Abstract
Background
Surgical complications contribute to the significant mortality following hip fractures in the elderly. The purpose of this study was to increase our knowledge of surgical complications by evaluating compensation claims following hip fracture surgery in Norway. Further, we investigated whether the size and location of performing institutions would influence surgical complications.
Methods
We collected data from the Norwegian System of Patient Injury Compensation (NPE) and the Norwegian Hip Fracture Register (NHFR) from 2008 to 2018. We classified institutions into 4 categories based on annual procedure volume and geographical location.
Results
90,601 hip fractures were registered in NHFR. NPE received 616 (.7%) claims. Of these, 221 (36%) were accepted, which accounts for .2% of all hip fractures. Men had nearly a doubled risk of ending with a compensation claim compared to women (OR: 1.8, CI, 1.4-2.4, P < .001). Hospital-acquired infection was the most frequent reason for accepted claims (27%). However, claims were rejected if patients had underlying conditions predisposing to infection. Institutions treating fewer than 152 hip fractures (first quartile) annually, had a statistically significant increased risk (OR: 1.9, CI, 1.3-2.8, P = .005) for accepted claims compared to higher volume facilities.
Discussion
The fewer registered claims in our study could be due to the relatively high early mortality and frailty in this patient group, which may decrease the likelihood of filing a complaint. Men could have undetected underlying predisposing conditions that lead to increased risk of complications. Hospital-acquired infection may be the most significant complication following hip fracture surgery in Norway. Lastly, the number of procedures performed annually in an institution influences compensation claims.
Conclusions
Our findings indicate that hospital acquired infections need greater focus following hip fracture surgery, especially in men. Lower volume hospitals may be a risk factor.
Keywords: compensation claims, hip fractures, hip fracture register, Norwegian system of patient injury compensation
Introduction
A hip fracture has a formidable impact on the individual as well as the society. The 1-year mortality rate is between 20-30%, 1 and the total 1-year health and care cost is around €100000. 2 Swift and accurate surgery is of the outmost importance for this frail group of patients. 3
The Norwegian System of Patient Injury Compensation (NPE) is a government bureau that handles compensation claims in the case of presumed patient injury due to a treatment error. Certain criteria are required for a claim to be accepted. First of all, these errors must arise in the course of the treatment or during the follow-up period, and they include incorrect/missed diagnosis, surgical errors or absence of surgery. The particular medical care must be classified as incorrect in accordance with the NPE regulations. The complication must have economical or functional consequences for the patient, formerly set at a medical impairment of minimum 15%. If the claim is not filed within 3 years from the outset of the complication, it will not be considered for compensation (www.npe.no).
Normally, proof of error is not a requisition in the case of postoperative infection. This particular claim will be accepted without an identifiable fault in the line of treatment. In Norway, the complaint can only be filed by the patient, and not by the treating surgeon.
The Norwegian Hip Fracture Register (NHFR) was established in 2005, with aims to monitor the safety of hip fractures, and to provide knowledge on the performance of newly developed methods. 4 Approximately 86% of hip fractures treated with an osteosynthesis and 92% of hip fractures treated with a prosthesis are reported to the NHFR.5,6 There is evidence that low surgical volume increases the risk of readmissions, mortality, and certain complications after hip fracture surgery. 7 Whether this association is also true for injury compensation due to treatment errors has, to our knowledge, not been studied. We aimed to increase our knowledge of surgical complications by investigating compensation claims filed by patients to NPE and identifying the most common reasons for complaints following surgical treatment of hip fractures. Further, we aimed to evaluate if the risk of accepted claims correlate with institutional procedure volume. Finally, as a previous study recently has shown regional variation in the hip fracture treatment in Norway, 8 we aimed to compare compensation claims between the 4 health regions in Norway.
Methods
Patients
All patients who filed a claim to the NPE following hip fracture surgery from 2008-2018 were included. Data on annual volume of hip fracture surgery per institution was collected from the NHFR for the same period.
Methods
The total annual procedure volume in Norway was divided by quartiles. The institutions were placed in their respective quartiles according to their annual volume. The lowest quartile (Q1) consisted of 11 institutions with an annual volume of less than 152 hip fractures. Quartile 2 (Q2) consisted of 15 institutions that performed 152-303 procedures per year. The third quartile (Q3) consisted of 2 institutions with an annual surgical volume of 304-455 hip fractures, and finally, the highest volume quartile (Q4) consisted of 8 institutions that performed 456-606 hip fractures yearly. Further, the institutions were grouped geographically into the 4 administrative health regions of Norway: Northern Norway (NN), Central Norway (CN), Western Norway (WN) and Southern-Eastern Norway (SEN). The claims from NPE were stratified by health region, institution, patient`s age and gender, type of procedure performed (osteosynthesis or arthroplasty), type of complication, and any fatalities. The reason for the claims and the decision made by the NPE (accepted or rejected claims) were recorded. The primary outcome was the proportion of procedures resulting in an accepted claim, with the individual institution as the analysis unit.
Statistics
Mean (SD) or median (range) described continuous variables while categorical data were presented in frequencies. The institutions by procedure volume were compared using ANOVA after asserting conditions were met, and P-values adjusted for multiple testing by Tukey’s comparison test. Associations were quantified by odds ratio (OR) with 95% confidence intervals (CIs). We used omnibus chi-square test to analyse difference in proportions between groups using adjusted standardized residuals to assess which comparisons contributed most for tests with more than 2 groups. A P-value <.05 was deemed statistically significant. The data was analysed using IBM SPSS version 27 (IBM Corp, Armonk, NY, USA).
Results
During the study period (2008-2018), 90,601 hip fractures were reported to the NHFR. The NPE received 616 compensation claims related to hip fracture management, accounting for .7% of all reported hip fractures in the study period. Of these, 221 (36%) were accepted, which accounts for .2% of all hip fractures. In the first half of the study period, 80 claims were accepted, with an increased trend in the second half of the study period with 141 accepted claims. The acceptance rate between men and women who filed a complaint was similar (38% for men and 34% for women, P = .3). However, when considering the total number of procedures performed during the study period, men had nearly a doubled risk of ending with a compensation claim accepted by NPE (OR: 1.8, CI, 1.4-2.4, P < .001) compared to women. There was no age difference between patients with accepted or rejected claims (62 years, range 9-92 and 62 years, range 3-95 respectively) (Table 1).
Table 1.
Demography of Hip Fracture Procedures Reported to the Norwegian Hip Fracture Register and Claims due to Treatment Injuries Following Hip Fracture Procedures filed to the Norwegian System of Patient Injury Compensation during 2008-2018.
| Hip Fracture Procedures Reported to NHFR | Claims Filed to NPE | Accepted Claims | Rejected Claims | |
|---|---|---|---|---|
| Number | 90,601 | 616 (100%) | 221 (36%) | 395 (64%) |
| Age, mean (SD) range | 80 (11) 3-106 |
62 (18) 3-106 |
62 (19) 9-92 |
62 (18) 3-95 |
| Females, n (%) | 62,306 (69) | 352 (57) | 120 (54) | 232 (59) |
| Males, n (%) | 28,295 (31) | 264 (43) | 101 (46) | 163 (41) |
SD, standard deviation; NHFR, Norwegian Hip Fracture Register; NPE, Norwegian System of Patient Injury Compensation.
The most common reason for accepted claims was hospital-acquired infection (59 patients, 27%), followed by failed osteosynthesis (29 patients, 13%) and malreduced fracture (20 patients, 9%) (Table 2). Almost 8% of the accepted claims were due to erroneous rotation of the affected limb. Nine claims were accepted due to delayed reoperation, of which 7 were due to failed osteosynthesis of the femoral neck. Five claims (2%) were accepted due to lack of indication and unnecessary removal of hardware that led to an infection. One accepted claim involved a patient operated on the wrong side. Six claims involved fatalities. Of these, 1 was related to delayed postoperative reinstitution of an oral anticoagulant, 1 was linked to failed osteosynthesis, 3 were due to infection and sepsis, and 1 was associated with lack of post-operative observation leading to suicide. In all 6 cases involving fatalities, NPE granted compensation to the next of kin.
Table 2.
Reasons for Accepted Claims by the Norwegian System of Patient Injury Compensation for Treatment Injuries Following Hip Fracture Procedures During 2008-2018.
| Reasons for Accepted Claims | Osteosynthesis, n (%) | Prosthesis, n (%) | All n (%) |
|---|---|---|---|
| Hospital-acquired infection | 31 (21) | 28 (36) | 59 (27) |
| Failed osteosynthesis | 29 (20) | 0 | 29 (13) |
| Malreduced fracture | 20 (14) | 0 | 20 (9.0) |
| Rotational error | 17 (12) | 1 (1.3) | 18 (8.1) |
| Early prosthesis loosening | 0 | 15 (19) | 15 (6.8) |
| Anisomelia | 7 (4.9) | 8 (10) | 15 (6.8) |
| Malposition of implant | 0 | 10 (13) | 10 (4.5) |
| Lack of follow-up | 8 (5.6) | 2 (2.6) | 10 (4.5) |
| Inadequate supervision | 6 (4.2) | 3 (3.9) | 9 (4.1) |
| Delayed reoperation | 7 (4.9) | 2 (2.6) | 9 (4.1) |
| Pain | 6 (4.2) | 1 (1.3) | 7 (3.2) |
| Nerve injury | 1 (.7) | 4 (5.2) | 5 (2.3) |
| Wrong surgical method | 5 (3.5) | 0 | 5 (2.3) |
| No indication of surgery | 3 (2.1) | 1 (1.3) | 4 (1.8) |
| Abductor deficiency | 0 | 2 (2.6) | 2 (.9) |
| Inadequate medication | 1 (.7) | 0 | 1 (.5) |
| Delayed healing of fracture | 1 (.7) | 0 | 1 (.5) |
| Lack of information | 1 (.7) | 0 | 1 (.5) |
| Incomplete treatment | 1 (.7) | 0 | 1 (.5) |
| Total | 144 (100) | 77 (100) | 221 (100) |
The most common complaint in rejected claims was pain where no treatment error could be identified (134 patients (34%)), followed by failed osteosynthesis for femoral neck fracture in 53 patients (13%) and hospital-acquired infection in 44 patients (11%). Thirty-five patients, nearly 9% of the rejected claims, were due to intraoperative nerve injury leading to a drop foot. No fatalities were recorded among the rejected claims.
Institutional Procedure Volume
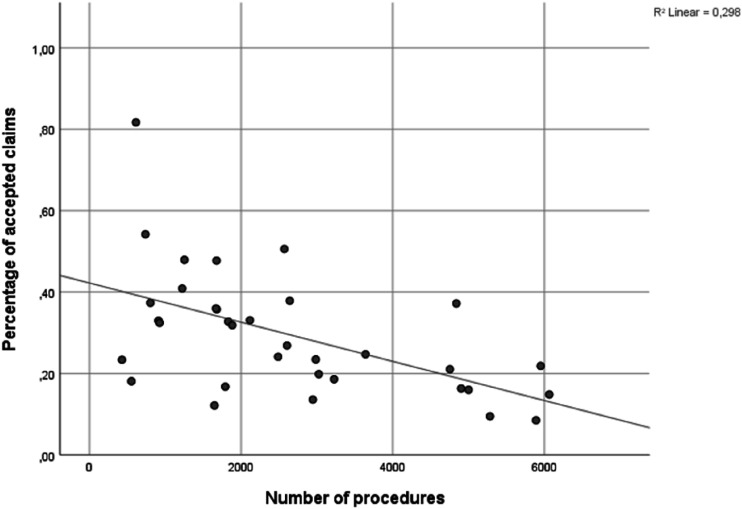
The lowest volume hospitals (<152 hip fractures per year, Q1) had a statistically significant increased risk (OR: 1.9, CI, 1.3-2.8) for accepted claims in proportion of procedures compared to the other quartiles. There was also a statistically significant difference between Q2 and Q4 (OR: 1.6, CI, 1.2-2.2) (Table 3). A negative correlation between hospital procedure volume and proportion of accepted claims was found (P = .001, Spearman r = −.30) (Figure 1).
Table 3.
Risk of Accepted Claims from the Norwegian System of Patient Injury Compensation During 2008-2018 by Annual Procedure Volume Divided by Quartiles into Quartiles.
| Quartiles (Q) | Odds Ratio | 95% CI |
|---|---|---|
| Q1 vs all other | 1.9 | 1.3 to 2.8 |
| Q1 vs Q2 | 1.5 | 1.0 to 2.2 |
| Q1 vs Q3 | 2.0 | 1.1 to 3.7 |
| Q1 vs Q4 | 2.5 | 1.6 to 3.7 |
| Q2 vs Q3 | 1.3 | .8 to 2.3 |
| Q2 vs Q4 | 1.6 | 1.2 to 2.2 |
| Q3 vs Q4 | 1.2 | .7 to 2.1 |
Q1, Quartile 1 (<152 annual procedures); Q2, Quartile 2 (152-303 annual procedures); Q3, Quartile 3 (304-455 annual procedures); Q4, Quartile 4 (>456 annual procedures); CI, Confidence interval.
Figure 1.
Accepted claims stratified by annual institutional procedure volume. Y-axis represents the percentage of accepted claims by total number of surgeries. The P-value for the regression line is .01.
Regional Procedure Volume
No statistically significant difference in accepted claims per procedure volume between the different health regions could be found (P = .1) (Figure 2).
Figure 2.
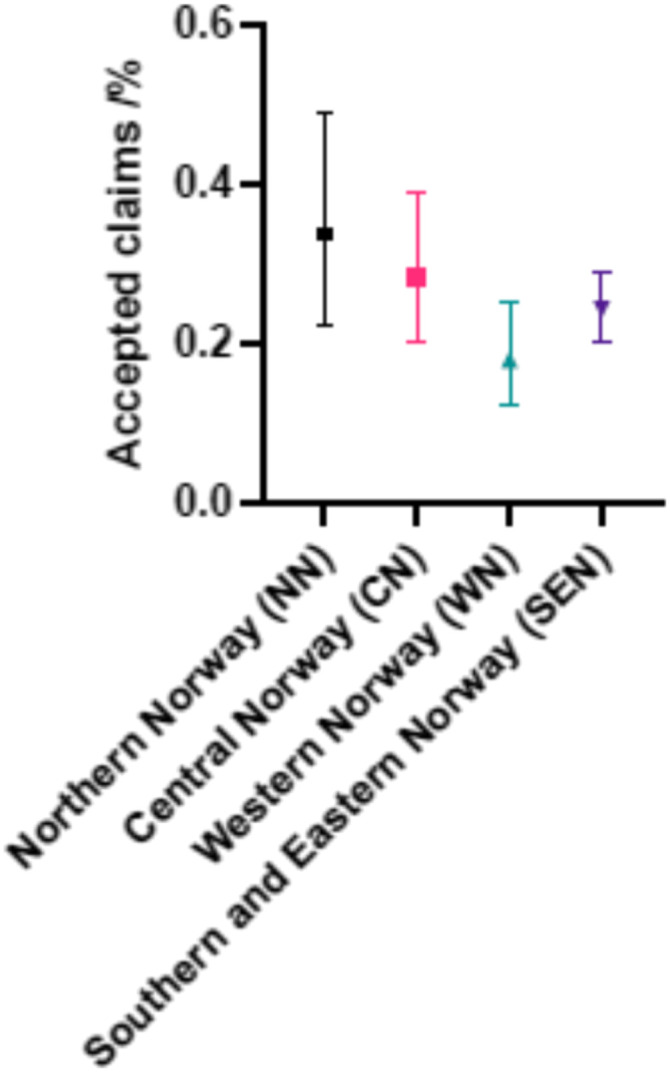
Risk of accepted claims from the Norwegian System of Patient Injury Compensation during 2008-2018 by annual procedure volume divided into administrative health regions. NN (Northern Norway), CN (Central Norway), WN (Western Norway), SEN (Southern Eastern Norway). Omnibus chi-square test of proportions of accepted claim between the 4 health regions was not significant (P = .08).
Discussion
We have several interesting findings that could be relevant for surgical practice. Firstly, we found fewer registered claims in our study compared to similar studies for elective procedures. Secondly, men had nearly a doubled risk of ending with a compensation claim compared to women. Thirdly, hospital-acquired infection was the most frequent reason for accepted claims following hip fracture surgery in Norway. Lastly, institutions with the lowest number of procedures performed annually (fewer than 152 hip fractures) had a higher percentage of accepted compensation claims compared to higher volume facilities. We found no statistically significant difference in accepted claims between the 4 geographical health regions.
According to our findings, only 616 claims out of 90,601 operations for hip fracture were filed between 2008 – 2018 in Norway, accounting for .7%, which is surprisingly low when comparing it to the 1.9% for elective hip arthroplasty. 9 The comparable percentage for UK is approximately .02% for hip fractures, which demonstrates a very different litigious society between Norway and the UK regarding hip fractures. 10 The medical-legal system in the Scandinavian countries are based on the no-blame principle, where the cases are handled outside the legal system and NPE compensates the cost of an injury. Whereas in the UK and the US it is the judicial system that manages the injury compensation through tort liability. 10
Deilkås et al found a significantly higher rate of surgical adverse events in Norwegian hospitals (1.4%) compared to Swedish hospitals (.6%), which can be explained by a more centralized care in Sweden compared to Norway. 11
The relatively high early mortality and frailty (including cognitive impairment) in this patient group may decrease the likelihood of filing a complaint. 12 Patient expectations may also influence the amount of complaints. A relatively healthy elective hip arthroplasty patient will most likely have higher demands to function than an elderly hip fracture patient. NPE accepted 36% of claims representing .2% of all hip fracture surgeries reported to NHFR in the study period. This is a lower percentage than for elective hip arthroplasty (.8%), 9 and knee arthroplasty (.5%). 13 This may be explained by the increased morbidity of patients with hip fractures, making them more prone to complications than healthier patients scheduled for elective arthroplasty. It is likely that NPE deems complications following hip fracture surgery to be caused by the injury itself or the patient’s comorbidity rather than hospital error, and therefore rejects claims more often than after elective surgery.
We found a statistically significant increased possibility for accepted claims in favour of men. Although twice as many women were treated for a hip fracture, the number of accepted claims were similar between the sexes. There may be several reason for this discrepancy. Women could be under-reporting complications or have a higher threshold for submitting a complaint than men. Further, men may possess predisposing conditions leading to increased risk for complications. 14
The main reason for accepted claims was hospital-acquired infection, which is also the dominant reason for accepted claims after elective hip- and knee arthroplasty.9,13 In the database from the National Health Service Litigation Authority (NHSLA) regarding hip fractures in the period from 1995 to 2012, only 9 out of 229 granted claims was due to postoperative infection. 15 In their data, the most common reason for litigation was missed or delayed diagnosis, accounting for roughly 30% of cases. 15 Another study from the UK reviewed the data from the NHSLA in the period from 2005 to 2015, and they also found that the most common reason for litigation was a delay in diagnosis, accounting for nearly 40%. 16 When comparing the NPE to the NHSLA data we may conclude that the main difference in reason for acceptable claim is missed or delayed diagnosis in the UK, while it is infection and failed osteosynthesis in Norway.
The NPE is dependent on designated experts to determine whether a claim is to be accepted or not. This introduces subjectivity in the decision making. Usually, a treatment error must have occurred for a claim to be accepted. However, an exception is made for severe complications, even though no treatment error has been identified. This was true for 59 of the patients with accepted claims. However, 44 patients with hospital-acquired infection had their claims rejected due to underlying conditions predisposing the patients to infection. The patients with accepted claims due to infection were slightly younger than patients with rejected claims (67 and 70 years respectively). NPE rejected compensation claims for infection due to predisposing risk factors more often following hip fracture surgery than after elective hip and knee procedures.9,13
Motor nerve palsy is uncommon following primary total hip arthroplasty, 17 but it is a frequent cause for malpractice claims. 18 In our material, 35 of 40 claims due to drop-foot after implantation of a hemiprosthesis were rejected by NPE, as this complication was regarded as a well-known complication to the surgery, and not a treatment error. Yet, 5 patients were granted compensation due to similar injuries. The reason for this incongruity in accepting or rejecting claims after nerve injury would require a more detailed analysis of each NPE case, which was not available in the dataset. There seems to be an inconsistency among NPE’s experts in when compensation should be granted due to infection and nerve injuries following surgical treatment for hip fractures. A clearer guideline is desirable.
The unfortunate incident with wrong side surgery occurred in 2008. A previous study on NPE cases after anterior cruciate ligament reconstruction found 2 cases of wrong-side surgery. 19 Together this highlights that albeit rare, wrong-side surgery do happen, and vigilance is paramount. In 2012, all hospitals in Norway implemented the use of the safe surgery protocol initiated by the World Health Organization to prevent such errors. 3
We categorized the accepted claims into an osteosynthesis group and an arthroplasty group. Some reasons for accepted claims are not applicable for both groups, such as malposition of implants, malreduced fractures, and failed osteosynthesis. We found approximately equal number of hospital-acquired infections in each group. However, 8 patients were granted compensation due to lack of follow-up after osteosynthesis compared to only 2 patients in the arthroplasty group. Perhaps institutions have better routines for follow-up after arthroplasty, or the risk for treatment error are higher after osteosynthesis. 20
Lastly, institutions with the lowest number of procedures performed annually (fewer than 152 hip fractures) had a higher percentage of accepted compensation claims compared to higher volume facilities. We could not identify regional differences in treatment error that leads to compensation claims after hip fracture surgery.
It is likely that many treatment errors were never reported, especially for very old patients. 21 Dementia will render patients less likely to file complaints. Furthermore, our study only evaluated the effect of institutional volume, not individual surgeon volume, which could influence the results. However, surgery is a teamwork, which could explain why low-volume surgeons in high-volume institutions do well. 22 As such, we believe the institutional volume is relevant to evaluate the effect of surgery volume on compensation claims.
In conclusion, our findings suggest that patients need to be made aware of their rights to compensation, especially in the elderly. Hospital acquired infections need greater focus following hip fracture surgery. The increased complications for men needs further elucidation and lower volume hospitals may be a risk factor.
There are some limitations to our study. Our data is collected from a single country, with a public compensation scheme based on the principle of no blame, which may reduce the generalizability of our study. However, the purpose of this study was to evaluate compensation claims due to treatment errors to identify areas for potential improvement in patient care, which should be of universal interest.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics: The Regional Ethical Committee (REK) judged approval not necessary as all data are based on already anonymized records (REK 15.10.10). The Norwegian Hip Fracture Register is financed by the Western Norway Regional Health Authority.
ORCID iDs
John Magne Hoseth https://orcid.org/0000-0002-1219-1997
Tommy Frøseth Aae https://orcid.org/0000-0003-3643-0822
References
- 1.Morri M, Ambrosi E, Chiari P, et al. One-year mortality after hip fracture surgery and prognostic factors: a prospective cohort study. Sci Rep. 2019;9(1):18718. doi: 10.1038/s41598-019-55196-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hektoen LF, Saltvedt I, Sletvold O, Helbostad JL, Lurås H, Halsteinli V. One-year health and care costs after hip fracture for home-dwelling elderly patients in Norway: results from the Trondheim Hip Fracture Trial. Scand J Publ Health. 2016;44(8):791-798. doi: 10.1177/1403494816674162 [DOI] [PubMed] [Google Scholar]
- 3.Ahlberg J, Pukk-Härenstam K. [Safe surgery saves lives - 10 years of Swedish experience]. Lakartidningen. 2018;115:E7UC. 115Tio år Med WHO:s Checklista För Säker Kirurgi - Säker Kirurgi Räddar Liv – 10 Års Erfarenheter. [PubMed] [Google Scholar]
- 4.Gjertsen JE, Engesaeter LB, Furnes O, et al. The Norwegian hip fracture Register: experiences after the first 2 years and 15,576 reported operations. Acta Orthop. 2008;79(5):583-593. doi: 10.1080/17453670810016588 [DOI] [PubMed] [Google Scholar]
- 5.Kristensen TB, Dybvik E, Kristoffersen M, et al. Cemented or uncemented hemiarthroplasty for femoral neck fracture? Data from the norwegian hip fracture register. Clin Orthop Relat Res. 2020;478(1):90-100. doi: 10.1097/corr.0000000000000826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Furnes OGJ, Hallan G, Visnes H, Gundersen T, Fenstad AM, Dybvik E, et al. Annual Report Norwegian National Advisory Unit on Arthroplasty and Hip Fractures. Bergen: Health Bergen HF; 2021:2021. [Google Scholar]
- 7.Maceroli M, Nikkel LE, Mahmood B, et al. Total hip arthroplasty for femoral neck fractures: improved outcomes with higher hospital volumes. J Orthop Trauma. 2016;30(11):597-604. doi: 10.1097/bot.0000000000000662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kjærvik C, Stensland E, Byhring HS, Gjertsen JE, Dybvik E, Søreide O. Hip fracture treatment in Norway: deviation from evidence-based treatment guidelines: data from the Norwegian Hip Fracture Register, 2014 to 2018. Bone Jt Open. 2020;1(10):644-653. doi: 10.1302/2633-1462.110.Bjo-2020-0124.R1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aae TF, Jakobsen RB, Bukholm IRK, Fenstad AM, Furnes O, Randsborg PH. Compensation claims after hip arthroplasty surgery in Norway 2008-2018. Acta Orthop. 2021;92(3):311-315. doi: 10.1080/17453674.2021.1872901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aae TF, Lian ØB, Årøen A, Engebretsen L, Randsborg PH. Compensation claims after knee cartilage surgery is rare. A registry-based study from Scandinavia from 2010 to 2015. BMC Muscoskel Disord. 2020;21(1):287. doi: 10.1186/s12891-020-03311-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deilkås ET, Bukholm G, Lindstrøm JC, Haugen M. Monitoring adverse events in Norwegian hospitals from 2010 to 2013. BMJ Open. 2015;5(12):e008576. doi: 10.1136/bmjopen-2015-008576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Magnéli M, Unbeck M, Samuelsson B, et al. Only 8% of major preventable adverse events after hip arthroplasty are filed as claims: a Swedish multi-center cohort study on 1,998 patients. Acta orthopaedica. 2020;91(1):20-25. doi: 10.1080/17453674.2019.1677382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Randsborg PH, Aae TF, Bukholm IRK, Fenstad AM, Furnes O, Jakobsen RB. Compensation claims after knee arthroplasty surgery in Norway 2008-2018. Acta Orthop. 2021;92(2):189-193. doi: 10.1080/17453674.2020.1871187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Panula VJ, Alakylä KJ, Venäläinen MS, et al. Risk factors for prosthetic joint infections following total hip arthroplasty based on 33,337 hips in the finnish arthroplasty register from 2014 to 2018. Acta Orthop. 2021;92(6):665-672. doi: 10.1080/17453674.2021.1944529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ring J, Talbot C, Cross C, Hinduja K. NHSLA litigation in hip fractures: lessons learnt from NHSLA data. Injury. 2017;48(8):1853-1857. doi: 10.1016/j.injury.2017.06.009 [DOI] [PubMed] [Google Scholar]
- 16.Fanous R, Sabharwal S, Altaie A, Gupte CM, Reilly P. Hip fracture litigation: a 10-year review of NHS Litigation Authority data and the effect of national guidelines. Ann R Coll Surg Engl. 2017;99(1):17-21. doi: 10.1308/rcsann.2016.0277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Farrell CM, Springer BD, Haidukewych GJ, Morrey BF. Motor nerve palsy following primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87(12):2619-2625. doi: 10.2106/jbjs.C.01564 [DOI] [PubMed] [Google Scholar]
- 18.Patterson DC, Grelsamer RP, Bronson MJ, Moucha CS. Lawsuits after primary and revision total hip arthroplasties: a malpractice claims analysis. J Arthroplasty. 2017;32(10):2958-2962. doi: 10.1016/j.arth.2017.04.044 [DOI] [PubMed] [Google Scholar]
- 19.Randsborg PH, Bukholm IRK, Jakobsen RB. Compensation after treatment for anterior cruciate ligament injuries: a review of compensation claims in Norway from 2005 to 2015. Knee Surg Sports Traumatol Arthrosc. 2018;26(2):628-633. doi: 10.1007/s00167-017-4809-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fang C, Gudushauri P, Wong TM, Lau TW, Pun T, Leung F. Increased fracture collapse after intertrochanteric fractures treated by the dynamic hip screw adversely affects walking ability but not survival. BioMed Res Int. 2016;2016:4175092. doi: 10.1155/2016/4175092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martin A, Vanhegan I, Dean B. Hip hemiarthroplasty for fractured neck of femur; a freedom of information study to assess national variation in implant selection and procurement. Surgeon. 2019;17(6):346-350. doi: 10.1016/j.surge.2018.12.002 [DOI] [PubMed] [Google Scholar]
- 22.Wilson S, Marx RG, Pan TJ, Lyman S. Meaningful thresholds for the volume-outcome relationship in total knee arthroplasty. J Bone Joint Surg Am. 2016;98(20):1683-1690. doi: 10.2106/jbjs.15.01365 [DOI] [PubMed] [Google Scholar]