Abstract
Background:
Large variations exist in the reported frequency and etiology of posterior and combined shoulder instability in the active-duty military population.
Purpose:
To compare imaging and clinical examination findings as well as reoperation rates between active-duty military patients who underwent surgery for anterior, posterior, and combined-type shoulder instability.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
A retrospective review was conducted on patients treated surgically for shoulder instability from a single military base from January 2010 to December 2019. Each case was characterized as isolated anterior, isolated posterior, or combined, according to arthroscopic findings. Information was collected on patient characteristics, history of trauma, time to surgery, associated pathological findings, and survivorship at a minimum 2-year follow-up.
Results:
Overall, 416 patients (n = 394 men; n = 22 women), with a mean age of 29.1 years, underwent primary shoulder stabilization surgery during the study period. There were 158 patients (38%) with isolated anterior instability, 139 (33%) with isolated posterior instability, and 119 (29%) with combined instability. A history of trauma was more prevalent with isolated anterior instability (129 [81.7%]) than with either isolated posterior (95 [68.4%]) or combined instability (73 [61.3%]) (P = .047 and P = .001, respectively). Patients with anterior instability were significantly more likely to be diagnosed on the preoperative physical examination when compared with patients with posterior instability (93% vs 79.1%; P < .001) or combined instability (93% vs 75.6%; P < .001) and were also more likely to have a discrete labral tear detected on a preoperative magnetic resonance arthrogram than patients with posterior instability (82.9% vs 63.3%; P < .001). There was no significant difference in the rate of medical discharge or recurrent instability requiring reoperation between groups.
Conclusion:
The study findings indicated that young, active-duty military patients are at increased risk for isolated posterior and combined-type shoulder instability, with posterior and combined instability collectively accounting for over 60% of instability cases in this cohort. Orthopaedic surgeons should be aware of instability when evaluating and treating young, active-duty military patients with shoulder pain, even in the absence of diagnostic physical examinations or imaging findings.
Keywords: arthroscopy, military training, posterior instability, shoulder instability, shoulder surgery
Shoulder instability is a common cause of pain and disability among active-duty members of the military.5,7,16,20,21,27 The glenohumeral joint is vulnerable to subluxation or dislocation when placed in compromising positions or subjected to repetitive load-bearing forces. 18 High–shoulder demand activities, such as push-ups and overhead lifting, which are required as part of military training, predispose soldiers to increased rates of these events and subsequent instability.4,14,26
Operative management is often indicated for the treatment of glenohumeral instability, particularly in high–shoulder demand populations whose symptomology may be refractory to conservative measures. 18 Successful restoration of stability requires the selection of appropriate surgical techniques as indicated by the anatomic location of the labral injury. 18 This is of particular importance in patients presenting with isolated posterior or combined anterior and posterior types of instability patterns, as these subtypes have historically been more difficult to identify preoperatively because of variability in clinical presentation and imaging findings.2,11,18 While anterior instability is the predominant subtype of instability diagnosed in the general population, higher incidences of posterior and combined instability have been reported in military cohorts, as well as in other young, active patient populations. #
The purpose of this study was to describe the epidemiology and etiology of surgically treated shoulder instability within a large, single-center cohort of active-duty military patients. Additionally, we sought to compare postoperative return to active-duty and reoperation rates among patients who underwent stabilization surgery for anterior, posterior, and combined-type instability. We hypothesized that military patients would experience relatively higher rates of posterior and combined-type instability when compared with civilian cohorts. Additionally, because of the known difficulty in diagnosing posterior and/or combined instability, we anticipated that patients with combined and posterior instability would experience higher rates of reoperation and medical discharge from the military.
Methods
This study is a retrospective analysis of prospectively collected data from active-duty military patients who underwent primary shoulder stabilization between January 2010 and December 2019. Institutional review board approval was obtained before beginning the study.
All active-duty military patients aged 18 to 50 years from a single military base who underwent a primary surgical procedure for shoulder instability with a minimum 2-year follow-up were eligible for inclusion in this study. Patients with a history of shoulder surgery and patients with instability secondary to generalized ligamentous laxity were excluded. All patients had activity-related pain that was severe enough to interfere with both activities of daily living and military job requirements and had failed ≥3 months of conservative management, including physical therapy, nonsteroidal anti-inflammatory drugs, limited-duty profiling, and home exercise programs before being considered for surgery. Additionally, all patients had at least a physical examination or imaging finding consistent with instability. A positive examination for anterior instability was defined as positive apprehension, relocation, and anterior release tests. Posterior apprehension, jerk, and Kim tests were performed to identify posterior instability, and an examination was considered diagnostic of posterior instability if 2 out of 3 tests were positive. A clinical diagnosis of combined instability was defined as an examination that was positive for both anterior and posterior instability.
Patient characteristics, including age, sex, and laterality, were obtained. Duration of symptoms, preoperative chief complaint, and mechanism of injury were also recorded. Traumatic etiology was defined as symptom onset after a specifically recalled acute event. All patients underwent a preoperative 1.5-T magnetic resonance arthrogram (MRA) (gadolinium contrast; sequences included T1, T2, and T2 fat-suppressed) as part of their clinical evaluation. Imaging reports were obtained, and findings, as reported by a board-certified musculoskeletal radiologist, were recorded. Operative reports were reviewed to determine the location of the labral tear, concomitant pathologies, and procedures performed. The direction of instability was labeled as anterior (2 o’clock to 6 o’clock position for a right shoulder), posterior (7 o’clock to 10 o’clock position for a right shoulder), or combination anterior-posterior . Medical discharge from the military and reoperation rates were collected as part of the postoperative evaluation.
Statistical Analysis
Statistical analyses were performed using the SPSS 20 software package (IBM). Chi-square tests were used to compare categorical variables between cohorts, and analysis of variance (ANOVA) tests were utilized to compare continuous data series with a normal distribution of variance. If ANOVA was found to be significant, post hoc chi-square comparisons were performed to determine the comparison of significance. As multiple comparisons were made among continuous data, we utilized the Tukey method to minimize the rate of type I error. Statistical significance was determined at P < .05. Bonferroni and Yates corrections were applied to chi-square post hoc analyses.
Results
During the study period, 5 orthopaedic surgeons performed 453 arthroscopic evaluations before shoulder stabilization procedures on patients from a single military base. A total of 37 patients were excluded because of a prior shoulder surgery, leaving 416 (91.8%) primary shoulder stabilization procedures performed on active-duty military patients (n = 394 men; n = 22 women) available for analysis. The mean age of the patients was 29.1 years (range 18-50 years). The direction of instability was determined arthroscopically and categorized as anterior in 158 (38.0%) patients, posterior in 139 (33.4%), and combined in 119 (28.6%) (Figure 1).
Figure 1.
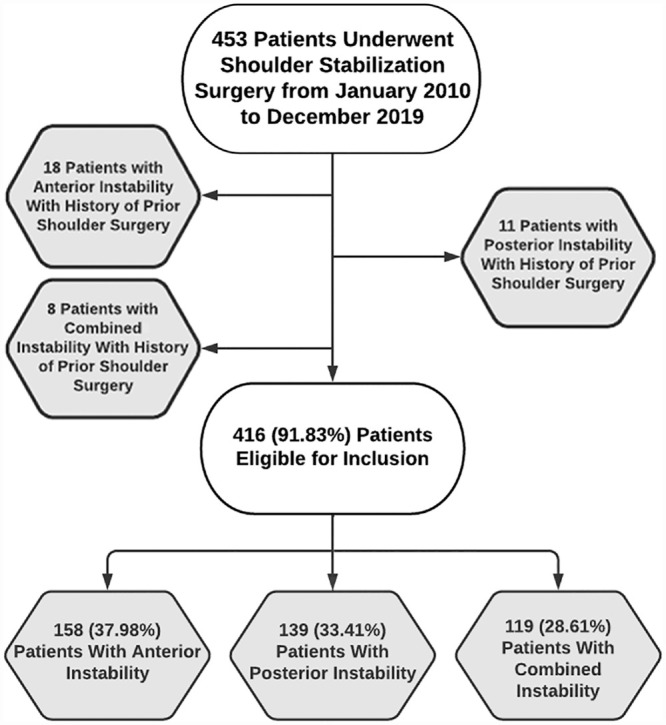
Flow diagram of the study enrollment procedure.
The anterior instability cohort was significantly younger than the posterior instability group (27.9 vs 30.1 years, respectively; P = .042). The mean age of patients in the combined group did not differ significantly from the mean age of patients in either the anterior or the posterior group. There were no statistically significant differences between the 3 groups regarding sex, side of surgery, or hand dominance (P = .172, P = .170, and P = .086, respectively).
Specific traumatic events were significantly more common in patients with anterior instability (129/158 [81.6%]) than with either posterior (95/139 [68.3%]) or combined instability (73/119 [61.3%]) (P = .047 and P = .001, respectively). There was no statistically significant difference in the history of traumatic events between patients with posterior instability and patients with combined instability (P = .240). Compared with patients with anterior instability (145/158 [91.77%]) (P < .0001 overall), those with posterior (139/139 [100%]) and combined instability (119/119 [100%]) were more likely to experience pain. Patients with anterior instability (151/158 [95.57%]) were significantly more likely to endorse subjective instability than patients with posterior (101/139 [72.66%]) or combined instability (83/119 [69.74%]) (P < .0001 overall).
The mean interval between the onset of symptoms and the date of the surgery was significantly greater in patients with anterior instability than with posterior instability (30.43 vs 22.47 months, respectively; P = .043). The mean time to surgery for patients with combined instability was 23.01 months, which was not significantly different from the mean time in patients with anterior or posterior instability (P = .081 and P = .987, respectively) (Table 1).
Table 1.
Patient Characteristics a
| Anterior (n = 158) |
Posterior (n = 139) |
Combined (n = 119) |
X 2 | P | |
|---|---|---|---|---|---|
| Age at surgery, y | 27.9 (18-48) | 30.1 (18-50) | 29.5 (18-50) | N/A | Overall: .0437 Ant vs post: .0421 Ant vs comb: NS Post vs comb: NS |
| Age at injury, y | 25.4 (13.7-47.6) | 28.3 (14-48.7) | 27.6 (10-49.9) | N/A | Overall: .0038 Ant vs post: .0044 Ant vs comb: .0468 Post vs comb: NS |
| Follow-up, mo | 90.71 ± 29.90 | 88.55 ± 24.20 | 90.21 ± 22.49 | N/A | .7635 |
| Male sex | 146 (92.4) | 132 (95) | 116 (97.5) | 3.52 | .1724 |
| Right shoulder affected | 97 (61.4) | 82 (59) | 60 (50.4) | 3.55 | .1698 |
| Dominant arm involved | 102 (64.6) | 90 (64.8) | 63 (52.9) | 4.91 | .0859 |
| History of traumatic event | 129 (81.6) | 95 (68.3) | 73 (61.3) | Overall: 8.64 Ant vs post: 6.36 Ant vs comb: 13.16 Post vs comb: 1.38 |
Overall: .0133 (adjusted alpha = .0167) Ant vs post: Praw, .0117; Pcorrected, .0474 Ant vs comb: Praw, .0003; Pcorrected, .0010 Post vs comb: Praw, .2395; Pcorrected, ≥.9999 |
| Time from symptom onset to surgery, mo | 30.43 (1-240) | 22.47 (1-192) | 23.01 (1-96) | N/A | Overall: .0275 Ant vs post: .0430 Ant vs comb: NS Post vs comb: NS |
| Endorsed pain at presentation | 145 (91.77) | 139 (100) | 119 (100) | Overall: 21.91 Ant vs post: 11.96 Ant vs comb: 10.27 Post vs comb: N/A |
Overall: <.0001 (adjusted alpha = .01667) Ant vs post: Praw, .0003; Pcorrected, .0018 Ant vs comb: Praw, .0008; Pcorrected, .0048 Post vs comb: Praw, .9999; Pcorrected, .9999 |
| Endorsed subjective instability at presentation | 151 (95.57) | 101 (72.66) | 83 (69.74) | Overall: 37.10 Ant vs post: 30.18 Ant vs comb: 34.51 Post vs comb: 0.27 |
Overall: <.0001 (adjusted alpha .01667) Ant vs post: Praw, <.0001; Pcorrected, ≤.001 Ant vs comb: Praw, <.0001; Pcorrected, ≤.001 Post vs comb: Praw, .7056; Pcorrected, .9999 |
Data are expressed as mean (range), mean ± SD, or No. of patients (%). Bold P values indicate statistically significant differences (P < .05). Ant, anterior; Comb, combined; N/A, not applicable; NS, not significant; Post, posterior.
Patients with anterior instability were significantly more likely to be accurately diagnosed on the preoperative physical examination when compared with patients with posterior instability (93% vs 79.1%; P < .001) or combined-type instability (93% vs 75.6%; P < .001). There was no difference in the proportion of patients accurately diagnosed on the physical examination between the posterior and combined instability cohorts (P = .601). Patients with anterior instability were also more likely to have a labral tear detected on the preoperative MRA when compared with patients with posterior instability (82.9% vs 63.3%; P < .001). Also, 86 of 119 (72.3%) patients with combined instability had a labral tear visualized on the MRA, which did not differ significantly from patients with anterior or posterior instability (P = .048 and P = .162, respectively) (Table 2). However, both anterior and posterior tears were detected in only 31 (25.8%) patients with combined instability. In 31 patients (25.8%), only the posterior component of the tear was detected, and in 24 patients (22.7%), only the anterior component of the tear was detected.
Table 2.
Preoperative Clinical and Radiographic Diagnosis a
| Anterior (n = 158) |
Posterior (n = 139) |
Combined (n = 119) |
X 2 | P | |
|---|---|---|---|---|---|
| Clinical diagnosis | 147 (93.04) | 110 (79.14) | 90 (75.63) | Overall: 14.62 Ant vs post: 11.0977 Ant vs comb: 15.2688 Post vs comb: 0.2735 |
Overall: <.0001 (adjusted alpha: .02) Ant vs post: Praw, .0009; Pcorrected, .0052 Ant vs comb: Praw, .0001; Pcorrected, .0006 Post vs comb: Praw, .6010; Pcorrected, ≥.9999 |
| MRA diagnosis | 131 (82.91) | 88 (63.31) | 86 (72.27) | Overall: 17.63 Ant vs post: 13.6773 Ant vs comb: 3.9252 Post vs comb: 1.9536 |
Overall: <.001 (adjusted alpha: .0167) Ant vs post: Praw, .0002; Pcorrected, .0008 Ant vs comb: Praw, .0476; Pcorrected, .1998 Post vs comb: Praw, .1622; Pcorrected, .7547 |
Data are expressed as n (%). Bold P values indicate statistically significant differences (P < .05). Ant, anterior; Comb, combination; MRA, magnetic resonance arthrogram; Post, posterior.
There were no significant differences in rates of concomitant pathology between groups. Long head of the biceps tendon pathology was noted in 23.4% of patients with anterior instability, 35.3% of patients with posterior instability, and 26.9% of patients in the combined instability group (P = .072). Likewise, glenohumeral osteochondral defects were noted in 6.3%, 13.7%, and 10.9% of patients with anterior, posterior, and combined instability, respectively (P = .105). There was no statistically significant difference in concomitant rotator cuff tears between patients with posterior, anterior, or combined instability (12.2%, 7%, and 7.6%, respectively; P = .23) (Table 3). Regarding concomitant procedures performed, a higher proportion of patients with posterior and combined instability underwent subacromial bursectomy (P < .0006). Overall ANOVA indicated that biceps tenodesis was performed at a different rate among the 3 instability subtypes (P = .009) (Table 4); however, individual post hoc comparisons failed to reach significance.
Table 3.
Concomitant Pathologies at Glenohumeral Joint During Arthroscopy a
| Anterior (n = 158) |
Posterior (n = 139) |
Combined (n = 119) |
X 2 | P | |
|---|---|---|---|---|---|
| LHB tendon | 37 (23.4) | 49 (35.3) | 32 (26.9) | 5.27 | .0715 |
| Articular cartilage loss (OCD grade 3) | 10 (6.3) | 19 (13.7) | 13 (10.9) | 4.52 | .1046 |
| Full-thickness rotator cuff tears | 11 (7) | 17 (12.2) | 9 (7.6) | 2.90 | .2349 |
Data are expressed as n (%). LHB, long head of the biceps; OCD, osteochondral defect.
Table 4.
Concomitant Procedures According to Type of Instability a
| Procedure | Anterior (n = 158) |
Posterior (n = 139) |
Combined (n = 119) |
X 2 | P |
|---|---|---|---|---|---|
| Subacromial bursectomy | 69 (43.7) | 98 (70.5) | 87 (73.1) | Overall: 32.57 Ant vs post: 21.63 Ant vs comb: 23.91 Post vs comb: 0.2145 |
Overall: < .00001 (adjusted alpha: .0167) Ant vs post: Praw, <.0001; Pcorrected, <.0006 Ant vs comb: Praw, <.0001; Pcorrected, <.0006 Post vs comb: Praw, .6790; Pcorrected, ≥.9999 |
| Biceps tenodesis | 37 (23.4) | 48 (34.5) | 32 (26.9) | Overall: 9.44 | Overall: .0089 Individual post hoc comparisons: NS |
| Arthroscopic distal clavicle resection | 17 (10.8) | 25 (18) | 11 (9.2) | 5.31 | .0704 |
| Debridement of glenoid OCD | 10 (6.3) | 14 (10.1) | 11 (9.2) | 1.49 | .4739 |
| Debridement of humeral head OCD | 3 (1.9) | 5 (3.6) | 4 (3.4) | 0.90 | .6387 |
| SLAP repair | 23 (14.6) | 20 (14.4) | 23 (19.3) | 0.7731 | .6793 |
| Rotator cuff repair | 11 (7) | 15 (10.8) | 10 (8.4) | 1.3849 | .5003 |
| Rotator cuff debridement | 18 (11.4) | 15 (10.8) | 12 (10.1) | 0.1206 | .9415 |
| Remplissage | 24 (15.2) | N/A | 12 (10.1) | 1.56 | .2109 |
Data are expressed as n (%). Bold P values indicate statistically significant differences (P < .05). Ant, anterior; Comb, combined; N/A, not applicable; NS, not significant; OCD, osteochondral defect; Post, posterior; SLAP, superior labrum anterior and posterior.
Regarding survivorship, there was no significant difference between the 3 groups in the rate of recurrent instability requiring revision at the latest follow-up (5.48%, 3.91%, and 5.50% for anterior, posterior, and combined instability, respectively; P = .797). Additionally, there was no significant difference in the percentage of patients who had been medically discharged from the military at the latest follow-up between the anterior, posterior, and combined instability cohorts (6.85%, 4.69%, and 8.26%, respectively; P = .530) (Table 5).
Table 5.
Survivorship at the Latest Follow-up a
| Anterior (n = 146) |
Posterior (n = 128) |
Combined (n = 109) |
X 2 | P | |
|---|---|---|---|---|---|
| Lost to follow-up | 12 (7.59) | 11 (7.91) | 10 (8.40) | .0608 | .9700 |
| Recurrent instability requiring revision | 8 (5.48) | 5 (3.91) | 6 (5.50) | .4536 | .7971 |
| Medically discharged | 10 (6.85) | 6 (4.69) | 9 (8.26) | 1.2693 | .5391 |
Data are expressed as n (%).
Discussion
Our cohort of 416 active-duty patients with surgically treated shoulder instability demonstrated higher rates of posterior and combined-type instability than previously reported in civilian populations. 18 Additionally, patients with posterior and combined-type instability were less likely to have physical examinations or magnetic resonance imaging (MRI) findings than patients with anterior instability. At the latest follow-up, >90% of patients in all groups were able to remain in the military. No significant differences in the rate of medical discharge or recurrent instability requiring revision were noted between groups.
The findings of this investigation are in line with previous studies, suggesting that young, active-duty military patients are at increased risk for posterior and combined-type instability when compared with civilian populations (Table 6). The incidence of posterior instability has been reported to account for up to 24% of all shoulder instability in military patients.8,11,17,23,24,28 High rates of posterior instability have also been reported among certain high–shoulder demand athletes.11,15,18 This contrasts with the rate of posterior instability in general civilian populations, which is estimated to account for 2% to 10% of surgically treated cases of instability.1,6,10,12,18 This increased rate of posterior and combined-type instability observed in military cohorts may be attributable to the physical demands required by daily training and physical readiness testing, as posterior instability is thought to be most often caused by recurrent microtrauma rather than traumatic instability events.6,18,27 Our findings reflect this, as patients with posterior and combined instability were significantly less likely to report a history of a traumatic event than patients with anterior instability, a trend that has been previously well-documented in the literature.6,18,19 Furthermore, patients with posterior instability were significantly older than those with anterior instability, which aligns with the notion that posterior instability often results from a “wear-and-tear” type mechanism. 18 However, it is also noteworthy that while patients with posterior and combined instability were significantly less likely to report a history of trauma when compared with anterior instability, >60% of patients in both groups did endorse a traumatic etiology, suggesting that military patients may be at higher risk for traumatic posterior instability rather than secondary to a purely degenerative mechanism when compared with civilian cohorts. 18 Interestingly, patients with posterior instability also had a shorter mean time from symptom onset to surgery when compared with patients with anterior instability. It is plausible that posterior instability may lead to greater pain and dysfunction, particularly in military patients who are required to regularly engage in activities that stress the posterior labrum (eg, push-ups and bench press), possibly contributing to the shorter time to surgery observed in this cohort.
Table 6.
Studies Focusing on Characteristics of Shoulder Instability a
| Study | Anterior | Posterior | Combined |
|---|---|---|---|
| In active military populations | |||
| Owens et al 17 (2007) | 94 (80.3) | 12 (10.3) | 11 (9.4) |
| Song et al 23 (2015) | 132 (57.4) | 56 (24.2) | 43 (18.6) |
| Yow et al 28 (2021) | 210 (47) | 80 (18) | 153 (35) |
| Swan et al 24 (2022) | 94 (30.2) | 76 (24.4) | 136 (43.7) |
| Present study | 158 (38) | 139 (33) | 119 (29) |
| In civilian populations | |||
| Blomquist et al 3 (2012) | 336 (83.1) | 40 (9.9) | 28 (6.9) |
Data are expressed as No. of patients or shoulders (%).
Of note, patients with posterior and combined-type instability were less likely to have positive physical examination or MRI findings when compared with patients with anterior instability. These variants of instability have historically been considered more challenging to diagnose when compared with anterior instability.2,13,18 Patients with posterior instability often present with generalized shoulder pain and decreased athletic performance and are less likely to report a subjective feeling of instability or characteristic mechanism of injury.13,18 While the combination of positive Kim and Jerk tests on physical examinations has previously been reported to have a sensitivity of 97% for detecting posterior instability,9,18 only 79.1% of patients with posterior instability and 75.6% of those with combined instability in our study had a clinical examination consistent with their postoperative diagnosis. This contrasts with the 93% of patients with anterior instability who had characteristic findings on physical examination. Patients with posterior and combined-type instability were also significantly less likely to have positive findings on the preoperative MRA. Posterior instability may be caused by multiple different pathologic lesions, and certain variants of posterior labral pathology, such as Kim lesions, are known to be more challenging to diagnose on imaging, possibly contributing to this observed discrepancy. 22 Interestingly, MRA was less reliable than physical examination for all 3 variants of instability. Altogether, these findings suggest that posterior and combined-type instability are common pathologies in military populations that may be more challenging to recognize preoperatively. Our study highlights the importance of maintaining a high index of suspicion when evaluating young, active patients presenting with pain as the predominant symptom causing shoulder dysfunction and suggests that a negative MRA in the setting of a positive physical examination, or vice versa, should not cause orthopaedic surgeons to doubt their diagnosis. Furthermore, these findings call attention to the utility of obtaining a thorough history. Certain key elements in a patient’s history, such as instability events and position of the arm at the time of injury, may help to guide decision making when evaluating patients with an otherwise unclear clinical picture.
Interestingly, there was no statistically significant difference in the number of patients medically discharged between groups, nor was there a difference in the number of patients with recurrent instability requiring revision surgery. Few studies have directly compared postoperative outcomes between anterior and posterior patterns of instability. Bernhardson et al 2 found that while clinical outcomes after arthroscopic stabilization were significantly improved in both groups, outcome scores for anterior instability were statistically superior in all domains when compared with patients with posterior instability. Furthermore, a systematic review by Vopat et al 25 found that patients with anterior shoulder instability were 2.31 times more likely to return to sports than patients with posterior instability. With regard to combined-type instability, Scanaliato et al 20 reported an overall rate of return to active duty of 92.31% at midterm follow-up after 270° labral repair, as well as clinically significant improvements in postoperative patient-reported outcome scores. While our analysis did not include functional outcome scores, >90% of patients in all groups remained in the military at the latest follow-up, suggesting that these patients had regained sufficient shoulder function to meet the basic demands of Army duty. Additionally, few patients in each group required revision instability procedures, with no significant variation noted between each type of instability. This is of interest, as previously reported data suggest that patients with anterior instability are at 1.53 times greater risk of suffering from postoperative instability 25 ; we are not aware, however, of any existing studies that have directly compared reoperation rates between instability patterns.
Limitations
This study is not without limitations. First, the retrospective nature of this study represents a significant limitation. All procedures were performed by multiple orthopaedic surgeons at a single center on a predominantly male cohort of military patients, potentially introducing selection bias and limiting the generalizability of our findings to broader populations. Our investigation was also limited to patients with shoulder instability requiring operative management and, therefore, may not accurately reflect the characteristics of patients with instability not requiring surgical intervention. Furthermore, the physical demands and job requirements of this military cohort make nonoperative management of shoulder instability less favorable, resulting in more patients opting for surgical stabilization. Data regarding how many patients required duty modifications were not available because of the nature of our outcome database, and our analysis did not include clinical outcome scores, limiting our ability to fully evaluate and compare postoperative function. Additionally, it is possible that some patients will go on to require reoperation or medical discharge from the military, as our minimum follow-up period was limited to 2 years. Last, demographic characteristics, including specific military occupation and rank, were not available, nor were the specifics regarding traumatic instability events.
Conclusion
The findings of this study suggest that young, active-duty military patients are at increased risk for isolated posterior and combined-type shoulder instability when compared with civilian patient populations. Additionally, patients with posterior and combined-type instability are less likely to have physical examinations or MRI findings than patients with anterior instability. Orthopaedic surgeons should maintain a high index of suspicion for instability when evaluating and treating young, active military patients who present with shoulder pain, even in the absence of diagnostic preoperative examinations or imaging findings.
Final revision submitted January 18, 2023; accepted January 30, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: J.C.D. has received hospitality payments from Stryker. N.P. has received consulting fees from Mitek. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto. Ethical approval for this study was waived by Carson-Carthage Area Hospital (ref No. 2021-3).
References
- 1.Antoniou J, Duckworth DT, Harryman DT. Capsulolabral augmentation for the management of posteroinferior instability of the shoulder. J Bone Joint Surg Am. 2000;82(9):1220-1230. [DOI] [PubMed] [Google Scholar]
- 2.Bernhardson AS, Murphy CP, Aman ZS, LaPrade RF, Provencher MT. A prospective analysis of patients with anterior versus posterior shoulder instability: a matched cohort examination and surgical outcome analysis of 200 patients. Am J Sports Med. 2019;47(3):682-687. [DOI] [PubMed] [Google Scholar]
- 3.Blomquist J, Solheim E, Liavaag S, Schroder CP, Espehaug B, Havelin LI. Shoulder instability surgery in Norway: the first report from a multicenter register, with 1-year follow-up. Acta Orthop. 2012;83(2):165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bokshan S, Kotchman H, Li L, DeFroda S, Cameron K, Owens B. Incidence of posterior shoulder instability in the United States Military: demographic considerations from a high-risk population. Am J Sports Med. 2021;49(2):340-345. [DOI] [PubMed] [Google Scholar]
- 5.Flint JH, Pickett A, Owens BD, et al. Recurrent shoulder instability in a young, active, military population and its professional implications. Sports Health. 2018;10(1):54-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fronek J, Warren RF, Bowen M. Posterior subluxation of the glenohumeral joint. JBJS. 1989;71(2):205-216. [PubMed] [Google Scholar]
- 7.Galvin JW, Ernat JJ, Waterman BR, Stadecker MJ, Parada SA. The epidemiology and natural history of anterior shoulder instability. Curr Rev Musculoskelet Med. 2017;10(4):411-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Javed S, Gheorghiu D, Torrance E, Monga P, Funk L, Walton M. The incidence of traumatic posterior and combined labral tears in patients undergoing arthroscopic shoulder stabilization. Am J Sports Med. 2019;47(11):2686-2690. [DOI] [PubMed] [Google Scholar]
- 9.Kim SH, Park JS, Jeong WK, Shin SK. The Kim test: a novel test for posteroinferior labral lesion of the shoulder—a comparison to the jerk test. Am J Sports Med. 2005;33(8):1188-1192. [DOI] [PubMed] [Google Scholar]
- 10.Krøner K, Lind T, Jensen J. The epidemiology of shoulder dislocations. Arch Orthop Trauma Surg. 1989;108(5):288-290. [DOI] [PubMed] [Google Scholar]
- 11.Lanzi JT, Chandler PJ, Cameron KL, Bader JM, Owens BD. Epidemiology of posterior glenohumeral instability in a young athletic population. Am J Sports Med. 2017;45(14):3315-3321. [DOI] [PubMed] [Google Scholar]
- 12.Longo UG, Rizzello G, Loppini M, et al. Multidirectional instability of the shoulder: a systematic review. Arthroscopy. 2015;31(12):2431-2443. [DOI] [PubMed] [Google Scholar]
- 13.Millett PJ, Clavert P, Hatch GFR, Warner JJP. Recurrent posterior shoulder instability. J Am Acad Orthop Surg. 2006;14(8):464-476. [DOI] [PubMed] [Google Scholar]
- 14.Owens BD, Agel J, Mountcastle SB, Cameron KL, Nelson BJ. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med. 2009;37(9):1750-1754. [DOI] [PubMed] [Google Scholar]
- 15.Owens BD, Campbell SE, Cameron KL. Risk factors for posterior shoulder instability in young athletes. Am J Sports Med. 2013;41(11):2645-2649. [DOI] [PubMed] [Google Scholar]
- 16.Owens BD, Dawson L, Burks R, Cameron KL. Incidence of shoulder dislocation in the United States military: demographic considerations from a high-risk population. J Bone Joint Surg Am. 2009;91(4):791-796. [DOI] [PubMed] [Google Scholar]
- 17.Owens BD, Duffey ML, Nelson BJ, DeBerardino TM, Taylor DC, Mountcastle SB. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med. 2007;35(7):1168-1173. [DOI] [PubMed] [Google Scholar]
- 18.Provencher MT, Leclere LE, King S, et al. Posterior instability of the shoulder: diagnosis and management. Am J Sports Med. 2011;39(4):874-886. [DOI] [PubMed] [Google Scholar]
- 19.Robinson CM, Aderinto J. Recurrent posterior shoulder instability. J Bone Joint Surg Am. 2005;87(4):883-892. [DOI] [PubMed] [Google Scholar]
- 20.Scanaliato JP, Dunn JC, Fares AB, Czajkowski H, Parnes N. Outcomes of 270° labral repair for combined shoulder instability in active-duty military patients: a retrospective study. Am J Sports Med. 2022;50(2):334-340. [DOI] [PubMed] [Google Scholar]
- 21.Scanaliato JP, Dunn JC, Fitzpatrick KV, Czajkowski H, Parnes N. Double-pulley remplissage in active-duty military population with off-track anterior shoulder instability results in improved outcomes and low recurrence at minimum 4-year follow-up. Arthroscopy. 2022;38(3):743-749. [DOI] [PubMed] [Google Scholar]
- 22.Smark CT, Barlow BT, Vachon TA, Provencher MT. Arthroscopic and magnetic resonance arthrogram features of Kim’s lesion in posterior shoulder instability. Arthroscopy. 2014;30(7):781-784. [DOI] [PubMed] [Google Scholar]
- 23.Song DJ, Cook JB, Krul KP, et al. High frequency of posterior and combined shoulder instability in young active patients. J Shoulder Elbow Surg. 2015;24(2):186-190. [DOI] [PubMed] [Google Scholar]
- 24.Swan ER, Lynch TB, Sheean AJ, Schmitz MR, Dickens JF, Patzkowski JC. High incidence of combined and posterior labral tears in military patients with operative shoulder instability. Am J Sports Med. 2022;50(6):1529-1533. [DOI] [PubMed] [Google Scholar]
- 25.Vopat ML, Coda RG, Giusti NE, et al. Differences in outcomes between anterior and posterior shoulder instability after arthroscopic Bankart repair: a systematic review and meta-analysis. Orthop J Sports Med. 2021;9(5):23259671211006437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Waterman B, Owens BD, Tokish JM. Anterior shoulder instability in the military athlete. Sports Health. 2016;8(6):514-519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wolfe JA, Christensen DL, Mauntel TC, Owens BD, LeClere LE, Dickens JF. A history of shoulder instability in the military: where we have been and what we have learned. Mil Med. 2018;183(5–6):e158-e165. [DOI] [PubMed] [Google Scholar]
- 28.Yow BG, Wade SM, Bedrin MD, Rue JPH, LeClere LE. The incidence of posterior and combined AP shoulder instability treatment with surgical stabilization is higher in an active military population than in the general population: findings from the US Naval Academy. Clin Orthop Relat Res. 2021;479(4):704-708. [DOI] [PMC free article] [PubMed] [Google Scholar]


