Abstract
Case series summary
Three cats (five stifles) were diagnosed with varying degrees of pelvic limb lameness secondary to medial patellar luxations (MPLs). Lameness did not resolve with medical management in any cat before referral for orthopedic evaluation. All cats underwent semi-cylindrical recession trochleoplasty (SCRT), medial fascial release and lateral imbrication for surgical repair of MPLs. All cats were re-evaluated at 3 and 8 weeks postoperatively and two cats were also evaluated at 16 weeks postoperatively. At the final rechecks, all cats had resolution of lameness of the operated limb(s) and no evidence of recurrence of patellar luxation.
Relevance and novel information
This case series demonstrated SCRT with soft tissue reconstruction as an acceptable option for surgical correction in three cats with MPLs. Short-term outcomes revealed minor complications and all patellae remained centralized.
Keywords: Medial patellar luxation, semi-cylindrical recession trochleoplasty, lameness, trochlear recession
Introduction
Medial patellar luxation (MPL) has been recognized as the most common cause of feline developmental pelvic limb lameness.1–4 Many clinically normal cats have some degree of patellar laxity that is considered normal, while some cats are asymptomatic in the presence of patellar luxation.1,3,5,6 Clinical signs of MPL in cats may include a crouching or shuffling gait, reluctance to jump, bowlegged conformation and intermittent locking of the affected stifle joint(s) during extension.1–4
The most commonly used grading scheme for patellar luxation is a I–IV scale initially described by Putnam 7 for use in dogs. Owing to the increased laxity in the feline stifle, multiple clinicians have proposed alternative grading schemes for feline patellar luxation, including a ‘– to 3+’ scale, A–D scale and modifications of the Putnam scale to account for cats that exhibit patellar laxity (or subluxation) without fully luxating their patella outside of the trochlear ridge.1,5–9 It has been suggested that the severity of luxation (Putnam grade) may not correlate with the severity of lameness, as similar severity of clinical signs may be seen across various Putnam grades. 3 For cats with low-grade patellar luxations (Putnam grades I and II), non-surgical management has been reported to provide an excellent outcome in 47% of cases and a good outcome in 29% of cases. 3 However, in cats with higher-grade patellar luxations (Putnam grades III and IV), the outcomes were not as favorable, suggesting surgical intervention may be indicated in cats with higher-grade luxations or those with persistent lameness.2,3
The described surgical treatment options for canine patellar luxations include the following: femoral trochleoplasty (recession or abrasion); tibial tuberosity transposition (TTT); capsular/retinacular release; capsular/retinacular imbrication; patellar stabilization procedures including figure-of-eight or antirotational sutures; and corrective osteotomies in severe cases.10–13 Traditionally, the surgical techniques recommended for repair of feline MPLs have been the same utilized for repair of canine MPLs.3,8,14,15 The implementation of these procedures in cats has resulted in good clinical outcomes, 3 with up to 74% of stifles successfully corrected without complications. 14 The same study reported an overall complication rate of 26%, of which 20% were major complications. 14 Of these, the most common major complication was implant related (when TTT was utilized), and the overall patellar reluxation rate across the various MPL reparative procedures performed was 5%. 14 Other techniques, such as sulcal ridge prostheses 16 and patellar groove replacement (PGR), 17 have rarely been adapted for use in cats.
Femoral trochleoplasty is considered a mainstay for the surgical management of patellar luxation in cats.10,11,14,18,19 Multiple trochleoplasty techniques have been reported, with trochlear wedge recession (TWR) and trochlear block recession (TBR) being among the more common cartilage preservation techniques performed.6,18–20 There is emerging evidence that suggests that the wider, flatter shape of the feline patella may prevent stable tracking with trochleoplasty techniques, potentially necessitating a parasagittal patellectomy.15,21 In particular, one cadaveric study showed that TBR did not improve patellar recession, as the wide feline patella rode the trochlear ridges instead of sinking into the deepened sulcus. 21 The unique anatomy of the feline stifle, as well as the relatively high complication rate associated with surgical correction of feline patellar luxation, warrants investigation into alternative sulcoplasty techniques.
Semi-cylindrical recession trochleoplasty (SCRT) is a novel technique performed in canine MPLs, yielding similar functional outcomes as TBR, as reported in a recent pilot study. 19 The proposed benefits of the SCRT over TBR include its subjectively easier application, particularly in small patients, and the resulting rounded osteotomy reducing the chance of fracturing of the trochlear ridges. 19 Other benefits include the production of ample, residual, corticocancellous bone that can be used as an autograft if TTT is performed. 19 When considering the smaller size of most cats, as well as the previously reported wider shapes of the feline patellae, investigation into use of the SCRT in cases of feline MPL is warranted.
To the authors’ knowledge, the use of the SCRT technique has not been reported in feline MPL correction. The purpose of this case series was to describe the adaptation and use of SCRT in the treatment of feline MPL, and to report on the short-term outcomes and complications. For the purposes of this study, the modified Putnam grading scale as described by Smith et al1,7 was used, in which an additional subgrade (subgrade I) was developed to describe cats in which the patella could not be manually luxated out of the trochlear groove but had excessive side-to side motion or could be pushed to sit on the trochlear ridge without luxating beyond it.
Case series description
Three cats with higher-grade (grade III or IV) MPLs underwent SCRTs performed by one residency-trained surgeon (SV). Pre- and postoperative radiographs (Figure 1) were obtained for all cats. Analgesia included fentanyl constant rate infusions (CRIs) and a single subcutaneous (SC) injection of robenacoxib (Onsior; Elanco Animal Health) before transitioning to oral buprenorphine, gabapentin and robenacoxib. One week of antibiotics (amoxicillin trihydrate/clavulanate potassium [Clavamox Drops; Zoetis]) was also prescribed.
Figure 1.
(a) Preoperative orthogonal stifle radiographs of case 1 showing a grade III/IV medial patellar luxation (MPL). (b) Immediate postoperative radiographs revealing a centralized patella. (c) Final radiographs 8 weeks after MPL repair confirm radiographic healing with a centralized patella
Case 1
Case 1 was a 6-month-old neutered male domestic shorthair cat with bilateral MPLs. The cat acutely developed bilateral pelvic limb lameness with the inability to jump. Medical management was attempted for 12 days without improvement before referral. The examination revealed bilateral weightbearing pelvic limb lameness with a crouched stance, discomfort on stifle extension and bilateral grade IV/IV MPLs.
A left-sided lateral stifle approach with bilateral parapatellar arthrotomy (to facilitate guidewire placement [Figure 2a] and as a prerequisite for adjunctive soft tissue repair) was made (Table 1). An SCRT (SCRT Instrument Set; New Generation Devices) was performed, as described by Blackford-Winders et al. 19 An aiming guide (AR-1510H, AR-1510F; Arthrex) was used to place a 0.045 inch Kirschner wire (K-wire) in a distal to proximal direction, centered caudal to the femoral sulcus. The K-wire was inserted just cranioproximal to the intercondylar fossa and exited approximately 3 mm proximal to the sulcus. A cutting guide was placed onto the K-wire to guide a 6 mm SCRT saw blade. A trochleoplasty was performed and the superficial osteochondral semi-cylinder autograft was preserved. A deeper cut was then performed using the 5 mm blade. This second, 3 mm deeper cut, created a femoral autograft of 2–3 mm that was removed from the field. The K-wire was removed and the remaining discrepancies in the sulcal ridge width/depth were amended with a rasp. The osteochondral autograft was then pressed into place (Figure 2b). The patella was reduced, with approximately 50% of the patella now sitting below the trochlear ridges. Lateral imbrication and medial release were performed as previously described 6 and the site closed routinely.
Figure 2.
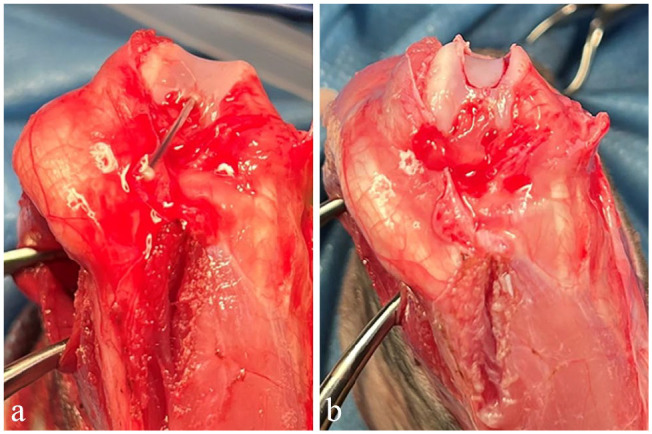
Intraoperative craniocaudal view of the flexed stifle before and after semi-cylindrical recession trochleoplasty (case 1): (a) axial view of the left stifle during exploration via bilateral parapatellar arthrotomy showing a markedly shallow trochlear groove. A K-wire has been inserted just proximal to the intercondylar fossa, exiting approximately 3 mm proximal to the most proximal edge of the femoral sulcus in preparation for use of the cutting guide and (b) replacement of the osteochondral autograft after trochleoplasty revealing the improved depth of the trochlear groove and good autograft-femoral contact
Table 1.
Case details of cats that underwent surgical correction for medial patellar luxations (MPLs)
| Variable | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| Age | 6 months | 10 months | 3 years |
| Breed | DSH | DSH | DMH |
| Sex | M(N) | F(N) | F(N) |
| Weight (kg) | 3.0 | 3.7 | 3.6 |
| Preoperative patellar luxation grade | IV/IV (L) IV/IV (R) |
III/IV (L) III/IV (R) |
III/IV (L) III/IV (R) |
| Abnormalities found during joint exploration (side noted in parenthesis) | Markedly shallow trochlear groove (bilateral) | Markedly shallow trochlear groove (L) | Markedly shallow trochlear groove (bilateral); eburnation of the medial trochlear ridge (bilateral) |
| SCRT blade sizes used (in order of use) | 6 mm, 5 mm | 7 mm, 6 mm | 6 mm, 5 mm, 4 mm |
| Intraoperative assessment of tibial tuberosity position | Reasonably aligned with quadriceps mechanism; TTT not performed | Reasonably aligned with quadriceps mechanism; TTT not performed | Reasonably aligned with quadriceps mechanism; TTT not performed |
| Soft tissue reconstructive procedures performed | Lateral imbrication and medial release | Lateral imbrication and medial release | Lateral imbrication and medial release |
DSH = domestic shorthair; DMH = domestic mediumhair; F(N) = female neutered; L = left; M(N) = male neutered; MPL = medial patellar luxation; R = right; SCRT = semi-cylindrical recession trochleoplasty; TTT = tibial tuberosity transposition
The 2-week recheck was unremarkable. An identical right-sided procedure was then performed 1 month postoperatively.
No complications were identified at the 10-day or 3-week rechecks after the right-sided procedure. Postoperative stifle radiographs were performed 8 weeks after the right MPL repair (12 weeks after the left side), which confirmed centralized patellae.
The final recheck examination was performed 16 weeks after the right MPL repair (20 weeks after the left). There was no visual pelvic limb lameness, and non-painful stifle peri-articular fibrosis and excellent range of motion were noted bilaterally. The patellae remained centralized, but subjective bilateral patellar laxity (modified Putnam subgrade I/IV) was present.
Case 2
Case 2 was a 10-month-old neutered female domestic shorthair cat with bilateral MPLs. The cat acutely developed left pelvic limb lameness with no inciting cause. Medical management was attempted for several weeks without improvement before referral. Examination revealed a bilateral crouched pelvic limb gait, bilateral grade III/IV MPLs and mild pelvic limb muscle atrophy.
Left MPL correction was performed as described for case 1 apart from blade sizes (Table 1). No complications were identified during recheck exams. Radiographs of the left stifle were obtained 8 weeks after surgery, revealing a normal left patella location and moderate stifle effusion.
The 16-week recheck revealed no visual left pelvic limb lameness, a centralized patella and excellent stifle range of motion. There was a persistent weightbearing right pelvic limb lameness with failure to extend the right stifle, moderate internal rotation of the right stifle compared to the left (Figure 3) and a static grade III/IV right MPL. At the time of publication, the cat’s owners were considering right MPL correction.
Figure 3.
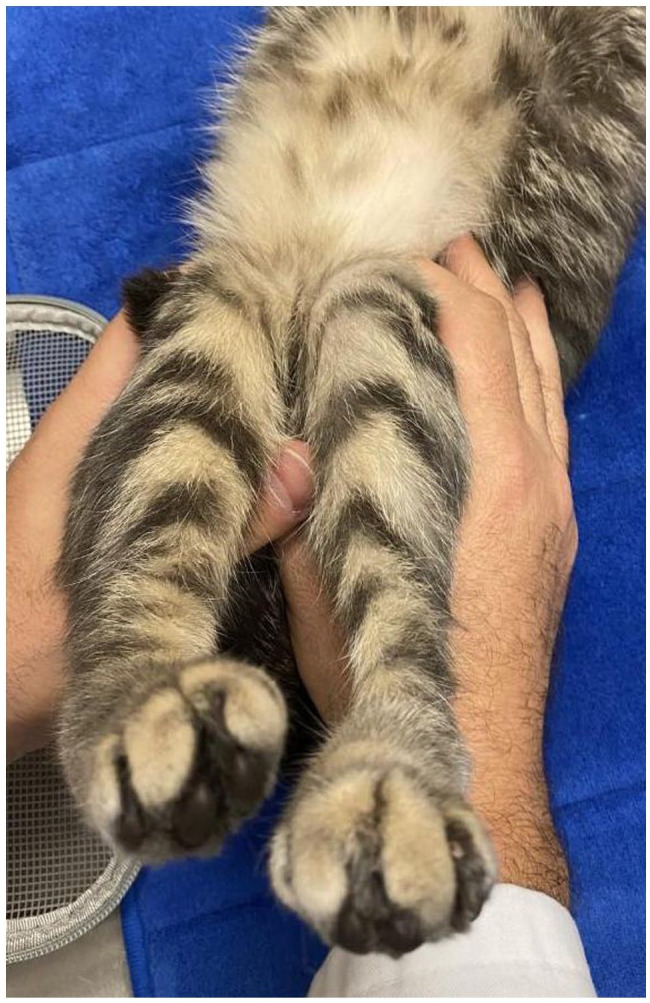
Internal rotation of the right stifle (with grade III/IV medial patellar luxation [MPL]) compared with the left in dorsal recumbency at case 2’s 16-week recheck examination after repair of the left MPL
Case 3
Case 3 was an estimated 3-year-old neutered female domestic mediumhair cat with bilateral MPLs. The cat consistently exhibited bilateral pelvic limb lameness and crouched gait since adoption. Medical management was attempted for several months without improvement before referral. Orthopedic examination revealed bilateral grade III/IV MPLs, left pelvic limb weakness with fasciculations and the right femoral sulcus was subjectively more palpably shallow than the left.
Left MPL correction was performed as described for case 1 apart from blade sizes and the use of a third blade (Table 1). No complications were identified during initial recheck examinations. The 8-week postoperative radiographs of the left stifle revealed a centralized patella and incidental meniscal mineralization. An examination of the left pelvic limb revealed no lameness, excellent stifle range of motion and a centralized patella; under sedation, the left patella had a grade I/IV medial luxation during full stifle extension.
An identical (Table 1) right-sided MPL repair was performed 8 weeks after the left SCRT. No complications were identified at the 1-week and 3-week rechecks after the right-sided SCRT.
The final recheck was performed 16 weeks after the left MPL repair (8 weeks after the right). Stifle radiographs confirmed centralized patellae and incidental meniscal mineralization. The cat remained sound, and the left patella could no longer be luxated. There was mild bilateral patellar laxity (modified Putnam subgrade I/IV).
Discussion
Historically, techniques described for use in the correction of canine MPLs have been adapted for use in felines due to the paucity of feline-specific literature. With reports emerging in support of the unique features of the feline patella,15,21 research into more feline-appropriate corrective procedures is warranted. This case series describes excellent short-term outcomes in three cats (five stifles) after SCRTs for the treatment of feline MPL.
Trochleoplasty is considered a fundamental component of MPL correction in most patients.10,11,14,18,19 In normal cadaveric feline stifles, the patella has been found to be up to 1 mm wider than the trochlea, with only 10–20% of the patella recessed under the trochlear ridges. 21 After TBR on these stifles, no improvement in patellar recession was present, as the patella was too wide to sink into the recessed sulcus. 21 Parasagittal patellectomy was developed to narrow the patella and allow for improved patellar recession when combined with traditional trochleoplasties.15,21 In this case series, subjective intraoperative assessment revealed approximately 50% of the patella to be sitting below the trochlear ridges after SCRT in all cats without parasagittal patellectomy. The authors theorize that this may be due to the use of a rounded, power-driven saw blade allowing for the precise creation of a wide osteotomy. However, it is also possible that cats in this series had patellae that fit into the trochlear ridge.
The rate of patellar reluxation at the time of final recheck in this case series was 0/5 stifles (0%). Reluxation rates as low as 5% have been reported in some feline studies 14 vs 8% in dogs. 11 In dogs, rates were significantly reduced (25% to 6%) when a TTT was performed, 11 but no significant difference was found in a similar feline study. 14 Furthermore, performing a sulcoplasty did not statistically reduce feline reluxations 14 compared with a significant reduction in canines (21% to 6%). 11 Theoretically, this is due to the relatively thinner and wider feline patella in relation to the femoral sulcus.4,14,15,21 A 0% short-term reluxation rate in our study is comparable to previous reports, but a larger population of cats undergoing SCRT procedures would be necessary to better delineate the true risk of reluxation and appropriately compare it to reported data. One cat developed a (temporary) reluxation at the 8-week evaluation, but the luxation had resolved (even under heavy sedation) at the time of the final recheck. As this (temporary) reluxation required no treatment for resolution, it was classified as a minor complication, as proposed by Cook et al, 22 for the purposes of this study. The cause of resolution is unknown but continued soft tissue remodeling is suspected. A longer-term follow-up would be necessary to monitor for recurrence.
Two cats (four stifles) developed clinically insignificant patellar laxity (modified Putnam subgrade I/IV patellar luxation). Multiple reports suggest many cats appear to have a degree of patellar laxity.1,3,15 In one study, 31/33 (94%) cats exhibited laxity without lameness. 1 At the time of publication (>6 and 5 months after surgery for case 1 and case 3, respectively), both cats were ambulating without owner-perceived lameness. The initial results are supportive of previous reports, suggesting patellar laxity is subclinical in most felines.
TTT is considered a mainstay in the repair of many canine and feline MPLs by correcting the malalignment of the quadriceps mechanism (when indicated).2–4,6,8,10–15 Combining TTT with a trochleoplasty has been shown to result in a five-fold decrease in the rate of patellar reluxation in one canine study, 12 but similar benefits have yet to be definitively shown in a similar feline study. 14 In fact, 22% of cats had TTT implant-related complications, 14 compared with only 4% of dogs. 12 Furthermore, the most common major complication was implant related (TTT) in cats vs patellar reluxation in dogs.12,14 The cause of the increased rate of TTT-related complications in the cat compared with the dog is unknown, but use of overly large (‘dog-sized’) implants, unique handling properties of feline bone, differences in tuberosity size, conformation (more stifle flexion during ambulation) and higher avulsive forces (ie, jumping) have been proposed. 14 The decision on whether to perform a TTT is often clinician-dependent and made on intraoperative assessment of the alignment of the quadriceps mechanism and propensity of the patella to continue to luxate after other reparative procedure(s) (ie, trochleoplasty ± medial release and lateral imbrication). As such, intraoperative assessment of quadriceps alignment in the stifles in this study revealed reasonable alignment (ie, no excessive deviation from midline) in all stifles, and a TTT was deemed unnecessary. The authors propose assessing quadriceps alignment and weighing the risk vs benefit of performing a TTT in feline MPL correction (risk of implant-related complications vs patellar reluxation).
One limitation of this study is its small case size. Gathering data on a larger number of cats undergoing correction of their patellar luxation may be challenging considering that the incidence of clinically significant MPLs in cats is believed to be as low as 14%. 1 Furthermore, to the authors’ knowledge, limited institutions are currently utilizing the SCRT procedure in treatment of MPL in dogs, let alone feline patients. Further studies pooling data across multiple hospitals over a longer period would allow for increased case numbers.
The ideal parameters for semi-cylindrical trochleoplasty width and depth are currently unknown in canines and felines. Biomechanical cadaveric studies may aid in the further development of procedural specifications and provide further insight into potential limitations and risks; however, finding an adequate and representative sample size may be challenging considering the low incidence of feline MPLs 1 (particularly in cadavers). Until data from such studies are available, removal of the minimal amount of the trochlea that prevents continued patellar luxation appears judicious.
Additional limitations include the use of only intraoperative assessment of patellar recession and patellofemoral contact. While postoperative radiographs confirmed centralized patellae, no information on the true degree of patellar recession or patellofemoral contact was possible. The long-term importance of these factors in light of an appropriately tracking patella on examination in felines is unknown, 21 though some human literature postulates that the loss of normal patellofemoral contact may lead to cartilage degradation and osteoarthritis formation. 23 Postoperative assessment with CT and a longer-term follow-up are ideal.
Further limitations include the lack of objective measurements of limb function. While all cats returned to subjectively normal function on their surgical limb(s), no objective assessments of limb function such as force-plate analysis or questionnaires were utilized. Questionnaires should be considered to allow for assessment of owner-perceived postoperative outcomes. Force-plate analysis is ideal and has historically been used as a non-invasive objective assessment of gait, though the increased cost and potential for non-compliance of feline patients in a hospital setting may preclude its use in clinical practice.
Other limitations of this study include lack of longer-term follow-up. All cases had a minimum follow-up of 2 months (and all but one stifle had a minimum follow-up of 4 months); however, it is possible that longer-term complications could develop. While bone generally returns to full strength in 12 weeks, poorly vascularized soft tissues (like fascia) may take closer to 1 year. 24 The primary focus of this study was the SCRT procedure; however, all SCRTs were paired with soft tissue reconstructive procedures, which may not have healed by the time of publication. While the development of longer-term complications is not anticipated, a longer follow-up is necessary to definitively identify and evaluate the significance of any occurrences.
Conclusions
The SCRT procedure was successfully performed in three cats (five stifles) with excellent short-term functional outcomes. While the initial results appear promising, larger, longer-term prospective studies are warranted for further evaluation on the use of SCRT in correction of feline MPLs.
Acknowledgments
The authors would like to thank the dedicated nursing staff of PBVS for their care of the SCRT cats and all of their patients.
Footnotes
Accepted: 16 May 2023
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The open-access publication of this article was supported by VCA. The authors received no financial support for the research and authorship of this article.
Ethical approval: The work described in this manuscript involved the use of non-experimental (owned or unowned) animals. Established internationally recognized high standards (‘best practice’) of veterinary clinical care for the individual patient were always followed and/or this work involved the use of cadavers. Ethical approval from a committee was therefore not specifically required for publication in JFMS Open Reports. Although not required, where ethical approval was still obtained, it is stated in the manuscript.
Informed consent: Informed consent (verbal or written) was obtained from the owner or legal custodian of all animal(s) described in this work (experimental or non-experimental animals, including cadavers) for all procedure(s) undertaken (prospective or retrospective studies). No animals or people are identifiable within this publication, and therefore additional informed consent for publication was not required.
ORCID iD: Kristen Deom  https://orcid.org/0000-0003-3052-9477
https://orcid.org/0000-0003-3052-9477
References
- 1.Smith GK, Langenbach A, Green PA, et al. Evaluation of the association between medial patellar luxation and hip dysplasia in cats. J Am Vet Med Assoc 1999; 215: 40–45. [PubMed] [Google Scholar]
- 2.Houlton JEF, Meynink SE. Medial patellar luxation in the cat. J Small Anim Pract 1989; 30: 349–352. [Google Scholar]
- 3.Loughin CA, Kerwin SC, Hosgood G, et al. Clinical signs and results of treatment in cats with patellar luxation: 42 cases (1992-2002). J Am Vet Med Assoc 2006; 228: 1370–1375. [DOI] [PubMed] [Google Scholar]
- 4.Beer AJC, Langley-Hobbs S, Belch A.Comparison of hindlimb conformation in cats with and without medial patellar luxation. Vet Comp Orthop Traumatol 2023; 36: 10–20. [DOI] [PubMed] [Google Scholar]
- 5.Engvall E, Bushnell N.Patellar luxation in Abyssinian cats. Feline Pract 1990; 18: 20–22. [Google Scholar]
- 6.Hudson C.Surgical correction of patellar luxation in cats. TVP 2014; 4: 32–37. [Google Scholar]
- 7.Putnam RW.Patellar luxation in the dog. MSc thesis, University of Guelph, Canada, 1968. [Google Scholar]
- 8.Grierson J.Hips, elbows and stifles: common joint diseases in the cat. J Feline Med Surg 2012; 14: 23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Voss K, Langley-Hobbs SJ, Montavon PM.Stifle joint. In: Montavon PM, Voss K, Langley-Hobbs SJ. (eds). Feline orthopedic surgery and musculoskeletal disease. Edinburgh: Elsevier, 2009, pp 475–490. [Google Scholar]
- 10.Rossanese M, German AJ, Comerford E, et al. Complications following surgical correction of medial patellar luxation in small-to-medium-size dogs. Vet Comp Orthop Traumatol 2019; 32: 332–340. [DOI] [PubMed] [Google Scholar]
- 11.Arthurs GI, Langley-Hobbs SJ.Complications associated with corrective surgery for patellar luxation in 109 dogs. Vet Surg 2006; 35: 559–566. [DOI] [PubMed] [Google Scholar]
- 12.Cashmore RG, Havlicek M, Perkins NR, et al. Major complications and risk factors associated with surgical correction of congenital medial patellar luxation in 124 dogs. Vet Comp Orthop Traumatol 2014; 27: 263–270. [DOI] [PubMed] [Google Scholar]
- 13.Linney WR, Hammer DL, Shott S.Surgical treatment of medial patellar luxation without femoral trochlear groove deepening procedures in dogs: 91 cases (1998–2009). J Am Vet Med Assoc 2011; 238: 1168–1172. DOI: 10.2460/javma.238.9.1168. [DOI] [PubMed] [Google Scholar]
- 14.Rutherford L, Langley-Hobbs SJ, Whitelock RJ, et al. Complications associated with corrective surgery for patellar luxation in 85 feline surgical cases. J Feline Med Surg 2015; 17: 312–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rutherford L, Arthurs GI.Partial parasagittal patellectomy: a novel method for augmenting surgical correction of patellar luxation in four cats. J Feline Med Surg 2014; 16: 689–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mills J, Hargittai T.Treatment of feline patellar luxation with polyethylene sulcal ridge prostheses. J Small Anim Pract 2020; 61: 704–709. [DOI] [PubMed] [Google Scholar]
- 17.Jaworski J, Krukowski M, Gosling M, et al. Patellar groove replacement in a cat. Vet Comp Orthop Traumatol 2022; 5: e71–e77. [Google Scholar]
- 18.Johnson AL, Probst CW, DeCamp CE, et al. Comparison of trochlear block recession and trochlear wedge recession for canine patellar luxation using a cadaver model. Vet Surg 2001; 30: 140–150. [DOI] [PubMed] [Google Scholar]
- 19.Blackford-Winders CL, Daubert M, Rendahl AK, et al. Comparison of semi-cylindrical recession trochleoplasty and trochlear block recession for the treatment of canine medial patellar luxation: a pilot study. Vet Comp Orthop Traumatol 2021; 34: 183–190. [DOI] [PubMed] [Google Scholar]
- 20.Talcott KW, Goring RL, de Haan JJ.Rectangular recession trochleoplasty for treatment of patellar luxation in dogs and cats. Vet Comp Orthop Traumatol 2000; 13: 39–43. [Google Scholar]
- 21.Brioschi V, Rutherford L, Newell K, et al. Computed tomographic assessment of block recession trochleoplasty and partial parasagittal patellectomy in cats. Vet Comp Orthop Traumatol 2020; 33: 102–109. [DOI] [PubMed] [Google Scholar]
- 22.Cook JL, Evans R, Conzemius MG, et al. Proposed definitions and criteria for reporting time frame, outcome, and complications for clinical orthopedic studies in veterinary medicine. Vet Surg 2010; 39: 905–908. [DOI] [PubMed] [Google Scholar]
- 23.Marder RA, Swanson TV, Sharkey NA, et al. Effects of partial patellectomy and reattachment of the patellar tendon on patellofemoral contact areas and pressures. J Bone Jt Surg 1993; 75: 35–45. [DOI] [PubMed] [Google Scholar]
- 24.Shaw KK, Alvarez L, Foster SA, et al. Fundamental principles of rehabilitation and musculoskeletal tissue healing. Vet Surg 2020; 49: 22–32. [DOI] [PMC free article] [PubMed] [Google Scholar]



