Abstract
Sport-related concussion remains an area of high concern for contact sport athletes and their families, as well as for the medical and scientific communities. The National Football League (NFL), along with the NFL Players Association and experts in the field, has developed protocols for the detection and management of sport-related concussions. This article reviews the NFL’s most recent concussion protocol including preseason education and baseline testing for players, concussion surveillance by gameday medical teams and neurotrauma consultants and athletic trainers, gameday concussion protocol and procedures, and return to participation guidelines.
Keywords: football, sports medicine, concussion
Introduction
Sport-related concussion (SRC) continues to attract both media and scientific attention [22]. The burden of SRC, coupled with continued public interest, has led professional sports organizations to develop concussion guidelines and management protocols for the detection and treatment of concussive injuries in their players. The National Football League (NFL), in collaboration with the National Football League Players Association (NFLPA) and under the auspices of the NFL’s Head, Neck and Spine (HN&S) Committee and the NFLPA’s Mackey White Committee, published a concussion protocol in 2013 [26], followed by various revisions [9]. This protocol is reviewed at least annually, and the most up-to-date version is posted on the NFL website [25]. This article reviews the NFL’s current concussion protocol, describes NFL and NFLPA efforts to reduce concussion and manage this injury among NFL players, and offers strategies for concussion detection and management applicable to all levels of play in American football.
The HN&S Committee’s Concussion Protocol
Offseason and Preseason Activities
In the NFL, efforts at concussion mitigation begin in the offseason with player education on (1) the signs and symptoms of concussion, (2) the specifics of the NFL protocol (including education on the roles of various medical personnel involved in the detection and management of concussive injury), and (3) the importance of reporting any indication of concussion, including those observed in other players. Every team’s medical staff performs annual preseason physical examinations on all players, including review of pertinent neurologic issues and details and outcomes of all prior concussions.
A club-designated neuropsychologist consultant (NPC) assists in conducting preseason baseline neurocognitive testing on all players at least once every 3 years. This may consist of a computerized neurocognitive test (eg, the immediate post-concussion assessment and cognitive testing [ImPACT]), specific traditional paper and pencil neurocognitive tests (NFL Paper and Pencil Battery), or a combination of these. Every 2 years, players also undergo baseline testing with the NFL’s Locker Room Comprehensive Concussion Assessment, based on the Sport Concussion Assessment Tool (SCAT) [6]. The SCAT is a standardized evaluation developed by the International Consensus Conference on Concussion in Sport that combines “red flags” (eg, deteriorating level of consciousness, double vision, severe or increasing headache) and observable concussion signs (eg, disorientation or confusion), the Glasgow Coma Scale, Maddocks’ questions (orientation questions specific to sport), a symptom checklist, a cognitive screening, and a neurologic examination (including a cervical spine evaluation, oculomotor testing, pupillary exam, finger-to-nose test, tandem gait, and a standardized balance assessment [modified Balance Error Scoring System]) [6]. All preseason baseline test results are uploaded into a league-wide electronic medical record system.
The Game Day Concussion Surveillance Team
The NFL’s HN&S Committee has made specific efforts to identify players with concussion quickly and accurately at the time of injury and remove them from play to mitigate further injury. Concussion identification in this hyperacute phase is often challenging due to the heterogeneity of presentations, the possibility of delayed symptom onset, a lack of validated biomarkers, under-reporting or lack of awareness of relevant symptoms, and the fact that routine imaging is typically normal [13]. Also, the NFL sideline environment, as in other professional sports, can pose logistical challenges to identifying concussed players: crowded sidelines, rapid speed of play, injuries away from the ball, and player pileups can hinder observations by medical staff. For this reason, it has been important to recruit and train experts at identifying concussive injury behavior and position them strategically on and around the field of play. Even when one of these professionals observes a visible sign of concussion [31], these findings are limited in sensitivity (73% of concussed individuals having any one sign) and specificity (65% of non-concussed individuals having any one sign) [8]. This emphasizes the importance of the rapid synthesis of available data about the player, the mechanism of suspected injury, and the examination findings into an informed return-to-play or remove-from-play decision.
As part of detection and diagnostic efforts, in 2011, the NFL positioned an athletic trainer (AT) spotter in the video booth [17] and added a second spotter the following year. The role of the AT spotter is to identify injuries, some that may have gone undetected by sideline medical staff, and to assist in describing the mechanism of injury and observed injury behavior. Athletic trainer spotters watch the game via an Injury Video Replay System (IVRS), which provides multiple views of each play from cameras positioned throughout the stadium. With the assistance of an IVRS operator, the AT spotter can review plays multiple times, at slower speeds, and from various camera angles. The AT spotter may activate the concussion protocol by alerting team medical staff of observed mechanisms of injury and injury behavior indicative of a possible head or neck injury. Once a potential injury is identified, the game video in which the injury occurred is “tagged” with an electronic label. Sideline medical personnel have dedicated video monitors (and IVRS operators) that are used to review injury video as part of their comprehensive evaluation of the athlete. The tagged injury video is replayed by the IVRS operator for the sideline medical personnel and is also saved for post-game review. Radio communication between AT spotters and sideline medical staff facilitates initiation and completion of evaluations. Athletic trainer spotters also can call a “medical timeout” if they observe that game play is about to continue and a player has yet to receive medical attention. An AT spotter must meet the following criteria: (1) be a certified AT, (2) have a 4-year undergraduate degree, (3) have a minimum of 10 years of athletic training experience, (4) have significant college or professional sports experience, (5) have not been employed by an NFL team for at least 5 years, and (6) cannot cover any games involving a team with which they were previously employed [17].
To augment the expertise of the AT spotter, the Unaffiliated Neurotrauma Consultant (UNC) program was initiated with a pilot program in 2012 to improve injury detection by stationing concussion experts on each sideline [18]. Unaffiliated Neurotrauma Consultants are experts in traumatic brain and spinal cord injury, defined by demonstrated experience with neurotrauma and the following qualifications: (1) board certified or board eligible physician in neurology, neurologic surgery, emergency medicine, physical medicine, and rehabilitation or (2) any primary care Certificate of Added Qualification sports medicine certified. Unaffiliated Neurotrauma Consultants must have documented independence from any NFL team and must be locally credentialed at the American College of Surgeons level I or II trauma center which is specifically designated by the stadium [11]. In 2017, UNCs began to undergo additional NFL-specific training which is now annual. Unaffiliated Neurotrauma Consultants are selected jointly by the NFL and NFLPA and are regularly evaluated with at least annual reviews. Unaffiliated Neurotrauma Consultants assist with identifying mechanisms of injury and injury behavior and are present for every neurologic evaluation conducted during a game. Ultimately, the team physician makes final game day return-to-play decisions [9,25]. Unaffiliated Neurotrauma Consultants, team physicians, team ATs, and AT spotters communicate via radio throughout the game and work in close partnership throughout evaluations. The success of the UNC program has led to the addition of a third UNC who is co-located in the booth with the AT spotters.
Game Day Concussion Protocols and Procedures
Game day begins with a medical huddle 60 minutes before kickoff (the “60-Minute Medical Meeting”) that includes the medical staff from both teams, game officials, UNCs, all medical emergency response personnel including paramedics, ambulance personnel, other medical staff, and the radio communications team. During this meeting, all medical staff are introduced to each other and review their roles and the established emergency action plan including identification of the designated trauma center. Prior to kickoff, 1 UNC is assigned to each team and 1 is assigned to the spotter booth. After the 60-Minute Medical Meeting, UNCs meet individually with the team medical staff they have been assigned to so that any logistical or player-specific concerns can be addressed.
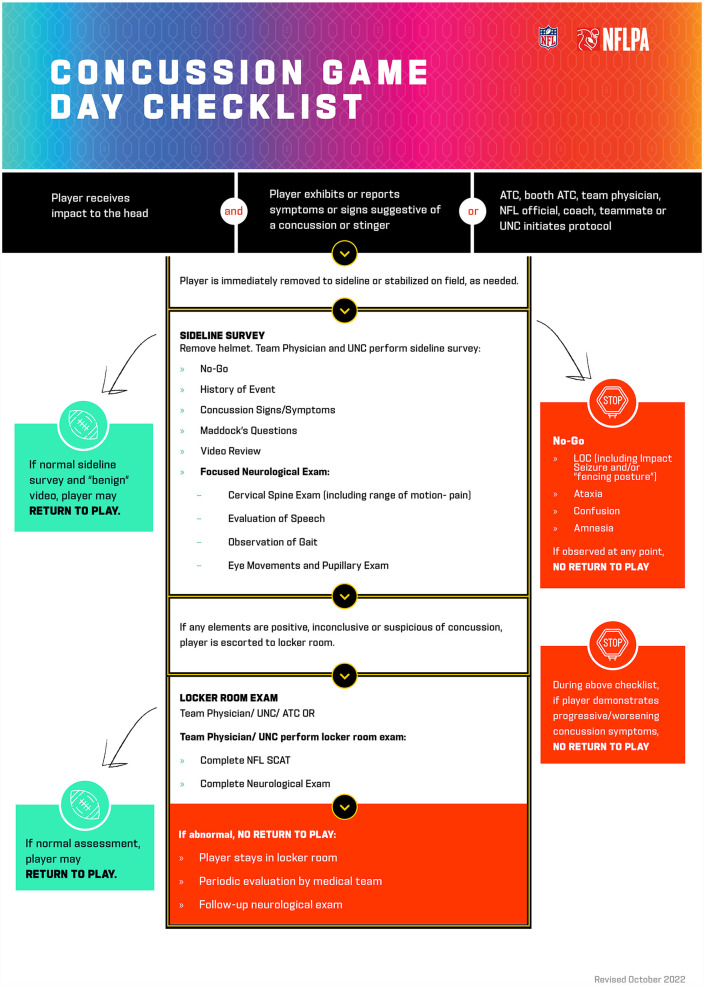
During the game, if a player reports symptoms, exhibits signs, has brachial plexus or cervical root neuropraxia (also referred to as a “stinger” or “burner”), or is identified by others (club ATs, AT spotters, club physicians, coaches, teammates, referees, booth UNC, or sideline UNCs) as having any issue of concern for concussive injury, that player is immediately removed from competition and undergoes evaluation before returning to competition [25]. Medical staff follow the Concussion Game Day Checklist (Fig. 1), a standardized, stepwise examination protocol to aid in medical decision-making. Initial concussion screening is typically conducted in a blue sideline tent allowing for privacy and isolation of the athlete from distractions that could hinder the examination. Upon this initial screening, the event history is reviewed (with video analysis from the booth UNC and AT spotters) for “no-go signs” including loss of consciousness, seizure or posturing, ataxia, confusion, and amnesia. If any of these signs is present, the player is taken to the locker room for more detailed evaluation and is not permitted to return to that game [25].
Fig. 1.
The NFL’s Concussion Game Day Checklist. NFL National Football League, UNC unaffiliated neurotrauma consultant, SCAT Sport Concussion Assessment Tool, ATC Athletic Trainer Certified, LOC loss of consciousness.
In the absence of no-go signs, the checklist is continued and the player is prompted to describe details of the suspected injury and any symptoms. The Maddocks questions, 5 game-specific orientation questions, have been shown to be more sensitive and specific than standard orientation questions [21]. A neurologic examination is performed, with attention to the cervical spine, speech, gait, coordination, balance, eye movements, and pupils. The sideline UNC and team physician also review video of the play using the IVRS cart on each sideline. If the assessment is normal and concussion is not suspected, the team physician may clear the player to return to the game [25].
For suspected concussion or any concerning sign or symptom discovered in the sideline tent evaluation, the athlete is then taken to the locker room for the NFL’s Locker Room Comprehensive Concussion Assessment [9,25]. This assessment involves a more detailed evaluation including the SCAT; the results can be compared with an athlete’s preseason baseline SCAT results. The Madden rule states that any player diagnosed with a concussion must be removed from play, is escorted to and monitored in the locker room, and cannot return to competition on the same day (and not until after medical clearance).
Athletes not diagnosed with concussion and allowed to return to the game are re-evaluated periodically and screened for delayed-onset symptoms. They are reassessed before leaving the stadium and again the following day with, at a minimum, a focused neurologic exam and symptom checklist. If either of these is abnormal, a more thorough evaluation is performed, including the full NFL Locker Room Comprehensive Concussion Assessment.
Return-to-Participation
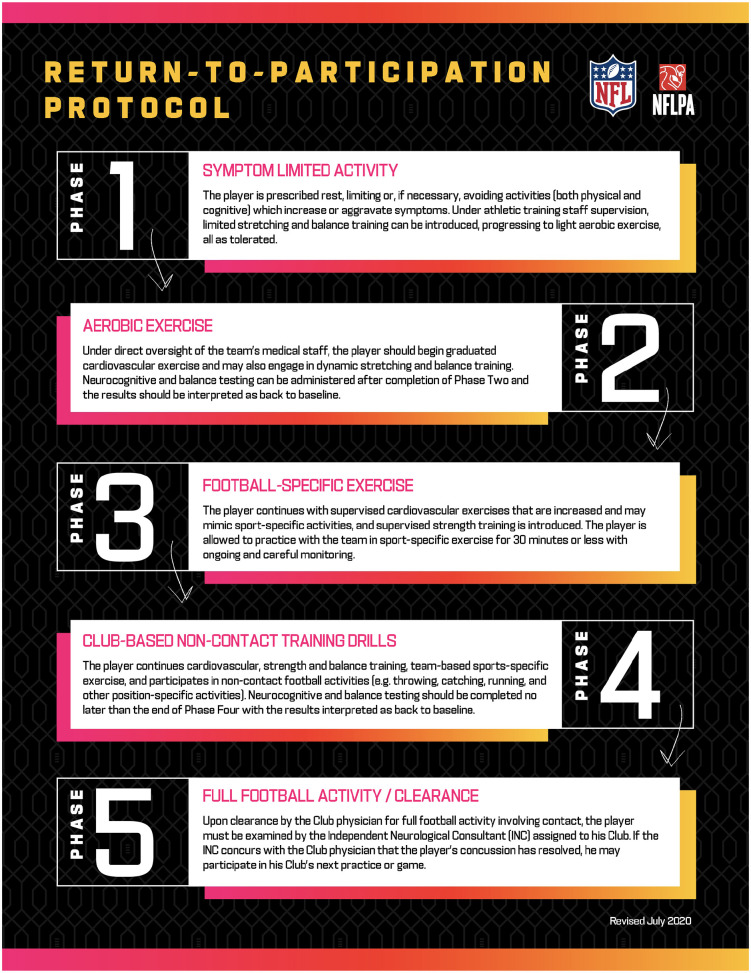
The NFL has a structured 5-phase concussion return-to-participation (RTP) protocol that must be completed in sequential order (Fig. 2). The RTP protocol is based on up-to-date scientific data and recommendations from the Consensus Statement on Concussion in Sport and is reviewed and changed as needed [23] (This article precedes the publication of recommendations from the Sixth International Consensus Conference on Concussion in Sport held in Amsterdam in October 2022. Those recommendations may lead to a review and modification of the NFL protocol.). Throughout the stepwise RTP process, athletes are observed for signs and symptoms of concussion at progressively more intense levels of physical activity. There is no set timeline for RTP in the NFL, and there is no mandate for amounts of time between different phases, allowing players to progress at their own speed. A recent study of concussions in the NFL indicated that the RTP process requires a median of 9 days (a mean of 15 days), a metric that has remained stable over 6 years [19].
Fig. 2.
The NFL’s return-to-participation protocol. NFL National Football League, ATC Athletic Trainer Certified, LOC loss of consciousness.
An athlete is monitored by a medical team member at each step of the RTP protocol. An independent neurologic consultant (INC), a credentialed physician with neurologic expertise, must confirm the team physician’s decision to clear the player from the concussion prior to full RTP. The INC may be consulted as needed to monitor the athlete’s recovery. In addition, the athlete must undergo repeat neurocognitive testing and a face-to-face clinical interview with the Club NPC (no earlier than completion of Phase 2 and no later than Phase 4). Post-injury neurocognitive testing typically includes the NFL paper and pencil battery of neurocognitive tests and computerized ImPACT testing. Athletes must demonstrate a return to their preseason neurocognitive baseline before exposure to football contact activities, unless the club physician determines there is a non–concussion-related cause.
Once the athlete demonstrates the ability to engage in all non-contact football activities without exacerbation of symptoms, the club physician may clear the player for full football activity involving contact in practice. If that is tolerated without signs or symptoms and the club physician concludes the player’s concussion has resolved, he or she may clear the player to return to full participation. Upon clearance by the club physician, the player must be examined by the INC; if the INC confirms the club physician’s conclusion that the player’s concussion has resolved, the player is considered cleared.
Concussion Reduction Efforts in the NFL
The NFL recorded 1302 concussions between 2015 and 2019. There was a statistically significant 23% decrease in game-related concussions between the 2015–2017 seasons and the 2018–2019 seasons [20]. This reduction may be attributed in part to the following factors.
Rule Changes
Within the NFL, concussion risk is the greatest in games [16], during kickoffs and punts [16], while tackling or being tackled [20], and among certain positions (cornerbacks, linemen, and tight ends) [16,20]. These data have led to rule changes targeting higher-risk plays in an effort to reduce the likelihood of concussion. Since 2002, over 50 evidence-based safety-related rule changes have been implemented [27], including alterations in the structure of the kickoff play, elimination of blind-side blocks, use of the helmet during play, and expansion of defenseless player protection.
Equipment Changes
Helmet design has been a focus of improved safety. In 2018, many helmets that were determined to be under-performing in laboratory tests were prohibited from on-field use [2]. These decisions were based on testing performed by biomechanical engineering experts contracted with the NFL and NFLPA. Innovations in helmet design have also led to the availability of position-specific helmets that account for the unique location and speed of head impact for certain positions. A helmet specific to the offensive and defensive line position was introduced for the 2021 season, and a quarterback-specific version has been introduced for the 2023 season. Another initiative involving the use of a soft-shell helmet cover (a version of the Guardian Cap designed specifically for NFL players) was required for certain positions during the 2022 preseason in an effort to reduce the force of head impact for positions with historically higher numbers of concussions [10]. It will be required for additional positions for the 2023 preseason, regular season, and post-season.
Beyond Professional Football: Improving Football Safety at All Levels
Participation in youth, middle school, and high school sports has been shown to have significant health, psychological, and social benefits [7,32], all increasingly important as young people face exceptional mental and physical health challenges [14,15]. As with any activity, it is important to weigh the benefits of sports participation against the risk of potential injury, including concussion. Youth may be at greater risk for concussion and prolonged recovery than professional athletes due to a number of physical, developmental, and health-related factors [30], as well as varied access to trained medical and sideline resources like ATs and physicians. Consequently, effective, low-cost strategies to reduce concussion risk for younger football players are important.
Many of the NFL initiatives used to prevent, identify, and manage concussion can be adapted to younger football players. Education of players, coaches, and parents is an effective low- or no-cost mitigation strategy; basic and no-cost concussion education is available for student-athletes, parents, and coaches through the Centers for Disease Control and Prevention [11]. A recent study indicated that high school students who receive concussion education express increased intentions to report symptoms and demonstrate improved concussion knowledge [4].
Resources available for the public to aid in the identification of concussion include the Concussion Recognition Tool (CRT), which includes a list of red flags that warrant emergency department evaluation, signs and symptoms of concussion, and a brief cognitive exam [5]. The CRT was designed to help guide people without medical training on when an athlete should be removed from play or seek additional care. Continued discussion of the benefits of identification and self-reporting of symptoms among young athletes remains a key factor.
The U.S.A. Football’s Heads Up program aims to refine tackling and blocking techniques and has been shown to result in lower concussion rates by up to 32% [29]. This reinforces the important role that coaches have in injury prevention and suggests that contact training and restrictions are major modifiable factors in concussion prevention among youth and adolescents [28]. The benefits of adopting this at youth levels can carry safe playing styles through high school, collegiate, and professional football.
Similar to rule changes implemented in the NFL, leagues may also consider implementing their own data-driven rule changes to mitigate concussion risk based on their own unique observations and needs. At the league and team levels, decisions to limit or eliminate contact in practice can be considered, as this approach has been shown to decrease concussion incidence in the Ivy League [3].
Widespread recognition of the importance of ATs and the benefit of their active role in player education, injury evaluation, and partnership with physicians in the RTP process could affect concussion recognition and management. Athletic trainers are at the frontline of concussion care in American high schools; however, as many as 34% of secondary schools do not have access to an AT and only 51% of schools have a full-time AT [1]. Athletic trainers positively influence the care of concussed students [24], and finding ways to fund AT access in all secondary schools nationwide is imperative.
Other potentially useful, low-cost strategies include adoption of baseline testing with computerized tests, which can be helpful in RTP decision-making, especially when access to a neuropsychologist is limited. Baseline testing with other sport-specific tools (eg, SCAT) to assist in evaluation also can be helpful.
In summary, nearly all professional sports organizations have taken measures to reduce concussion risk and improve outcomes for their athletes. The NFL has established a comprehensive approach to its concussion program, from prevention through detection, management, and return, which may provide useful strategies for other sporting leagues.
Supplemental Material
Supplemental material, sj-docx-1-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Supplemental material, sj-docx-2-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Supplemental material, sj-docx-3-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Supplemental material, sj-docx-4-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Supplemental material, sj-docx-5-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Supplemental material, sj-docx-6-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Supplemental material, sj-docx-7-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Supplemental material, sj-docx-8-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Supplemental material, sj-pdf-9-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: J.J., MD, and M.H., MD, report no potential conflicts of interest. C.M., PhD, MSPH, and E.B.W, PhD, are full-time employees of IQVIA, which is a paid research consultancy with the National Football League. J.C., MD, R.R., PhD, ATC, and G.S., PhD, are paid consultants to the NFL Player Health and Safety Department. A.S., MD, is a salaried employee of the National Football League. B.V., MD, is a contracted neurotrauma expert for Global Medical Response and a compensated member of the NFL’s Head, Neck and Spine Committee. He is a full-time employee of Eli Lilly and owns stock in the company; however, the content of this article reflects his own work as a subject-matter expert and is not affiliated in any manner with Eli Lilly.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Human/Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent: Informed consent was not required for this review article.
References
- 1.American College of Surgeons. Level I and II TQIP: an overview. Date unknown. Available at: https://www.facs.org/quality-programs/trauma/quality/trauma-quality-improvement-program/level-i-and-ii-tqip/. Accessed May 15, 2023.
- 2.Bailey AM, McMurry TL, Cormier JM, et al. Comparison of laboratory and on-field performance of American Football Helmets. Ann Biomed Eng. 2020;48(11):2531–2541. 10.1007/s10439-020-02627-5. [DOI] [PubMed] [Google Scholar]
- 3.Bretzin AC, Tomczyk CP, Wiebe DJ, Covassin T. Avenues for sport-related concussion prevention in high school football: effect of limiting collision practices. J Athl Train. 2022;57(8):733–740. 10.4085/1062-6050-0341.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daneshvar DH, Yutsis M, Baugh CM, et al. Evaluating the effect of concussion-education programs on intent to report concussion in high school football. J Athl Train. 2021;56(11):1197–1208. 10.4085/509-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Echemendia RJ, Meeuwisse W, McCrory P, et al. The concussion recognition tool 5th edition (CRT5). Br J Sports Med. 2017;51(11):870–871. 10.1136/bjsports-2017-097508. [DOI] [PubMed] [Google Scholar]
- 6.Echemendia RJ, Meeuwisse W, McCrory P, et al. The sport concussion assessment tool 5th edition (SCAT5). Br J Sports Med. 2017;51(11):848–850. 10.1136/bjsports-2017-097506. [DOI] [PubMed] [Google Scholar]
- 7.Eime RM, Young JA, Harvey JT, Charity MJ, Payne WR. A systematic review of the psychological and social benefits of participation in sport for children and adolescents: informing development of a conceptual model of health through sport. Int J Behav Nutr and Phys Activ. 2013;10(1):1–21. 10.1186/1479-5868-10-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Elbin RJ, Zuckerman SL, Sills AK, Crandall JR, Lessley DJ, Solomon GS. Sensitivity and specificity of on-field visible signs of concussion in the National Football League. Neurosurgery. 2020;87(3):530–537. 10.1093/neuros/nyaa072. [DOI] [PubMed] [Google Scholar]
- 9.Ellenbogen RG, Batjer H, Cardenas J, et al. National football league head, neck and spine committee’s concussion diagnosis and management protocol: 2017-18 season. Br J Sports Med. 2018;52(14):894–902. https://doi.org/10.1136.bjsports-2018-099203. [DOI] [PubMed] [Google Scholar]
- 10.Guardian cap debuts at training camps league-wide. https://nflcommunications.com/Pages/GUARDIAN-CAP-DEBUTS-AT-TRAINING-CAMPS-LEAGUE-WIDE.aspx. Published July 29, 2022. Accessed May 15, 2023.
- 11.HEADS UP to Youth Sports. Date unknown. https://www.cdc.gov/headsup/youthsports/training/index.html. Accessed May 15, 2023.
- 12.Huggins RA, Coleman KA, Attanasio SM, et al. Athletic Trainer services in the secondary school setting: the athletic training locations and services project. J Athl Train. 2019;54(11):1129–1139. 10.4085/1062-6050-12-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jindal G, Gadhia RR, Dubey P. Neuroimaging in sports-related concussion. Clin J Sport Med. 2021;40(1):111–121. 10.1016/j.csm.2020.08.004. [DOI] [PubMed] [Google Scholar]
- 14.Jones EA, Mitra AK, Bhuiyan AR. Impact of COVID-19 on mental health in adolescents: a systematic review. Int J Env Res Pub Health. 2021;18(5):2470. 10.3390/ijerph18052470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones SE, Ethier KA, Hertz M, et al. Mental health, suicidality, and connectedness among high school students during the COVID—19 pandemic—adolescent behaviors and experiences survey, United States, January-June 2021. MMWR Suppl. 2022;71(3):16–21. 10.15585/mmwr.su7103a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lessley DJ, Kent RW, Funk JR, et al. Video analysis of reported concussion events in the National Football League during the 2015-2016 and 2016-2017 seasons. Am J Sports Med. 2018;46(14):3502–3510. 10.1177/0363546518804498. [DOI] [PubMed] [Google Scholar]
- 17.Mack C, Myers E, Barnes R, Solomon G, Sills A. Engaging Athletic trainers in concussion detection: overview of the National Football League ATC spotter program, 2011–2017. J Athl Train. 2019;54(8):852–857. 10.4085/1062-6050-181-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mack C, Sendor RR, Solomon G, et al. Enhancing concussion management in the national football league: evolution and initial results of the unaffiliated neurotrauma consultants program, 2012-2017. Neurosurgery. 2020;87(2):312–319. 10.1093/neuros/nyz481. [DOI] [PubMed] [Google Scholar]
- 19.Mack CD, Herzog MM, Solomon G, et al. Return to full participation following concussion in the National Football League, 2015 through 2020. Clin J Sport Med. 2022;32(6):e605–e613. 10.1097/JSM.0000000000001050. [DOI] [PubMed] [Google Scholar]
- 20.Mack CD, Solomon G, Covassin T, Theodore N, Cárdenas J, Sills A. Epidemiology of concussion in the National Football League, 2015-2019. Sports Health. 2021;13(5):423–430. 10.1177/19417381211011446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maddocks DL, Dicker GD, Saling MM. The assessment of orientation following concussion in athletes. Clin J Sport Med. 1995;5(1):32–35. 10.1097/00042752-199501000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Mathieu F, Ellis MJ, Tator CH. Concussion education in Canadian medical schools: a 5 year follow-up survey. BMC Med Educ. 2018;18:1–5. 10.1186/s12909-018-1416-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McCrory P, Meeuwisse W, Dvorak J, et al. Consensus statement on concussion in sport—the 5th international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838–847. 10.1136/bjsports-2017-097699. [DOI] [PubMed] [Google Scholar]
- 24.McGuine TA, Pfaller AY, Post EG, Hetzel SJ, Brooks A, Broglio SP. The influence of athletic trainers on the incidence and management of concussions in high school athletes. J Athl Train. 2018;53(11):1017–1024. 10.4085/1062-6050-209-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.NFL Head, Neck and Spine Committee. Concussion diagnosis and management protocol. Available at: https://static.www.nfl.com/image/upload/v1665264248/league/moexjmdzy2kvjtqsdpbx.pdf. Published October 8, 2022. Accessed May 15, 2023.
- 26.NFL Head, Neck and Spine Committee. Protocols Regarding Diagnosis and Management of Concussion. New York, NY: National Football League; 2013. [Google Scholar]
- 27.NFL health and safety related rules changes since 2002. Available at: https://www.nfl.com/playerhealthandsafety/equipment-and-innovation/rules-changes/nfl-health-and-safety-related-rules-changes-since-2002. Published September 26, 2019. Accessed May 15, 2023.
- 28.Pankow MP, Syrydiuk RA, Kolstad AT, et al. Head games: a systematic review and meta-analysis examining concussion and head impact incidence rates, modifiable risk factors, and prevention strategies in youth tackle football. Sports Med. 2022;52(6):1259–1272. 10.1007/s40279-021-01609-4. [DOI] [PubMed] [Google Scholar]
- 29.Shanley E, Thigpen C, Kissenberth M, et al. Heads up football training decreases concussion rates in high school football players. Clin J Sport Med. 2021;31(2):120–126. 10.1097/jsm.0000000000000711. [DOI] [PubMed] [Google Scholar]
- 30.Van Ierssel J, Osmond M, Hamid J, Sampson M, Zemek R. What is the risk of recurrent concussion in children and adolescents aged 5-18 years? A systematic review and meta-analysis. Br J Sports Med. 2021;55(12):663–669. 10.1136/bjsports-2020-102967. [DOI] [PubMed] [Google Scholar]
- 31.Zuckerman SL, Elbin RJ, Sills AK, et al. Concussions in the National Football League: the evolution of video review for assessing the frequency and reliability of visible signs. Phys Sportsmed. 2020;48(4):424–429. 10.1080/00913847.2020.1731379. [DOI] [PubMed] [Google Scholar]
- 32.Zuckerman SL, Tang AR, Richard KE, et al. The behavioral, psychological, and social impacts of team sports: a systematic review and meta-analysis. Phys Sportsmed. 2021;49(3):246–261. 10.1080/00913847.2020.1850152. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Supplemental material, sj-docx-2-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Supplemental material, sj-docx-3-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Supplemental material, sj-docx-4-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Supplemental material, sj-docx-5-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Supplemental material, sj-docx-6-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Supplemental material, sj-docx-7-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Supplemental material, sj-docx-8-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®
Supplemental material, sj-pdf-9-hss-10.1177_15563316231177207 for The National Football League Concussion Protocol: A Review by Jaclyn Jacobi, Erin B. Wasserman, Christina D. Mack, Morgan Heinzelmann, Javier Cárdenas, Robb Rehberg, Gary Solomon, Allen Sills and Bert Vargas in HSS Journal®