Introduction
Preparticipation physical examination (PPE) is essential to preserve the health and safety of athletes during training and competition. There are numerous benefits to players who participate in competitive athletics, including the aerobic and strength benefits associated with training and competition [4,19]. Given the rigors of American football, the PPE is especially important. Physical and mental demands on players increase as their careers advance, prompting a need for regular examination at all levels.
In recent years, a collaborative effort of professional associations, including the American Medical Society for Sports Medicine (AMSSM), American College of Sports Medicine (ACSM), American Orthopaedic Society for Sports Medicine (AOSSM), American Osteopathic Academy of Sports Medicine (AOASM), American Academy of Pediatrics (AAP), and American Academy of Family Physicians (AAFP), has standardized these evaluations [2]. A primary goal of the PPE is preventing catastrophic events during sport. It is also an opportunity to evaluate the athlete’s general well-being and health status. The PPE should include a review of medical, surgical, social, and family histories, as well as any current medication or supplement use.
An effective PPE depends on timing and setting. For example, when possible, the PPE is performed well in advance of the start of the season to allow time for referrals or additional testing. The PPE is a dedicated appointment, ideally held at the office of a primary care physician [15]. However, at the collegiate level and with sports that have large teams (like football), PPEs are often performed in groups with a coordinated medical team. In this environment, athletes should complete forms detailing their medical history in advance of the appointment. Privacy should be assured for the examination and for discussion of sensitive aspects of the history. The head team physician should be involved with coordinating and planning to ensure the necessary aspects of the PPE are completed [2].
Patient History
Medical History and Medication Use
A thorough review of the medical history should be completed. This can be done on a standardized form before the athlete meets the provider. This assessment should include a review of current medication use, including prescription and over-the-counter medications and dietary supplements. Depending on the level of competition and athletic governing body, certain medications may require the completion of a therapeutic exemption form [11,14]. A review of the athlete’s allergies is also important. Documentation of specific reactions should be completed. It is also crucial that athletes with an anaphylactic allergy understand the importance of and always have access to emergency medication in the event of an allergic condition.
Knowing if an athlete has ever been restricted or disqualified from football participation is important, as this can start a dialogue regarding pertinent medical history. Most athletes with controlled chronic illness can participate in football. For athletes with diabetes, special care should be taken to ensure they understand their insulin and carbohydrate needs around practice and games. Blood-borne pathogens, such as HIV and hepatitis, are not disqualifying conditions for football participation. Given this, routine screening is not indicated, but vaccination against hepatitis B can reduce risk of transmission [26]. The COVID-19 vaccination status should be discussed, and all athletes without a contraindication should be vaccinated against COVID-19. Use of any durable medical device, such as a prosthetic, should also be reported, and regulations by the governing athletic body should be noted.
Cardiovascular History
Personal medical histories surrounding the cardiopulmonary system should focus on exertional symptoms. Inquire about history of exertional chest pain or discomfort, unexplained syncope or near syncope, exertional palpitations, irregular heartbeat, excessive exertional dyspnea or fatigue, heart murmur, or hypertension. Positive findings should be considered in tandem with the physical examination; it is reasonable to restrict athletes from training and play while completing further evaluation. Records of prior testing, such as electrocardiogram (ECG) or echocardiogram, should be obtained and reviewed to avoid repeating evaluations.
Exertional heat illness, including heat stroke, poses substantial risk to football players, especially during the preseason [6]. History of prior heat illness should prompt questioning to determine the circumstances surrounding that event. The equipment required for football also increases the risk of exertional heat stroke. For football players who are new to a warm climate, acclimatization (eg, increasing the athlete’s exposure to heat gradually over a period of days) reduces the risk of heat illness. During the PPE, review the athlete’s hydration and nutrition status and discuss the importance of maintaining both to minimize risk of heat illness. Counseling on hydration is especially important for football players with sickle cell trait. Periods of intense physical exertion in hot and humid conditions can increase the risk of sickling in athletes with this trait, and such acute episodes can be challenging to differentiate from collapse secondary to exertional heat illness. These episodes should be avoided given the increased risk of rhabdomyolysis and sudden cardiac death [25].
Athletes with a history of venous thromboembolism present a unique challenge regarding participation and clearance for football. An individualized approach developed with a hematology consultant can allow for participation in some cases [24].
Neurologic History
A football player’s neurologic history should focus on chronic conditions, such as epilepsy, concussion, and transient brachial plexus injuries, commonly known as stingers. For athletes with seizure disorders, clearance may depend on the type and severity of seizures experienced, as well as how well seizures are controlled [9]. Discussion with the athlete’s managing neurologist, or consultation with a sports neurologist, may be necessary. The number, severity, treatment, and recovery time of concussions should also be documented. Unfortunately, there is a lack of evidence-based recommendations on when to disqualify an athlete from football participation due to prior brain injury. A discussion of the risks of continued participation with the athlete (and in the case of a minor, the parents) is necessary to reach a shared decision on continued participation [27]. The nature of football increases risks of transient brachial plexus injuries; hence, a history of recurrent stingers should be noted. An athlete who reports an episode in which symptoms affected both upper extremities may have sustained cervical cord neurapraxia; this warrants radiographic evaluation of the cervical spine to assess for cervical spinal stenosis [18].
Respiratory History
Current or prior history of respiratory issues, such as asthma or exercise-induced bronchospasm (EIB), should be noted. It is also important to differentiate EIB from exercise-induced laryngeal obstruction, given the similarities in presentation. The severity of any respiratory pathology should be documented, as well as any medications. An asthma action plan should be in place for any athlete with diagnosed asthma [13]. Special care should be taken to ensure access to rescue medications for these athletes.
Gastrointestinal and Genitourinary History
Gastrointestinal and genitourinary issues do not typically limit participation in football, but risks of participation should be discussed with the patient. The history should focus on the presence of any solitary organ, the absence of an organ such as the spleen or a testicle, and the presence of any unusual abdominal bulge or mass. Any chronic condition, such as inflammatory bowel disease, should be noted. Questions on symptoms of a hernia will add to the components of the physical examination. In the case of a symptomatic hernia, referral for repair is indicated. The nutritional status of those participating in football should also be evaluated. Screening for eating disorders, including binge eating disorder and relative energy deficiency, should be considered [7,8].
Dermatologic History
Skin infections are a common indication for restriction from sport participation. Fortunately, most indications for restriction are secondary to readily treatable conditions, thus making these restrictions temporary. Whether the athlete has ever been restricted from participation because of a skin condition or a particular dermatologic condition is recurrent should be noted [22].
Musculoskeletal History
A history of musculoskeletal pathologies is clearly relevant to participation in sport. If an athlete has suffered a bone stress injury, a recurrent musculoskeletal injury, or an overuse injury, it may indicate a nutritional deficiency or metabolic concern. It is also beneficial to know whether an athlete has injured a bone, tendon, ligament, or joint; the nature of treatment for those prior injuries; and whether participation in football was restricted due to the injury. Access to prior imaging studies or treatment notes can help guide counseling on participation in football. Timing of prior injuries and determining the status of recent injuries are important as they pertain to participation clearance [2].
Mental Health History
While special care is taken to evaluate an athlete’s physical well-being, the same level of care should be used in assessing mental health [5]. This can be especially challenging given the social stigma surrounding mental health issues [10]. Screening for conditions such as anxiety, depression, and substance use disorders should be integrated into the PPE. Evaluation of suicidality or prior suicide attempts should be performed as indicated. The PPE may also be an opportunity to educate on the harms of hazing and bullying, as well as to screen for victims of these situations. This is also the time to screen for sexual abuse or misconduct, as well as issues surrounding sexuality and gender identity [6]. Practitioners should be aware of the reporting expectations in their state, as well as the resources that exist in their community, and be ready to help athletes navigate these to provide the support and treatment they need as indicated by findings during the PPE.
Surgical History
It is important to note the type of surgery and dates of any prior surgical procedures. This may help to reveal underlying chronic medical conditions or ongoing medical issues. Following surgery, evaluation and clearance by the team physician and surgical team is necessary before an athlete can return to play.
Family History
Family history can reveal risks that may otherwise be missed in the PPE—for example, if an athlete has a family history of sudden and unexpected premature death, deaths prior to age 50, disability from heart disease prior to age 50, or cardiac conditions known to cause sudden cardiac death. History of such events in family members younger than 35 should raise concern for genetic pathologies, including hypertrophic cardiomyopathy, Marfan syndrome, and long QT syndrome, among others [17].
Social History
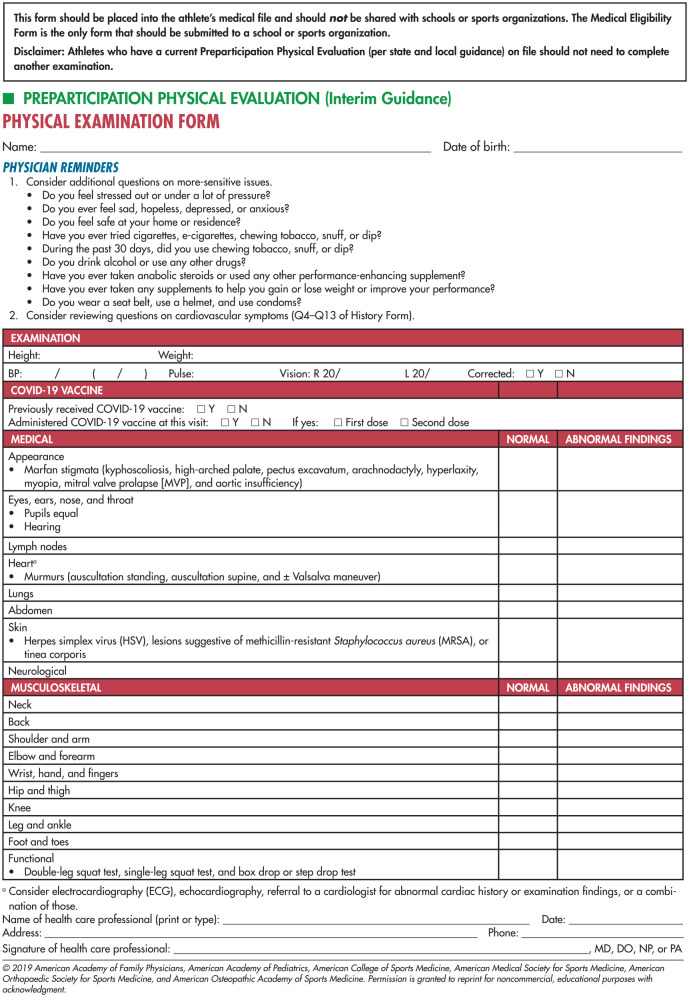
A comprehensive social history is a vital part of a conversation on important but sometimes under-recognized components of health such as substance use, including alcohol, tobacco, cannabis, performance-enhancing drugs, or other illicit substances. Counseling on cessation of unhealthy substance use should be provided, and the individual performing the PPE should have knowledge of resources for treatment options. Reminders of safety guidelines, including wearing a seat belt and safe sexual practices, should be considered as well (Fig. 1).
Fig. 1.
Preparticipation physical evaluation: Physical examination form from American Academy of Family Physicians, American Academy of Pediatrics, American College of Sports Medicine, American Medical Society for Sports Medicine, American Orthopaedic Society for Sports Medicine, and American Osteopathic Academy of Sports Medicine, 2019.
Physical Examination
Cardiac Examination
While each component of the physical examination is important, the cardiovascular system warrants special consideration. Sudden cardiac arrest or death is rare in athletes, but careful consideration may lead to further risk reduction. Blood pressure screening should be a routine part of the PPE. The cardiac examination begins with simple visual observation of the athlete. Suspicion for Marfan syndrome often begins with phenotypical signs such as kyphoscoliosis, high-arched palate, pectus excavatum, arm span greater than height, and arachnodactyly. A scoring system is available to quantify these findings [3]. In addition, checking for joint and skin hyperlaxity is appropriate [16]. Auscultation of the heart at each listening post identifies murmurs. The auscultation should be done supine, standing, and with Valsalva to better identify and categorize any murmurs. The point of maximal impulse should be identified to make sure that it is not lateralized as in the setting of certain cardiomyopathies. Palpation of the femoral and radial pulse should be done to determine whether they are simultaneous. This examination may identify aortic coarctation [1,2].
Reasons to deny participation until further evaluation include the following [2]:
Marfanoid habitus with a score >7
hypertension >140 systolic or >90 diastolic for ages 18 and above or more than 90% age, sex, and height for adolescents
greater than grade 2/6 murmur that radiates laterally, present in middle-late systole, accompanied by a click, louder or changing quality with dynamic maneuvers, holosystolic, or diastolic
family history of sudden cardiac death
Additional cardiac screening consisting of an ECG and/or echocardiogram may be considered to detect conditions that put individuals at risk of cardiac arrest or death. However, the optimal strategy is a matter of debate and depends on the population involved and the resources available. If additional cardiac screening is employed, medical staff should ensure the use of updated athlete-specific criteria to minimize false positive results and costly follow-up testing [21,23].
Neurologic Examination
The nervous system examination should be driven by the patient’s history including concussions, brachial plexus injuries (stingers), single or multiple limb weakness, or headache. A complete neurologic examination includes testing cranial nerves II to XII, deep tendon reflexes, and motor function, sensory function, and cerebellar function. Balance testing may be performed at the time of PPE to evaluate for cerebellar pathology, although this can be subjective unless there is a well-established baseline of the athlete’s balance prior to PPE. Various methods of balance testing are available, although an office-based Balance Error Scoring System (BESS) or modified BESS test is a simple, office-based examination to evaluate balance. Deep tendon reflexes can be performed at the biceps, brachioradialis, triceps, quadriceps, and Achilles tendons; any asymmetry should be noted. If there is a history of recurrent or persistent stingers, an upper limb neural tension test should be performed on the affected side to help evaluate for cervical radiculopathy [1,2].
Reasons to deny participation until further evaluation include the following [2]:
cervical or lumbar radiculopathy
ataxia
altered sensation or motor function
Respiratory Examination
Asthma is one of the most common respiratory problems in athletes. Review the history and medications before physical examination to drive decision-making. With the patient in a seated position, conduct auscultatory examination of the lungs along the anterior and posterior chest. The breath sounds should be equal bilaterally. If adventitious lung sounds such as rales, rhonchi, wheezes, rubs, or coughing with forced expiration are heard, further evaluation is warranted. Visual examination may reveal additional findings such as allergic shiners, nasal polyps, ocular erythema, or pharyngeal cobblestoning that can be suggestive of underlying allergic conditions. In an athlete with a history of exercise-induced asthma, consideration for vocal cord dysfunction can be based on history [1,2].
Reasons to deny participation until further evaluation include the following [2]:
symptomatic or uncontrolled asthma
excessive shortness of breath with activity
Gastrointestinal/Genitourinary
In asymptomatic athletes, the abdominal examination may be of low yield, but it is aimed at identifying abnormalities or sequelae of illness such as splenomegaly after mononucleosis infection. The abdominal examination should be performed with the athlete supine. All 4 quadrants should be palpated and inspected visually. The examination should focus on identifying abdominal masses, rigidity, or a gravid uterus [1,2].
The male genitourinary examination should be completed if indicated based on history, with the use of a chaperone, if necessary. With the athlete standing, the provider looks for testicular asymmetry, undescended testicle, hernia, or testicular masses [1,2].
Reasons to deny participation until further evaluation include the following [2]:
organomegaly
gravid uterus
testicular abnormalities or missing testicle
identification of an abdominal or inguinal hernia
missing a paired organ
Dermatologic Examination
Visual examination of the skin, especially important for exposed areas that may have contact with other players or equipment, is used to identify fungal, bacterial, or other infections. Several contagious skin infections may be identified and should be treated prior to sport participation [22]. This examination can also identify self-inflicted marks that would warrant further mental health discussion and evaluation.
Reasons to deny participation until further evaluation include an active infectious skin condition [2,20].
Musculoskeletal
The musculoskeletal examination can be approached in a general manner or an injury-specific manner. The history has been shown to be 92% sensitive in detecting significant injuries [12]. The general examination may be used to help identify muscle imbalance, range of motion asymmetry, or focal areas of pain. It may include cervical, thoracic, and lumbar range of motion. Gross motor strength can be tested and should be compared side-to-side. Range of motion of the shoulders, elbows, wrists, hips, knees, and ankles can be assessed and compared bilaterally. Functional movement tests can be used to aid in detection of asymmetry. These tests might include a single leg squat or a box drop test. The Beighton score can be calculated for athletes if there is concern for hyperlaxity [16]. If any abnormalities are noted or the individual has a specific complaint, a full examination of the involved joint should be employed. This may need to be done at a later visit [1,2].
Reasons to deny participation until further evaluation include gross abnormalities or asymmetry [1,2].
Conclusion
The PPE is a relatively extensive effort to identify multiple areas of intervention in athletes of all ages and all levels of competition. While it may appear to be time-intensive, this examination can be completed in an efficient and timely manner, especially with practice and a team-based approach. Continued practice and research will aim to improve the PPE and more accurately identify risk factors for morbidity and mortality in this population. This guide may act as a starting point for more detailed examination. For a more in-depth review of PPE recommendations, please consult the collaborative effort mentioned in the introduction of PPE: Preparticipation Physical Evaluation, 5th Ed. [2].
Supplemental Material
Supplemental material, sj-docx-1-hss-10.1177_15563316231174439 for The Preparticipation Physical Examination for American Football Athletes by Matthew Leiszler, Jacob Holtz and Cody Ward in HSS Journal®
Supplemental material, sj-docx-2-hss-10.1177_15563316231174439 for The Preparticipation Physical Examination for American Football Athletes by Matthew Leiszler, Jacob Holtz and Cody Ward in HSS Journal®
Supplemental material, sj-docx-3-hss-10.1177_15563316231174439 for The Preparticipation Physical Examination for American Football Athletes by Matthew Leiszler, Jacob Holtz and Cody Ward in HSS Journal®
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Human/Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent: Informed consent was not required for this technical article.
Required Author Forms: Disclosure forms provided by the authors are available with the online version of this article as supplemental material.
References
- 1.American Academy of Pediatrics. Sports and medical organizations encourage COVID-19 vaccine conversations be part of all sports physicals. August3, 2021. Available at: https://www.aap.org/en/news-room/news-releases/aap/2021/sports-and-medical-organizations-encourage-covid-19-vaccine-conversations-be-part-of-all-sports-physicals. Accessed 21 April, 2023.
- 2.Bernhardt DT, Roberts WO. eds. PPE: Preparticipation Physical Evaluation. 5th ed.Itasca, IL: American Academy of Pediatrics; 2019. [Google Scholar]
- 3.Calculation of Systemic Score. The Marfan Foundation. Updated 2022. Available at: https://marfan.org/dx/score. Accessed November 12, 2022.
- 4.Carbone PS, Smith PJ, Lewis C, LeBlanc C.Promoting the participation of children and adolescents with disabilities in sports, recreation, and physical activity. Pediatrics. 2021;148(6):e2021054664. 10.1542/peds.2021-054664. [DOI] [PubMed] [Google Scholar]
- 5.Chang C, Putukian M, Aerni G, et al. Mental health issues and psychological factors in athletes: detection, management, effect on performance and prevention: American Medical Society for Sports Medicine position statement—executive summary. Br J Sports Med. 2020;54:216–220. [DOI] [PubMed] [Google Scholar]
- 6.Cooper ER, Ferrara MS, Casa DJ, et al. Exertional heat illness in American football players: when is the risk greatest? J Athl Train. 2016;51(8):593–600. 10.4085/1062-6050-51.8.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Souza MJ, Koltun KJ, Williams NI.The role of energy availability in reproductive function in the female athlete triad and extension of its effects to men: an initial working model of a similar syndrome in male athletes. Sports Med. 2019;49(suppl. 2):125–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dakanalis A, Clerici M, Caslini M, et al. Predictors of initiation and persistence of recurrent binge eating and inappropriate weight compensatory behaviors in college men. Int J Eat Disord. 2016;49:581–590. [DOI] [PubMed] [Google Scholar]
- 9.Dubow JS, Kelly JP.Epilepsy in sports and recreation. Sports Med. 2003;33(7):499–516. [DOI] [PubMed] [Google Scholar]
- 10.Egan KP.Supporting mental health and well-being among student-athletes. Clin Sports Med. 2019;38(4):537–544. [DOI] [PubMed] [Google Scholar]
- 11.Gerrard D, Pipe A.Therapeutic use exemptions. Med Sport Sci. 2017;62:55–67. [DOI] [PubMed] [Google Scholar]
- 12.Gomez JE, Lantry BR, Saathoff KN.Current use of adequate preparticipation history forms for heart disease screening of high school athletes. Arch Pediatr Adolesc Med. 1999;153:723–726. [DOI] [PubMed] [Google Scholar]
- 13.Gonzalez A, Mares AV, Espinoza DR.Common pulmonary conditions in sport. Clin Sports Med. 2019;38(4):563–575. [DOI] [PubMed] [Google Scholar]
- 14.Ketterly J.Sports medicine: ergogenic aids. FP Essent. 2022;518:23–28. [PubMed] [Google Scholar]
- 15.MacDonald J, Schaefer M, Stumph J.The preparticipation physical evaluation. Am Fam Physician. 2021;103(9):539–546. [PubMed] [Google Scholar]
- 16.Malek S, Reinhold EJ, Pearce GS.The Beighton score as a measure of generalized joint hypermobility. Rheumatol Int. 2021;41(10):1707–1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maron BJ, Levine BD, Washington RL, et al. ; American Heart Association Electrocardiography and Arrhythmias Committee of Council on Clinical Cardiology, Council on Cardiovascular Disease in Young, Council on Cardiovascular and Stroke Nursing, Council on Functional Genomics and Translational Biology, and American College of Cardiology. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: task force 2—preparticipation screening for cardiovascular disease in competitive athletes: a scientific statement from the American Heart Association and American College of Cardiology. Circulation. 2015;132(22):e267–e272. [DOI] [PubMed] [Google Scholar]
- 18.Miller DJ, Blum AB, Levine WN, Ahmad CS, Popkin CA.Preparticipation evaluation of the young athlete: what an orthopaedic surgeon needs to know. Am J Sports Med. 2016;44(6):1605–1615. [DOI] [PubMed] [Google Scholar]
- 19.Momma H, Kawakami R, Honda T, et al. Muscle-strengthening activities are associated with lower risk and mortality in major non-communicable diseases: a systematic review and meta-analysis of cohort studies. BJSM. 2022;56:755–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Federation of State High School Associations. NFHS medical release form for wrestler to participate with skin lesion(s). Revised April2015. Available at: https://www.nfhs.org/media/869160/2015-16-nfhs-wrestling-skin-lesion-form-april-2015-final.pdf. Accessed November 13, 2022.
- 21.Petek BJ, Drezner JA, Churchill TW.The international criteria for electrocardiogram interpretation in athletes: common pitfalls and future directions. Cardiol Clin. 2023;41(1):35–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peterson AR, Nash E, Anderson BJ.Infectious disease in contact sports. Sports Health. 2019;11(1):47–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sharma S, Drezner JA, Baggish A, et al. International recommendations for electrocardiographic interpretation in athletes. Eur Heart J. 2018;39(16):1466–1480. [DOI] [PubMed] [Google Scholar]
- 24.Swan D, Carter-Brzezinski L, Thachil J.Management of venous thromboembolism in athletes. Blood Rev. 2021;47:100780. [DOI] [PubMed] [Google Scholar]
- 25.Wang H, Martone M, Owens ME, et al. NCAA Division I American football players with sickle cell trait have altered hematological responses and hydration status. Sci Rep. 2021;11(1):1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.World Health Organization. Hepatitis B. Updated June 24, 2022. Available at: https://www.who.int/news-room/fact-sheets/detail/hepatitis-b. Accessed November 11, 2022.
- 27.Wilson JC, Patsimas T, Cohen K, Putukian M.Considerations for athlete retirement after sport-related concussion. Clin Sports Med. 2021;40(1):187–197. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-hss-10.1177_15563316231174439 for The Preparticipation Physical Examination for American Football Athletes by Matthew Leiszler, Jacob Holtz and Cody Ward in HSS Journal®
Supplemental material, sj-docx-2-hss-10.1177_15563316231174439 for The Preparticipation Physical Examination for American Football Athletes by Matthew Leiszler, Jacob Holtz and Cody Ward in HSS Journal®
Supplemental material, sj-docx-3-hss-10.1177_15563316231174439 for The Preparticipation Physical Examination for American Football Athletes by Matthew Leiszler, Jacob Holtz and Cody Ward in HSS Journal®