Summary
Negative symptoms of schizophrenia manifest as reduced motivation and pleasure (MAP) and impaired emotional expressivity (EXP). These can occur as primary phenomena, but have also been suggested to occur secondary to other clinical factors, including antipsychotic-induced sedation. However, this relationship has not been established formally. Here, we examined the effect of antipsychotic-induced sedation (assessed via the proxy of total daily sleep duration) on MAP and EXP in a cohort of 187 clozapine-treated patients with schizophrenia followed for over 2 years on average, using multilevel regression and mediation models. MAP, but not EXP, was adversely influenced by sedation, independently of the severity of psychosis or depression. Moreover, clozapine impaired MAP indirectly by worsening sedation, but after accounting for clozapine-induced sedation, clozapine improved MAP. Our results highlight the importance of addressing sedative side-effects of antipsychotics to improve clinical outcomes.
Keywords: negative symptoms, psychopharmacology, antipsychotic, motivation, apathy
Although ‘negative’ symptoms of schizophrenia play a central role in long-term outcome,1 they remain poorly treated in clinical practice, where treatment is typically centred on minimising ‘positive’ (psychotic) symptoms. Once considered a single construct, recent work has described five distinct negative symptom domains: avolition, asociality, anhedonia, alogia (or poverty of speech) and blunted affect.2 Newer clinical assessment tools have been designed to cover these five principal domains, including the Brief Negative Symptoms Scale (BNSS).3 Latent structure analyses have reduced the five symptom domains into two main clinical factors: (a) impaired motivation and pleasure (MAP), comprising avolition, asociality and anhedonia; and (b) deficits in emotional expressivity (EXP),3 comprising alogia and blunted affect (but see Strauss et al2). Negative symptoms can also be classified as primary and secondary. Primary negative symptoms are intrinsic to schizophrenia, whereas secondary negative symptoms are caused by medication side-effects, psychosis, depression, substance misuse and social deprivation.1 This distinction is relevant clinically, as there is currently no treatment for primary negative symptoms, whereas secondary negative symptoms are potentially treatable.1
Antipsychotic-induced akinesia and sedation are cited as a source of secondary negative symptoms, but there is only weak anecdotal evidence for this association.4 We investigated the longitudinal effect of antipsychotic-induced sedation on negative symptoms in a well-characterised cohort of individuals with schizophrenia treated with clozapine, one of the most sedating antipsychotics.5 Participants were assessed for sedation (assessed using total hours of sleep per day6) and for negative symptoms using the BNSS.3 We addressed three questions: (a) Does sedation influence negative symptoms and, if so, does it affect MAP or EXP? (b) Is the effect independent of other confounders? (c) What is the direct and indirect impact of clozapine on MAP? We hypothesised that drug-induced sedation would specifically impair MAP, even after controlling for other clinical variables.
Method
Study design and participants
This was a naturalistic longitudinal study of clozapine-treated patients attending Cambridgeshire and Peterborough NHS Foundation Trust, UK. The cohort has been well characterised for sociodemographic and clinical information, including the Positive and Negative Syndrome Scale (PANSS) and the Calgary Depression Scale for Schizophrenia (CDSS).7 The cohort has been described in detail elsewhere6 (see Supplementary Methods, available online at http://dx.doi.org/10.1192/bjp.2022.191).
Assessments of sedation and negative symptoms
As a proxy for sedation, we used the total number of hours of sleep per day (overall daytime and night-time sleep). We have previously shown that this measure provides a reliable estimate of antipsychotic-induced sedation.6 As in our previous work, we corroborated the self-reported total number of hours of sleep through additional questions about sleep habits6 (Supplementary Methods).
Negative symptoms were assessed using the 13-item BNSS.3 The ‘Lack of normal distress’ item (item 4) was not considered, as it is not typically included in the analysis of negative symptoms.3 We used the two main clinical factors of MAP (sum of items 1–3 and 5–8) and EXP (sum of items 9–13).3 For readability, we reversed the score for each domain severity so that 6 denoted normal and 0 denoted impaired; consequently, when added up to calculate MAP and EXP severity, increased scores more intuitively reflected improved clinical presentation (more motivation and more emotional expression respectively).
Statistical analyses
The association between sedation and the severity of negative symptoms was assessed using multilevel regression models. We ran two separate models, with MAP and EXP as the dependent variables. A random-effect intercept was fitted for each participant, and the main (fixed slope) variable was sedation. We covaried for age at baseline, gender, positive symptoms, depression, clozapine dose, smoking (categorical variable: yes versus no), number of units of alcohol consumed per week (1 UK unit is 10 ml) and aripiprazole dose. Aripiprazole was included as we have previously shown the independent effect of aripiprazole in reducing sedation6 and because it is the most common augmentation medication in this cohort, and thus could reliably be modelled statistically.
Finally, a multilevel mediation model was used to assess the longitudinal effect of clozapine on motivation, both directly and indirectly via its effect on sedation. We included the same set of covariates as above. Coefficients, their 95% confident intervals (CIs) and P-values were estimated for each path and for the total direct and indirect paths, with a random-effect intercept for each participant.
All statistical analyses were performed using R (version 3.5.0), for Windows, with the ImerTest (version 3.1-2) and Mediation (version 4.5.0) packages.
Results
A total of 187 clozapine-treated individuals were included, with 398 face-to-face assessments (mean follow-up period of 25 months). Clinical and sociodemographic data are shown in Supplementary Tables 1 and 2. All participants had been on clozapine for at least 1 year at baseline assessment.
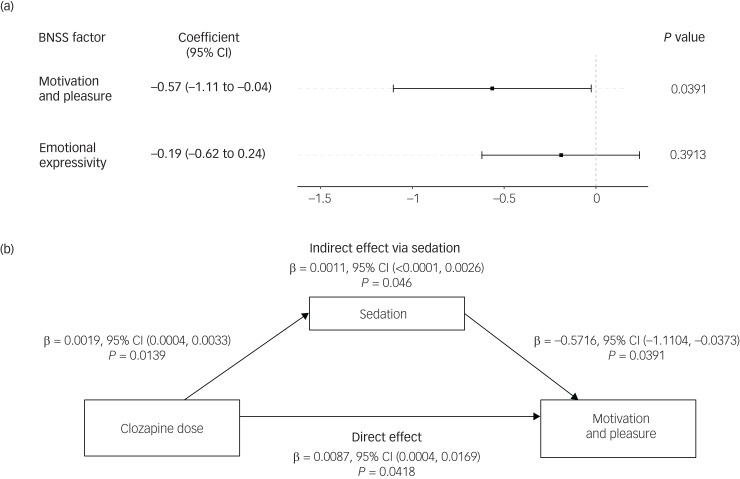
We found a significant association between the level of sedation and MAP longitudinally (β = −0.57, P = 0.039), such that increased sedation levels were linked to reduced MAP levels within participants (Fig. 1(a)). In addition to sedation, the severity of psychosis and depression (other known causes of secondary negative symptoms) were associated with a significant worsening of MAP (Supplementary Table 3). By contrast, there was no such association between sedation levels and EXP (β = −0.19, P = 0.391). For completeness,2 exploratory analyses on the association between sedation levels and each negative symptom domain were conducted (Supplementary Fig. 2).
Fig. 1.
(a) Predictors of individual differences in motivation and pleasure. Results of the linear mixed-effects model estimating the predictors of motivation and pleasure (sum of items 1–3 and 5–8 on the Brief Negative Symptom Scale, BNSS) across the clinical assessments longitudinally. Categorical variables were gender and smoking. (b) The direct effect and indirect effect (via sedation) of clozapine on motivation and pleasure, estimated from a multilevel mediation model. A random intercept was set for each participant. Age, gender, alcohol consumption and aripiprazole dose were included as covariates. For the paths to motivation and pleasure, we also controlled for psychosis (measured via the Positive and Negative Syndrome Scale) and score on the Calgary Depression Scale for Schizophrenia as additional covariates, as these are known causes of secondary negative symptoms.
To explore the specific effect of clozapine-induced sedation on MAP, we performed a longitudinal multilevel mediation analysis (Fig. 1(b)). This allowed us to separate, statistically, the clozapine-related sedation component and test its effect on MAP within participants, while still controlling for other potentially confounding clinical variables. We found a significant effect of clozapine-related sedation on MAP (β = −0.0011, P = 0.046), suggesting that clozapine-related sedation worsened MAP within participants. However, after accounting for the clozapine-related sedation, clozapine improved MAP within participants (β = 0.0087, P = 0.042).
Discussion
We found that sedation (measured through the proxy of total sleep duration) impaired MAP, but did not affect EXP, as measured longitudinally using the BNSS. The effect of sedation on MAP was independent of other sources of secondary negative symptoms, such as psychosis or depression. To our knowledge, our study provides the first data-supported link between sedation and secondary negative symptoms, and specifically MAP. When interpreting our results, the main limitations of our analyses should be considered, namely the use of a single clinical rater and the need for larger samples to ask more specific questions about other clinical modifiers (see Supplementary Discussion).
A major strength of our study comes from the use of longitudinal mediation analysis to measure the direct and indirect effect of an antipsychotic medication on negative symptoms. This method allowed us to explore the direction of the association of clozapine dose with motivation, both through its sedative effect (indirect) and after accounting for clozapine-related sedation (direct) – all while controlling for potential confounders. We found evidence that clozapine directly improves motivation, but this is opposed by the negative (but smaller) effect of clozapine-induced sedation on motivation. This result is consistent with earlier findings suggesting that clozapine improves negative symptoms,8 but there is contradictory evidence in the literature.9 A potential explanation for these mixed results is that previous research did not dissect the different (and opposite) effects of clozapine on sedation and motivation, as we did in this study. These results argue for the optimisation of clozapine dose to minimise secondary negative symptoms when treating psychosis in schizophrenia, so as to improve long-term clinical outcome.
Unlike the effect on MAP, we found no association between sedation and EXP. This distinct effect on a specific negative symptom factor raises the intriguing speculation that there are distinct modulators and thus potential treatments for MAP and EXP deficits in schizophrenia. Such a hypothesis requires future clinical and basic research to assess both MAP and EXP independently and supports the use of these clinical factors to describe negative symptoms10 (see ‘Future directions’ in the Supplementary Discussion).
Our results highlight the deleterious effect of antipsychotic-induced sedation on motivation and call for regular assessment of sedation as a potentially treatable cause of motivation deficits in people with schizophrenia.
Acknowledgements
We thank clozapine clinic patients and carers for their support in this research.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1192/bjp.2022.191.
click here to view supplementary material
Data availability
Data are available from the corresponding author on reasonable request.
Author contributions
N.W., C.J., B.K. and E.F.-E. designed the study. N.W., C.J. and E.F.-E. collected information and prepared the database. N.W., S.C. and R.N.C. conducted or supervised analyses. N.W., S.C., B.K. and E.F.-E. prepared the manuscript. All authors contributed to and approved the final version.
Funding
N.W. was funded by a National Institute for Health and Care Research (NIHR) Academic Clinical Fellowship (ACF-2019-14-013). This research was also supported in part by the NIHR Cambridge Biomedical Research Centre (BRC-1215-20014), the NIHR ARC East of England and, for E.F.-E., the 2018 CPFT Flexibility and Sustainability Award (FSA). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. S.C.'s research was supported by the Medical Research Council (grant MC_PC_17213) and the UK Alzheimer's Society (grant AS-PG-16-006). R.N.C.'s research is supported by the Medical Research Council (grants MC_PC_17213, MR/W014386/1).
Declaration of interest
B.K. receives licensing royalties from ProPhase LLC for use of the Brief Negative Symptom Scale (BNSS) by for-profit groups; these fees are donated to the Brain and Behavior Research Foundation. He has also received honoraria and travel support from ProPhase LLC for training pharmaceutical company raters on the BNSS; consulting fees and/or travel support from Lundbeck, Acadia, ProPhase LLC, Otsuka and Minerva Neurosciences; fees from anonymised investors through Guideposts and Decision Resources Group; and an honorarium from Otsuka for preparation of educational materials. He is part-owner of Quantic Innovations, which provides services related to digital phenotyping of people with psychiatric disorders, with clients including Karuna Therapeutics. R.N.C. consults for Campden Instruments Ltd.
References
- 1.Galderisi S, Mucci A, Buchanan RW, Arango C. Negative symptoms of schizophrenia: new developments and unanswered research questions. Lancet Psychiatry 2018; 5: 664–77. [DOI] [PubMed] [Google Scholar]
- 2.Strauss GP, Ahmed AO, Young JW, Kirkpatrick B. Reconsidering the latent structure of negative symptoms in schizophrenia: a review of evidence supporting the 5 consensus domains. Schizophr Bull 2019; 45: 725–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kirkpatrick B, Strauss GP, Nguyen L, Fischer BA, Daniel DG, Cienfuegos A, et al. The Brief Negative Symptom Scale: psychometric properties. Schizophr Bull 2011; 37: 300–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Putten T, May PRA. “Akinetic depression” in schizophrenia. Arch Gen Psychiatry 1978; 35: 1101–7. [DOI] [PubMed] [Google Scholar]
- 5.Huhn M, Nikolakopoulou A, Schneider-Thoma J, Krause M, Samara M, Peter N, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet 2019; 394: 939–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fernandez-Egea E, Chen S, Jenkins C, Turrion C, Mitchell SP, Dodwell DJF, et al. The effect of clozapine on self-reported duration of sleep and its interaction with 23 other medications: a 5-year naturalistic study. J Clin Psychopharmacol 2021; 41: 534–9. [DOI] [PubMed] [Google Scholar]
- 7.Mortimer AM. Symptom rating scales and outcome in schizophrenia. Br J Psychiatry 2007; 191(suppl 50): s7–14. [DOI] [PubMed] [Google Scholar]
- 8.Rosenheck R, Dunn L, Peszke M, Cramer J, Xu W, Thomas J, et al. Impact of clozapine on negative symptoms and on the deficit syndrome in refractory schizophrenia. Am J Psychiatry 1999; 156: 88–93. [DOI] [PubMed] [Google Scholar]
- 9.Buchanan RW, Breier A, Kirkpatrick B, Ball P, Carpenter WT. Positive and negative symptom response to clozapine in schizophrenic patients with and without the deficit syndrome. Am J Psychiatry 1998; 155: 751–60. [DOI] [PubMed] [Google Scholar]
- 10.Fernandez-Egea E, Wolpe N. Is it time to change the term negative symptoms? Eur Neuropsychopharmacol 2022; 59: 7–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1192/bjp.2022.191.
click here to view supplementary material
Data Availability Statement
Data are available from the corresponding author on reasonable request.