in diameter was identified. The dorsal surface of the right ligamentum flavum was dark brown and hematoma was observed within the multiple layers of the HLF. The mass was easily separated from the dura mater, although it adhered to the posterior longitudinal ligament. The content of the mass was determined to be blood, and no significant disc herniation was observed. The L4 and L5 nerve roots on the right side were slightly stretched due to the presence of the mass.
The pathological examination revealed the presence of extravasated fibrin, blood, and hemosiderin deposits surrounded by necrotic ligament tissue, indicating a pattern consistent with LFH. No evidence of malignancy was observed in the examination, further supporting the diagnosis of LFH.
Following the procedure, the patient achieved complete recovery and was discharged from the hospital within 2 days. During the 1-month follow-up, the patient presented unassisted and remained free from pain, exhibiting no symptoms. At the most recent visit, occurring 2 years after the surgical treatment, the patient remained asymptomatic and continued to experience a pain-free state.
Discussion
Our patient experienced a rapid recovery following surgical removal of the LFH, which is consistent with previous reports in the literature. To date, a total of 30 cases of lumbar LFH have been documented (Table 1) [1,2,[4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25],28], and surgical intervention was performed in all these cases. Notably, the preoperative diagnosis of LFH remains challenging in the majority of these cases. MRI imaging is considered the preferred method for preoperative diagnosis of LFH, as it can reveal the heterogeneous intensity of the mass lesion that is contiguous with the ligamentum flavum.
Table 1.
Reported cases of lumbar ligamentum flavum hematoma.
| Authors | Patient's gender | Age | Level |
|---|---|---|---|
| Sweasey et al. [5] | M | 43 | L4/5 |
| M | 60 | L2/3 | |
| Baker and Hanson [6] | F | 58 | L5/S1 |
| Cruz-Conde et al. [7] | M | 57 | L4/L5 |
| Mahallati et al. [8] | M | 30 | L3/L4 |
| Minamide et al. [9] | M | 76 | L3/L4 |
| Hirakawa et al. [10] | M | 50 | L4/L5 |
| Yuceer et al. [11] | M | 67 | L2/L3 |
| Chi et al. [12] | M | 64 | L3/L4 |
| Mizuno et al. [13] | F | 45 | L4/L5 |
| Yamaguchi et al. [14] | M | 62 | L4/L5 |
| Albanese et al. [15] | F | 70 | L1/L2 |
| Keynan et al. [16] | F | 75 | L3/L4 |
| Shimada et al. [17] | F | 83 | L2/L4 |
| Spuck et al. [18] | F | 64 | L2/L3 |
| M | 62 | L4/L5 | |
| Gazzeri et al. [19] | F | 59 | L3/L4 |
| Kotil and Bilge [20] | M | 74 | L4/L5 |
| M | 80 | L4/L5 | |
| Kono et al. [21] | M | 64 | L4/L5 |
| Miyakoshi et al. [22] | M | 71 | L3-L5 |
| Takahashi et al. [23] | F | 53 | L3/L4 |
| M | 61 | L5/S1 | |
| Ohba et al. [1] | M | 52 | L5/S1 |
| Ghent et al. [24] | M | 62 | L3/L4 |
| Liu et al. [2] | M | 76 | L4/L5 |
| Ozdemir et al. [4] | M | 63 | L2/L3 |
| Ishimoto et al. [25] | F | 71 | L4/L5 |
| Hisamitsu et al. [28] | F | 69 | L4/L5 |
| Sahri et al. [31] | M | 74 | L3/L4 |
The rarity of LFH and its similarity in clinical presentation to other conditions, such as disc herniation, tumors, and abscesses, contribute to the difficulty in making a preoperative diagnosis. In our case, the initial radiological examination raised suspicion for a space-occupying lesion, but the exact nature of the lesion could not be definitively determined prior to surgery. This highlights the importance of considering LFH as a potential differential diagnosis in cases presenting with similar clinical features.
The ligamentum flavum is an elongated ligamentous structure found in humans, spanning from the second cervical vertebra to the lumbosacral region. Comprising approximately 80% elastic fibers and 20% collagen, these ligaments play a supportive role in maintaining an upright posture. The exact pathogenesis of LFH remains unclear [3,9,19,26]. However, it has been hypothesized that degenerative or hypertrophic changes in the ligamentum flavum may lead to vascular proliferation within the tissue, rendering it susceptible to rupture following minor trauma [3]. While minor trauma or injury to the ligamentum flavum often occurs during lumbar punctures for epidural or intrathecal injections, there have been cases of LFH without any history of trauma or related injections [23]. The ligamentum flavum is typically characterized by a lack of significant vascularity, with only a few small vessels traversing it. Yayama et al. [27] performed a histological and immunohistochemical investigation into the degenerative alterations occurring in the ligamentum flavum. Their findings demonstrated significant microangiogenesis in the vicinity of disrupted elastic fibers and collagen fibrils.
Furthermore, all previously reported cases of lumbar LFH underwent surgical interventions, as nonoperative therapy was not effective. Consistent with the literature, our case also demonstrated favorable outcomes following surgical management. Complete removal of the hematoma in our patient resulted in immediate symptom relief and rapid recovery, confirming the efficacy of surgical intervention as the preferred treatment approach for LFH.
Due to the limited number of cases and the requirement for surgical intervention to establish a diagnosis, there are no prospective randomized trials available for LFH. The current standard of care involves surgical excision through laminectomy or hemilaminectomy. While most cases are managed surgically, there is a single case report describing the successful use of endoscopic treatment with favorable outcomes [1].
In addition, the histopathological examination conducted after our patient's surgery revealed the presence of necrotic ligament tissue surrounding the hematoma, indicating a paucity of blood vessels in the affected area. This observation may explain why LFH exhibits distinct signal patterns on MRI compared to typical hematomas, including epidural hematomas [2].
The MR imaging findings of LFH typically demonstrate signal characteristics consistent with blood, which can evolve over time due to the degradation of oxy-hemoglobin into hemosiderin. The location and morphology of LFH often mimic those of an extradural tumor, leading to a provisional preoperative diagnosis of tumor in approximately 25%-44% of LFH cases [29]. Contrast enhancement, although rare, has been occasionally observed in LFH. However, when present, it typically manifests as mild to moderate enhancement at the periphery of the lesion [29,30].
It is crucial for clinicians to maintain a high index of suspicion for LFH, especially in cases where other diagnoses are inconclusive or where there is a discrepancy between clinical presentation and imaging findings. Prompt recognition and appropriate surgical intervention can lead to successful outcomes, as demonstrated in our case and the previously reported cases.
Conclusion
LFH is a rare cause of spinal nerve compression, and its preoperative diagnosis remains challenging due to its rarity and overlapping clinical presentations with other conditions. Surgical removal of the hematoma provides excellent results, with rapid recovery and resolution of symptoms. Increased awareness of LFH among clinicians can lead to timely diagnosis and appropriate management, improving patient outcomes.
Patient consent
Written, informed consent for publication was obtained from the patient.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Ohba T., Ebata S., Ando T., Ichikawa J., Clinton D., Haro H. Lumbar ligamentum flavum hematoma treated with endoscopy. Orthopedics. 2011;34(7):e324–e327. doi: 10.3928/01477447-20110526-27. [DOI] [PubMed] [Google Scholar]
- 2.Liu H.P., Chen C.L., Chen N.F., Liao C.Y., Ou C.Y. Ligamentum flavum hematoma due to stretching exercise. Am J Emer Med. 2016;34(10):2058.e3–2058.e6. doi: 10.1016/j.ajem.2016.03.042. [DOI] [PubMed] [Google Scholar]
- 3.Tamura T., Sakai T., Sairyo K., Takao S., Kagawa S., Katoh S., Yasui N. Hematoma in the cervical ligamentum flavum. Report of a case and review of the literature. Skelet Radiol. 2010;39:289–293. doi: 10.1007/s00256-009-0805-8. [DOI] [PubMed] [Google Scholar]
- 4.Ozdemir B., Kanat A., Batcik O.E., Gucer H., Yolas C. Ligamentum flavum hematomas: why does it mostly occur in old Asian males? Interesting point of reported cases: review and case report. J Craniovertebr Junct Spine. 2016;7(1):7. doi: 10.4103/0974-8237.176605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sweasey T.A., Coester H.C., Rawal H., Blaivas M., McGillicuddy J.E. Ligamentum flavum hematoma: report of two cases. J Neurosurg. 1992;76(3):534–537. doi: 10.3171/jns.1992.76.3.0534. [DOI] [PubMed] [Google Scholar]
- 6.Baker J.K., Hanson G.W. Cyst of the ligamentum flavum. Spine. 1994;19(9):1092–1094. doi: 10.1097/00007632-199405000-00019. [DOI] [PubMed] [Google Scholar]
- 7.Cruz-Conde R., Berjano P., Buitron Z. Ligamentum flavum hematoma presenting as progressive root compression in the lumbar spine. Spine. 1995;20(13):1506–1509. doi: 10.1097/00007632-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Mahallati H., Wallace C.J., Hunter K.M., Bilbao J.M., Clark A.W. MR imaging of a hemorrhagic and granulomatous cyst of the ligamentum flavum with pathologic correlation. Am J Neuroradiol. 1999;20(6):1166–1168. [PMC free article] [PubMed] [Google Scholar]
- 9.Minamide A., Yoshida M., Tamaki T., Natsumi K. Ligamentum flavum hematoma in the lumbar spine. J Orthop Sci. 1999;4:376–379. doi: 10.1007/s007760050119. [DOI] [PubMed] [Google Scholar]
- 10.Hirakawa K., Hanakita J., Suwa H., Matsuoka N., Oda M., Muro H., Fukushima T. A post-traumatic ligamentum flavum progressive hematoma: a case report. Spine. 2000;25(9):1182–1184. doi: 10.1097/00007632-200005010-00021. [DOI] [PubMed] [Google Scholar]
- 11.Yüceer N., Başkaya M.K., Smith P., Willis B.K. Hematoma of the ligamentum flavum in the lumbar spine: case report. Surg Neurol. 2000;53(6):598–600. doi: 10.1016/s0090-3019(00)00187-7. [DOI] [PubMed] [Google Scholar]
- 12.Chi T.W.C., Li K.T., Chieng P.U. Post-traumatic ligamentum flavum hematoma: a case report. Kaohsiung J Med Sci. 2004;20(1):41–43. doi: 10.1016/S1607-551X(09)70083-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mizuno J, Nakagawa H, Inoue T, Hashizume Y. Ligamentum flavum hematoma in the lumbar spine. Neurol Med Chir (Tokyo) 2005;45(4):212–215. doi: 10.2176/nmc.45.212. [DOI] [PubMed] [Google Scholar]
- 14.Yamaguchi S, Hida K, Akino M, Seki T, Yano S, Iwasaki Y. Ligamentum flavum hematoma in the lumbar spine. Neurol Med Chir (Tokyo) 2005;45(5):272–276. doi: 10.2176/nmc.45.272. [DOI] [PubMed] [Google Scholar]
- 15.Albanese A., Braconi A., Anile C., Mannino S., Sabatino G., Mangiola A. Spontaneous haematoma of ligamentum flavum. Case report and literature review. J Neurosurg Sci. 2006;50(2):59–61. [PubMed] [Google Scholar]
- 16.Keynan O., Smorgick Y., Schwartz A.J., Ashkenazi E., Floman Y. Spontaneous ligamentum flavum hematoma in the lumbar spine. Skelet Radiol. 2006;35:687–689. doi: 10.1007/s00256-005-0945-4. [DOI] [PubMed] [Google Scholar]
- 17.Shimada Y., Kasukawa Y., Miyakoshi N., Hongo M., Ando S., Itoi E. Chronic subdural hematoma coexisting with ligamentum flavum hematoma in the lumbar spine: a case report. Tohoku J Exp Med. 2006;210(1):83–89. doi: 10.1620/tjem.210.83. [DOI] [PubMed] [Google Scholar]
- 18.Spuck S., Stellmacher F., Wiesmann M., Kranz R. A rare cause of radicular complaints: ligamentum flavum hematoma. Clin Orthop Relat Res®. 2006;443:337–341. doi: 10.1097/01.blo.0000195412.21988.41. [DOI] [PubMed] [Google Scholar]
- 19.Gazzeri R, Canova A, Fiore C, Galarza M, Neroni M, Giordano M. Acute hemorrhagic cyst of the ligamentum flavum. J Spinal Disord Tech. 2007;20(7):536–538. doi: 10.1097/BSD.0b013e31804b4605. [DOI] [PubMed] [Google Scholar]
- 20.Kotil K., Bilge T. A ligamentum flavum hematoma presenting as an L5 radiculopathy. J Clin Neurosci. 2007;14(10):994–997. doi: 10.1016/j.jocn.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 21.Kono H., Nakamura H., Seki M., Motoda T. Foot drop of sudden onset caused by acute hematoma in the lumbar ligamentum flavum: a case report and review of the literature. Spine. 2008;33(16):E573–E575. doi: 10.1097/BRS.0b013e31817c6cb5. [DOI] [PubMed] [Google Scholar]
- 22.Miyakoshi N., Kasukawa Y., Ando S., Shimada Y. Two-level ligamentum flavum hematoma in the lumbar spine. Case report. Neurol Med-Chir. 2008;48(4):179–182. doi: 10.2176/nmc.48.179. [DOI] [PubMed] [Google Scholar]
- 23.Takahashi H., Wada A., Yokoyama Y., Fukushi S., Sakurai T., Shibuya K., Suguro T. Ligamentum flavum haematoma: a report of two cases. J Orthop Surg. 2009;17(2):212–215. doi: 10.1177/230949900901700219. [DOI] [PubMed] [Google Scholar]
- 24.Ghent F., Ye X., Yan M., Mobbs R.J. A contrast-enhancing lumbar ligamentum flavum haematoma. Case Rep. 2014;2014 doi: 10.1136/bcr-2013-202521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ishimoto Y., Kawakami M., Curtis E., Cooper C., Moriguchi N., Nakagawa Y. A succession of MRI scans supports the diagnosis of lumbar ligamentum flavum hematoma: a case report and review of the literature. Case Rep Orthop. 2018;2018 doi: 10.1155/2018/2860621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Miyakoshi N., Shimada Y., Kasukawa Y., Ando S. Ligamentum flavum hematoma in the cervical spine—case report. Neurol Med-Chir. 2006;46(11):556–558. doi: 10.2176/nmc.46.556. [DOI] [PubMed] [Google Scholar]
- 27.Yayama T., Kobayashi S., Sato R., Uchida K., Kokubo Y., Nakajima H., et al. Calcium pyrophosphate crystal deposition in the ligamentum flavum of degenerated lumbar spine: histopathological and immunohistological findings. Clin Rheumatol. 2008;27(5):597–604. doi: 10.1007/s10067-007-0754-3. [DOI] [PubMed] [Google Scholar]
- 28.Hisamitsu Y., Uchikado H., Makizono T., Miyagi T., Miyahara T. Case of lumbar ligamentum flavum hematoma with epidural hematoma resulting in cauda equina compression. Surg Neurol Int. 2022;13:550. doi: 10.25259/SNI_967_2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Takahashi M., Satomi K., Hasegawa A., Hasegawa M., Taki N., Ichimura S. Ligamentum flavum hematoma in the lumbar spine. J Orthop Sci. 2012;17:308–312. doi: 10.1007/s00776-011-0083-x. [DOI] [PubMed] [Google Scholar]
- 30.Takeno K., Kobayashi S., Miyazaki T., Yayama T., Baba H. Microsurgical excision of hematoma of the lumbar ligamentum flavum. Joint Bone Spine. 2010;77(4):351–354. doi: 10.1016/j.jbspin.2010.01.018. [DOI] [PubMed] [Google Scholar]
- 31.Sahri IE, Tlemcani ZC, Abide A, Obame FLO, Ramdani H, Mohammed M, et al. Ligamentum flavum hematoma in the lumbar spine mimicking spinal tumor: a case report and review of the literature. Radiol Case Rep. 2023;2023 doi: 10.1016/j.radcr.2023.05.073. [DOI] [PMC free article] [PubMed] [Google Scholar]