Abstract
BACKGROUND:
The aim of this study is to evaluate the indications and efficacy of facial nerve decompression through an endoscopic transcanal approach for patients with traumatic facial paralysis.
Methods:
This single-center retrospective study included 11 patients with traumatic facial paralysis from February 2018 to April 2019. We compared the facial nerve and auditory function before and after operation so as to reveal the feasibility and effect of the surgical approach.
Results:
All 11 patients have successfully received facial nerve decompression through endoscopic transcanal approach. Facial nerve function was objectively evaluated by electroneurography test and House-Brackmann facial nerve grading system. All patients were graded HB-VI with electroneurography ≥ 95% before surgery. The recovery of facial nerve function was good (HB-I or II) (90.9%) a year after surgery with only one case (9.1%) for HB-III. Preoperative high-resolution computed tomography showed that 1 patient had ossicular chain interruption, which was confirmed during operation. Meanwhile, 2 patients with air-bone gap >35 dBHL and whose computed tomography failed to diagnose were found with ossicular chain interruption during operation. The air-bone gap of patients with normal ossicular chain connection was all <30 dBHL. The average air-bone gap was reduced from 27.5 ± 10.1 dBHL to 7.8 ± 3.3 dBHL after operation.
Conclusion:
Preoperative high-resolution computed tomography combined with localization test can accurately estimate the location of facial nerve injury. Facial nerve decompression through endoscopic transcanal approach can decompress the geniculate ganglion to pyramidal segment of facial nerve, which is suitable for patients with traumatic facial paralysis of this segment. In addition, air-bone gap >35 dBHL may indicate the ossicular chain interruption when it is difficult to be completely judged by high-resolution computed tomography.
Keywords: Facial nerve decompression, endoscopy, transcanal approach, traumatic facial paralysis
Introduction
Traumatic facial paralysis is one of the most important causes of peripheral facial paralysis, accounting for about 17% of its incidence, second to Bell’s facial paralysis.1 Temporal bone fracture is the main cause of traumatic facial paralysis, and the incidence of facial paralysis in such patients can reach 7-10%.1-3
The traditional surgical method is to decompress facial nerve through microscopic mastoid approach. Although it can achieve good effects, patients will have more bone grinding off and greater trauma. With the pursuit of minimal invasive surgery, the application of endoscopy has gradually expanded in recent years.4,5 At present, there are only a few reports on the treatment of patients with traumatic facial paralysis through endoscopic transcanal approach. The results show that the facial paralysis and hearing level of patients after operation have been improved, which proves the feasibility and effect of this approach to a certain extent. Due to the small number of cases, it is hard to form good clinical reference evidence.5
Therefore, our study retrospectively analyzed 11 cases of patients with traumatic facial paralysis treated by facial nerve decompression through endoscopic transcanal approach and further comprehensively explored the indications and efficacy of this approach, hoping to provide reference for its clinical application.
Methods
Patient Selection
Of all the patients with facial paralysis treated at our hospital from February 2018 to April 2019, 11 cases met the inclusion criteria:
HB-VI before surgery.
A greater than 95% reduction in amplitude on electroneurography (ENoG) test relative to the unaffected side of the face before surgery.
High-resolution CT (HRCT) showed fracture lines of temporal bone involving geniculate ganglion or tympanic segment of facial nerve through mastoid process, but with no involvement of inner ear structure.
Sufficient doses of steroids had been taken in the first 2 weeks after onset, and there was no improvement in the degree of facial paralysis.
No relevant surgical history or systemic disease affecting prognosis.
Patients with traumatic facial paralysis simultaneously suffered from other facial nerve diseases were excluded.
This study has been approved by the Ethics Committees of Shanghai Ninth People’s Hospital Affliated to Shanghai Jiao Tong University School of Medicine (SH9H-2022-T284-1). All 11 patients were fully informed about the possible complications and inevitable ossicular chain reconstruction during the surgery.
Clinical Data
Our retrospective study was based on the clinical data of 11 patients who suffered from peripheral facial nerve paralysis caused by temporal bone fracture in our hospital (Table 1). The age ranged from 11 to 59 years. The causes of trauma included 6 cases of traffic accident (54.5%), 4 cases of falling injury (36.4%), and 1 case of head hit injury (9.1%). According to the medical history, 9 cases had immediate onset of facial paralysis, and the other 2 were found severe facial paralysis after awaking from craniocerebral trauma whom we speculated that were also highly likely to have an immediate onset. It is certain that these 11 patients with facial paralysis came to our hospital after initial conservative treatment at other hospitals without recovery. The duration of preoperative paralysis ranged from 14 days to 92 days, with an average of 48 days. All operations were performed by the same operator. All patients were followed up for at least 12 months to evaluate the recovery of facial nerve function and hearing reconstruction.
Table 1.
Patient Data and Preoperative Evaluation Results
| Patient no. | Age (Years) | Gender | Side | Duration of Preoperative Facial Paralysis (Days) | Location of Injury | HB Grade | ABG (dBHL) | ENoG (%) |
|---|---|---|---|---|---|---|---|---|
| 1 | 33 | M | L | 16 | HSFN | VI | 23.8 | 100 |
| 2 | 40 | M | R | 86 | HSFN | VI | 27.5 | 96 |
| 3 | 40 | M | R | 54 | HSFN、GG | VI | 17.5 | 100 |
| 4 | 11 | M | R | 14 | HSFN | VI | 27.5 | 97 |
| 5 | 44 | F | R | 21 | HSFN | VI | 17.5 | 95 |
| 6 | 53 | F | L | 24 | HSFN | VI | 23.8 | 96 |
| 7 | 46 | M | L | 92 | HSFN、GG | VI | 37.5 | 98 |
| 8 | 36 | F | L | 21 | HSFN | VI | 46.3 | 100 |
| 9 | 59 | F | L | 86 | HSFN、GG | VI | 12.5 | 100 |
| 10 | 56 | M | R | 56 | HSFN、GG | VI | 28.8 | 95 |
| 11 | 12 | F | L | 60 | HSFN | VI | 37.5 | 97 |
ABG, air-bone gap; ENoG, electroneurography; GG, geniculate ganglion; HSFN, horizontal segment of the facial nerve.
Preoperative Examination
Before operation, HRCT of temporal bone was used to evaluate the site of facial nerve injury, ENoG test to evaluate the injury degree of facial nerve function, and pure tone audiometry (PTA) to evaluate the hearing level. At the same time, we combined the results of localization test, House-Brackmann (HB) grade, and endoscopic examination.
Assessment of Location of Facial Nerve Injury
All patients underwent HRCT of temporal bone before operation, and facial nerve enhanced MRI examination when necessary. The diagnosis of temporal bone fracture, the range of fracture line involvement, and the range of facial nerve swelling were determined according to the imaging results. At the same time, the tear overflow test, stapedius reflex test, and taste test were conducted before operation to assist in judging the injury site of facial nerve.
Assessment of Facial Nerve Function
The grade of facial nerve injury was evaluated by ENoG test and HB grade.
Assessment of Post-traumatic Hearing Level
All patients underwent bilateral endoscopic examination before operation to evaluate whether there were post-traumatic external auditory meatus stenosis and tympanic membrane perforation. At the same time, bilateral PTA should be performed to calculate the average hearing threshold and air-bone gap (ABG) and evaluate whether there was post-traumatic hearing loss.
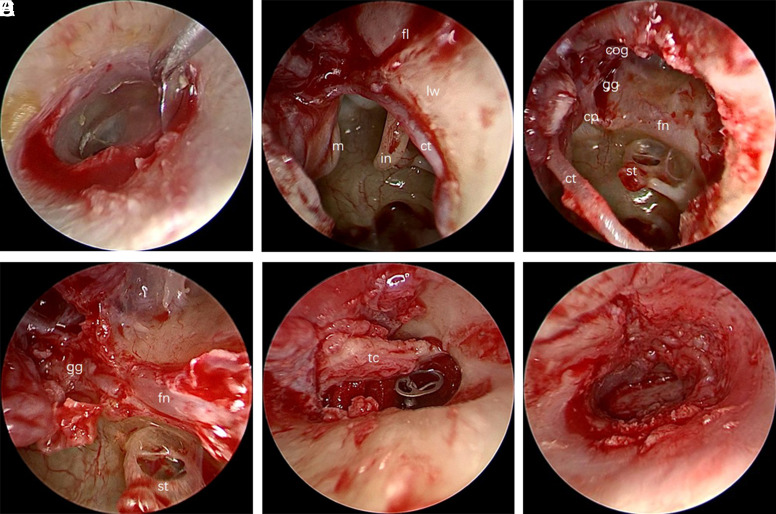
Surgical Method
All surgeries of facial nerve decompression through endoscopic transcanal approach were performed by a single experienced surgeon. Intraoperative facial nerve monitoring was applied in all cases. An incision was made through the external auditory canal (EAC) from the superior 10 o’clock position to the inferior 6 o’clock position (Figure 1A) to create a standard tympanomeatal flap. The tympanic membrane flap of the external auditory meatus was turned up, the lateral wall of attic was exposed (Figure 1B), and the tympanic membrane was separated from the short process of malleus, retaining the complete tympanic membrane. During the operation, we found 2 cases of incudostapedial joint dislocation, and one had stapes neck fracture. Then the epitympanic recess and the short crus of incus were exposed and the incus was removed. Malleus scissors was used to cut the malleus with the manubrium of malleus retained (Figure 1C). The tegmen tympani upward and the cone segment with the stapedial muscle were exposed as the symbol. After grinding off the bone on the surface of horizontal segment of facial nerve, the geniculate ganglion of facial nerve was located at the front and upper part of cochleariform process. Then the operator ground off the odontoid process and the air cells of the anterior superior tympanic chamber. Tracking the superficial greater petrosal nerve forward along the bottom of the middle cranial fossa, the geniculate ganglion of facial nerve was completely exposed (Figure 1D). After that, the operator removed the bone at the junction of the geniculate ganglion and the beginning of the labyrinthine segment inward and cut the facial nerve sheath from here to the pyramidal segment to complete a decompression. Removal of the bone canal of facial nerve depended on its thickness. For the thinner bone canal, it could be removed by curette directly. For the thicker one, we first grounded out the thick bone canal with low-speed micro-drill and then used the curette to scrape the remaining bone on the surface of facial nerve. When the facial nerve sheath was fully exposed, the scythe was used to cut and decompress. After the decompression, the nerve was covered with dexamethasone gelatin sponge. An electrophysiological examination was performed both before and after the procedures. The presence of stimulation-evoked potential waves was detected by electrodes in the peripheral facial muscles or the stapedius reflex, which were recorded as they may be relevant to the patient’s prognosis. After the decompression, reconstruction of the ossicular chain with titanium prosthesis (TTP-Vario Partial Prosthesis, Heinz Kurz GmbH, Germany) was performed (Figure 1E). The tragus cartilage with perichondrium was excised and placed between the tympanic membrane and the artificial ossicules and then the lateral wall of the attic was reconstructed. Finally, the operator restored the tympanic flap of the EAC (Figure 1F). The EAC was stuffed with absorbent material and gauze for about 2 weeks after surgery.
Figure 1.
Steps of transcanal endoscopic decompression of tympanic facial nerve. (A) Make a curved external auditory canal incision. (B) Turn up the tympanic membrane flap of the external auditory meatus. (C) Grind off the lateral wall of the attic and remove the incus and malleus. (D) Grind off the bone canal of facial nerve and cut the facial nerve sheath. (E) Implant artificial auditory ossicles and reconstruct the lateral wall of the attic. (F) Restore the tympanic flap of the external auditory meatus. cp, cochleariform process; ct, chorda tympani nerve; fl, fracture line; fn, facial nerve; gg, geniculate ganglion; in, incus; lw, lateral wall of the attic; m, malleus; tc, tragus cartilage.
Efficacy Assessment
All patients were followed up for at least 12 months. Endoscopy was performed 2 weeks after operation to evaluate the situation of EAC. At 6 and 12 months after operation, 2 doctors of our department evaluated their HB grade of facial nerve function. If necessary, ENoG test was used to evaluate the recovery of facial nerve. The standard of satisfactory recovery of facial nerve function was HB-I or -II on the surgical side 12 months after operation. The hearing reconstruction was evaluated by PTA 12 months after operation.
Statistical Methods
Statistical Package for Social Sciences Version 24.0. (IBM SPSS Corp.; Armonk, NY, USA) statistical software was used for analysis. The changes in neurological function before and after operation were compared by paired sample nonparametric test (Wilcoxon signed rank test). Fisher’s correction test was used to count the number of patients with satisfactory and unsatisfactory recovery of facial nerve function 12 months after operation. Independent 2-sample t-test was used to compare the relevance between time of preoperative facial paralysis and surgical efficacy. Paired t-test was used to the changes in hearing level before and after operation. The difference was significant when P < .05. The data were expressed as mean ± standard deviation(x±s).
Results
Location of Facial Nerve Injury
Preoperative HRCT of the temporal bone showed that the fracture line of temporal bone in all patients involved geniculate ganglion or tympanic segment of facial nerve through mastoid process, but there was no involvement of inner ear structure. Combined with the results of the tear overflow test, stapedius reflex test, and taste test, the injury site was located in the tympanic segment, which was consistent with the intraoperative findings. During the operation, we found that all cases had different degrees of facial nerve and geniculate ganglion edema. Among them, 4 patients had fracture pieces inserted into facial nerve and 1 had incus displacement and compression (Table 2). All patients had no facial nerve rupture.
Table 2.
Injury Confirmed during Operation
| Patient no. | Location of Injury | Type of Injury |
|---|---|---|
| 1 | HSFN | I, II |
| 2 | HSFN | I |
| 3 | HSFN, GG | I |
| 4 | HSFN | I, II |
| 5 | HSFN | I, II |
| 6 | HSFN | I |
| 7 | HSFN, GG | I |
| 8 | HSFN | I, III |
| 9 | HSFN, GG | I |
| 10 | HSFN, GG | I, II |
| 11 | HSFN | I |
GG, geniculate ganglion; HSFN, horizontal segment of the facial nerve; I, edema; II, fracture piece oppression; III, incus oppression.
Facial Nerve Recovery
The facial nerve function was evaluated by HB grade. All 11 patients with facial paralysis were HB-VI preoperatively. Compared to the unaffected side, the injured side of every patient showed a greater than 95% reduction in amplitude of the ENoG test, and the average was a greater than 97.6%, including 4 cases of 100%, 2 cases of 95%, 96%, and 97% respectively, and 1 case of 98%. Six months after operation, the facial nerve function of all patients recovered in varying degrees, including 2 cases of HB-I, 6 cases of -II, and 3 cases of -III. Twelve months after operation, the facial nerve function of all patients was improved compared with that before operation (P = .002), including 7 cases of HB-I, 3 cases of -II, and 1 case of -III (Table 3). All patients had paralysis for 14-92 days before operation, with an average duration of 48 days. Among them, we found that 7 patients (63.6%) made a full recovery to HB-I during follow-up, whose average duration of preoperative paralysis was 34.6 days, while for 4 patients (36.4%) with incomplete recovery (HB-II or -III), it was 72 days. There was no significant difference in statistics. Due to insufficient number of cases, more samples need to be further studied.
Table 3.
Facial Nerve Function after Operation
| Patient no. | Age (Years) | Duration of Preoperative Facial Paralysis (Days) | Average Duration of Preoperative Facial Paralysis (days) | House-Brackmann (HB) grade | P | |
|---|---|---|---|---|---|---|
| 6 mon after Operation | 12 mon after Operation | |||||
| 2 | 40 | 86 | 72 | II | II | 0.09704 |
| 6 | 53 | 24 | III | II | ||
| 7 | 46 | 92 | II | II | ||
| 9 | 59 | 86 | III | III | ||
| 1 | 33 | 16 | 34.6 | II | I | |
| 3 | 40 | 54 | III | I | ||
| 4 | 11 | 14 | I | I | ||
| 5 | 44 | 21 | II | I | ||
| 8 | 36 | 21 | II | I | ||
| 10 | 56 | 56 | II | I | ||
| 11 | 12 | 60 | I | I | ||
It is classified by House-Brackmann grade which is internationally common used, and the classification standards are as follows. HB grade I: Normal symmetrical function; HB grade II: Slight weakness noticeable only on close inspection, Complete eye closure with minimal effort, Slight asymmetry of smile with maximal effort, Synkinesis barely noticeable, contracture or spasm absent; HB grade III: Obvious weakness, but not disfiguring, May not be able to lift eyebrow, Complete eye closure and strong but asymmetrical mouth movement, Obvious, but not disfiguring synkinesis, mass movement or spasm.
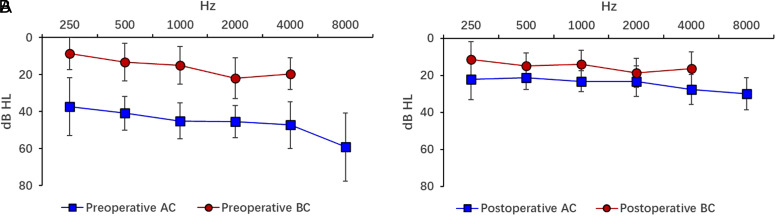
Hearing Function
Postoperative PTA results showed that the average hearing threshold of air conduction (AC) was 44.7 ± 7.73 dBHL, the average hearing threshold of bone conduction (BC) was 17.4 ± 9.1dBHL, and the average ABG was 27.5 ± 10.1 dBHL. Three cases were confirmed as traumatic ossicular chain interruption during operation, including 2 cases of incudostapedial joint dislocation and 1 stapes neck fracture. Eight patients without ossicular chain interruption and 2 patients with incudostapedial joint dislocation have undergone ossicular chain reconstruction with partial ossicular replacement prosthesis(PORP), and 1 with stapes neck fracture has undergone ossicular chain reconstruction with total ossicular replacement prosthesis(TORP). The PTA was re-examined 12 months after operation. All patients achieved the improvement of audiological results. The average hearing threshold of AC was 23.9 ± 5.5 dBHL, the average hearing threshold of BC was 16.02 ± 6.5 dBHL, and the average ABG was reduced to 7.8 ± 3.3 dBHL. The postoperative ABG was smaller than that before operation, which was less than 20 dBHL 12 months after operation (Figure 2), and the difference was statistically significant (t = 7.332, P < .001).
Figure 2.
Mean hearing level before and after operation. (A) Mean hearing level before operation. (B) Mean hearing level after operation. The mean bone conduction hearing level after operation was improved and the air-bone gap was reduced compared with that before operation, and the difference was statistically significant. AC, air conduction; BC, bone conduction.
Among the 3 patients with ossicular chain interruption before operation, the preoperative ABG was >35 dBHL and the average was 40.4 dBHL. Among the patients without ossicular chain interruption before operation, the preoperative ABG was <30 dBHL and the average was 22.6dB, which had statistically significant difference compared with the patients with ossicular chain interruption (Table 4).
Table 4.
Comparison of Preoperative Ossicular Chain Interruption with Corresponding CT and Hearing Injury
| Patient No. | Type of Ossicular Chain Interruption Confirmed During Operation | Preoperative CT Diagnosis | Preoperative ABG (dBHL) | Preoperative Average ABG (dBHL) | P |
|---|---|---|---|---|---|
| 7 | Incudostapedial joint dislocation | Not found | 37.5 | 40.4 | 0.00194 |
| 8 | Incudostapedial joint dislocation | Found | 46.3 | ||
| 11 | Colliculus stapedis fracture | Not found | 37.5 | ||
| 1 | Not found | Not found | 23.8 | 22.6 | |
| 2 | Not found | Not found | 27.5 | ||
| 3 | Not found | Not found | 17.5 | ||
| 4 | Not found | Not found | 27.5 | ||
| 5 | Not found | Not found | 17.5 | ||
| 6 | Not found | Not found | 23.8 | ||
| 9 | Not found | Not found | 12.5 | ||
| 10 | Not found | Not found | 31.3 |
ABG, air-bone gap; CT, computed tomography.
Postoperative Complications
Two patients had mild synkinesis on the operative side, and 3 had mild tinnitus after operation, which had no significant impact on their life. All patients had no other complications.
Discussion
Facial paralysis will seriously affect patients’ normal social life and make them suffer great psychological pain.6,7 Therefore, active and effective treatment of facial paralysis is of great significance to improve physical and mental health of patients.
The choice of surgical approach for facial nerve decompression for traumatic facial paralysis is mainly based on the preoperative evaluation of the location of facial nerve injury and hearing level. Tympanic pathway is often selected for the vertical and horizontal segments of facial nerve injury, which can expose the distal nerve of geniculate ganglion to the stylomastoid foramen, and ossicular chain reconstruction can be performed at the same time. The middle cranial fossa approach can expose the labyrinthine segment, geniculate ganglion, and part of the tympanic segment, retaining the mastoid middle ear structure and do not affect the ossicular chain, which is suitable for patients with practical hearing and facial nerve injury located in geniculate ganglion and internal auditory canal. However, the 2 approaches require a retroauricular incision and more normal bone grinding off. Although the operation effect is good, the operation trauma is relatively large, and the recovery time is long, with skin scar left, which affects the beauty.
With the accumulation of clinical experience and the further understanding of the concept and technology of endoscopy, endoscopy is increasingly widely used in ear surgery. The advantage of endoscopy is that it makes full use of the natural canal as the surgical channel to avoid retroauricular incision and large-scale normal bone grinding off, which can reduce surgical trauma and shorten the recovery time.8 Endoscopy can overcome the limitations of the operation field in the past microsurgery, and comprehensively and clearly expose the structures such as incudostapedial joint, tympanic segment of facial nerve, and geniculate ganglion,5 so as to make a full and complete facial nerve decompression.9 Studies have shown that about 65.8% of patients with temporal bone fractures have different degrees of conductive hearing loss, especially those with ossicular chain interruption.10-13 Endoscopy can fully expose the structure of malleus handle and stapes under direct vision, so it can provide favorable conditions for the exploration and reconstruction of ossicular chain, to guarantee a better postoperative hearing recovery.
At present, there are few reports on the effect of facial nerve decompression through endoscopic transcanal approach for patients with traumatic facial paralysis. Kahinga et al5 have reported 2 cases of traumatic facial paralysis treated through endoscopic transcanal approach. The preoperative nerve function was HB-IV and HB-V, respectively, and recovered to HB-II and –III, respectively, after operation. The postoperative hearing level was improved.5 The study confirmed the feasibility and efficacy of this approach to a certain extent, but because of the small number of cases and the short follow-up time, it failed to form good clinical reference evidence. The anatomical study of Marchioni et al4 demonstrated that endoscopic transcanal approach can fully expose the geniculate ganglion to the pyramidal segments of the facial nerve, which provided evidence for the use of this pathway in patients with traumatic facial paralysis of tympanic facial nerve injury. Therefore, we conducted this study. The facial nerve function of all patients get different degrees of recovery 12 months after facial nerve decompression through endoscopic transcanal approach compared with that before surgery (P = .002), and the hearing level was also improved, which indicates the feasibility and surgical effect of this pathway to some extent.
The location of facial nerve injury before operation was mainly evaluated by HRCT of temporal bone combined with localization test. In our study, all cases underwent HRCT before operation, and the segments of facial nerve injury were judged according to the clinical manifestations localization test results. Preoperative CT showed that the facial nerve injury was mainly located between the geniculate ganglion and the pyramidal segments, which was basically confirmed with the findings during operation, indicating the feasibility of this positioning evaluation method, which can lay a foundation for the selection of decompression approach. In addition, HRCT also has a certain value in evaluating the existence of ossicular chain interruption. Although the specificity is high, the sensitivity is low, which is also difficult to accurately judge the fine structure injury such as stapes fracture, especially for those with tympanic hematocele in the early stage after injury, it is easy to miss the diagnosis. One patient in our study was diagnosed as incudostapedial joint dislocation by CT before operation, which was confirmed in operation. But 1 case of incudostapedial joint dislocation and 1 case of stapes neck fracture were not clear before operation, which were found during operation. Our results showed that the ABG of patients with ossicular chain interruption was >35 dBHL, while the others were <35 dBHL (P <0.01) (Table 4). Therefore, the preoperative ABG may have a reference value for judging ossicular chain interruption. Even if it is difficult to determine by HRCT, the ossicular chain interruption should be considered to make full preparations for hearing reconstruction.
The operation time of traumatic facial paralysis is mainly based on the examination results of ENoG test. Fisch has proposed that decompression surgery should be considered once ENoG > 90% within 6 days after facial nerve injury, whether it is rapid or late-onset facial paralysis. Chang and Cass14 have pointed out that within 14 days after injury, the recovery effect of facial paralysis in patients with ENoG > 95% is poor, so facial nerve decompression should be performed as soon as possible. However, because patients with temporal bone fractures are often accompanied by intracranial injury or other serious combined injuries at the same time, it is not suitable for early surgical decompression, and ENoG test cannot be performed in time to evaluate the degree of facial nerve injury. Previous study has reported that patients who delayed facial nerve decompression surgery 1-3 months after injury achieved good recovery of facial nerve function.15 In the 12-month follow-up of the 11 patients in this study, all the 7 patients with relatively shorter preoperative duration of facial paralysis (average was 34.6 days and none of them was longer than 2 months) have recovered to HB-I, while the rest 4 patients who recovered to HB-II or -III had longer preoperative duration of facial paralysis (average was 72 days and 3 of them was longer than 2 months). Although there was no statistical significance (P = 0.09704), considering the small sample size, it may also suggest that the duration of facial paralysis may be an important factor affecting the prognosis to some extent. Therefore, we advocate early surgery for patients with traumatic facial paralysis for better postoperative efficacy. Whether this is an important prognostic factor remains to be further studied with larger sample size in the future.
The retrospective study, the small number of cases, and the lack of long-term results in these patients are the main limitations of our present study, which makes it difficult to conduct stratified and in-depth analysis of prognostic factors affecting the efficacy, such as age, duration of facial paralysis, onset time, and so on. Therefore, this is our preliminary study. Future studies will enroll more patients with multicenter cooperation and increase the duration of follow-up to analyze the relationship between surgical effect and different prognostic factors.
Conclusion
Facial nerve decompression through endoscopic transcanal approach can decompress the geniculate ganglion to the pyramidal segment of facial nerve, which is suitable for patients with traumatic facial paralysis of this segment. Preoperative HRCT combined with localization test can accurately estimate the location of facial nerve injury. Ossicular chain reconstruction during the operation can obtain good audiological recovery, especially for patients with ossicular chain interruption, which is helpful to improve conductive hearing loss. In addition, ABG >35 dBHL has a certain reference value for diagnosis of ossicular chain interruption when it is difficult to be completely judged by HRCT.
Footnotes
Ethics Committee Approval: This study was approved by Ethics Committee of Shanghai Ninth People’s Hospital Affliated to Shanghai Jiao Tong University School of Medicine (Approval No: SH9H-2022-T284-1, Date: September 23, 2022).
Informed Consent: Written informed consent was obtained from the patients who agreed to take part in the study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – L.X.; Design – W.S., L.X.; Supervision – Z.W.; Resources – Z.W.; Materials – W.S., L.X.; Data Collection and/or Processing – Y.W.; Analysis and/or Interpretation – Y.W.; Literature Search – Z.W.; Writing – W.S.; Critical Review – Z.W.
Declaration of Interests: The authors have no conflict of interest to declare.
Funding: This work was supported by Science and Technology Commission of Shanghai Municipality (Grant No. 19441900100 to Zhaoyan Wang).
Reference
- 1. Shankar A, George S, Somaraj S. Evaluation of clinical outcome in traumatic facial nerve paralysis. Int Arch Otorhinolaryngol. 2021;26(1):e010 e019. ( 10.1055/s-0040-1718962) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dahiya R, Keller JD, Litofsky NS, Bankey PE, Bonassar LJ, Megerian CA. Temporal bone fractures: otic capsule sparing versus otic capsule violating clinical and radiographic considerations. J Trauma. 1999;47(6):1079 1083. ( 10.1097/00005373-199912000-00014) [DOI] [PubMed] [Google Scholar]
- 3. Brodie HA, Thompson TC. Management of complications from 820 temporal bone fractures. Am J Otol. 1997;18(2):188 197. ( 10.1016/S0196-0709(97)90107-1) [DOI] [PubMed] [Google Scholar]
- 4. Marchioni D, Alicandri-Ciufelli M, Piccinini A, et al. Surgical anatomy of transcanal endoscopic approach to the tympanic facial nerve. Laryngoscope. 2011;121(7):1565 1573.( 10.1002/lary.21819) [DOI] [PubMed] [Google Scholar]
- 5. Kahinga AA, Han JH, Moon IS. Total transcanal endoscopic facial nerve decompression for traumatic facial nerve palsy. Yonsei Med J. 2018;59(3):457 460. ( 10.3349/ymj.2018.59.3.457) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Movérare T, Lohmander A, Hultcrantz M, Sjögreen L. Peripheral facial palsy: speech communication and oral motor function. Eur Ann Otorhinolaryngol Head Neck Dis. 2017;134(1):27 31. ( 10.1016/j.anorl.2015.12.002) [DOI] [PubMed] [Google Scholar]
- 7. Hamour AF, Mendez AI, Biron VL, et al. Development of the Alberta facial clinical evaluation scale: a patient-centred outcomes instrument for facial nerve paralysis. Clin Otolaryngol. 2019;44(6):919 926. ( 10.1111/coa.13400) [DOI] [PubMed] [Google Scholar]
- 8. Ilea A, Butnaru A, Sfrângeu SA, et al. Role of mastoid pneumatization in temporal bone fractures. AJNR Am J Neuroradiol. 2014;35(7):1398 1404. ( 10.3174/ajnr.A3887) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bonali M, Ghirelli M, Ghizzo M, et al. Endoscopic transcanal approach to geniculate ganglion hemangioma and simultaneous facial nerve reinnervation: a case report. J Int Adv Otol. 2019;15(1):165 168. ( 10.5152/iao.2019.5342) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bonali M, Anschuetz L, Fermi M, et al. The variants of the retro- and hypotympanum: an endoscopic anatomical study. Eur Arch Otorhinolaryngol. 2017;274(5):2141 2148. ( 10.1007/s00405-017-4492-0) [DOI] [PubMed] [Google Scholar]
- 11. Yalçıner G, Kutluhan A, Bozdemir K, Cetin H, Tarlak B, Bilgen AS. Temporal bone fractures: evaluation of 77 patients and a management algorithm. Ulus Travma Acil Cerrahi Derg. 2012;18(5):424 428. ( 10.5505/tjtes.2012.98957) [DOI] [PubMed] [Google Scholar]
- 12. Tos M. Prognosis of hearing loss in temporal bone fractures. J Laryngol Otol. 1971;85(11):1147 1159. ( 10.1017/s0022215100074569) [DOI] [PubMed] [Google Scholar]
- 13. Podoshin L, Fradis M. Hearing loss after head injury. Arch Otolaryngol. 1975;101(1):15 18. ( 10.1001/archotol.1975.00780300019004) [DOI] [PubMed] [Google Scholar]
- 14. Chang CY, Cass SP. Management of facial nerve injury due to temporal bone trauma. Am J Otol. 1999;20(1):96 114. ( 10.1021/bk-2000-0738.ch007) [DOI] [PubMed] [Google Scholar]
- 15. Quaranta A, Campobasso G, Piazza F, Quaranta N, Salonna I. Facial nerve paralysis in temporal bone fractures: outcomes after late decompression surgery. Acta Otolaryngol. 2001;121(5):652 655.( 10.1080/00016480119531) [DOI] [PubMed] [Google Scholar]



 Content of this journal is licensed under a
Content of this journal is licensed under a