Summary
Background
The disease burden of gastrointestinal disease (GD) in China is high, with significant variation across provinces. A comprehensive agreed set of indicators could guide rational resource allocation to support better GD outcomes.
Methods
This study collected data from multiple sources, including national surveillance, surveys, registration systems, and scientific research. Literature reviews and Delphi methods were used to obtain monitoring indicators; the analytic hierarchy process was used to determine indicator weights.
Findings
The China Gastrointestinal Health Index (GHI) system consisted of four dimensions and 46 indicators. The weight of the four dimensions from high to low included the prevalence of gastrointestinal non-neoplastic diseases and gastrointestinal neoplasms (GN) (0.3246), clinical treatment of GD (0.2884), prevention and control of risk factors (0.2606), and exposure to risk factors (0.1264). The highest indicator weight of GHI rank was the successful smoking cessation rate (0.1253), followed by the 5-year survival rate of GN (0.0905), and the examination rate of diagnostic oesophagogastroduodenoscopy (0.0661). The overall GHI for China in 2019 was 49.89, varying from 39.19 to 76.13 across all sub-regions. The top five sub-regions in the total GHI score were in the eastern region.
Interpretation
GHI is the first system designed to monitor gastrointestinal health systematically. In the future, data from sub-regions of China should be used to test and improve the GHI system for its impact.
Funding
This research was supported by the National Health Commission of China, the First Affiliated Hospital of Naval Medical University (2019YXK006), and the Science and Technology Commission of Shanghai Municipality (21Y31900100).
Keywords: China gastrointestinal health index, Index system, Delphi method, Analytic hierarchy process, Weight, Monitoring
Research in context.
Evidence before this study
In the past, comprehensive evaluation was challenging and restricted by the insufficient availability of regional survey data on epidemiology, exposure to risk factors, treatment capabilities for diseases, and treatment outcomes. We searched PubMed from database inception to 2023 without applying any language restrictions, using the following search string: ("Monitoring" [Title/Abstract] OR "Epidemiological Monitoring" [MeSH Terms]) AND "health index" [Title/Abstract]. We systematically reviewed the 116 search results and found 15 relevant original research articles. The advent of big data, coupled with the completion of large-scale surveys and the growing demand for health monitoring, has led to the creation of comprehensive health monitoring indices. These indices, such as the cardiovascular health index, the Child health index, and the Injury index, are designed to assess the health status of groups and provide quantitative guidance for intervention strategies. However, there is no comprehensive evaluation system for regional gastrointestinal health monitoring.
Added value of this study
By utilizing the Delphi method and analytic hierarchy process, a comprehensive index system was established for the quantitative evaluation of regional gastrointestinal health. Along with the scientific evaluation, the GHI includes four dimensions and 46 indicators that can be used by provincial managers to easily and quickly identify areas that need improvement in terms of gastrointestinal disease prevention and control.
Implications of all the available evidence
Our research findings have practical applications for decision-makers who need to assess the effectiveness of policies. Specifically, our results can help identify and address the pain points associated with gastrointestinal diseases. Our research offers valuable insights into the rational allocation of regional resources. By utilizing these insights, low economic regions can invest more effectively in areas of need, while avoiding investments in low output and low efficiency sectors.
Introduction
The gastrointestinal system, including the gastrointestinal tract and accessory organs, plays a vital role in digestion, absorption, metabolism, and maintenance of human health. Gastrointestinal diseases (GD) include gastrointestinal non-neoplastic diseases (GNND) and gastrointestinal neoplasms (GN), which have become important contributors to disability-adjusted life-years (DALYs) and mortality.1 The disease burden of GN is increasing worldwide, and gastric, liver, and colorectal cancers account for three of the top five cancer-related deaths.2 GN accounted for 26% of global cancer incidence and 35% of all cancer-related deaths in 2018.3 China should put more resources into preventing and controlling GN than the United States and the United Kingdom, with a population of 1.4 billion and a special period of cancer transformation.4 Concerns over GNND are also increasing, and besides death, they cause pain, affect the quality of life of patients, and bring a huge economic burden to social development.5, 6, 7, 8
The prevention and control of GD is a process that requires individualized intervention, especially lifestyle changes through education or expensive medical intervention. Long-term and sustained preventive measures require action at global and national levels.9,10 The first step is effectively assessing the prevalence of GD, the risk of GD, and the effectiveness of GD prevention and control. In implementing this initial step, establishing a monitoring system and related indicators to measure the burden and changes in GD is necessary. In the global action plan for the prevention and control of non-communicable diseases 2013–2020, the World Health Organization (WHO) has encouraged the monitoring of chronic diseases and tumours to reduce mortality by 25%.11 The National Institutes of Health (NIH) of the United States provided $3.1 billion to evaluate the annual disease burden and cost of, and carry out research on, gastrointestinal, liver, and pancreatic diseases in 2020, with GI research continuing to capture roughly 7% of the NIH budget.12 In China, long-term plans and policies have been implemented to enhance the surveillance of chronic diseases and tumours, reduce the probability of premature death by 30%, and increase the average life expectancy to 79 years by 2030 compared with the rate in 2015.13, 14, 15, 16
It is necessary to evaluate and monitor the health of the digestive system to achieve the national goal of GD prevention and control in China.17,18 Indicators can be used to monitor disease control and prevention. For example, the adenoma detection rate (ADR) reflects the frequency of colonoscopy and promotes early screening for colorectal tumours, however, it does not measure the GD status of the population.19 Although incidence and mortality are commonly used indicators to evaluate the disease burden of GD, they were unable to fully reflect the prevention and control capabilities.20 System-based monitoring has brought about gains in supply-demand balance for multi-disease prevention.9,21 However, there has been no monitoring of GD, which has compromised equity in the supply and demand of medical resources.
Importantly, an innovative index of GD would help policymakers understand the current situation of GD in China, increase public awareness of GD, and support research to control incidence of GD. Therefore, we reported development of the China Gastrointestinal Health Index (GHI); based on comprehensive and objective data related to GD, the GHI reflects the health status of the digestive system in the Chinese population. Specifically, this paper introduces the establishment of the GHI, describes the processes to select and weight each indicator, and proposes the use of GHI.
Methods
To assess the health status of the digestive system in the Chinese population, a comprehensive GHI should reflect the current prevalence and risk of GD, evaluate the effectiveness of prevention and treatment measures, and emphasise public health policies and population-based and community interventions. To construct the GHI, we conducted a literature review, sought expert advice, screened indicators using the Delphi method, and determined indicator weights using the analytical hierarchy process (AHP). Fig. 1 presents a step-by-step process of the literature review, expert discussion, indicator screening, weight definition, and GHI construction.
Fig. 1.
Process of constructing of GHI.
Defining GHI dimensions
First, guided by the monitoring needs of WHO and Healthy China 2030 for monitoring chronic diseases and tumours and drawing on the research of the cardiovascular health index (CHI), it was determined that the GHI should be composed of four dimensions; the prevalence of GNND and GN, exposure to risk factors, prevention and control of risk factors, and clinical treatment of GD.12,21,22 Using data sources currently available from the National Center for Chronic and Non-communicable Disease Control and Prevention of the Chinese Center for Disease Control and Prevention (CDC) and National Digestive Endoscopy Improvement System (NDEIS), including the study on the burden of disease by the provinces in China, the surveillance survey of chronic diseases and risk factors in China, the epidemiology of digestive system diseases in China, the endoscopic quality control data of NDEIS, and other data sources, we sorted the existing digestive health indicator-related data in the four dimensions. Furthermore, we extensively searched relevant literature to collect widely recognised risk factors for GNND and GN and searched various public data sources at the national level to obtain relevant data. In addition, a wide range of experts in the digestive field was solicited to consult about the indicators and data availability for the diagnosis and treatment of GD. Finally, multiple expert discussion rounds were used to define the GHI indicator. eTable 1 shows the definition, calculation methods and data sources of GHI indicators.23, 24, 25, 26, 27, 28
Defining the GD indicator system using the Delphi method
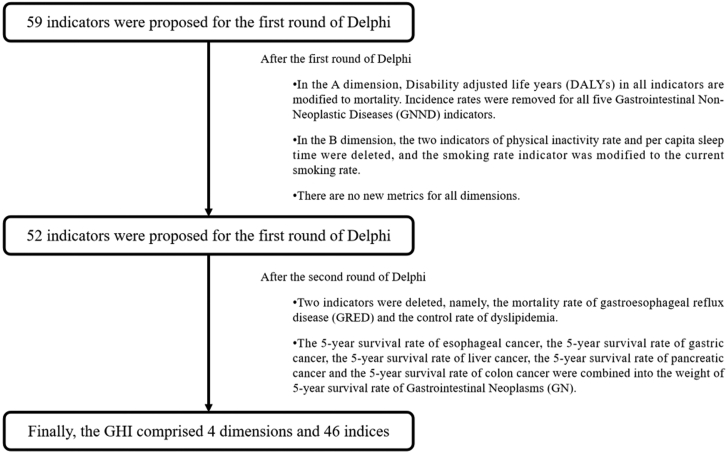
Through literature review, we established an indicator database and conducted a pilot survey to develop an expert consultation questionnaire. Next, we defined the indicator through two rounds of the Delphi method.29 Firstly, professionals in chronic disease prevention and treatment and clinical experts in GD participated in the group consultation. Secondly, the experts scored the importance of each indicator (from 1 representing the lowest degrees of importance to 4 representing the highest degrees of importance) and listed the reasons and evidence of each dimension. The indicator was accepted when the mean value of the index importance score was ≥3 and the coefficient of variation ≤0.5. Finally, the second round of the Delphi method was used to calculate the average and coefficient of variation of each indicator importance score, remove indicators that did not meet the inclusion criteria, and add new indicators according to the suggestions of the experts. The authority coefficient (Cr) was used to express the degree of authority of an expert. The mean and interquartile range (IQR) of the importance scores of each indicator were used to measure the degree of concentration of expert opinions. The higher the mean, the shorter the IQR, indicating that experts' opinions on the importance of indicators were more concentrated. The coordination of experts' judgments on all indicators was represented by the coefficient of variation and Kendall's W. The collected Delphi expert consultation questionnaire was used to establish a database with EpiData v3.1 (Odense, Denmark), double-entry of data was performed, and SPSS software (version 20.0; IBM, USA) was used for data analysis. Fig. 2 shows a flowchart of the Delphi method.
Fig. 2.
Flowchart of Delphi process.
Defining GHI weight with AHP
AHP was used to define the indicator weights for the GHI.30 Firstly, the indicators were layered, and a target tree was established. The indicators of each dimension were used to form a hierarchical structure, and a GHI weight evaluation target tree was constructed. Secondly, YAAHP software (Shanxi Yuan Decision Software Technology Co., Ltd., China) was used to establish a hierarchical structure of the goal tree and generate a pairwise judgment matrix of indicators. Seven senior experts in the field of GD prevention and control were selected to compare the importance of each indicator within the same matrix. The expert group listed the judgment matrix (Table 1) in the questionnaire according to the GHI weight and used the evaluation criteria in Table 2 to assign certain weights to the indicators of the same level according to their values in the previous index. The consistency of the expert judgment matrix was calculated to test the logic of the judgment. When the consistency index (CI) or random consistency ratio (CR) was less than 0.10, the judgment matrix achieved strong consistency, and the weight coefficients were consistent. If consistency was not met, the expert was asked to repeat the scoring process until the consistency of each matrix met the target before submitting the matrix scoring results. This study was based on the scores of experts and the initial weight coefficient, normalised weight coefficient, and combination weight coefficient of each indicator. According to the principle of equal scores for each expert, we determined the average of the scores of the experts and calculated the final weight of each level and indicator. Fig. 3 shows the AHP process.
Table 1.
Examples of judgment matrices marking.
| B1 environmental factors | B2 biological factors | B3 lifestyle | |
|---|---|---|---|
| B1 environmental factors | 1 (b11) | 3(B12) | 5 (b13) |
| B2 biological factors | 1/3 (b21) | 1 (b22) | 3 (b23) |
| B3 lifestyle | 1/5 (b31) | 1/3 (b32) | 1 (b33) |
The above scores are not the real marks used in the AHP for evaluating CHI weights.
Table 2.
Marking criteria of each level of the goal tree.
| Comparison score | Relative importance | Description |
|---|---|---|
| 1 | Equally important | Both contribute equally to the goal |
| 3 | Slightly important | From experience, one indicator is slightly more favourable than the other |
| 5 | More important | From experience, one indicator is more favourable than the other |
| 7 | Very important | One indicator is more favourable than the other and has been proven in practice |
| 9 | Absolutely important | Significant degree of importance |
| (2, 4, 6, 8) | The median value of two adjacent degrees | Use when a compromise is required |
Fig. 3.
Procedure of AHP.
Calculation of GHI markers
Based on the indicator selected by the Delphi method and the indicator weight defined by AHP, the GHI was constructed to calculate the gastrointestinal health score of different regions in China. Regional GHI allows comparisons between different regions, which have different population size, economic development, urban-rural mix, and health systems, and can help formulate public health policies. The maximum score for the GHI is 100 points; the higher the score of each region, the better the GD-related health status.
Due to the differences in dimension, order of magnitude, and reflection of the content of each indicator, the measurement of GHI involved several major steps, including original database data cleaning, index calculation, co-directional transformation, standardisation, percentage transformation, and weighted summation. Firstly, the same trend conversion was adopted for each indicator so that the orientation of the indicators reflecting the health status was consistent with the orientation of the health status represented by GHI. Subsequently, we standardised the index. Preliminary analysis showed that most indexes had a normal distribution. Therefore, the standard normal transformation was used to remove the dimension of each index so that all the transformed indexes obey the standard normal distribution with a mean value of 0 and a standard deviation of 1. The transformation formula is as follows:
refers to the mark of the i th index after standard normal transformation, refers to the initial or co-directional value of the i th index, refers to the mean value of the i th index for each Chinese province, and refers to the standard deviation of the i th index for each province.
Notably, a percentage conversion was necessary to ensure that the final value was between 0 and 100. This was performed by calculating the area under the standard normal distribution curve to the left of the Z value. For any standard normalised index , its score was :
Finally, combined with the standard normalised score and weight of each index, the scores of the different dimensions and the final GHI score of each province were calculated. The calculation method is as follows:
N refers to the number of indicators in a certain dimension or the total number of indicators, and refers to the standard normalised score of the ith index, refers to the index weight.
Ethical considerations
The data involved in this study protected the research subjects through anonymisation and removal of identifying information. This study was a secondary analysis of public survey data involving only province-level indicator results. The original informed consent involved in this study allowed for secondary analysis, and no additional consent was required.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. All authors confirmed that they had full access to all the data in the study and accepted the responsibility to submit for publication.
Results
GHI dimensions and indicators
The intention is that the GHI should be a comprehensive set of objective and specific indices. The composite index model is usually complex and uncertain; therefore, it is necessary to include various factors affecting the index to reflect instantaneity, stability, and continuity. For this reason, we established an index system with four dimensions as follows: the prevalence of GNND and GN, the exposure to risk factors, the prevention and control of risk factors, and the clinical treatment of GD. These dimensions enable researchers to focus on specific elements. Through a literature review, 46 indicators were selected, and an index base was established.
Screening of indicators
In the first round of the Delphi method, we distributed 103 questionnaires (89 experts in the clinical digestive field and 14 experts in the public health field) and received 76 questionnaires (62 experts in the clinical digestive field and 14 experts in the public health field). The degree of enthusiasm of experts was 73.79%. In the second round of the Delphi method, we distributed 76 questionnaires (62 clinical digestive experts and 14 public health experts) and received 68 questionnaires (56 clinical digestive experts and 12 public health experts). For the indicators, the average degree of familiarity, knowledge to judge the program, and the Cr of the experts were 0.85, 0.88, and 0.87, respectively, indicating that the experts selected in this study had relatively high authority.
The opinions of experts were highly concentrated. In the first round of Delphi expert consultation indicators, the importance scores were 35 (IQR: 3.0, 4.0) and 9 (IQR: 4.0, 4.0), with the average importance scores between 2.62 and 3.84. Additionally, in the second round of indicators, the importance scores were 21 (IQR: 3.0, 4.0) and 20 (IQR: 4.0, 4.0), with the mean importance scores between 2.47 and 3.91. The opinions of the experts were highly coordinated. In the first round, the mean coefficient of variation was 0.23 (0.11–0.36). In the second round of indicators, the mean coefficient of variation was 0.16 (0.07–0.42); The Kendall's W of the two rounds of expert consultation were 0.195 and 0.393, respectively, with both P < 0.05, indicating the coordination of the experts' judgments on all indicators was consistent.
According to the principle of indicator screening, after two rounds of the Delphi method, the GHI comprised four dimensions and 46 indicators (Table 3). The data sources (eTable 1) for these indicators included the Global Burden of Disease China (2019), Digestive Endoscopy Annual Data of NEDIS (2019), Chronic Disease Risk Factor Surveillance in China (2019), Chinese Journal of Health Statistics 2020, Report on the State of the Ecology and Environment in China 2019, Inflammatory Bowel Disease Annual Data (2021), annual data of Helicobacter pylori specialist clinics (2021), and annual data on Helicobacter pylori infection in China (2021).
Table 3.
Indicators and weights in GHI.
| Dimension | Sub-dimension | Number | Indicator | Weight |
|---|---|---|---|---|
| A prevalence of GNND and GN | A1 prevalence of GN | A01 | Incidence of oesophageal cancer | 0.028 |
| A02 | Mortality of oesophageal cancer | 0.0208 | ||
| A03 | Incidence of stomach cancer | 0.0401 | ||
| A04 | Mortality of stomach cancer | 0.0271 | ||
| A05 | Incidence of colorectal cancer | 0.0198 | ||
| A06 | Mortality of colorectal cancer | 0.0149 | ||
| A07 | Incidence of liver cancer | 0.0341 | ||
| A08 | Mortality of liver cancer | 0.0097 | ||
| A09 | Incidence of pancreatic cancer | 0.0083 | ||
| A10 | Mortality of pancreatic cancer | 0.0341 | ||
| A2 prevalence of GNND | A11 | Prevalence of liver cirrhosis | 0.0166 | |
| A12 | Mortality of liver cirrhosis | 0.0088 | ||
| A13 | Prevalence of peptic ulcer | 0.0063 | ||
| A14 | Mortality of peptic ulcer | 0.0018 | ||
| A15 | Prevalence of gastro-oesophageal reflux disease | 0.0065 | ||
| A16 | Prevalence of IBD | 0.0122 | ||
| A17 | Mortality of IBD | 0.0046 | ||
| A18 | Prevalence of pancreatitis | 0.0216 | ||
| A19 | Mortality of pancreatitis | 0.0093 | ||
| B exposure to risk factors | B1 environmental factors | B01 | Quality of drinking water | 0.0394 |
| B2 biological factors | B02 | HP infection rate | 0.0122 | |
| B03 | Incidence of hepatitis B and C | 0.0184 | ||
| B3 lifestyle | B04 | Current smoking rate | 0.0159 | |
| B05 | Per capita salt intake | 0.008 | ||
| B06 | Harmful drinking rate | 0.005 | ||
| B07 | Excessive intake of red meat | 0.0056 | ||
| B08 | Insufficient intake rate of vegetable and fruit | 0.0053 | ||
| B09 | Obesity rate | 0.0104 | ||
| B10 | Prevalence of dyslipidemia | 0.0062 | ||
| C prevention and control of risk factors | C1 prevention and control of high-risk factors | C01 | Successful smoking cessation rate | 0.1253 |
| C2 endoscopic screening | C02 | The examination rate of diagnostic oesophagogastroduodenoscopy | 0.0661 | |
| C03 | The examination rate of diagnostic colonoscopy | 0.0232 | ||
| C3 early diagnosis and early treatment of tumours | C04 | Proportion of early cancer in all oesophageal cancer during diagnostic EGD | 0.0139 | |
| C05 | Proportion of early cancer in all gastric cancer during diagnostic EGD | 0.018 | ||
| C06 | Proportion of early cancer in all colorectal cancer during diagnostic colonoscopy | 0.0079 | ||
| C07 | Adenoma detection rate of colonoscopy | 0.0062 | ||
| D clinical treatment of GD | D1 therapeutic capacity | D01 | Proportion of hospitals with gastroenterology department | 0.0194 |
| D02 | Number of gastrointestinal endoscopists | 0.019 | ||
| D03 | Proportion of hospitals with gastrointestinal endoscopy centers | 0.0247 | ||
| D04 | Proportion of hospitals with emergency gastroscopic haemostasis capability | 0.0365 | ||
| D05 | Proportion of hospitals providing primary endoscopic techniques | 0.0234 | ||
| D06 | Proportion of hospitals providing advanced endoscopic techniques | 0.0415 | ||
| D07 | Proportion of regional medical centers for IBD | 0.0113 | ||
| D08 | Proportion of HP standardised outpatient demonstration centers | 0.0111 | ||
| D2 treatment outcome | D09 | Complete resection rate of ESD for early cancer | 0.011 | |
| D10 | 5-Year survival rate of GN | 0.0905 |
ESD, endoscopic submucosal dissection; EGD, oesophagogastroduodenoscopy; IBD, inflammatory bowel disease; HP, Helicobacter pylori.
Index weight
According to the AHP results, the weights of the four dimensions from high to low were as follows: the prevalence of GNND and GN (0.3246), clinical treatment of GD (0.2884), prevention and control of risk factors (0.2606), and exposure to risk factors (0.1264). Regarding the prevalence of GNND and GN, the weight of GN (0.2369) was higher than that of GNND (0.0877). In the dimension of exposure to risk factors, the weight coefficients of the secondary indicators in descending order were lifestyle (0.0564), environmental factors (0.0394), and biological factors (0.0306). In the dimension of prevention and control of risk factors, the weight coefficients of secondary indicators in descending order were prevention and control of high-risk factors (0.1253), endoscopic screening (0.0893), and early diagnosis and treatment of tumours (0.046). In the clinical treatment of GD, therapeutic capacity (0.1869) was higher than the treatment outcome (0.1015). Table 3 shows the list of the weights of the indexes.
Results of GHI
The GHI average score in China was 49.89, with 14 and 17 provinces scoring higher and lower than the national average, respectively. Zhejiang had the highest GHI (76.13), followed by Shanghai (70.44) and Peking (62.73). The lowest scoring provinces were Shanxi (33.19), Qinghai (33.85), and Inner Mongolia (39.77). Fig. 4, eFigs. 1–4, and Table 4 show the detailed GHI results. The ranking of GHI sub-dimensions and secondary indicators are shown in eTables 2 and 3, respectively. The GHI maps can be accessed as an open-source tool through https://digestive-web.doctorworking.cn/ (eFigs. 5–9).
Fig. 4.
GHI scores of provinces in China.
Table 4.
GHI and dimension scores for Chinese provinces.
| Item | GHI | A the prevalence of GNND and GN | B the exposure to risk factors | C the prevention and control of risk factors | D the clinical treatment of GD |
|---|---|---|---|---|---|
| Weight | 0.3246 | 0.1264 | 0.2606 | 0.2884 | |
| Mean score | 49.89 | 16.81 | 6.46 | 12.49 | 14.13 |
| Maximum score | 76.13 | 21.98 | 9.32 | 22.99 | 26.44 |
| Minimum score | 33.19 | 8.36 | 3.55 | 5.13 | 2.54 |
| Max/min score | 2.3 | 2.6 | 2.6 | 4.5 | 10.4 |
Discussion
This study was carried out with multi-centre cooperation, and the team researchers came from the CDC, NEDIS, tertiary hospitals, and other health administrative departments. All data required to calculate GHI were obtained from high-quality research (Global Burden of Disease China) and officially released Chinese data (Digestive Endoscopy Annual Data of the National Health Commission and Chronic Disease Risk Factor Surveillance in China of CDC). These representative data ensured the consistency and stability of the study. The GHI adopted the comprehensive index method and comprehensively compared the indicators of different characteristics, categories, and measurement units. To construct a composite index, we used a literature review, the Delphi method, and AHP, a process commonly used to assess and monitor chronic disease prevention and control systems.21,29,30 In a literature review, we combined qualitative and quantitative analysis using the Delphi method and AHP to summarise the back-to-back evaluation results and face-to-face evaluation opinions of experts, and finally established the GHI system, with the derived weights of the 46 indices.
Three core concepts the development of the GHI. The first was the advantage of a comprehensive evaluation, as evidenced by the successful application of the cardiovascular index.31 The GHI dimensions and indicators reflect the need to adopt a comprehensive method to assess the health status of the digestive system of the ideal population. The GHI included indicators to assess the quality of work performed by clinicians (ADR and complete resection rate of endoscopic submucosal dissection for early cancer), indicators of the impact of a healthy lifestyle (smoking rate, obesity rate, and insufficient fruit and vegetable intake rate), digestive system health influencing factors (hepatitis incidence, Helicobacter pylori infection rate, blood lipids, and blood sugar), clinical treatment indicators, and early screening indicators based on public health intervention populations (early tumour detection rate and penetration rate of endoscopy). The GHI is a multidimensional and multi-index concept. The China GHI is weighted 32% to reflect the current prevalence and disease burden of GD, and 68% for the three dimensions of GD measures.
The GHI can provide a focus on surveillance of GD. Among the three dimensions used to monitor GD, clinical treatment of GD was weighted highest at 28.84%. Within this dimension, 5-year survival rate of GN was weighted 0.0905, accounting for the highest proportion, followed by the proportion of hospitals providing advanced endoscopic techniques (0.0415) and the proportion of hospitals with emergency gastroscopic haemostasis capability (0.0365). These three indicators ranked second, fourth, and seventh of the 46 GHI indicators, respectively. The highest weighted indicator was the successful smoking cessation rate (0.1253). This reflects the importance of smoking cessation in influencing better outcomes for early diagnosis, early treatment, and prevention and treatment of GN.3,32,33 In the GHI, the weight of the prevention and control dimension of risk factors was 26.06%. Risk factor intervention can effectively reduce the incidence and mortality of GD, especially GN, and this effect applies to the complete life cycle of the entire population and individuals. As an example, amongst possible cancer control measures in Australia, “smoke-free” initiatives have the potential have the largest impact on potential years of life lost.34 In addition, the popularisation and effective use of endoscopy can improve the benefits of early tumour screening and prevention in the entire population.35,36 As a developing country, China has relatively scarce health resources, and the average number of endoscopies, and the average number of endoscopists is far below demand. Comprehensive early diagnosis, treatment, and prevention measures have been proven to be the most cost-effective interventions in the disease control field, especially in cancer prevention and treatment.37,38 In the clinical treatment of GD dimension, therapeutic capacity weighting was the highest; therefore, it is crucial to improve the capacity for diagnosis and treatment, especially prevention, screening and early control of GD.
Monitoring will contribute to the optimisation of resource allocation and use in China’s sub-regions. Research by the WHO showed that low- and middle-income countries performed poorly in monitoring and researching diseases and risk interventions in response to chronic disease epidemics.11 Similarly, this also applies to China, and the increasing burden of GD in China has led the government to implement policies and programs to address this increase.13, 14, 15 The GHI can be used to support China’s GD goals, including increasing life expectancy, reducing premature mortality, and optimising the distribution of medical resources between sub-regions. Similar to the success of CHI, the GHI can facilitate inter-provincial comparisons, through assessing a province’s performance with respect to achieving control of GD incidence, prevention and control of GD risks, and GD treatment.39 For example, the total GHI score of Shanghai ranked second, but the index identifies components that can be improved. The exposure to environmental risk factors is relatively high (mainly due to poor surface water quality), as is GD burden (reflected in morbidity and mortality). It is suggested that these should be the focus of digestive health intervention in Shanghai. Additionally, the GHI can increase public awareness of GD, help policymakers evaluate the policies relating to GD, and provide a reference for developing countries with a relative lack of medical resources on how to monitor GD prevention and control.
The future use of GHI involves evaluating the scores among provinces, improving the dimensions and indicator scores for each province, and improving the evaluation system of GHI. The eastern region of China has higher GHI scores than the western region. The five provinces with the highest GHI are all in the eastern region, the Shanxi Province, with the lowest score in the central region, and the other four provinces in the lowest scoring five are in the western region. Endoscopic screening, early diagnosis, early treatment, and therapeutic capacity are generally better in the eastern region. However, the prevalence and disease burden of GN is relatively heavy, and individual areas such as Shanghai are exposed to serious environmental risk factors (poor surface water quality). Governance in this area should be strengthened. Biological risk factor exposure (e.g., Helicobacter pylori infection and the incidence of hepatitis B and C), prevention and control of high-risk factors (the successful smoking cessation rate), endoscopic screening, and treatment outcomes were generally poor in the western and central regions. The results for each province can be used to support implementation of targeted interventions and policies, for example strengthening the efforts supporting smoking cessation and endoscopic screening in Shanxi, preventing and treating Helicobacter pylori infection and hepatitis B and C in Qinghai, and strengthening education about healthy diets in Inner Mongolia. In the future, we will regularly publish national and provincial GHI scores, research regional and municipal GHI evaluation systems, and formulate GD prevention and control measures in pilot cities based on GHI results.
This study had several limitations. One of the limitations of this study was the lack of process indicators relating to clinical treatment of GD. Considering the lack of recognised indicators of the GD treatment process and the scarcity of corresponding national data, this secondary indicator could not be included in the GHI. In the future, we plan to conduct corresponding research and collect and monitor indicators related to the treatment process. Another limitation of the study was the lack of accurate information on 5-year survival rates for oesophageal, gastric, colorectal, liver, and pancreatic tumours by province. The low quality of single-disease epidemiological studies in some provinces would impact the reliability of GHI evaluations. After expert discussion, these were replaced by the 5-year survival rate of patients with GN. This substitution affects the precision of provincial intervention policies. In addition, although both literature review and the Delphi method are utilized to decrease the heterogeneity of indicators, the bias resulting from heterogeneity cannot be entirely eradicated, like other indexes. As a solution, we plan to enhance the relevant dimensions in the updated version of the GHI in order to decrease heterogeneity and enhance clinical significance. Finally, indicators such as disability adjusted life years and mortality to incidence ratio were not included in the GHI. This is because the GHI is mainly used by sub-regional managers to find the weak links, so the indicators should be easy to understand and apply. Although this will affect the evaluation effectiveness of the disease burden dimension, the impact on the exposure of weak links is acceptable. We will further refine the indicators during application, validation, and feedback.
In summary, the GHI of China is a comprehensive evaluation system to support control of GD. The comprehensive GHI score helps us to improve our understanding of GD in a more intuitive and simple way. The GHI evaluation system has 46 indicators within four dimensions. These dimensions and indicators enable different GHI researchers to focus on specific elements that can support GD prevention and control, reduce disease morbidity and mortality, and promote the improvement of GD management in China. We will collect data and calculate the GHI scores over several years, identify changes in GD, and evaluate relevant policies and interventions.
Contributors
Zhao-Shen Li, Rong Wan, Mai-Geng Zhou, and Luo-Wei Wang designed the study. Zhi-Yuan Cheng, Ye Gao, and Han Lin conceptualized and wrote this article with assistance and feedback from the other co-authors. Fan Mao took on the work of methodology and data calculation. Ying-Ying Jiang and Ting Ling Xu took on the work of data calculation. Chang Sun and Lei Xin took on the work of project administration. Zhao-Shen Li and Rong Wan took on the work of conceptualization and supervision. Mai-Geng Zhou took on the work of project administration and resources. Luo-Wei Wang took on the work of funding acquisition and writing review and editing. Mai-Geng Zhou, Ya-Min Bai, Li-Min Wang, Cheng-Shi Yu, Ying-Ying Jiang, Fan Mao, Wen-Qiang Wei, Wan-Qing Chen, Jian-Ping Hu, Zhao-Shen Li, Luo-Wei Wang, Zhen-Dong Jin, Yi-Qi Du, Min-Hu Chen, Ying-Lian Xiao, Ren Mao, Xiao-Hua Hou, Jia-Ming Qian, Hong Yang, Li-Ya Zhou, Nong-Hua Lv, Duo-Wu Zou, Bang-Mao Wang, Bin Lv, Jing-Yuan Fang, Kai-Chun Wu, Yan-Qing Li, and Xiao-Ping Zou made substantial contributions to ensure the scientific nature of the index. All authors had full access to all the data in the study and accept responsibility for the decision to submit the manuscript for publication.
Data sharing statement
The raw data for GHI make publicly available through Mendeley Data (Cheng, Zhiyuan (2023), "The raw data of the China Gastrointestinal Health Index," Mendeley Data, V1, https://doi.org/10.17632/rrhbrsxzr8.1). Delphi method questionnaires are available in supplemental materials (pp 16–34).
Declaration of interests
Luo-Wei Wang has received research support from the National Health Commission of China, the First Affiliated Hospital of Naval Medical University (2019YXK006), and the Science and Technology Commission of Shanghai Municipality (21Y31900100). All other authors declare no competing interests.
Acknowledgements
The authors would like to thank the members of the CGHEG for their professional guidance on the GHI construction. Experts from CGHEG include the Policy Steering Group [Mai-Geng Zhou, Ya-Min Bai, Li-Min Wang, Cheng-Shi Yu, Ying-Ying Jiang, and Fan Mao (National Center for Chronic and Noncommunicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention); Wen-Qiang Wei and Wan-Qing Chen (National Cancer Center); Yu-Hui Zhang (Health Development Research Center of the National Health Commission); Jian-Ping Hu (Statistical Information Center of the National Health Commission)] and Clinical Profesional Group [Zhao-Shen Li, Luo-Wei Wang, Zhen-Dong Jin, and Yi-Qi Du (The First Affiliated Hospital of Naval Military Medical University); Min-Hu Chen, Ying-Lian Xiao, and Ren Mao (The First Affiliated Hospital of Sun Yat-sen University); Xiao-Hua Hou (Union Hospital Affiliated to Tongji Medical College, Huazhong University of Science and Technology); Jia-Ming Qian and Hong Yang (Peking Union Medical College Hospital); Li-Ya Zhou (Peking University Third Hospital); Nong-Hua Lv (The First Affiliated Hospital of Nanchang University); Duo-Wu Zou (Ruijin Hospital Affiliated to Shanghai Jiao Tong University School of Medicine); Bang-Mao Wang (Tianjin Medical University General Hospital); Bin Lv (The First Affiliated Hospital of Zhejiang University of Traditional Chinese Medicine); Jing-Yuan Fang (Renji Hospital of Shanghai Jiao Tong University School of Medicine); Kai-Chun Wu (Xijing Hospital of Air Force Military Medical University); Yan-Qing Li (Qilu Hospital of Shandong University); Xiao-Ping Zou (Nanjing Drum Tower Hospital)]. We would also like to thank the experts and professors who participated in the Delphi method and the staff of the National Center for Chronic and Noncommunicable Disease Control and Prevention who participated in data collection and collation. The Delphi questionnaires and raw data can be found in the Multimedia Appendices.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100810.
Contributor Information
Zhao-Shen Li, Email: zhsl@vip.163.com.
Rong Wan, Email: doctorwanrong@126.com.
Mai-Geng Zhou, Email: maigengzhou@126.com.
Luo-Wei Wang, Email: wangluoweimd@126.com.
China Gastrointestinal Health Expert Group (CGHEG):
Mai-Geng Zhou, Ya-Min Bai, Li-Min Wang, Cheng-Shi Yu, Ying-Ying Jiang, Fan Mao, Wen-Qiang Wei, Wan-Qing Chen, Yu-Hui Zhang, Jian-Ping Hu, Zhao-Shen Li, Luo-Wei Wang, Zhen-Dong Jin, Yi-Qi Du, Min-Hu Chen, Ying-Lian Xiao, Ren Mao, Xiao-Hua Hou, Jia-Ming Qian, Hong Yang, Li-Ya Zhou, Nong-Hua Lv, Duo-Wu Zou, Bang-Mao Wang, Bin Lv, Jing-Yuan Fang, Kai-Chun Wu, Yan-Qing Li, and Xiao-Ping Zou
Appendix A. Supplementary data
References
- 1.Vos T., Lim S.S., Abbafati C., et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sung H., Ferlay J., Siegel R.L., et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 3.Qiu H., Cao S., Xu R. Cancer incidence, mortality, and burden in China: a time-trend analysis and comparison with the United States and United Kingdom based on the global epidemiological data released in 2020. Cancer Commun. 2021;41(10):1037. doi: 10.1002/cac2.12197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arnold M., Abnet C.C., Neale R.E., et al. Global burden of 5 major types of gastrointestinal cancer. Gastroenterology. 2020;159(1):335–349.e15. doi: 10.1053/j.gastro.2020.02.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiao J., Wang F., Wong N.K., et al. Global liver disease burdens and research trends: analysis from a Chinese perspective. J Hepatol. 2019;71(1):212–221. doi: 10.1016/j.jhep.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 6.Jairath V., Feagan B.G. Global burden of inflammatory bowel disease. Lancet Gastroenterol Hepatol. 2020;5(1):2–3. doi: 10.1016/S2468-1253(19)30358-9. [DOI] [PubMed] [Google Scholar]
- 7.Xie X., Ren K., Zhou Z., Dang C., Zhang H. The global, regional and national burden of peptic ulcer disease from 1990 to 2019: a population-based study. BMC Gastroenterol. 2022;22(1):58. doi: 10.1186/s12876-022-02130-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ouyang G., Pan G., Liu Q., et al. The global, regional, and national burden of pancreatitis in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. BMC Med. 2020;18(1):388. doi: 10.1186/s12916-020-01859-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tung K.T.S., Wong R.S., Ho F.K., et al. Development and validation of indicators for population injury surveillance in Hong Kong: development and usability study. JMIR Public Health Surveill. 2022;8(8) doi: 10.2196/36861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li Y., Zhang C., Zhan P., Fu H., Yip W. Trends and projections of universal health coverage indicators in China, 1993–2030: an analysis of data from four nationwide household surveys. Lancet Reg Health West Pac. 2023;31 doi: 10.1016/j.lanwpc.2022.100646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization Global action plan for the prevention and control of noncommunicable diseases 2013-2020 [Internet] 2013. https://apps.who.int/iris/handle/10665/94384 iii, 103 p. Available from:
- 12.Peery A.F., Crockett S.D., Murphy C.C., et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2021. Gastroenterology. 2022;162(2):621–644. doi: 10.1053/j.gastro.2021.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.CPC Central Committee State Council the plan for “Healthy China 2030” 2016 [Internet] http://www.gov.cn/gongbao/content/2016/content_5133024.htm Available from:
- 14.China’s medium and long-term plan for the prevention and treatment of chronic diseases (2017-2025) [Internet] http://www.gov.cn/xinwen/2017-02/14/content_5167942.htm Available from: [DOI] [PMC free article] [PubMed]
- 15.Work plan for comprehensively improving the comprehensive capacity of county-level hospitals (2018-2020) [Internet] http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=1610d9f0341642b3b9c44d7491c98b4c Available from:
- 16.Bai Y., Zhang Y., Zotova O., et al. Healthy cities initiative in China: progress, challenges, and the way forward. Lancet Reg Health West Pac. 2022;27 doi: 10.1016/j.lanwpc.2022.100539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.So W.K.W., Chan D.N.S., Law B.M.H., Rana T., Wong C.L. Achieving equitable access to cancer screening services to reduce the cancer burden in the Asia-Pacific region: experience from Hong Kong. Lancet Reg Health West Pac. 2022;29 doi: 10.1016/j.lanwpc.2022.100587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xu L., Zhou C., Luo S., Chan D.K., McLaws M.L., Liang W. Modernising infectious disease surveillance and an early-warning system: the need for China’s action. Lancet Reg Health West Pac. 2022;23 doi: 10.1016/j.lanwpc.2022.100485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schottinger J.E., Jensen C.D., Ghai N.R., et al. Association of physician adenoma detection rates with postcolonoscopy colorectal cancer. JAMA. 2022;327(21):2114. doi: 10.1001/jama.2022.6644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Global Burden of Disease 2019 Cancer Collaboration. Kocarnik J.M., Compton K., et al. Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 2022;8(3):420–444. doi: 10.1001/jamaoncol.2021.6987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jiang Y., Mao F., Li Y., et al. Construction of China cardiovascular health index. BMC Public Health. 2018;18(1):937. doi: 10.1186/s12889-018-5647-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World health statistics 2022: monitoring health for the SDGs, sustainable development goals [Internet] https://www.who.int/publications-detail-redirect/9789240051157 Available from:
- 23.China health statistical yearbook 2020 [Internet] http://www.nhc.gov.cn/mohwsbwstjxxzx/tjtjnj/202112/dcd39654d66c4e6abf4d7b1389becd01.shtml Available from:
- 24.Bulletin on the State of China’s ecological environment 2019 [Internet] https://www.mee.gov.cn/hjzl/sthjzk/zghjzkgb/ Available from:
- 25.Xin L., Gao Y., Cheng Z., et al. Utilization and quality assessment of digestive endoscopy in China: results from 5-year consecutive nationwide surveys. Chin Med J. 2022;135(16):2003–2010. doi: 10.1097/CM9.0000000000002366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhou X.Z., Lyu N.H., Zhu H.Y., et al. Large-scale, national, family-based epidemiological study on Helicobacter pylori infection in China: the time to change practice for related disease prevention. Gut. 2023;72(5):855–869. doi: 10.1136/gutjnl-2022-328965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gao Y., Xin L., Lin H., et al. Machine learning-based automated sponge cytology for screening of oesophageal squamous cell carcinoma and adenocarcinoma of the oesophagogastric junction: a nationwide, multicohort, prospective study. Lancet Gastroenterol Hepatol. 2023;8(5):432–445. doi: 10.1016/S2468-1253(23)00004-3. [DOI] [PubMed] [Google Scholar]
- 28.Xin L., Gao Y., Wang T.J., et al. EUS development in China: results from national surveys in 2013 and 2020. Endosc Ultrasound. 2023;12(1):90–95. doi: 10.4103/EUS-D-22-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hasson F., Keeney S., McKenna H. Research guidelines for the Delphi survey technique: Delphi survey technique. J Adv Nurs. 2000;32(4):1008–1015. [PubMed] [Google Scholar]
- 30.Schmidt K., Aumann I., Hollander I., Damm K., von der Schulenburg J.M.G. Applying the analytic hierarchy process in healthcare research: a systematic literature review and evaluation of reporting. BMC Med Inform Decis Mak. 2015;15(1):112. doi: 10.1186/s12911-015-0234-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhou M., Liu J., Jiang Y., et al. Use of the cardiovascular health index to assess cardiovascular health in China: an integral innovative approach. Lancet. 2018;392 [Google Scholar]
- 32.Mabe K., Inoue K., Kamada T., Kato K., Kato M., Haruma K. Endoscopic screening for gastric cancer in Japan: current status and future perspectives. Dig Endosc. 2022;34(3):412–419. doi: 10.1111/den.14063. [DOI] [PubMed] [Google Scholar]
- 33.Kanth P., Inadomi J.M. Screening and prevention of colorectal cancer. BMJ. 2021;374 doi: 10.1136/bmj.n1855. [DOI] [PubMed] [Google Scholar]
- 34.Ward J.E., Young J.M., Jilfs P. Population-based cancer control: where is the greatest benefit from proven strategies to ‘Regain’ years of life lost prematurely? Aust N Z J Public Health. 1999;23(5):538–540. doi: 10.1111/j.1467-842x.1999.tb01314.x. [DOI] [PubMed] [Google Scholar]
- 35.Săftoiu A., Hassan C., Areia M., et al. Role of gastrointestinal endoscopy in the screening of digestive tract cancers in Europe: European Society of Gastrointestinal Endoscopy (ESGE) position statement. Endoscopy. 2020;52(4):293–304. doi: 10.1055/a-1104-5245. [DOI] [PubMed] [Google Scholar]
- 36.Zong L., Abe M., Seto Y., Ji J. The challenge of screening for early gastric cancer in China. Lancet. 2016;388(10060):2606. doi: 10.1016/S0140-6736(16)32226-7. [DOI] [PubMed] [Google Scholar]
- 37.National Cancer Center, China. Expert Group of the Development of China Guideline for the Screening. Early Detection and Early Treatment of Colorectal Cancer China guideline for the screening, early detection and early treatment of colorectal cancer (2020, Beijing) Zhonghua Zhong Liu Za Zhi. 2021;43(1):16–38. doi: 10.3760/cma.j.cn112152-20210105-00010. [DOI] [PubMed] [Google Scholar]
- 38.He J., Chen W.Q., Li Z.S., et al. China guideline for the screening, early detection and early treatment of esophageal cancer (2022, Beijing) Zhonghua Zhong Liu Za Zhi. 2022;44(6):491–522. doi: 10.3760/cma.j.cn112152-20220517-00348. [DOI] [PubMed] [Google Scholar]
- 39.Status of cardiovascular disease epidemics and its risk factors prevention and control in China: an evaluation based on China cardiovascular health index of 2017. Zhonghua Yu Fang Yi Xue Za Zhi. 2021;55(11):1280–1286. doi: 10.3760/cma.j.cn112150-20210822-00817. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.