Abstract
Objectives
Clinical reasoning (CR) is important in health professions, because it ensures patient safety and decreases morbidity. CR should be introduced early in medical school. Health educators play a major role in advocating for the use of CR among students; however, educators themselves can be a barrier to the incorporation of CR; consequently, CR training sessions for educators have been proposed as a potential solution. This scoping review was conducted to highlight studies on CR training among health educators.
Methods
A scoping review was performed to identify studies on CR training sessions for health educators. PubMed, SciVerse Scopus, Web of Science Core Collection, EBSCO Medline Complete and ERIC databases were searched with terms including clinical reasoning, diagnostic reasoning, teacher and trainer, to identify articles published between 1991 and 2021.
Results
The initial search yielded 6587 articles; after careful selection, n = 12 articles were included in this scoping review. Most CR training sessions were in the medical field, were conducted in North America, and involved clinical educators. The sessions focused on the fundamentals and steps of CR; biases and debiasing strategies; and learners' difficulties with various teaching formats, such as didactic presentations, facilitated small group sessions with case discussions, roleplay, and use of tools and a mobile application. Educators and students had positive perceptions regarding the conduct and effectiveness of the training sessions.
Conclusions
These training sessions were rated highly; however, longitudinal feedback regarding the application of learnt CR teaching strategies is necessary.
Keywords: Clinical reasoning, Health educators, Training
المخلص
أهداف البحث
التفكير السريري مهم في المهن الصحية لأنه يضمن سلامة المرضى ويقلل من المعاناة ويجب أن يتم تقديمه مبكرا في كلية الطب. يلعب معلمو الصحة دورا كبيرا في التأكيد على أهمية التفكير السريري للطلاب؛ ومع ذلك، يعتبر المعلمون أنفسهم أحد العوائق في تطبيق التفكير السريري مع جلسات تدريب، وقد اقترحت إحدى الحلول أن يكون ذلك. تم إجراء هذه المراجعة النطاقية للتأكيد على الأدبيات المتعلقة بتدريب معلمي الصحة على التفكير السريري.
طرق البحث
تم إجراء مراجعة نطاقية للبحث عن الأدبيات المتعلقة بجلسات تدريب التفكير السريري لمعلمي الصحة. تم البحث في مواقع مثل بوب ميد، سكوبس، ويب أوف ساينس، إبسكو مدلاين كومبليت وإريك باستخدام مصطلحات البحث التي تشمل التفكير السريري، التفكير التشخيصي، المعلم، والمدرب من عام 1991 حتى عام 2021.
النتائج
أسفر البحث الأولي عن 6,587 مقالا، وبعد اختيار دقيق، تم تضمين 12 مقالا في هذه المراجعة النطاقية. كانت غالبية جلسات تدريب التفكير السريري من مجال الطب، وأجريت في أمريكا الشمالية وشملت معلمين سريريين. ركزت هذه الجلسات على أساسيات التفكير السريري، خطوات التفكير السريري، التحيزات واستراتيجيات التخلص من التحيز، وصعوبات التفكير السريري في المتعلمين باستخدام تنسيقات مختلفة مثل العروض التعليمية، وجلسات المجموعات الصغيرة الميسرة مع مناقشة الحالات، وأدوار اللعب واستخدام الأدوات وتطبيقات الهاتف المحمول. أبدى المعلمون والطلاب تقديرا إيجابيا لهذه الجلسات التدريبية من حيث سيرها وفاعليتها المتوقعة.
الاستنتاجات
على الرغم من تقييم هذه الجلسات التدريبية بشكل عال، إلا أنه يلزم الحصول على ملاحظات طويلة المدى حول تطبيق استراتيجيات تدريس التفكير السريري المكتسبة.
الكلمات المفتاحية: التفكير السريري, معلمو الصحة, التدريب
Introduction
Clinical reasoning (CR) has been shown to be an important process in which a correct diagnosis and treatment plan are obtained after various problem-solving steps. However, CR has many facets, and the current literature contains differing views regarding the definition of CR.1 For the purpose of this scoping review, CR is defined as a skill, process or outcome in which healthcare providers diagnose and treat patients by observing, collecting and interpreting relevant clinical data.2 Five clinical reasoning education domains were defined by Cooper et al. in 20213: CR concepts; history taking and physical examination; choosing and interpreting diagnostic tests; problem identification and management; and shared decision-making.
In CR, thorough history taking, physical examination and investigations are repeated until a sound diagnosis and management plan is made according to patients' complaints.4 CR is of interest to many health educators, because an inability to apply CR in diagnosing a patient's condition may lead to diagnostic error, which has been recognized to cause preventable harm to patients worldwide.5 These errors are due primarily to cognitive failures, such as incorrect synthesis of information from patients' history, physical examination and investigation findings.6
CR is used in day-to-day patient encounters by personnel with experience ranging from novice (e.g., medical students) to expert (e.g., clinical consultants). However, medical students and clinical consultants use differing approaches to CR. According to dual process theory (DPT), non-analytical (type 1) and analytical (type 2) approaches to CR have been widely discussed in studies.7, 8, 9 The type 1 approach to CR is based on intuition or pattern recognition, in which unconscious comparisons are made with past examples and experiences; this approach is widely used by experts or educators.10 In contrast, in the type 2 approach, careful analysis of the relationships among signs and symptoms, and physical examination and laboratory findings is performed to determine a diagnosis.7 The type 2 approach, also known as a hypothetico-deductive approach, is usually used by inexperienced personnel10 and novice medical students. Experts or educators have flexibility to alternate between these approaches until a sound diagnosis is made, particularly for complex cases. However, the relevant cognitive processes occurring in the minds of the educators are not directly communicated to medical students. Unless these processes are verbally explained in detail, medical students will be unable to grasp the cognitive approach used by educators.11 Because medical students are considered novice to the CR process, educators play crucial roles in training students to reason competently and preparing them for the working environment.
In advocating for CR teaching and learning, the barriers to CR must be addressed. Because CR itself is complex and multidimensional, its intrinsic nature has been demonstrated to be a barrier. A lack of knowledge transfer and application from pre-clinical to clinical students, as well as limited opportunities to practice CR, are several identified environmental barriers. In addition educators themselves have been demonstrated to be a barrier, because they may lack awareness of their own CR process and consequently provide insufficient constructive feedback to students.12
Although the medical community agrees on the importance of CR, surveys by Rencic et al. in 201713 and Kononowicz et al. in 202014 have indicated that most respondents' institutions lack a longitudinal CR curriculum and qualified faculty to teach CR. Most educators in medical schools have no formal training in teaching15 and have developed their teaching skills informally through personal experience. In addition to their teaching duties, educators are responsible for patient care, research and administrative work, which account for a large proportion of their schedule.15 Given the multiple roles played by educators and their hectic schedules, introducing CR as a separate training session may be beneficial to help educators better understand CR. For educators to teach CR, they must first understand what CR is, what to teach and how to teach it.
Provision of training sessions imbued with CR concepts and strategies would help educators become more aware of the concepts and educational strategies of CR and implement them in teaching. This scoping review is aimed at highlighting studies on the conduct of educator training session in CR.
Materials and Methods
Methods
In addressing studies on CR training sessions for health educators, we performed a scoping review to identify the type, extent and nature of available evidence. To do so, we referred to the frameworks of Arksey and O'Malley, 200516 and Levac et al., 201017 which consist of the following stages: (1) identification of research questions; (2) identification of relevant studies; (3) study selection; (4) charting of the data; and 5) collation, summarization and reporting of the results.
Identification of research questions
This scoping review was aimed at answering the following main research question: what is the nature of the CR training sessions for undergraduate health profession educators? Several secondary research questions were subsequently identified through team discussion:
-
•
RQ1: Who are the participants in CR training sessions for undergraduate health profession educators?
-
•
RQ2: What are the learning outcomes of CR training sessions for undergraduate health profession educators?
-
•
RQ3: What are the methods and formats of CR training sessions for undergraduate health profession educators?
-
•
RQ4: What is the feedback regarding CR training sessions for undergraduate health profession educators?
In deciding on these research questions, we sought to understand the demographics and background of educators in CR training sessions (RQ1). We also sought to identify the aims and learning outcomes; how training sessions are conducted; which aspects of CR are included; and the educators' feedback regarding these training sessions (RQs 2–4).
Identification of relevant studies
The following electronic databases and search engines were used in May 2022: PubMed, SciVerse Scopus, Web of Science Core Collection and EBSCO Medline Complete and Education Resources Information Center (ERIC). Search terms regarding clinical reasoning and diagnostic reasoning, combined with trainers and teachers were used to search the abstracts, titles and keyword sections of the articles in each database and search engine. The major search strings were as follows: (“clinical reasoning”) OR (“diagnostic reasoning”) AND (“teach∗”) AND (“train∗”; Appendix A). The reference list of selected studies was also searched to identify any potential related references.
Study selection
The database searching was performed according to the following set of predetermined inclusion and exclusion criteria:
-
(1)
Articles published between 1st January 1991 and 31st December 2021
-
(2)
Original articles in peer-reviewed journals
-
(3)
Full-text articles in the English language
-
(4)
Original articles on conducting CR training session for educators.
The starting year of 1991 was chosen because studies using a clinical presentation-based curricular model, according to the principle of encouraging students to engage in schema and inductive reasoning, began to be published that year.18 The search results from the databases were exported to the EndNote 20 bibliographic manager for compilation. Duplicate citations were removed, and the remaining citations' titles and abstracts were screened for their relevance according to the predetermined inclusion criteria and relevant keywords (clinical reasoning/diagnostic reasoning/teacher/trainer). The full text of the remaining articles was then examined, and the chosen articles were compiled for a data extraction process. Any discrepancies in the selection of articles were resolved by discussion between authors.
Charting the data
We created an Excel file in which the related information from the selected articles was charted. The file contained variables such as general information (date of publication, authors and authors' institutions) and information on the CR training sessions for educators (learning objectives, participants, duration, content, format and other aspects). The first author conducted the initial analysis identifying the necessary variables from the selected studies, and input them into the Excel file, which was then reviewed by the second author. Any discrepancies were resolved via discussion between the authors.
Collation, summarization and reporting of the results
The Excel spreadsheets were compiled, and the extracted data were summarized according to the identified research questions, and are reported in the results section. The data were categorized according to the year of publication; country of origin of the research; participants; learning outcomes; and training session conduct, content and feedback. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews (PRISMA-ScR guidelines) were followed for reporting results in this scoping review.
Results
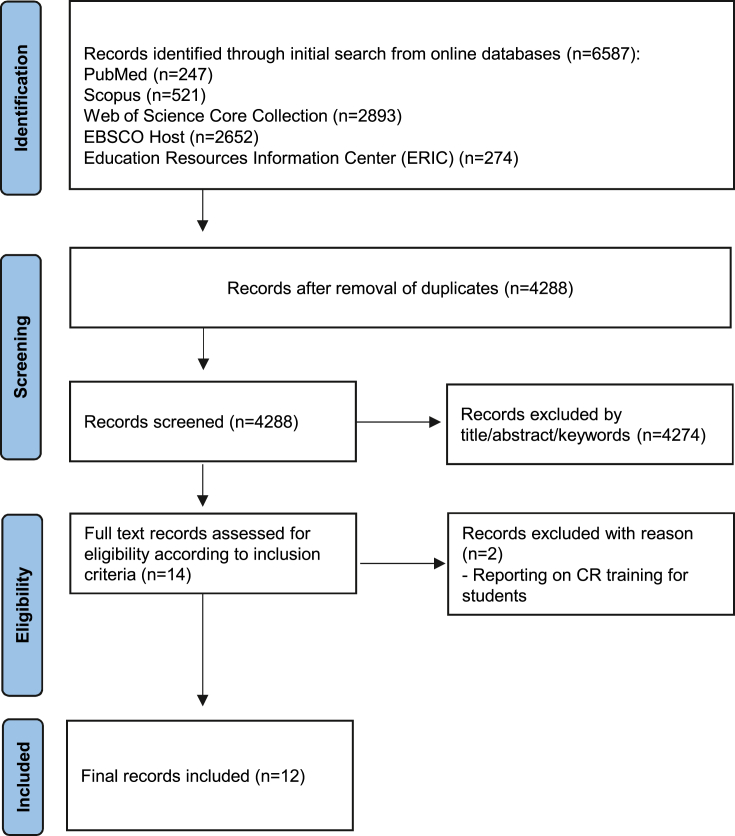
The literature search in online databases yielded 6587 potentially relevant articles. After removal of duplicates; screening of titles and abstracts; and reading through these articles, we identified only 12 articles meeting all inclusion criteria, which were included in this scoping review (Figure 1).
Figure 1.
Flowchart of the article selection process.
Characteristics of the CR training sessions for undergraduate health profession educators (RQ1)
From the selected articles, the first two reported CR training sessions for undergraduate health profession educators were published in 2011; subsequently, ten articles were published between 2013 and 2021. Researchers from North America (United States and Canada) published most the articles (75%, n = 9), and researchers from Australia, Taiwan and South Africa published one article each. Most articles (75%, n = 9) were in the field of medicine, and the remainder were from nursing and other health professions (physical therapy, occupational therapy, audiology, and speech and language therapy; Table 1). Most training sessions (91.6%, n = 11) were designed and developed for educators teaching students in the clinical years, whereas only one training session was designed and developed for educators teaching students in the clinical and pre-clinical years.
Table 1.
Number of articles reporting on CR training sessions for educators, according to health professionals' fields.
| Health professionals' field | Number of articles reporting on CR training sessions |
|---|---|
| Medicine | 9 |
| Nursing | 1 |
| Other (physical therapy, occupational therapy, audiology and speech and language therapy) | 2 |
CR training session for undergraduate health profession educators—objectives, content, format and feedback (RQs 2, 3 and 4)
Training session types and learning outcomes
The CR training sessions for the undergraduate healthcare profession were categorized into sessions to train and guide educators regarding the domains of CR education,19, 20, 21, 22, 23, 24, 25, 26, 27 and sessions to guide educators in how to use a newly developed tool28,29 or mobile application30 to facilitate CR education. These sessions were conducted either as stand-alone sessions21, 22, 23, 24, 25, 26, 27, 28, 29, 30 or as an independent topic in a series of faculty development programs.19,20 These training sessions had similar aims of guiding and training educators in CR to empower them in their teaching. Specifically, these training sessions were aimed at providing guidance in the cognitive steps and CR framework21,22,25, 26, 27; diagnostic error and bias24; and identification of learners with CR difficulties.23,30
Content
For educators to be able to discuss and gain a uniform understanding of CR, these training sessions used terminology commonly described in CR studies. The content of the training sessions reported in this scoping review included cognitive theories in CR; steps or cognitive process in CR; educational strategies in applying steps in CR; cognitive errors and bias in CR; and CR problems among learners. For training sessions on the use of specifically developed tools or a mobile application, beyond the introduction of cognitive theory in CR, the entire session was dedicated to hands-on practice.
The main cognitive theory discussed was DPT,20,22, 23, 24,27 and the features of system 1 (pattern recognition) and system 2 (hypothetico-deductive), and the instances in which each approach should be used, were highlighted. In addition, Addy et al., 201622 have discussed use of a modified Bayesian approach in CR.
Problem identification25 and related data collection21 were among the initial steps in CR that were a focus in the training sessions. The educators were subsequently introduced to the concept of problem representation,21,26,29 i.e., a detailed summary of relevant clinical information. Educators were encouraged to use semantic qualifiers—i.e., opposing clinical terms, such as acute and chronic, or unilateral and bilateral—in the problem representation. The educators learnt about illness scripts,21,26,29 which synthesize knowledge regarding the pathophysiology of a particular disease and its signs and symptoms. The educators then compared and contrasted these illness scripts or differential diagnoses to achieve a sound diagnosis.
Another important CR concept introduced to the educators was cognitive errors or biases,23,24 including the importance of recognizing these biases and applying debiasing strategies. Domains of CR difficulty in learners, and strategies to overcome these difficulties, were the main focus of the training sessions conducted by Weinstein et al. in 2017.23
Format
All training sessions were conducted face-to-face, and incorporated both passive and active learning methods.19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30 In some training sessions,22,24 materials such as handouts, notes, PowerPoint presentation slides and trigger videos were shared with the educators before the start of the session. The educators were encouraged to refer to these materials during the training session, to aid in their understanding. During the training sessions, interactive lectures were conducted in large groups, and facilitated small group discussions (SGDs) discussions were subsequently conducted. In the SGDs, educators applied the CR concepts learnt from cases based on real scenarios in healthcare settings, in either print or video format. The cases used in these sessions were not specialty-specific, thus allowing the cases to be used by other specialties. Some sessions also used roleplay, to give the educators the opportunity to be both student and teacher. Large group debriefing and reflection sessions were usually conducted afterwards, to summarize the main messages with the educators. The training sessions usually ended with feedback sessions by the educators. In some training sessions,22,25,26 the educators conducted their own teaching sessions with students, by applying the CR strategies learnt. The students were then asked to share their feedback on the educators' teaching, in view of application of CR strategies.
For training sessions on the use of specifically designed tools28,29 and a mobile application,30 large group interactive sessions were held to introduce the tools and the application, which were followed by hands-on practice aided by trained facilitators.
Feedback
The feedback on the CR training sessions was divided into (1) educators' feedback regarding the manner in which the training was conducted, (2) educators' feedback on the effectiveness of the training, and (3) students' viewpoints regarding the effectiveness of the training sessions in terms of the educators' teaching. Some feedback was obtained before the training sessions,20,22,24,25,29 as part of a pre- and post-training session feedback comparison; however, most feedback was obtained at the end of the training sessions. In addition, some training sessions19,22,26 conducted feedback sessions 2 months to 1 year after the initial training sessions. Anonymous quantitative and qualitative questionnaires, were widely used, and were followed by face-to-face interviews and commitment to change statements.
Regarding the conduct of the training sessions, educators gave high ratings or scores regarding the supplementary materials provided,19,22,24,29 the quality and organization of the training sessions,21,22,29 the facilitation skill of the instructor or facilitator,20,22,23,29 and the active and interactive formats of the small group sessions.19, 20, 21,23,24 Educators perceived that the objectives of these training sessions were met19,22, 23, 24 and that they had gained confidence in applying CR strategies, such as the use of problem representation and illness scripts, in their subsequent teaching sessions.19,23,26,29 Most educators also reported that they were able to implement these CR strategies 2 months26 and 1 year19 after the completion of the training sessions. However, the educators were not comfortable in applying modified Bayesian techniques, such as establishing pre-test probabilities, 11 months after the completion of the training sessions.22
Feedback was also obtained from students involved in the training sessions. Simulated students reported that educators significantly improved in the use of problem representation26 between the pre and the post training sessions. Students also perceived more effective development of their CR skills after attending teaching sessions held by educators who had attended training on a modified Bayesian approach.22 Nursing students gave significantly higher teaching ability ratings to the educators who had attended the training sessions.25
The objectives, content, format and feedback of the CR training session for educators are summarized in Table 2.
Table 2.
Objectives, content, format and feedback regarding CR training sessions for educators.
| Author, year | Participants | Type of training | Duration | Objectives/aims | Content | Format | Feedback |
|---|---|---|---|---|---|---|---|
| Pien et al., 201116 | Clinical educators | Combination with other modules; each module run independently | 90 min | To develop, distribute and evaluate an adaptable resident educator and life-long learner curriculum using a train-the-trainer approach—general aim | No description of what is taught in the CR module |
|
|
| Atkinson & Nixon-Cave, 201117 | Physical therapy educators | Standalone | Not stated | To guide faculty members on the use of a tool developed on the basis of an ICF framework for reflection and mentoring | General concepts of mentorship; tool introduced as a mentoring guide | Workshop led by experienced clinicians and other mentors; no other information | Generally positive feedback: hypothesis component helped in reflection, improved prognostic indicators and recognition of biases, and guided mentoring |
| Dhaliwal, 201318 | Clinical educators | Standalone | 120 min | To teach front-line teachers to teach and understand cognitive steps in CR | Simplification of CR processes (data collection, problem representation, illness script content, and illness script comparison and selection) by technological analogies when looking for information online |
|
Post workshop evaluation data comparing this workshop with other faculty development programs in the same academic year High ratings in quality and organization of the session, and intention to change practice |
| Foster & Laurent, 201319 | Clinical educators | Combination with other modules; each module run independently | 90 min | To teach effective teaching relevant to working clinical teachers | Hypothetico-deductive process; CR theater approach to develop CR; emphasis on how to engage students in interpreting clinical information rather than recalling |
|
|
| Addy et al., 201620 | Clinical and pre-clinical educators | Standalone | 90 min | To teach CR using a modified Bayesian approach |
|
|
|
| Weinstein et al., 201721 | Clinical educators | Standalone | 90 min | To train clinical teachers to deconstruct CR problems in learners |
|
|
|
| Daniel et al., 201722 | Clinical educators | Standalone | 60 min | To train faculty educators on transferring concepts of bias and debiasing strategies in clinical practice |
|
|
Retrospective survey rating abilities before and after the session: significant improvements in self-reported perceptions of recognizing bias and applying debiasing strategies |
| Liao et al., 201923 | Nursing educators | Standalone | 480 min | To provide CR teaching skills to nursing educators |
|
|
|
| Schaye et al., 201924 | Clinical educators | Combination with other modules; each module run independently | 180 min | To teach the CR framework grounded in CR theory |
|
|
|
| Boileau et al., 201925 | Clinical educators | No elaborate training given to participants in how to use the mobile application | None | To test a mobile application developed for clinical teachers, to verify and describe CR difficulties in learners | Mobile application content based on a reference guide on domains of CR difficulties in learners |
|
Semi-structured interview before and after the trial period of the mobile app: the mobile app was concise, specific and easy to use, and helped clarify learners' CR difficulties, and facilitate learning and translation into practice |
| Cohen et al., 202026 | Clinical educators | Standalone | 60 or 120 min | To develop faculty skills in teaching diagnostic reasoning by using a theory-informed assessment tool, the Assessment of Reasoning Tool (ART) |
|
|
Post workshop evaluation: favorable ratings for facilitators and workshop; most noted that they would change their practice; ART itself was useful, but educators require additional information on how to apply ART in their educational setting |
| Talberg et al., 202127 | Physical therapy, occupational therapy, audiology and speech and language therapy educators | Standalone | Not stated | To train clinical educators in CR |
|
|
|
Discussion
RQ1: Who are the participants in CR training sessions for undergraduate health profession educators?
From the selected articles, the reporting on CR training sessions for educators started in 2011, and articles were published almost yearly thereafter until 2021. The steady numbers of training sessions might be considered to indicate increased awareness and better insight into the importance of educators updating their knowledge and improving their skills. These aligned well with the findings of the systematic review of Best Evidence Medical Education (BEME) on faculty development initiatives,31 which have indicated an increase in the number of faculty development programs over time. Diagnostic error has been identified as a critical area in healthcare, and a report from the National Academies of Sciences and Medicine in the United States32 has suggested that healthcare professional education and training in CR might provide a possible solution. Subsequently, researchers from North America embarked on CR training sessions, as evidenced by the high number of research contributions in this area identified in this scoping review. However, the lack of awareness of own CR33 may hinder researchers in other parts of the world in organizing such training sessions.
CR has been recommended to be introduced to medical students as early as possible,12 preferably during their pre-clinical years. However, the articles selected in this scoping review indicated that most of the CR training sessions were designed for educators teaching clinical students. Educators in pre-clinical or basic science subjects must also critically be aware of CR. A pressing need exists to incorporate CR during the pre-clinical or early years in medical school, to shape students' thinking skills. The differences in teaching and learning environments and methods between the pre-clinical and clinical years might have led medical educators to focus on CR primarily in the clinical years. The demand of the academic burden placed on pre-clinical or basic science educators, given that these subjects are taught on a tight timetable, might contribute to the lack of earlier CR introduction. Learning has focused on structured goals and knowledge recall,34 with sessions of active learning—such as problem-based learning and SGDs—interspersed between passive learning sessions. Little or minimal formal teaching on clinical aspects is provided during the pre-clinical years. However, the learning environment then evolves into clinical clerkship and knowledge synthesis in the clinical years,34 including assimilation and application of pre-existing biomedical and clinical knowledge. To introduce CR to pre-clinical or basic science students, educators must be aware of the CR concepts, cognitive steps and teaching strategies suitable for pre-clinical subjects. Moreover, educators must be able to incorporate these aspects into their teaching.
CR was used by all healthcare professionals, despite the diverse scope of the work and practice of these professions. For example, emergency physicians and paramedics treat patients in acute condition, thus necessitating a rapid CR process, particularly in determining a sound diagnosis and initial management plan.24 In contrast, for occupational therapists treating patients with established diagnoses, CR is applied primarily in patients' long-term support and management.35 According to this scoping review, most training sessions for educators were conducted in the medical profession; this pattern has also been observed in a recent scoping review by Young et al. in 20201 on CR studies in health professions, in which most studies on CR were found to be in the medical field. Other health professions must be encouraged to design and develop their own training sessions for educators, to cater the unique practices of each healthcare profession.
RQ2: What are the learning outcomes of CR training sessions for undergraduate health profession educators?
RQ3: What are the methods of the CR training sessions for undergraduate health profession educators?
For students to learn CR, the following goals should be achieved: (1) understanding reasoning; the cognitive process involved, the vocabulary and terminologies, and the map of the reasoning process; (2) integration of knowledge and skill; and (3) understanding uncertainty and diagnostic error, including an introduction to the concepts of bias and error.36 The CR training sessions in this scoping review addressed these goals with the inclusion of a cognitive approach in CR (DPT); the common terminologies used; the steps of CR; and the application of problem representation, with semantic qualifiers and formation of illness scripts, and cognitive biases and debiasing techniques. However, a single training session might not focus on all these goals, because time may be a limiting factor. In addition, the identification and remediation of learners with CR difficulties was a focus in these training sessions. The use of common CR terminologies might decrease confusion among health educators, as they were at the same level of understanding during any discussion.37 After data gathering, mental abstraction or problem representation is used to encapsulate the pertinent findings for each patient. Application of problem representation with related semantic qualifiers has been associated with strong CR.38 According to script theory, the manner in which information is stored and retrieved influences the interpretation of events that occurred39 and subsequently translates to the formation of illness scripts in which the predisposing conditions, pathophysiological insults and clinical consequences38 of different diseases are created in the mind. Illness scripts are dynamic, and new information may be added with the acquisition of new knowledge and experience. This form of knowledge storage in a clinically relevant manner may help students recall the appropriate illness script when faced with similar situations.10 To create problem representation and illness scripts, knowledge, experience and deliberate practice are important. The content of these training sessions may be referenced by other health professionals wishing to conduct such training in their own professions, albeit with modifications.
Various formats of training sessions were used to accommodate the goals of the institutions through incorporation of passive and active learning methods. In deciding how to conduct the training, consideration of learning theories, such as adult learning theory, and of elements of instructional design is important.40 These formats of active learning increase educators' participation, thereby allowing them to apply their knowledge learnt in practice; this aligns well with adult learning theory, in which adults prefer learning that is relevant to their daily issues. In addition, Kolb's experiential theory had also been referenced25,29 in the design and development of these training sessions. An important aspect in these CR training sessions is reflection or metacognition. Studies on CR strategies advocate for the use of metacognition in every step of the CR process, to potentially increase awareness of cognitive bias.41
RQ4: What is the feedback regarding the CR training sessions for educators?
Given the lack of a clear theoretical framework for how to develop faculty development programmes,42 the CR training sessions featured in this scoping review were found to be well-designed and accepted by the educators, on the basis of their feedback on how these sessions were conducted. Educational theories, such as constructivism, situated learning42 and adult learning,40 have been reported to be incorporated in such programmes. The aims, objectives and conduct may also differ according to institutions' unique concerns, initiatives and responsibilities to address, according to their institutional needs and culture.43
Although educators rated the content of the training sessions highly, and gained confidence in applying these CR strategies in their teaching, longitudinal follow-up of the educators did not occur after most training sessions. Some educators did respond to the post workshop feedback requests; however, these responses were based on the respondents' perceptions. An exception was the training session reported by Schaye et al.26 in 2019, in which simulated students rated educators' use of CR strategies during the teaching sessions. To ascertain the beneficial outcomes of these training sessions, a direct observation or empirical study must be conducted.24
Limitations
This scoping review has several limitations. Because the articles chosen were only in English language, some articles written on CR training in non-English journals might have been missed. Moreover, the articles chosen were from different healthcare professions, with different medical curricula and clinical exposure, thus potentially causing some variations in the conduct and content of the CR training sessions.
Conclusion
The CR training sessions were conducted primarily for clinical educators in the field of medicine. Although the educators rated these sessions highly and gained confidence, further empirical study is necessary to examine the actual application and effectiveness of these teaching strategies. Determining whether implementation of such training sessions for pre-clinical or basic science educators with longitudinal feedback might increase their awareness regarding CR and the domains of CR education should prove interesting.
Source of funding
This work was supported by Universiti Kebangsaan Malaysia's Faculty of Medicine Fundamental Grant (grant number: FF-2022-079).
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
Ethical approval was obtained on 14 April 2022 with approval number UKM PPI/111/8/JEP-2022-219.
Consent
Because this was a scoping review, consent is not applicable.
Authors contributions
SN: Conceptualization, Methodology, Analysis, Investigation and Writing—Original Draft. MNY: Conceptualization, Methodology, Investigation, Writing—Review & Editing and Supervision. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Acknowledgment
This scoping review was made possible by the support of Universiti Kebangsaan Malaysia's Faculty of Medicine Fundamental Grant (grant number: FF-2022-079).
Footnotes
Peer review under responsibility of Taibah University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jtumed.2023.06.002.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Young M.E., Thomas A., Lubarsky S., Gordon D., Gruppen L.D., Rencic J., et al. Mapping clinical reasoning literature across the health professions: a scoping review. BMC Med Educ. 2020;20:1–11. doi: 10.1186/s12909-020-02012-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daniel M., Rencic J., Durning S.J., Holmboe E., Santen S.A., Lang V., et al. Clinical reasoning assessment methods: a scoping review and practical guidance. Acad Med. 2019;94(6):902–912. doi: 10.1097/ACM.0000000000002618. [DOI] [PubMed] [Google Scholar]
- 3.Cooper N., Bartlett M., Gay S., Hammond A., Lillicrap M., Matthan J., et al. UK Clinical Reasoning in Medical Education (CReME) consensus statement group. Consensus statement on the content of clinical reasoning curricula in undergraduate medical education. Med Teach. 2021;43(2):152–159. doi: 10.1080/0142159X.2020.1842343. [DOI] [PubMed] [Google Scholar]
- 4.Pelaccia T., Tardif J., Triby E., Charlin B. An analysis of clinical reasoning through a recent and comprehensive approach: the dual-process theory. Med Educ Online. 2011;16(1):5890. doi: 10.3402/meo.v16i0.5890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization . 2016. Diagnostic errors. [Google Scholar]
- 6.Graber M.L., Franklin N., Gordon R. Diagnostic error in internal medicine. Arch Intern Med. 2005;165(13):1493–1499. doi: 10.1001/archinte.165.13.1493. [DOI] [PubMed] [Google Scholar]
- 7.Eva K.W. What every teacher needs to know about clinical reasoning. Med Educ. 2004;39(1):98–106. doi: 10.1111/j.1365-2929.2004.01972.x. [DOI] [PubMed] [Google Scholar]
- 8.Croskerry P. A universal model of diagnostic reasoning. Acad Med. 2009;84(8):1022–1028. doi: 10.1097/ACM.0b013e3181ace703. [DOI] [PubMed] [Google Scholar]
- 9.Lambe K.A., O'Reilly G., Kelly B.D., Curristan S. Dual-process cognitive interventions to enhance diagnostic reasoning: a systematic review. BMJ Qual Saf. 2016;25(10):808–820. doi: 10.1136/bmjqs-2015-004417. [DOI] [PubMed] [Google Scholar]
- 10.Pinnock R., Welch P. Learning clinical reasoning. J Paediatr Child Health. 2014;50(4):253–257. doi: 10.1111/jpc.12455. [DOI] [PubMed] [Google Scholar]
- 11.Pinnock R., Young L., Spence F., Henning M., Hazell W. Can think aloud be used to teach and assess clinical reasoning in graduate medical education? J Grad Med Educ. 2015;7(3):334–337. doi: 10.4300/JGME-D-14-00601.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khin-Htun S., Kushairi A. Twelve tips for developing clinical reasoning skills in the pre-clinical and clinical stages of medical school. Med Teach. 2019;41(9):1007–1011. doi: 10.1080/0142159X.2018.1502418. [DOI] [PubMed] [Google Scholar]
- 13.Rencic J., Trowbridge R.L., Fagan M., Szauter K., Durning S. Clinical reasoning education at US medical schools: results from a national survey of internal medicine clerkship directors. J Gen Intern Med. 2017;32(11):1242–1246. doi: 10.1007/s11606-017-4159-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kononowicz A.A., Hege I., Edelbring S., Sobocan M., Huwendiek S., Durning S.J. The need for longitudinal clinical reasoning teaching and assessment: results of an international survey. Med Teach. 2020;42(4):457–462. doi: 10.1080/0142159X.2019.1708293. [DOI] [PubMed] [Google Scholar]
- 15.Hoffert M.M., Passalacqua K.D., Haftka-George A., Abreu Lanfranco O., Martin R.A. A curriculum for enhancing physician teaching skills: the value of physician-educator partnerships. J Med Educ Curric Dev. 2021;8:1–11. doi: 10.1177/23821205211032013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arksey H., O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 17.Levac D., Colquhoun H., O'Brien K.K. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):1–9. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harasym P.H., Tsai T.C., Hemmati P. Current trends in developing medical students' critical thinking abilities. Kaohsiung J Med Sci. 2008;24(7):341–355. doi: 10.1016/S1607-551X(08)70131-1. [DOI] [PubMed] [Google Scholar]
- 19.Pien L.C., Taylor C.A., Traboulsi E., Nielsen C.A. A pilot study of a “resident educator and life-long learner” program: using a faculty train-the-trainer program. J Grad Med Educ. 2011;3(3):332–336. doi: 10.4300/JGME-03-03-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Foster K., Laurent R. How we make good doctors into good teachers: a short course to support busy clinicians to improve their teaching skills. Med Teach. 2013;35(1):4–7. doi: 10.3109/0142159X.2012.731098. [DOI] [PubMed] [Google Scholar]
- 21.Dhaliwal G. Developing teachers of clinical reasoning. Clin Teach. 2013;10(5):313–317. doi: 10.1111/tct.12082. [DOI] [PubMed] [Google Scholar]
- 22.Addy T.M., Hafler J., Galerneau F. Faculty development for fostering clinical reasoning skills in early medical students using a modified Bayesian approach. Teach Learn Med. 2016;28(4):415–423. doi: 10.1080/10401334.2016.1186551. [DOI] [PubMed] [Google Scholar]
- 23.Weinstein A., Gupta S., Pinto-Powell R., Jackson J., Appel J., Roussel D., et al. Diagnosing and remediating clinical reasoning difficulties: a faculty development workshop. MedEdPORTAL. 2017;13 doi: 10.15766/mep_2374-8265.10650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Daniel M., Carney M., Khandelwal S., Merritt C., Cole M., Malone M., et al. Cognitive debiasing strategies: a faculty development workshop for clinical teachers in emergency medicine. MedEdPORTAL. 2017;13 doi: 10.15766/mep_2374-8265.10646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liao H.C., Yang Y.M., Li T.C., Cheng J.F., Huang L.C. The effectiveness of a clinical reasoning teaching workshop on clinical teaching ability in nurse preceptors. J Nurs Manag. 2019;27(5):1047–1054. doi: 10.1111/jonm.12773. [DOI] [PubMed] [Google Scholar]
- 26.Schaye V., Janjigian M., Hauck K., Shapiro N., Becker D., Lusk P., et al. A workshop to train medicine faculty to teach clinical reasoning. Diagnosis. 2019;6(2):109–113. doi: 10.1515/dx-2018-0059. [DOI] [PubMed] [Google Scholar]
- 27.Talberg H., Camroodien-Surve F., Amosun S.L. Understanding of clinical reasoning by undergraduate students and clinical educators in health and rehabilitation sciences at a South African University: the implications for teaching practice. Afr J Health Prof Educ. 2021;13(4):247–252. [Google Scholar]
- 28.Atkinson H.L., Nixon-Cave K. A tool for clinical reasoning and reflection using the international classification of functioning, disability and health (ICF) framework and patient management model. Phys Ther. 2011;91(3):416–430. doi: 10.2522/ptj.20090226. [DOI] [PubMed] [Google Scholar]
- 29.Cohen A., Sur M., Weisse M., Moffett K., Lancaster J., Saggio R., et al. Teaching diagnostic reasoning to faculty using an assessment for learning tool: training the trainer. MedEdPORTAL. 2020;16 doi: 10.15766/mep_2374-8265.10938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Boileau E., Audétat M.C., St-Onge C. Just-in-time faculty development: a mobile application helps clinical teachers verify and describe clinical reasoning difficulties. BMC Med Educ. 2019;19(1):1–8. doi: 10.1186/s12909-019-1558-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Steinert Y., Mann K., Anderson B., Barnett B.M., Centeno A., Naismith L., et al. A systematic review of faculty development initiatives designed to enhance teaching effectiveness: a 10-year update: BEME Guide No. 40. Med Teach. 2016;38(8):769–786. doi: 10.1080/0142159X.2016.1181851. [DOI] [PubMed] [Google Scholar]
- 32.Committee on Diagnostic Error in Health Care; Board on Health Care Services; Institute of Medicine; The National Academies of Sciences, Engineering, and Medicine . In: Improving diagnosis in health care. Balogh E.P., Miller B.T., Ball J.R., editors. National Academies Press (US); Washington (DC): 2015. PMID: 26803862. [PubMed] [Google Scholar]
- 33.Angus L.M., Chur-Hansen A., Duggan P. A qualitative study of experienced clinical teachers' conceptualisation of clinical reasoning in medicine: implications for medical education. Focus Health Prof Educ Multidiscip J. 2018;19(1):52–64. [Google Scholar]
- 34.Chumley H., Olney C., Usatine R., Dobbie A. A short transitional course can help medical students prepare for clinical learning. Fam Med. 2005;37(7):496–501. [PubMed] [Google Scholar]
- 35.Higgs J., Jensen G.M. In: Clinical reasoning in the health professions. Higgs J., Jensen G.M., Loftus S., Christensen N., editors. Elsevier Health Sciences; 2019. Clinical reasoning: challenges of interpretation and practice in the 21st century; pp. 3–12. [Google Scholar]
- 36.Connor D.M., Dhaliwal G., Bowen J.L. In: Clinical reasoning in the health professions. Higgs J., Jensen G.M., Loftus S., Christensen N., editors. Elsevier Health Sciences; 2019. Teaching clinical reasoning in medical education courses; pp. 345–358. [Google Scholar]
- 37.Young M., Thomas A., Gordon D., Gruppen L., Lubarsky S., Rencic J., et al. The terminology of clinical reasoning in health professions education: implications and considerations. Med Teach. 2019;41(11):1277–1284. doi: 10.1080/0142159X.2019.1635686. [DOI] [PubMed] [Google Scholar]
- 38.Bowen J.L. Educational strategies to promote clinical diagnostic reasoning. N Eng J Med. 2006;355(21):2217–2225. doi: 10.1056/NEJMra054782. [DOI] [PubMed] [Google Scholar]
- 39.Lubarsky S., Dory V., Audétat M.C., Custers E., Charlin B. Using script theory to cultivate illness script formation and clinical reasoning in health professions education. Can Med Educ J. 2015;6(2):e61. [PMC free article] [PubMed] [Google Scholar]
- 40.Steinert Y., Mann K.V. Faculty development: principles and practices. J Vet Med Educ. 2006;33(3):317–324. doi: 10.3138/jvme.33.3.317. [DOI] [PubMed] [Google Scholar]
- 41.Cutrer W.B., Sullivan W.M., Fleming A.E. Educational strategies for improving clinical reasoning. Curr Probl Pediatr Adolesc Health Care. 2013;43(9):248–257. doi: 10.1016/j.cppeds.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 42.Steinert Y. Perspectives on faculty development: aiming for 6/6 by 2020. Perspect Med Educ. 2012;1(1):31–42. doi: 10.1007/s40037-012-0006-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schei E., Fuks A., Boudreau J.D. Reflection in medical education: intellectual humility, discovery, and know-how. Med Healthc Philos. 2019;22(2):167–178. doi: 10.1007/s11019-018-9878-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.